Pain management modalities US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pain management modalities. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pain management modalities US Medical PG Question 1: A 65-year-old man presents to the dermatology clinic to have a basal cell carcinoma excised from his upper back. The lesion measures 2.3 x 3.2 cm. He has a medical history significant for hypertension and diabetes mellitus type II, for which he takes lisinopril and metformin, respectively. He has had a basal cell carcinoma before which was excised in the clinic without complications. Which of the following modes of anesthesia should be used for this procedure?
- A. Moderate sedation
- B. Peripheral nerve block
- C. General anesthesia
- D. Spinal anesthesia
- E. Local anesthesia (Correct Answer)
Pain management modalities Explanation: ***Local anesthesia***
- This is the preferred method for **basal cell carcinoma excisions**, especially for lesions of this size and location, as it provides adequate pain control with minimal systemic effects.
- The patient's prior uncomplicated excision under local anesthesia further supports its suitability and safety for this procedure.
*Moderate sedation*
- While it can provide comfort, it involves systemic medications that carry risks of **respiratory depression** and **hemodynamic instability**, which are generally unnecessary for a routine skin excision in a stable patient.
- It also requires more extensive monitoring and recovery time compared to local anesthesia.
*Peripheral nerve block*
- A peripheral nerve block might be considered for larger or deeper excisions in specific anatomical areas, but for a typical basal cell carcinoma on the back, **infiltration with local anesthetic** is usually sufficient and less invasive than a nerve block.
- It is not routinely necessary for superficial skin excisions of this nature.
*General anesthesia*
- This is **excessive and unnecessary** for a routine basal cell carcinoma excision, especially given the patient's comorbidities of hypertension and diabetes, which would increase the risks associated with general anesthesia.
- General anesthesia is reserved for very extensive resections, complex reconstructions, or patients unable to cooperate under local anesthesia.
*Spinal anesthesia*
- **Spinal anesthesia** is typically used for procedures involving the lower abdomen, perineum, or lower extremities, and it is **not indicated** for an excision on the upper back.
- It carries risks such as post-dural puncture headache and hypotension, which are unwarranted for this type of superficial surgery.
Pain management modalities US Medical PG Question 2: A 32-year-old man with a history of alcohol binge drinking and polysubstance use is found down in his hotel room with bottles of alcohol, oxycodone, alprazolam, amphetamine-dextroamphetamine, and tadalafil. When EMS arrives, he appears comatose with pinpoint pupils and oxygen saturation of 80% on room air. He is intubated at the scene and airlifted to the nearest intensive care unit. Body temperature is 95 degrees F (35 degrees C). Creatine phosphokinase is 12,000 U/L. MRI of the brain demonstrates extensive infarcts consistent with acute hypoxic ischemic injury. Which of the following is the likely culprit for his overdose?
- A. Amphetamines
- B. Phosphodiesterase-5 (PDE-5) inhibitors
- C. Alcohol
- D. Benzodiazepines
- E. Opioids (Correct Answer)
Pain management modalities Explanation: ***Opioids***
- The patient's presentation with **pinpoint pupils**, **respiratory depression** (oxygen saturation 80%, requiring intubation), and coma is highly characteristic of **opioid overdose**.
- **Hypothermia** and **rhabdomyolysis** (elevated CK) are common complications of severe opioid toxicity due to prolonged immobility and hypoperfusion.
*Amphetamines*
- Amphetamine overdose typically causes **mydriasis (dilated pupils)**, **tachycardia**, **hypertension**, and **hyperthermia**, which are contrary to the patient's presentation.
- While amphetamines can cause rhabdomyolysis and altered mental status, the pinpoint pupils and hypothermia rule it out as the primary cause of his comatose state.
*Phosphodiesterase-5 (PDE-5) inhibitors*
- PDE-5 inhibitors like tadalafil primarily cause **vasodilation**, which can lead to **hypotension**, headaches, and flushing.
- They do not typically cause **respiratory depression**, **pinpoint pupils**, or coma, making it an unlikely culprit for this severe presentation.
*Alcohol*
- While excessive alcohol consumption can cause **CNS depression**, coma, and respiratory depression, it typically results in **dilated or normal pupils**, not pinpoint pupils.
- The combination of pinpoint pupils and severe respiratory depression points more strongly towards opioid toxicity.
*Benzodiazepines*
- Benzodiazepine overdose causes **CNS depression**, respiratory depression, and coma, but typically presents with **normal or slightly dilated pupils**.
- While benzodiazepines can exacerbate opioid effects, the classic **pinpoint pupils** are the key differentiating factor pointing to opioids.
Pain management modalities US Medical PG Question 3: A 25-year-old man is brought to the emergency department after his girlfriend discovered him at home in a minimally responsive state. He has a history of drinking alcohol excessively and using illicit drugs. On arrival, he does not respond to commands but withdraws all extremities to pain. His pulse is 90/min, respirations are 8/min, and blood pressure is 130/90 mm Hg. Pulse oximetry while receiving bag-valve-mask ventilation shows an oxygen saturation of 95%. Examination shows cool, dry skin, with scattered track marks on his arms and legs. The pupils are pinpoint and react sluggishly to light. His serum blood glucose level is 80 mg/dL. The most appropriate next step in management is intravenous administration of which of the following?
- A. Fomepizole
- B. Naltrexone
- C. Methadone
- D. Naloxone (Correct Answer)
- E. Phentolamine
Pain management modalities Explanation: ***Naloxone***
- The patient presents with classic signs of **opioid overdose**: altered mental status, **respiratory depression** (8/min), and **pinpoint pupils**.
- **Naloxone** is an opioid antagonist that rapidly reverses the effects of opioid toxicity and is the most appropriate first-line treatment in this scenario.
*Fomepizole*
- This medication is used as an antidote for **methanol** and **ethylene glycol poisoning**, which typically present with metabolic acidosis and renal failure, not pinpoint pupils and respiratory depression.
- There are no clinical signs in this patient indicative of methanol or ethylene glycol ingestion.
*Naltrexone*
- **Naltrexone** is an opioid antagonist used for long-term management of opioid use disorder or alcohol dependence, but it is not used in acute overdose resuscitation due to its slower onset and formulation (oral or long-acting injectable).
- Its primary role is to prevent relapse, not to reverse acute respiratory depression.
*Methadone*
- **Methadone** is a long-acting opioid agonist used for opioid replacement therapy and chronic pain management.
- Administering methadone would worsen the patient's opioid-induced respiratory depression and central nervous system depression.
*Phentolamine*
- **Phentolamine** is an alpha-adrenergic blocker used to treat hypertensive crises, particularly those caused by pheochromocytoma or extravasation of vasopressors.
- It has no role in managing opioid overdose and could lead to hypotension in this patient.
Pain management modalities US Medical PG Question 4: 2 hours after being admitted to the hospital because of a fracture of the right ankle, a 75-year-old man continues to complain of pain despite treatment with acetaminophen and ibuprofen. He has a history of dementia and cannot recall his medical history. The presence of which of the following features would most likely be a reason to avoid treatment with morphine in this patient?
- A. Severe hypertension
- B. Persistent cough
- C. Biliary tract dysfunction
- D. Tachypnea (Correct Answer)
- E. Watery diarrhea
Pain management modalities Explanation: ***Tachypnea***
- **Tachypnea** (increased respiratory rate) can indicate underlying **respiratory compromise**, making morphine use risky due to its potential for **respiratory depression**.
- In a 75-year-old with a fracture and possible underlying health issues, exacerbating respiratory distress with opioids could be dangerous.
*Severe hypertension*
- While morphine can cause **hypotension** due to vasodilation, it is not typically contraindicated in severe hypertension.
- In fact, the hypotensive effect of morphine can sometimes be beneficial in conditions like **acute pulmonary edema** associated with hypertension.
*Persistent cough*
- Morphine is known to have **antitussive effects**, meaning it can help suppress a cough.
- Therefore, a persistent cough would more likely be a reason *to use* morphine, rather than avoid it, especially if the cough is non-productive and distressing.
*Biliary tract dysfunction*
- Morphine can cause **spasm of the sphincter of Oddi**, leading to increased pressure in the biliary tract and potentially exacerbating pain in patients with biliary dysfunction.
- However, this is usually a concern for patients with pre-existing biliary colic or pancreatitis, and not a primary contraindication in acute pain management unless other safer alternatives are available.
*Watery diarrhea*
- Opioids like morphine are well-known to cause **constipation** by slowing gut motility, due to their action on mu-opioid receptors in the enteric nervous system.
- Therefore, watery diarrhea would not be a reason to avoid morphine; in some cases, the constipating effect could even be considered beneficial.
Pain management modalities US Medical PG Question 5: A 28-year-old woman with a past medical history of fibromyalgia presents to her primary care provider for her annual well visit. She reports that her pain has become more severe over the last several weeks and is no longer well-controlled by NSAIDs. She notes that the pain is beginning to interfere with her sleep and that she feels she no longer has energy to take care of her 2-year-old son. Upon questioning, the patient also endorses feeling more down than usual recently, little interest in seeing friends, and difficulty concentrating on her work. She admits to feeling that she would be “better off dead.” The patient feels strongly that the worsening pain is driving these changes in her mood and that she would feel better if her pain was better controlled. Which of the following is the best next step in management?
- A. Ask the patient if she has an idea about how she might hurt herself (Correct Answer)
- B. Initiate pharmacotherapy with duloxetine and refer for psychotherapy
- C. Ask the patient if she would voluntarily enter a psychiatric hospital
- D. Add acetaminophen and gabapentin to the patient’s pain regimen
- E. Initiate pharmacotherapy with amitriptyline and refer for psychotherapy
Pain management modalities Explanation: ***Ask the patient if she has an idea about how she might hurt herself***
- The patient's statement "feeling that she would be better off dead," combined with symptoms of depression (low mood, anhedonia, difficulty concentrating, low energy), indicates a **high risk of suicidality**.
- Directly inquiring about **suicidal ideation and plans** is the most crucial next step to assess the immediate danger and determine the appropriate level of intervention.
*Initiate pharmacotherapy with duloxetine and refer for psychotherapy*
- While duloxetine is an appropriate medication for both fibromyalgia pain and depression, and psychotherapy is beneficial, these actions do not address the **immediate safety concern** regarding suicide risk.
- Starting treatment without a thorough **suicide risk assessment** could be dangerous if the patient has an active plan or is imminent danger.
*Ask the patient if she would voluntarily enter a psychiatric hospital*
- This question is premature. Before discussing psychiatric hospitalization, it is essential to first assess the **severity and immediacy of suicidal intent** by directly asking about plans and means.
- A patient may deny voluntary admission even if at high risk, requiring a different approach.
*Add acetaminophen and gabapentin to the patient’s pain regimen*
- This option focuses solely on pain management, which, while relevant to fibromyalgia, **fails to address the severe depressive symptoms and suicidal ideation**.
- Treating pain alone without addressing the psychiatric crisis could lead to a catastrophic outcome.
*Initiate pharmacotherapy with amitriptyline and refer for psychotherapy*
- Amitriptyline can be used for fibromyalgia and depression, and psychotherapy is appropriate, but similar to duloxetine, this option **does not prioritize the immediate assessment of suicidality**.
- A comprehensive risk assessment must precede or occur simultaneously with treatment initiation in such a high-risk scenario.
Pain management modalities US Medical PG Question 6: A 36-year-old man is admitted to the hospital for treatment of burn wounds on his upper extremities. Analgesic therapy with an opioid drug is begun. Shortly after, the patient develops chills, diaphoresis, nausea, and abdominal pain. On further questioning, the patient reports that he has been smoking opium at home to help him ""deal with the depression and pain.” This patient was most likely given which of the following opioid drugs?
- A. Butorphanol (Correct Answer)
- B. Oxycodone
- C. Morphine
- D. Fentanyl
- E. Hydrocodone
Pain management modalities Explanation: ***Butorphanol***
- **Butorphanol** is a **mixed opioid agonist-antagonist** that acts as a **kappa (κ) receptor agonist** and **mu (μ) receptor antagonist/partial agonist**.
- In opioid-dependent patients who use **mu receptor agonists** (like opium), butorphanol can precipitate **acute opioid withdrawal** by displacing full agonists from mu receptors and blocking their effects.
- The patient's symptoms of chills, diaphoresis, nausea, and abdominal pain are classic signs of **acute opioid withdrawal syndrome**.
*Oxycodone*
- **Oxycodone** is a **full mu opioid receptor agonist** and would not precipitate withdrawal in an opioid-dependent patient.
- Administering oxycodone would provide continued mu receptor stimulation, potentially alleviating withdrawal symptoms or maintaining the patient's opioid dependence.
*Morphine*
- **Morphine** is a **full mu opioid receptor agonist** and would not cause withdrawal in an opioid-dependent individual.
- It would continue to stimulate mu opioid receptors, providing analgesia and preventing withdrawal symptoms.
*Fentanyl*
- **Fentanyl** is a potent **full mu opioid receptor agonist** and would provide continued opioid receptor stimulation.
- Its administration would prevent withdrawal and provide effective analgesia in an opioid-tolerant patient.
*Hydrocodone*
- **Hydrocodone** is a **full mu opioid receptor agonist** and would not induce withdrawal symptoms.
- Like other full agonists, it would continue mu receptor activation, providing analgesia without precipitating withdrawal.
Pain management modalities US Medical PG Question 7: A 42-year-old man presents to his family physician for evaluation of oral pain. He states that he has increasing pain in a molar on the top left of his mouth. The pain started 1 week ago and has been progressively worsening since then. His medical history is significant for hypertension and type 2 diabetes mellitus, both of which are currently controlled with lifestyle modifications. His blood pressure is 124/86 mm Hg, heart rate is 86/min, and respiratory rate is 14/min. Physical examination is notable for a yellow-black discoloration of the second molar on his left upper mouth. The decision is made to refer him to a dentist for further management of this cavity. The patient has never had any dental procedures and is nervous about what type of sedation will be used. Which of the following forms of anesthesia utilizes solely an oral or intravenous anti-anxiety medication?
- A. Minimal Sedation (Correct Answer)
- B. Dissociation
- C. Regional anesthesia
- D. Epidural anesthesia
- E. Deep sedation
Pain management modalities Explanation: ***Minimal Sedation***
- This involves using **oral** or **intravenous anti-anxiety medications** to help a patient relax while remaining conscious and responsive.
- The patient can still respond to verbal commands but is in a state of decreased anxiety and awareness.
*Dissociation*
- This is a state induced by certain drugs, like **ketamine**, where the patient feels detached from their body and environment.
- While it can be achieved intravenously, it is not solely an anti-anxiety medication effect and involves a different neurological state.
*Regional anesthesia*
- This involves injecting a **local anesthetic** near nerves to numb a specific part of the body, such as a limb or a jaw section for dental procedures.
- It primarily provides pain relief by blocking nerve signals and does not typically involve anti-anxiety medication as its sole component for sedation.
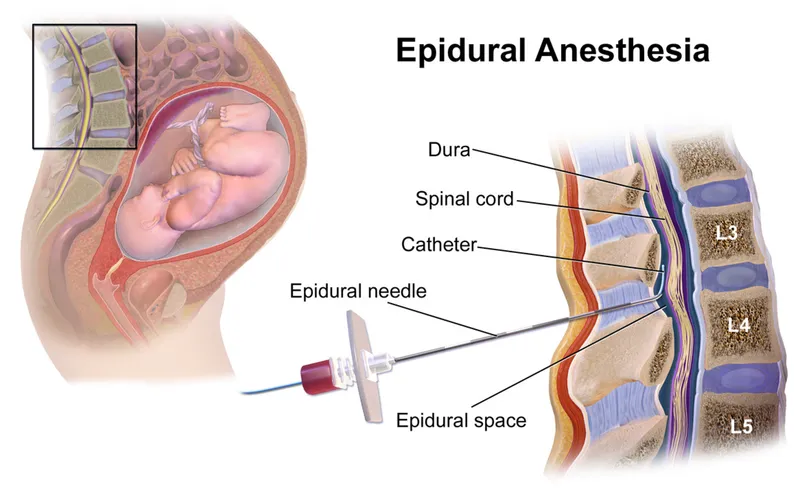
*Epidural anesthesia*
- This form of regional anesthesia involves injecting a **local anesthetic** into the **epidural space** surrounding the spinal cord to block pain signals.
- It is used for pain control during surgery or childbirth and does not involve oral or intravenous anti-anxiety medication as the primary method of sedation.
*Deep sedation*
- This involves a more profound depression of consciousness than minimal sedation, where the patient may be difficult to arouse but still responds purposefully to repeated or painful stimulation.
- While it can use intravenous medications, it typically involves a combination of sedatives and analgesics to achieve a deeper state of unresponsiveness, beyond just anti-anxiety medication.
Pain management modalities US Medical PG Question 8: A 67-year-old man comes to the clinic for establishment of care. He recently retired and moved to Florida with his wife. His past medical history includes hypertension, diabetes, chronic back pain, and hyperlipidemia. According to the patient, he takes lisinopril, metformin, atorvastatin, acetaminophen, and methadone. His previous doctor prescribed methadone for breakthrough pain as he has been having more severe pain episodes due to the recent move. He is currently out of his methadone and asks for a refill on the prescription. A physical examination is unremarkable except for mild lower extremity edema bilaterally and diffuse lower back pain upon palpation. What is the best initial step in the management of this patient?
- A. Refer the patient to a pain management clinic
- B. Inform the patient that methadone is not the best option and do not prescribe
- C. Encourage the patient to switch to duloxetine
- D. Assess the patient's pain medication history (Correct Answer)
- E. Prescribe a limited dose of methadone for breakthrough back pain
Pain management modalities Explanation: ***Assess the patient's pain medication history***
- It is crucial to gather a comprehensive **pain medication history** for a new patient on long-term opioids, especially when they are requesting a refill for a potentially high-risk medication like **methadone**. This includes understanding the duration of use, previous dosages, other medications tried, and the effectiveness of prior treatments.
- A comprehensive assessment helps to identify potential risks, such as **opioid tolerance**, dependence, or drug-drug interactions, and allows the physician to make an informed decision regarding the patient's ongoing pain management plan in accordance with **CDC guidelines** on opioid prescribing.
*Refer the patient to a pain management clinic*
- While referral to a pain management clinic may be appropriate later, the **initial step** should involve a thorough assessment by the primary care physician to understand the patient's immediate needs and history, especially given the new patient encounter.
- A direct referral without an initial evaluation could delay critical care decisions related to safe opioid prescribing and **withdrawal prevention**.
*Inform the patient that methadone is not the best option and do not prescribe*
- Simply refusing to prescribe methadone without a proper assessment and alternative plan can lead to **opioid withdrawal** and non-adherence to care, which can be dangerous for the patient.
- While methadone has significant risks, abruptly discontinuing it without a transition plan is generally discouraged, as it can cause severe **rebound pain** and withdrawal symptoms.
*Encourage the patient to switch to duloxetine*
- Duloxetine is an appropriate medication for **neuropathic pain** and **chronic musculoskeletal pain**, but it's not an immediate solution for breakthrough pain in a patient accustomed to methadone and should only be considered after a full assessment and discussion of risks and benefits.
- Switching to duloxetine without a clear understanding of the patient's current pain control, opioid dependence, and potential for withdrawal is premature and could exacerbate the patient's pain and lead to severe **withdrawal symptoms**.
*Prescribe a limited dose of methadone for breakthrough back pain*
- Prescribing methadone without a complete and thorough assessment of the patient's pain history, current dosage, and potential interactions with other medications is not safe practice, especially for a **new patient**.
- Methadone has a **long and variable half-life**, making it prone to accumulation and overdose, and requires careful titration and monitoring, which cannot be done without a full history.
Pain management modalities US Medical PG Question 9: A 72-year-old man is brought to the emergency department from hospice. The patient has been complaining of worsening pain over the past few days and states that it is no longer bearable. The patient has a past medical history of pancreatic cancer which is being managed in hospice. The patient desires no "heroic measures" to be made with regards to treatment and resuscitation. His temperature is 98.8°F (37.1°C), blood pressure is 107/68 mmHg, pulse is 102/min, respirations are 22/min, and oxygen saturation is 99% on room air. Physical exam reveals an uncomfortable elderly man who experiences severe pain upon abdominal palpation. Laboratory values reveal signs of renal failure, liver failure, and anemia. Which of the following is the best next step in management?
- A. Ketorolac and fentanyl
- B. Ketorolac
- C. Morphine (Correct Answer)
- D. No intervention warranted
- E. Morphine and fentanyl patch
Pain management modalities Explanation: ***Morphine***
- This patient is in **hospice** with **acute, unbearable pain** requiring **immediate relief** in the emergency department. **Intravenous or subcutaneous morphine** is the **best next step** as it provides **rapid onset of analgesia** (within 5-10 minutes for IV, 15-30 minutes for SC).
- In the **ED setting**, the priority is to achieve **immediate pain control** for this acute exacerbation. Once stabilized, a comprehensive long-acting regimen can be coordinated with hospice, but the question asks for the **best next step**, which is immediate-acting opioid administration.
- Morphine is appropriate despite renal failure in end-of-life care where **comfort is the primary goal**. Doses may need adjustment, but pain relief takes precedence in hospice patients.
*Ketorolac and fentanyl*
- **Ketorolac (NSAID)** is **contraindicated** in patients with **renal failure** and carries risk of **gastrointestinal bleeding**, especially concerning in advanced cancer with anemia.
- While fentanyl is appropriate for pain management, a **fentanyl patch** takes **12-24 hours** to reach therapeutic levels and is unsuitable for **acute pain** requiring immediate relief.
*Ketorolac*
- **Ketorolac (NSAID)** is contraindicated due to **renal failure** and would be insufficient for severe cancer-related pain.
- NSAIDs are generally avoided in hospice patients with multi-organ dysfunction and do not provide adequate analgesia for unbearable pain.
*Morphine and fentanyl patch*
- While this represents a comprehensive pain management approach, it is **not the best next step** in the **emergency department** for **acute pain**.
- **Fentanyl patches** have a **delayed onset** (12-24 hours to reach steady state) and are designed for **chronic, stable pain management**, not acute exacerbations.
- The immediate priority is rapid pain relief with short-acting opioids; long-acting formulations should be coordinated with hospice after acute stabilization.
*No intervention warranted*
- This is **unethical and inappropriate** given the patient's explicit complaint of unbearable pain.
- **Comfort and symptom management** are the primary objectives of hospice care, making pain relief an absolute necessity.
Pain management modalities US Medical PG Question 10: A 63-year-old man comes to the emergency department because of pain in his left groin for the past hour. The pain began soon after he returned from a walk. He describes it as 8 out of 10 in intensity and vomited once on the way to the hospital. He has had a swelling of the left groin for the past 2 months. He has chronic obstructive pulmonary disease and hypertension. Current medications include amlodipine, albuterol inhaler, and a salmeterol-fluticasone inhaler. He appears uncomfortable. His temperature is 37.4°C (99.3°F), pulse is 101/min, and blood pressure is 126/84 mm Hg. Examination shows a tender bulge on the left side above the inguinal ligament that extends into the left scrotum; lying down or applying external force does not reduce the swelling. Coughing does not make the swelling bulge further. There is no erythema. The abdomen is distended. Bowel sounds are hyperactive. Scattered rhonchi are heard throughout both lung fields. Which of the following is the most appropriate next step in management?
- A. Laparoscopic surgical repair
- B. Surgical drainage
- C. Antibiotic therapy
- D. Open surgical repair (Correct Answer)
- E. Surgical exploration of the testicle
Pain management modalities Explanation: ***Open surgical repair***
- The patient presents with a **painful, non-reducible inguinal hernia** that has likely **incarcerated** or **strangulated**, given the acute onset of severe pain, vomiting, and abdominal distension with hyperactive bowel sounds.
- In cases of suspected incarceration or strangulation, **urgent open surgical repair** is indicated to prevent **bowel ischemia** and its serious complications (e.g., perforation, sepsis).
*Laparoscopic surgical repair*
- While laparoscopic repair is an option for elective hernia repair, it is generally **contraindicated** in cases of **incarcerated or strangulated hernias** due to the higher risk of bowel injury, inadequate assessment of bowel viability, and longer operative times in an emergency setting.
- Also, the patient's **COPD** might make him a less ideal candidate for laparoscopy due to the risks associated with pneumoperitoneum.
*Surgical drainage*
- Surgical drainage is typically performed for abscesses or fluid collections, which are **not the primary issue** in this presentation.
- A hernia involves displacement of organs, not an accumulation of fluid or pus requiring drainage.
*Antibiotic therapy*
- Although antibiotics might be considered as an adjunctive therapy if infection is suspected or confirmed (e.g., with bowel necrosis), they are **not the definitive primary treatment** for an incarcerated or strangulated hernia.
- The mechanical obstruction and potential ischemia require surgical intervention for resolution.
*Surgical exploration of the testicle*
- While the bulge extends into the scrotum, the primary concern is the **incarcerated hernia** itself.
- Surgical exploration of the testicle would be indicated for conditions like testicular torsion, epididymitis, or testicular masses, which are not suggested by the presented symptoms.
More Pain management modalities US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.