Malignant hyperthermia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Malignant hyperthermia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Malignant hyperthermia US Medical PG Question 1: A 70-year-old man presents to his primary care physician for a general checkup. He states that he has been doing well and taking his medications as prescribed. He recently started a new diet and supplement to improve his health and has started exercising. The patient has a past medical history of diabetes, a myocardial infarction, and hypertension. He denies any shortness of breath at rest or with exertion. An ECG is performed and is within normal limits. Laboratory values are ordered as seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 6.7 mEq/L
HCO3-: 25 mEq/L
Glucose: 133 mg/dL
Ca2+: 10.2 mg/dL
Which of the following is the most likely cause of this patient's presentation?
- A. Medication (Correct Answer)
- B. Acute renal failure
- C. Hemolysis
- D. Dietary changes
- E. Rhabdomyolysis
Malignant hyperthermia Explanation: ***Medication***
- The patient's **hyperkalemia** (K+ 6.7 mEq/L) despite feeling well, suggests a common side effect of medications, particularly those used for his pre-existing conditions like **hypertension** (**ACE inhibitors**, **ARBs**, **spironolactone**) and **diabetes**.
- Medications are a frequent cause of asymptomatic electrolyte abnormalities, and given his complex medical history and the absence of acute symptoms, this is the most likely culprit.
*Acute renal failure*
- While acute renal failure can cause **hyperkalemia**, it typically presents with other symptoms such as **oliguria**, **fluid retention**, or other signs of organ dysfunction, which are not described.
- The patient is reported to be "doing well" without **shortness of breath** or other acute complaints, making acute renal failure less likely as the primary cause of isolated hyperkalemia.
*Hemolysis*
- **Hemolysis** can release intracellular potassium, leading to **pseudohyperkalemia**, but it would typically be suspected in cases of **blood draw errors** or conditions causing red blood cell breakdown, none of which are indicated.
- The patient's presentation does not include any signs or symptoms suggestive of red cell destruction.
*Dietary changes*
- While an extremely **high-potassium diet** or certain **supplements** could contribute to hyperkalemia, it is less common for dietary changes alone to cause such a significant elevation in a patient with normal organ function.
- Given his medical history, medication-induced hyperkalemia is a more direct and common explanation.
*Rhabdomyolysis*
- **Rhabdomyolysis** involves the breakdown of muscle tissue, releasing potassium and other intracellular contents, but it is usually associated with significant **muscle pain**, **weakness**, and elevated **creatine kinase**.
- The patient denies these symptoms and has no other indicators pointing towards severe muscle injury.
Malignant hyperthermia US Medical PG Question 2: A 59-year-old female presents to the emergency department after a fall. She reports severe pain in her right hip and an inability to move her right leg. Her past medical history is notable for osteoporosis, rheumatoid arthritis, and has never undergone surgery before. The patient was adopted, and her family history is unknown. She has never smoked and drinks alcohol socially. Her temperature is 98.8°F (37.1°C), blood pressure is 150/90 mmHg, pulse is 110/min, and respirations are 22/min. Her right leg is shortened, abducted, and externally rotated. A radiograph demonstrates a displaced femoral neck fracture. She is admitted and eventually brought to the operating room to undergo right hip arthroplasty. While undergoing induction anesthesia with inhaled sevoflurane, she develops severe muscle contractions. Her temperature is 103.4°F (39.7°C). A medication with which of the following mechanisms of action is indicated in the acute management of this patient’s condition?
- A. Ryanodine receptor antagonist (Correct Answer)
- B. Acetylcholine receptor agonist
- C. Serotonin 1B/1D agonist
- D. NMDA receptor antagonist
- E. GABA agonist
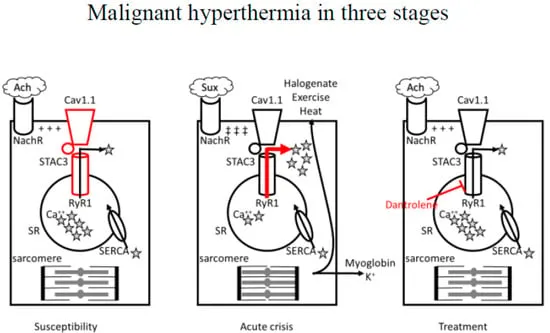
Malignant hyperthermia Explanation: ***Ryanodine receptor antagonist***
- The patient's presentation with **high fever**, **muscle rigidity**, and **tachycardia** shortly after induction with **sevoflurane** is highly suggestive of **malignant hyperthermia (MH)**.
- **Dantrolene**, a **ryanodine receptor antagonist**, is the specific treatment for MH, as it blocks the excessive release of **calcium** from the sarcoplasmic reticulum in muscle cells.
*Acetylcholine receptor agonist*
- **Acetylcholine receptor agonists** (e.g., succinylcholine) stimulate muscle contraction and would worsen the muscle rigidity seen in malignant hyperthermia.
- These agents are often triggers for malignant hyperthermia when combined with volatile anesthetics.
*Serotonin 1B/1D agonist*
- **Serotonin 1B/1D agonists** (e.g., triptans) are primarily used in the acute treatment of migraines.
- They have no role in the management of malignant hyperthermia and would not address the underlying pathophysiology.
*NMDA receptor antagonist*
- **NMDA receptor antagonists** (e.g., ketamine) are dissociative anesthetics and analgesics.
- They do not directly affect the calcium release channels in skeletal muscle responsible for malignant hyperthermia.
*GABA agonist*
- **GABA agonists** (e.g., benzodiazepines, propofol) are central nervous system depressants used for sedation and anesthesia.
- While they can have muscle relaxant properties, they do not specifically target the **ryanodine receptor** pathway involved in malignant hyperthermia.
Malignant hyperthermia US Medical PG Question 3: A 32-year-old man is brought to the emergency department after he was found unresponsive on the street. Upon admission, he is lethargic and cyanotic with small, symmetrical pinpoint pupils. The following vital signs were registered: blood pressure of 100/60 mm Hg, heart rate of 70/min, respiratory rate of 8/min, and a body temperature of 36.0°C (96.8°F). While being assessed and resuscitated, a sample for arterial blood gas (ABG) analysis was taken, in addition to the following biochemistry tests:
Laboratory test
Serum Na+ 138 mEq/L
Serum Cl- 101 mEq/L
Serum K+ 4.0 mEq/L
Serum creatinine (SCr) 0.58 mg/dL
Which of the following values would you most likely expect to see in this patient’s ABG results?
- A. pH: decreased, HCO3- : increased, Pco2: increased (Correct Answer)
- B. pH: increased, HCO3- : decreased, Pco2: decreased
- C. pH: decreased, HCO3- : decreased, Pco2: decreased
- D. pH: increased, HCO3- : increased, Pco2: increased
- E. pH: normal, HCO3- : increased, Pco2: increased
Malignant hyperthermia Explanation: ***pH: decreased, HCO3- : increased, Pco2: increased***
- The patient's **depressed respiratory rate** (8/min) indicates severe hypoventilation, leading to **CO2 retention** and subsequent **respiratory acidosis** (decreased pH, increased PaCO2).
- In **acute respiratory acidosis**, the body initiates immediate buffering, causing a **mild increase in HCO3-** (approximately 1 mEq/L per 10 mmHg rise in PaCO2). Over 3-5 days, renal compensation leads to more significant HCO3- retention, but in this acute presentation, some HCO3- elevation is expected from acute buffering mechanisms.
- The **decreased pH** indicates that compensation is incomplete, which is typical in the acute setting.
*pH: increased, HCO3- : decreased, Pco2: decreased*
- This pattern is characteristic of **respiratory alkalosis** (increased pH, decreased PaCO2) with metabolic compensation (decreased HCO3-), which would occur in hyperventilation, opposite to the patient's presentation.
- The patient's **slow respiratory rate** of 8/min directly contradicts the finding of decreased PaCO2.
*pH: decreased, HCO3- : decreased, Pco2: decreased*
- This suggests a **metabolic acidosis** (decreased pH, decreased HCO3-) with respiratory compensation (decreased PaCO2), typically seen in conditions like DKA or lactic acidosis.
- Although the pH is decreased, the patient's severe bradypnea (RR 8/min) indicates increased CO2 retention, not decreased CO2.
*pH: increased, HCO3- : increased, Pco2: increased*
- This combination of findings is indicative of **metabolic alkalosis** (increased pH, increased HCO3-) with respiratory compensation (increased PaCO2).
- This is inconsistent with the patient's pinpoint pupils, cyanosis, and **severe bradypnea**, which are classic signs of opioid overdose causing respiratory depression and acidosis, not alkalosis.
*pH: normal, HCO3- : increased, Pco2: increased*
- A normal pH despite increased HCO3- and PaCO2 indicates **fully compensated respiratory acidosis**, which requires days of renal compensation to develop.
- In this **acute, severe drug overdose** with profound respiratory depression, the body would not have sufficient time to achieve full compensation, thus the pH would remain low.
Malignant hyperthermia US Medical PG Question 4: Two-hours into recovery from general anesthesia for an orthopedic fracture, a 34-year-old woman develops fever and masseter muscle rigidity with lockjaw. She has no history of a similar episode. She has no history of serious illness and takes no medications. She appears confused. In the recovery room, her blood pressure is 78/50 mm Hg, the pulse is 128/min, the respirations are 42/min, and the temperature is 40.3°C (104.5°F). Cardiopulmonary examination shows no abnormalities. Laboratory studies show:
Serum
Na+ 145 mEq/L
K+ 6.5 mEq/L
Arterial blood gas on room air
pH 7.01
PCO2 78 mm Hg
HCO3− 14 mEq/L
PO2 55 mm Hg
The patient is reintubated. Which of the following is the most appropriate next step in pharmacotherapy?
- A. Lorazepam
- B. Diphenhydramine
- C. Dantrolene (Correct Answer)
- D. Labetalol
- E. Cyproheptadine
Malignant hyperthermia Explanation: ***Dantrolene***
- The patient exhibits classic signs of **malignant hyperthermia**, including
**masseter muscle rigidity**, **fever (40.3°C)**, **tachycardia (128/min)**,
**tachypnea (42/min)**, and **hypotension (78/50 mm Hg)**. The **elevated potassium (6.5
mEq/L)**, **acidosis (pH 7.01)**, and **hypercapnia (PCO2 78 mm Hg)**
further support this diagnosis.
- **Dantrolene** is the only specific antidote for malignant hyperthermia as
it acts as a **ryanodine receptor antagonist**, inhibiting calcium release
from the sarcoplasmic reticulum and thereby reducing muscle contracture and
heat production.
*Lorazepam*
- **Lorazepam** is a benzodiazepine used for treating seizures, anxiety, and
agitation, but it does **not address the underlying pathophysiology of
malignant hyperthermia**.
- While the patient appears confused, this is likely secondary to the
metabolic derangements and hyperthermia, not a primary indication for
lorazepam.
*Diphenhydramine*
- **Diphenhydramine** is an antihistamine used to treat allergic reactions or
sedation; it has no role in the management of malignant hyperthermia.
- It would not alleviate the muscle rigidity, hyperthermia, or metabolic
abnormalities seen in this patient.
*Labetalol*
- **Labetalol** is a beta-blocker used to manage hypertension and tachycardia,
but these are symptoms of malignant hyperthermia rather than the root
cause.
- While it could temporarily lower heart rate and blood pressure, it **does
not address the excessive calcium release** in skeletal muscle, which is
the hallmark of malignant hyperthermia.
*Cyproheptadine*
- **Cyproheptadine** is a serotonin antagonist used in the treatment of
serotonin syndrome.
- Malignant hyperthermia and serotonin syndrome share some clinical features
like hyperthermia, but the **trigger (anesthetic agents)** and underlying
mechanisms are different, making cyproheptadine ineffective here.
Malignant hyperthermia US Medical PG Question 5: A 35-year-old male patient is brought into the emergency department by emergency medical services. The patient has a history of schizophrenia and is on medication per his mother. His mother also states that the dose of his medication was recently increased, though she is not sure of the specific medication he takes. His vitals are HR 110, BP 170/100, T 102.5, RR 22. On exam, he cannot respond to questions and has rigidity. His head is turned to the right and remains in that position during the exam. Labs are significant for a WBC count of 14,000 cells/mcL, with a creatine kinase (CK) level of 3,000 mcg/L. What is the best treatment for this patient?
- A. Valproate
- B. Morphine
- C. Dantrolene (Correct Answer)
- D. Diazepam
- E. Lamotrigine
Malignant hyperthermia Explanation: ***Dantrolene***
- This patient presents with symptoms highly suggestive of **neuroleptic malignant syndrome (NMS)**, including a history of schizophrenia, recent medication increase, fever, rigidity, autonomic instability (tachycardia, hypertension), elevated WBC, and elevated CK.
- **Dantrolene** is a **direct-acting skeletal muscle relaxant** that reduces muscle rigidity and hyperthermia by inhibiting calcium release from the sarcoplasmic reticulum.
- In **severe NMS** with marked hyperthermia (T 102.5°F), significant muscle rigidity, and elevated CK (indicating rhabdomyolysis risk), Dantrolene is the most appropriate pharmacologic intervention to directly address the life-threatening muscle rigidity and prevent further complications.
*Valproate*
- **Valproate** is an **anticonvulsant** and **mood stabilizer** used for seizures, bipolar disorder, and migraine prevention.
- It does not directly address the pathophysiology of NMS, which involves central dopamine receptor blockade and muscle rigidity.
*Morphine*
- **Morphine** is an **opioid analgesic** primarily used for pain management.
- It would not alleviate the underlying muscle rigidity, hyperthermia, or autonomic dysfunction associated with NMS and could potentially worsen respiratory depression.
*Diazepam*
- **Diazepam** is a **benzodiazepine** used for anxiety, seizures, and muscle spasms, and can be helpful for agitation or mild rigidity.
- While it might provide some symptomatic relief and is used as adjunctive therapy in NMS, it is not the primary treatment for **severe NMS** with this degree of hyperthermia, marked rigidity, and elevated CK, and does not directly address the underlying muscle damage and rhabdomyolysis risk as effectively as Dantrolene.
*Lamotrigine*
- **Lamotrigine** is an **anticonvulsant** used for seizures and bipolar disorder, known for its risk of severe skin reactions.
- It has no role in the treatment of NMS and would not impact the patient's severe symptoms.
Malignant hyperthermia US Medical PG Question 6: A 33-year-old man presents to the emergency department acutely confused. The patient was found down at a local construction site by his coworkers. The patient has a past medical history of a seizure disorder and schizophrenia and is currently taking haloperidol. He had recent surgery 2 months ago to remove an inflamed appendix. His temperature is 105°F (40.6°C), blood pressure is 120/84 mmHg, pulse is 150/min, respirations are 19/min, and oxygen saturation is 99% on room air. Physical exam is notable for a confused man who cannot answer questions. His clothes are drenched in sweat. He is not making purposeful movements with his extremities although no focal neurological deficits are clearly apparent. Which of the following is the most likely diagnosis?
- A. Heat exhaustion
- B. Nonexertional heat stroke
- C. Neuroleptic malignant syndrome
- D. Malignant hyperthermia
- E. Exertional heat stroke (Correct Answer)
Malignant hyperthermia Explanation: ***Exertional heat stroke***
- This diagnosis is supported by the patient's presentation of **hyperthermia** (105°F), **tachycardia**, **confusion**, and a history of working at a **construction site** (suggesting physical exertion in a hot environment).
- The patient's **drenched clothes from sweat** indicate the body's initial attempt to cool down, but the extremely high core temperature and confusion signify a failure of thermoregulation.
*Heat exhaustion*
- While heat exhaustion also involves **sweating** and can present with elevated body temperature, the core temperature is typically **below 104°F (40°C)**, and **marked altered mental status** (like severe confusion) is less common or less severe.
- The patient's temperature of 105°F (40.6°C) and profound confusion are more indicative of heat stroke.
*Nonexertional heat stroke*
- Nonexertional (or classic) heat stroke usually affects populations with **compromised thermoregulation** (e.g., elderly, very young, chronically ill) who are exposed to high environmental temperatures **without significant physical exertion**.
- The patient's age (33) and history of working at a construction site make exertional heat stroke more likely than nonexertional.
*Neuroleptic malignant syndrome*
- NMS is characterized by **fever, muscle rigidity** (often "lead pipe" rigidity), **altered mental status**, and **autonomic instability** (including tachycardia and diaphoresis), and is associated with **antipsychotic medications** like haloperidol.
- However, NMS typically develops **gradually over days to weeks**, not acutely. The key differentiator here is the **clear environmental and exertional context** (construction site work), **acute onset** after being found down, and the **absence of characteristic muscle rigidity** that would be prominent in NMS.
- Heat stroke is more probable given the immediate occupational exposure and clinical timeline.
*Malignant hyperthermia*
- Malignant hyperthermia is a rare, life-threatening condition associated with exposure to certain **anesthetic agents** (e.g., succinylcholine, volatile anesthetics) or, less commonly, severe exertion in susceptible individuals.
- The patient's recent surgery was two months prior, and there is no mention of current exposure to triggers, making it unlikely to be the immediate cause of his acute presentation.
Malignant hyperthermia US Medical PG Question 7: A 55-year-old man with chronic pain on high-dose opioids (120 mg oral morphine equivalents daily) requires major spine surgery. Intraoperatively, he requires escalating doses of fentanyl with poor pain control. Postoperatively, his pain remains severe (10/10) despite maximum conventional multimodal analgesia including IV hydromorphone PCA, acetaminophen, and ketorolac. He becomes increasingly agitated and tachycardic. Evaluate the most comprehensive pain management strategy addressing the underlying pathophysiology.
- A. Increase PCA opioid dose to match home requirements plus surgical pain needs
- B. Transition to methadone for better mu-receptor coverage
- C. Ketamine infusion to address opioid-induced hyperalgesia and NMDA receptor sensitization (Correct Answer)
- D. Epidural analgesia with local anesthetic and low-dose opioid
- E. Regional nerve blocks with liposomal bupivacaine
Malignant hyperthermia Explanation: ***Ketamine infusion to address opioid-induced hyperalgesia and NMDA receptor sensitization***
- The patient exhibits **opioid-induced hyperalgesia (OIH)**, where high-dose opioids paradoxically increase pain sensitivity through **NMDA receptor** activation and central sensitization.
- **Ketamine** is an NMDA receptor antagonist that directly targets the underlying pathophysiology to reverse **central sensitization** and reduce the "wind-up" phenomenon.
*Increase PCA opioid dose to match home requirements plus surgical pain needs*
- Simply increasing the opioid dose in a patient with **OIH** can exacerbate the pain sensitization rather than alleviate it.
- This strategy fails to address the down-regulation of **mu-receptors** and the neuroplastic changes associated with chronic high-dose opioid use.
*Transition to methadone for better mu-receptor coverage*
- While **methadone** has NMDA antagonist properties, a rapid transition in the acute postoperative setting is pharmacokinetically complex and lacks the immediate efficacy of a **low-dose ketamine infusion**.
- Methadone titration is challenging due to its long **half-life** and risk of delayed respiratory depression in an agitated, acutely painful patient.
*Epidural analgesia with local anesthetic and low-dose opioid*
- While neuraxial techniques are normally effective, **major spine surgery** often complicates or precludes the placement of an epidural due to surgical site constraints or dural integrity.
- This approach may provide regional relief but does not systemically address the **centralized hyperalgesia** caused by chronic high-dose opioid therapy.
*Regional nerve blocks with liposomal bupivacaine*
- **Regional blocks** for extensive spine surgery may provide inadequate coverage for the broad dermatomal distribution involved in major spinal procedures.
- These blocks target **peripheral nerves** and do not address the **NMDA-mediated sensitization** in the central nervous system that is driving this patient's severe pain.
Malignant hyperthermia US Medical PG Question 8: A 70-year-old man with severe aortic stenosis (valve area 0.6 cm², mean gradient 55 mmHg) develops acute cholecystitis requiring surgery. He is symptomatic with exertional angina and dyspnea. Cardiology recommends TAVR before surgery, but the patient has signs of gallbladder perforation. The surgical team debates timing of interventions. Evaluate the optimal management strategy weighing cardiac and surgical risks.
- A. Emergency cholecystectomy under general anesthesia with careful hemodynamic monitoring
- B. Medical management of cholecystitis with antibiotics, TAVR in 6 weeks, then cholecystectomy
- C. Percutaneous cholecystostomy tube followed by TAVR, then delayed cholecystectomy (Correct Answer)
- D. Combined TAVR and cholecystectomy in one procedure
- E. Open cholecystectomy under epidural anesthesia to avoid general anesthesia risks
Malignant hyperthermia Explanation: ***Percutaneous cholecystostomy tube followed by TAVR, then delayed cholecystectomy***
- Severe, symptomatic **aortic stenosis (AS)** represents an extremely high perioperative risk for major non-cardiac surgery; a **percutaneous cholecystostomy** provides rapid source control for the gallbladder under local anesthesia without the hemodynamic stress of general anesthesia.
- This staged approach stabilizes the surgical emergency first, allowing for **Transcatheter Aortic Valve Replacement (TAVR)** to be performed under safer conditions before the patient undergoes a definitive cholecystectomy.
*Emergency cholecystectomy under general anesthesia with careful hemodynamic monitoring*
- The perioperative mortality risk for patients with **symptomatic severe AS** undergoing non-cardiac surgery is unacceptably high due to the inability to increase **cardiac output** in response to surgical stress.
- Induction of general anesthesia and **positive pressure ventilation** can lead to sudden, fatal drops in systemic vascular resistance and preload that the stenotic valve cannot accommodate.
*Medical management of cholecystitis with antibiotics, TAVR in 6 weeks, then cholecystectomy*
- Signs of **gallbladder perforation** constitute a surgical emergency that cannot be managed with antibiotics alone as it will likely lead to **septic shock**.
- Delaying definitive treatment for the gallbladder for 6 weeks in the presence of a perforation would likely result in patient death before cardiac optimization could occur.
*Combined TAVR and cholecystectomy in one procedure*
- Performing a **combined procedure** unnecessarily prolongs anesthesia time and increases the risk of complications such as **bleeding** from the anticoagulation required for TAVR.
- The inflammatory state from the acute cholecystitis and potential sepsis would significantly increase the risk of **TAVR complications**, including valve thrombosis or migration.
*Open cholecystectomy under epidural anesthesia to avoid general anesthesia risks*
- **Neuraxial anesthesia** (spinal or epidural) is generally **contraindicated** in severe aortic stenosis because it can cause rapid sympatholysis and severe **hypotension**.
- An open surgical approach is more invasive and causes more physiological stress than a percutaneous drain, which is the safer initial strategy for an unstable cardiac patient.
Malignant hyperthermia US Medical PG Question 9: A 42-year-old woman with a history of multiple anesthetic complications presents for elective surgery. Previous records indicate awareness during general anesthesia twice, prolonged paralysis after succinylcholine requiring 6 hours of ventilation, and a sibling with fatal anesthetic complication involving hyperthermia and rhabdomyolysis. Evaluate the comprehensive anesthetic plan that addresses all potential complications.
- A. Genetic testing before proceeding with any anesthetic
- B. Total intravenous anesthesia with propofol and remifentanil, avoid succinylcholine and volatile agents, use rocuronium with sugammadex reversal (Correct Answer)
- C. Standard general anesthesia with dantrolene prophylaxis
- D. Volatile anesthetic with BIS monitoring, avoid all muscle relaxants
- E. Regional anesthesia only without any general anesthetic agents
Malignant hyperthermia Explanation: ***Total intravenous anesthesia with propofol and remifentanil, avoid succinylcholine and volatile agents, use rocuronium with sugammadex reversal***
- **Total intravenous anesthesia (TIVA)** using propofol and remifentanil avoids **volatile anesthetics** and **succinylcholine**, which are mandatory triggers for **malignant hyperthermia (MH)** mentioned in the family history.
- Avoiding **succinylcholine** prevents prolonged paralysis due to suspected **pseudocholinesterase deficiency**, while **rocuronium** with **sugammadex** provides safe neuromuscular blockade and reliable reversal.
*Genetic testing before proceeding with any anesthetic*
- While **genetic testing** for **RYR1** or **BCHE** mutations is helpful, it is not a comprehensive "anesthetic plan" and would delay necessary elective surgery.
- Negative genetic results do not fully rule out **malignant hyperthermia** susceptibility; clinical precautions must be taken regardless.
*Standard general anesthesia with dantrolene prophylaxis*
- **Dantrolene prophylaxis** is no longer recommended; the standard of care is the strict avoidance of triggering agents like **isoflurane** or **sevoflurane**.
- Using standard anesthesia would involve **volatile agents**, which are contraindicated due to the high risk of **malignant hyperthermia** suggested by the sibling's death.
*Volatile anesthetic with BIS monitoring, avoid all muscle relaxants*
- **Volatile anesthetics** are absolute contraindications in patients at risk for **malignant hyperthermia**, regardless of monitoring techniques used.
- Avoiding all muscle relaxants may lead to poor surgical conditions, whereas **non-depolarizing agents** like **rocuronium** are safe in these patients.
*Regional anesthesia only without any general anesthetic agents*
- While **regional anesthesia** is a safe alternative, it may be insufficient depending on the surgical site or complexity of the procedure.
- A history of **anesthesia awareness** indicates a need for a controlled general anesthetic plan if surgery is not amenable to a simple block.
Malignant hyperthermia US Medical PG Question 10: A 65-year-old man develops postoperative delirium on day 2 after open AAA repair. He is agitated, pulling at his lines, and has waxing-waning confusion. His vital signs are stable, and laboratory values including sodium, glucose, and calcium are normal. He received 4 mg of morphine IV 2 hours ago for pain. Analyze the most appropriate pharmacologic intervention.
- A. Propofol infusion for sedation
- B. Haloperidol 0.5-1 mg IV or IM (Correct Answer)
- C. Increase morphine dose for better pain control
- D. Lorazepam 2 mg IV for sedation
- E. Diphenhydramine 25 mg IV for sleep
Malignant hyperthermia Explanation: ***Haloperidol 0.5-1 mg IV or IM***
- Low-dose **haloperidol** is the first-line pharmacologic agent for managing severe **postoperative delirium** when non-pharmacological measures fail or the patient is a danger to themselves.
- It has a safe profile in the elderly for brief use and does not cause significant **respiratory depression** unlike sedatives.
*Propofol infusion for sedation*
- **Propofol** is reserved for patients who are **intubated** in an ICU setting and is not appropriate for a patient on the general surgical floor.
- It can cause profound **hypotension** and requires continuous hemodynamic monitoring which is not indicated for this stable patient.
*Increase morphine dose for better pain control*
- **Opioids** are common triggers for delirium; increasing the dose of morphine would likely **worsen the confusion** rather than resolve it.
- While pain must be managed, alternative strategies like **regional anesthesia** or non-opioid medications should be prioritized in a delirious patient.
*Lorazepam 2 mg IV for sedation*
- **Benzodiazepines** are generally contraindicated in delirium because they often cause **paradoxical agitation** and worsen cognitive impairment.
- They should only be used as a first-line agent when delirium is caused by **alcohol withdrawal** or benzodiazepine withdrawal.
*Diphenhydramine 25 mg IV for sleep*
- **Diphenhydramine** has significant **anticholinergic** properties, which are strongly associated with the development and prolongation of **delirium**.
- Using this for sleep in an elderly postoperative patient increases the risk of **falls and further disorientation**.
More Malignant hyperthermia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.