Local anesthesia and nerve blocks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Local anesthesia and nerve blocks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Local anesthesia and nerve blocks US Medical PG Question 1: A 17-year-old male presents with altered mental status. He was recently admitted to the hospital due to a tibial fracture suffered while playing soccer. His nurse states that he is difficult to arouse. His temperature is 98.6 deg F (37 deg C), blood pressure is 130/80 mm Hg, pulse is 60/min, and respirations are 6/min. Exam is notable for pinpoint pupils and significant lethargy. Which of the following describes the mechanism of action of the drug likely causing this patient's altered mental status?
- A. Neuronal hyperpolarization due to sodium influx
- B. Neuronal depolarization due to sodium efflux
- C. Neuronal depolarization due to potassium influx
- D. Neuronal hyperpolarization due to potassium efflux (Correct Answer)
- E. Neuronal hyperpolarization due to chloride influx
Local anesthesia and nerve blocks Explanation: ***Neuronal hyperpolarization due to potassium efflux***
- The patient's symptoms of **altered mental status**, **pinpoint pupils**, and **respiratory depression** are classic for **opioid overdose**.
- Opioids act by binding to opioid receptors (mu, delta, kappa), which are **G-protein coupled receptors**. Activation of these receptors leads to **potassium efflux** and **calcium influx inhibition**, causing neuronal hyperpolarization and reduced neuronal excitability.
*Neuronal hyperpolarization due to sodium influx*
- **Sodium influx** typically causes depolarization, not hyperpolarization, making this option inconsistent with the mechanism of inducing neuronal inhibition.
- Hyperpolarization usually involves outward positive current (like potassium efflux) or inward negative current (like chloride influx).
*Neuronal depolarization due to sodium efflux*
- **Sodium efflux** (e.g., via the Na+/K+-ATPase) is crucial for maintaining resting membrane potential, but it does not directly lead to depolarization as described here.
- Depolarization is commonly associated with **sodium influx**, not efflux, causing the membrane potential to become more positive.
*Neuronal depolarization due to potassium influx*
- **Potassium influx** would make the cell less negative inside (depolarization), but this is not the primary mechanism of action for opioids.
- Opioids primarily cause **hyperpolarization** and reduced excitability, making this mechanism incorrect for the observed clinical picture caused by opioid overdose.
*Neuronal hyperpolarization due to chloride influx*
- While **chloride influx** does cause neuronal hyperpolarization (e.g., via GABA-A receptor activation by benzodiazepines), this is the mechanism for **GABAergic drugs**, not opioids.
- Opioids primarily achieve hyperpolarization through **potassium efflux**.
Local anesthesia and nerve blocks US Medical PG Question 2: A 75 year-old gentleman presents to his general practitioner. He is currently being treated for hypertension and is on a multi-drug regimen. His current blood pressure is 180/100. The physician would like to begin treatment with minoxidil or hydralazine. Which of the following side effects is associated with administration of these drugs?
- A. Persistent cough
- B. Cyanosis in extremities
- C. Fetal renal toxicity
- D. Systemic volume loss
- E. Reflex tachycardia (Correct Answer)
Local anesthesia and nerve blocks Explanation: ***Reflex tachycardia***
- Both **minoxidil** and **hydralazine** are direct arterial vasodilators, causing a significant drop in **peripheral vascular resistance**.
- This vasodilation triggers a **baroreflex response**, leading to an increase in heart rate and **cardiac contractility** to maintain cardiac output, resulting in reflex tachycardia.
*Persistent cough*
- **Persistent cough** is a common side effect associated with **ACE inhibitors**, such as lisinopril or enalapril, due to the accumulation of **bradykinin**.
- This side effect is not typically seen with **minoxidil** or **hydralazine**, which act directly on vascular smooth muscle to cause vasodilation.
*Cyanosis in extremities*
- **Cyanosis** (bluish discoloration of the skin and mucous membranes) usually indicates **hypoxemia** or poor peripheral perfusion.
- While sometimes associated with severe cardiogenic shock or specific drug toxicities like methemoglobinemia (not related to minoxidil or hydralazine), it is not a direct or typical side effect of these vasodilators.
*Fetal renal toxicity*
- **Fetal renal toxicity**, including **fetal renal dysfunction** and **oligohydramnios**, is a well-known risk associated with **ACE inhibitors** and **ARBs** during pregnancy.
- Neither **minoxidil** nor **hydralazine** are primarily linked to this specific fetal adverse effect, though hydralazine can be used in pregnancy for severe hypertension.
*Systemic volume loss*
- **Systemic volume loss** is usually caused by conditions like **dehydration**, excessive diuresis, or hemorrhage.
- While vasodilators can reduce blood pressure, they do not directly cause **systemic volume depletion**; rather, the reflex response to vasodilation can include fluid retention to counteract the blood pressure drop.
Local anesthesia and nerve blocks US Medical PG Question 3: A 47-year-old man with alcoholic cirrhosis is brought to the emergency department by ambulance 20 minutes after being involved in a high-speed motor vehicle collision. His pulse is 120/min, respirations are 28/min and labored, and blood pressure is 70/40 mm Hg. Physical examination shows ecchymoses over the trunk and abdomen. In preparation for an exploratory laparotomy, atracurium is administered as an anesthetic. Which of the following characteristics is the most likely reason that this drug was chosen over other drugs in the same class?
- A. Quickest onset of action
- B. Highest potency
- C. Prolonged depolarization
- D. Organ-independent elimination (Correct Answer)
- E. Low risk of bleeding
Local anesthesia and nerve blocks Explanation: ***Organ-independent elimination***
- **Atracurium** is metabolized by **Hofmann elimination** and **ester hydrolysis**, which are independent of renal or hepatic function.
- This is crucial for a patient with **alcoholic cirrhosis** and **hemodynamic instability**, where liver and kidney function may be compromised, preventing drug accumulation.
*Quickest onset of action*
- While a rapid onset is desirable in an emergency, atracurium does not have the **quickest onset of action** among neuromuscular blockers; **succinylcholine** is faster.
- The primary selection criterion here relates to the patient's underlying liver pathology and the drug's elimination profile.
*Highest potency*
- **Potency** refers to the dose required to produce a given effect, and while important, it is not the **most critical factor** in selecting atracurium for this patient.
- The patient's severe medical condition necessitates drug selection based on **metabolic profile** to minimize adverse effects.
*Prolonged depolarization*
- Atracurium is a **non-depolarizing neuromuscular blocker**, meaning it does not cause prolonged depolarization.
- **Succinylcholine** is a depolarizing agent, and its use might be contraindicated or require careful consideration in trauma patients with potential electrolyte imbalances.
*Low risk of bleeding*
- The risk of bleeding is generally not a direct characteristic of **neuromuscular blocking agents** themselves.
- The patient's **cirrhosis** and **trauma** are the primary factors contributing to a high risk of bleeding, which is managed independently of muscle relaxant choice.
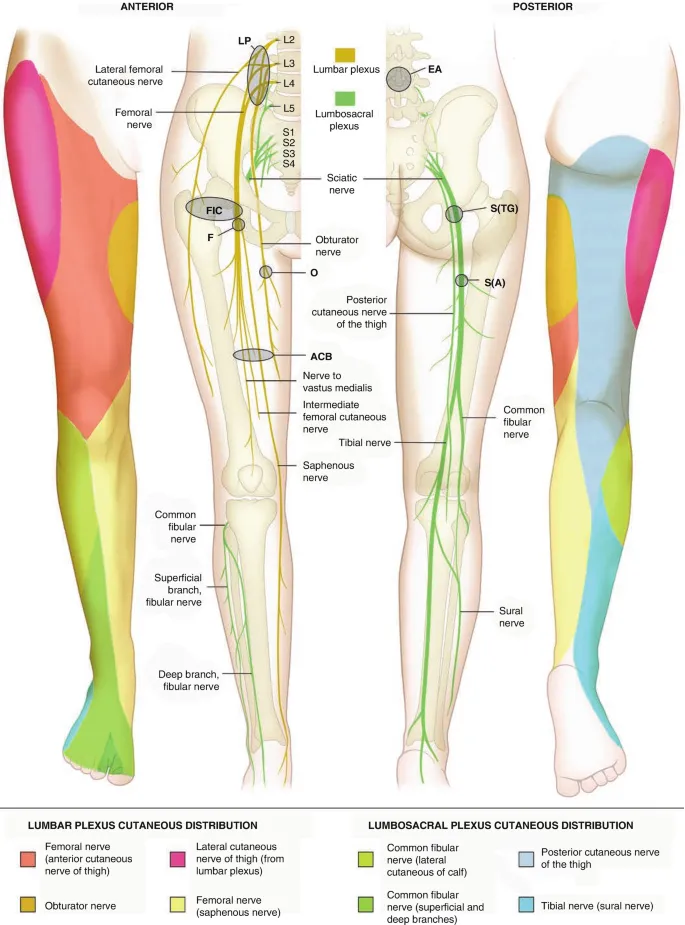
Local anesthesia and nerve blocks US Medical PG Question 4: A 31-year-old woman with multiple sclerosis comes to the physician because of a 4-day history of cramps in her left leg. Physical examination shows flexion of the left hip and increased tone in the thigh muscles. A local anesthetic block of which of the following nerves would most likely improve this patient's condition the most?
- A. Inferior gluteal nerve
- B. Superior gluteal nerve
- C. Femoral nerve (Correct Answer)
- D. Sciatic nerve
- E. Obturator nerve
Local anesthesia and nerve blocks Explanation: ***Femoral nerve***
- The **femoral nerve** innervates the **iliacus** (a primary hip flexor) and the **rectus femoris** (part of the quadriceps that assists in hip flexion), as well as the entire **quadriceps femoris group** (responsible for knee extension and contributing to increased thigh muscle tone).
- In this patient with spasticity, **hip flexion** is caused by hypertonicity of iliopsoas and rectus femoris, while **increased tone in thigh muscles** reflects quadriceps involvement.
- Blocking the femoral nerve would relax these muscles, thereby improving the **cramps, hip flexion, and increased thigh tone**.
*Inferior gluteal nerve*
- The **inferior gluteal nerve** primarily innervates the **gluteus maximus muscle**, which is involved in hip extension and external rotation, not hip flexion.
- Blocking this nerve would not directly address the symptoms of increased thigh muscle tone and hip flexion.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius, gluteus minimus**, and **tensor fasciae latae muscles**, which are involved in hip abduction and internal rotation.
- Its blockade would not relieve hip flexion or thigh muscle cramps.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (hip extension, knee flexion) and all muscles below the knee.
- While it affects leg muscles, it does not directly control the muscles causing **hip flexion and increased thigh tone** in this context.
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh (adductor longus, brevis, magnus, gracilis), leading to hip adduction.
- Blocking this nerve would not address hip flexion or the increased tone in the quadriceps muscles described.
Local anesthesia and nerve blocks US Medical PG Question 5: A 5-year-old boy undergoes MRI neuroimaging for the evaluation of worsening headaches and intermittent nausea upon awakening. He receives a bolus of intravenous thiopental for sedation during the procedure. Ten minutes after the MRI, the patient is awake and responsive. Which of the following pharmacological properties is most likely responsible for this patient's rapid recovery from this anesthetic agent?
- A. First-pass metabolism
- B. Redistribution (Correct Answer)
- C. Zero-order elimination
- D. Ion trapping
- E. Cytochrome P450 oxidation
Local anesthesia and nerve blocks Explanation: ***Redistribution***
- Thiopental is a highly **lipid-soluble** drug that rapidly crosses the **blood-brain barrier**, leading to quick onset of action.
- The drug then rapidly **redistributes** from the brain to other highly perfused tissues (e.g., muscle, fat) and then less perfused tissues, causing a rapid decrease in drug concentration at the site of action and thus termination of the anesthetic effect.
*First-pass metabolism*
- This refers to the **metabolism of a drug** before it reaches systemic circulation, typically after oral administration, and does not explain the termination of action for an intravenously administered drug like thiopental.
- While thiopental is ultimately metabolized by the liver, this process is slower than redistribution and does not account for the **rapid awakening**.
*Zero-order elimination*
- **Zero-order elimination** occurs when a constant amount of drug is eliminated per unit of time, regardless of the drug's concentration, often seen with drug saturation of elimination pathways.
- Thiopental elimination follows **first-order kinetics** at therapeutic doses, meaning a constant fraction of the drug is eliminated per unit time, and this describes slower, overall elimination, not rapid recovery.
*Ion trapping*
- **Ion trapping** occurs when a drug accumulates in a compartment due to differences in pH across a membrane and the drug's pKa, leading to ionization and reduced ability to diffuse back.
- This mechanism is important for drug excretion or distribution into specific compartments (e.g., accumulation of basic drugs in acidic urine) but does not explain the **rapid termination of CNS effects** via redistribution.
*Cytochrome P450 oxidation*
- **Cytochrome P450 (CYP450) oxidation** is a major pathway for drug metabolism in the liver, which is responsible for the eventual elimination of thiopental from the body.
- While important for overall drug clearance, the rate of CYP450 oxidation is too slow to account for the **rapid awakening** seen after a single bolus dose of thiopental; redistribution is the primary factor for rapid recovery.
Local anesthesia and nerve blocks US Medical PG Question 6: A 36-year-old male with fluctuating levels of consciousness is brought to the emergency department by ambulance due to a fire in his home. He currently opens his eyes to voice, localizes painful stimuli, responds when asked questions, but is disoriented and cannot obey commands. The patient’s temperature is 99°F (37.2°C), blood pressure is 86/52 mmHg, pulse is 88/min, and respirations are 14/min with an oxygen saturation of 97% O2 on room air. Physical exam shows evidence of soot around the patient’s nose and mouth, but no burns, airway obstruction, nor accessory muscle use. A blood lactate is 14 mmol/L. The patient is started on intravenous fluids.
What is the next best step in management?
- A. Methylene blue
- B. Hyperbaric oxygen
- C. Sodium thiosulfate and sodium nitrite
- D. Intravenous epinephrine
- E. 100% oxygen, hydroxycobalamin, and sodium thiosulfate (Correct Answer)
Local anesthesia and nerve blocks Explanation: ***100% oxygen, hydroxycobalamin, and sodium thiosulfate***
- This patient presents with signs of both **carbon monoxide poisoning** (fire exposure, disoriented, altered mental status) and **cyanide poisoning** (fire exposure, very high lactate, normal oxygen saturation despite altered mental status). This combination therapy directly addresses both.
- **100% oxygen** competes with carbon monoxide for hemoglobin binding and helps clear it, while **hydroxycobalamin** and **sodium thiosulfate** are antidotes for cyanide poisoning, converting cyanide into less toxic compounds.
*Methylene blue*
- **Methylene blue** is used to treat **methemoglobinemia**, a condition where iron in hemoglobin is oxidized, leading to impaired oxygen transport.
- The patient's symptoms (fire exposure, altered mental status, and a high lactate with normal SpO2) are not characteristic of methemoglobinemia, but rather strong indicators of carbon monoxide and cyanide poisoning.
*Hyperbaric oxygen*
- **Hyperbaric oxygen** is a treatment for severe carbon monoxide poisoning, but it is not the initial or sole treatment for a patient with suspected co-existing cyanide poisoning.
- While recommended for **severe CO poisoning**, it doesn't directly address cyanide toxicity, which is suggested by the metabolic acidosis with a high lactate level despite normal oxygen saturation.
*Sodium thiosulfate and sodium nitrite*
- This combination (the **Lilly kit**) is traditionally used to treat **cyanide poisoning**, with sodium nitrite inducing methemoglobinemia to sequester cyanide, and sodium thiosulfate aiding its excretion.
- The patient also requires treatment for **carbon monoxide poisoning**, and hydroxycobalamin is generally preferred over sodium nitrite as it does not induce methemoglobinemia, which can worsen hypoxia in CO poisoning.
*Intravenous epinephrine*
- **Epinephrine** is a powerful vasoconstrictor and bronchodilator primarily used to treat **anaphylaxis** or **cardiac arrest**.
- There is no indication of anaphylaxis or cardiac arrest in this patient, and epinephrine would not be an appropriate treatment for carbon monoxide or cyanide poisoning.
Local anesthesia and nerve blocks US Medical PG Question 7: Two hours after undergoing elective cholecystectomy with general anesthesia, a 41-year-old woman is evaluated for decreased mental status. BMI is 36.6 kg/m2. Respirations are 18/min and blood pressure is 126/73 mm Hg. Physical examination shows the endotracheal tube in normal position. She does not respond to sternal rub and gag reflex is absent. Arterial blood gas analysis on room air shows normal PO2 and PCO2 levels. Which of the following anesthetic properties is the most likely cause of these findings?
- A. Low blood solubility
- B. High lipid solubility (Correct Answer)
- C. Low brain-blood partition coefficient
- D. High minimal alveolar concentration
- E. Low cytochrome P450 activity
Local anesthesia and nerve blocks Explanation: ***High lipid solubility***
- Anesthetics with **high lipid solubility** accumulate in **adipose tissue** and are slowly released, prolonging their effect, especially in obese patients.
- The patient's **obesity (BMI 36.6 kg/m2)** contributes to a larger reservoir for lipid-soluble drugs, leading to delayed recovery and decreased mental status.
*Low blood solubility*
- **Low blood solubility** implies a rapid equilibrium between the lungs and the blood, leading to a **faster onset and offset** of anesthetic action.
- This property would result in a quicker recovery from anesthesia, which contradicts the patient's prolonged unconsciousness.
*Low brain-blood partition coefficient*
- A **low brain-blood partition coefficient** means the anesthetic does not accumulate significantly in brain tissue relative to blood.
- Agents with this property equilibrate quickly and leave the brain rapidly upon discontinuation, resulting in **fast recovery**, which is inconsistent with the patient's persistent decreased mental status.
*High minimal alveolar concentration*
- **High minimal alveolar concentration (MAC)** means that a higher concentration of the anesthetic gas is required to produce immobility in 50% of patients.
- A high MAC describes the **potency** of an anesthetic and does not directly explain prolonged recovery or decreased mental status in an obese patient, but rather indicates that a larger dose or concentration was needed to achieve anesthesia.
*Low cytochrome P450 activity*
- **Low cytochrome P450 activity** would lead to slower metabolism of drugs that are primarily cleared by this system, potentially prolonging their effects.
- While relevant for some drugs, the primary issue for inhaled anesthetics is their **physical distribution and elimination**, not typically metabolic clearance via Cytochrome P450 enzymes.
Local anesthesia and nerve blocks US Medical PG Question 8: A 28-year-old man comes to the emergency department for an injury sustained while doing construction. Physical examination shows a long, deep, irregular laceration on the lateral aspect of the left forearm with exposed fascia. Prior to surgical repair of the injury, a brachial plexus block is performed using a local anesthetic. Shortly after the nerve block is performed, he complains of dizziness and then loses consciousness. His radial pulse is faint and a continuous cardiac monitor shows a heart rate of 24/min. Which of the following is the most likely mechanism of action of the anesthetic that was administered?
- A. Activation of acetylcholine receptors
- B. Inactivation of ryanodine receptors
- C. Inactivation of sodium channels (Correct Answer)
- D. Activation of GABA receptors
- E. Inactivation of potassium channels
Local anesthesia and nerve blocks Explanation: ***Inactivation of sodium channels***
- Local anesthetics primarily work by reversibly blocking **voltage-gated sodium channels** in nerves.
- This prevents the influx of sodium ions, inhibiting the generation and propagation of **action potentials**, thus blocking pain signals.
- The clinical presentation of dizziness, loss of consciousness, and bradycardia represents systemic toxicity from intravascular absorption of the local anesthetic.
*Activation of acetylcholine receptors*
- Activation of **nicotinic or muscarinic acetylcholine receptors** is the primary mechanism of action for neuromuscular stimulants or parasympathomimetics, not local anesthetics.
- This would typically lead to muscle contraction or increased parasympathetic activity rather than analgesia and local nerve block.
*Inactivation of ryanodine receptors*
- Inactivation of **ryanodine receptors** primarily affects calcium release from the sarcoplasmic reticulum in muscle cells, crucial for excitation-contraction coupling.
- This mechanism is associated with drugs like dantrolene used for malignant hyperthermia, not local anesthetics.
*Activation of GABA receptors*
- Activation of **GABA-A receptors** is the primary mechanism of action for benzodiazepines and barbiturates, leading to widespread CNS depression and sedation.
- While systemic absorption of local anesthetics can cause CNS effects (as seen in toxicity), their primary therapeutic mechanism for nerve block is sodium channel inactivation, not GABA receptor activation.
*Inactivation of potassium channels*
- Inactivation of **potassium channels** would typically prolong repolarization and increase neuronal excitability or cause arrhythmias, depending on the specific channel.
- This is not the mechanism of action for local anesthetics, which prevent depolarization by blocking sodium channel activation.
Local anesthesia and nerve blocks US Medical PG Question 9: A 23-year-old man is brought to the emergency department by ambulance following a motor vehicle accident. He was pinned between 2 cars for several hours. The patient has a history of asthma. He uses an albuterol inhaler intermittently. The patient was not the driver, and admits to having a few beers at a party prior to the accident. His vitals in the ambulance are stable. Upon presentation to the emergency department, the patient is immediately brought to the operating room for evaluation and surgical intervention. It is determined that the patient’s right leg has a Gustilo IIIC injury in the mid-shaft of the tibia with a severely comminuted fracture. The patient’s left leg suffered a similar injury but with damage to the peroneal nerve. The anesthesiologist begins to induce anesthesia. Which of the following agents would be contraindicated in this patient?
- A. Halothane
- B. Propofol
- C. Etomidate
- D. Succinylcholine (Correct Answer)
- E. Neostigmine
Local anesthesia and nerve blocks Explanation: ***Succinylcholine***
- Given the history of the patient being pinned between two cars for several hours, there is a significant risk of **rhabdomyolysis** and subsequent hyperkalemia.
- **Succinylcholine**, a depolarizing neuromuscular blocker, can cause a sudden and significant release of potassium from muscle cells, leading to **life-threatening hyperkalemia** in patients with rhabdomyolysis or crush injuries.
*Halothane*
- While **halothane** has been associated with **malignant hyperthermia**, the patient's history does not directly suggest an increased risk for this condition here.
- It also has a bronchodilating effect, which could be beneficial for a patient with a history of **asthma**.
*Propofol*
- **Propofol** is a commonly used intravenous anesthetic for induction and maintenance, providing rapid onset and recovery.
- There are generally no specific contraindications for propofol in a patient with a crush injury or asthma.
*Etomidate*
- **Etomidate** is an intravenous anesthetic agent known for its **cardiovascular stability**, making it a good choice for hemodynamically unstable patients.
- It can cause adrenal suppression, but this is usually a concern with prolonged infusions, not a single induction dose.
*Neostigmine*
- **Neostigmine** is an acetylcholinesterase inhibitor used to reverse the effects of non-depolarizing neuromuscular blockers.
- It is not an induction agent and would not be used at the beginning of anesthesia induction.
Local anesthesia and nerve blocks US Medical PG Question 10: A 60-year-old man is brought to the emergency department 25 minutes after falling and hitting his left flank on a concrete block. He has severe left-sided chest pain and mild shortness of breath. He underwent a right knee replacement surgery 2 years ago. He has type 2 diabetes mellitus. He has smoked one pack of cigarettes daily for 42 years. Current medications include metformin, sitagliptin, and a multivitamin. He appears uncomfortable. His temperature is 37.5°C (99.5°F), pulse is 102/min, respirations are 17/min, and blood pressure is 132/90 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 96%. Examination shows multiple abrasions on his left flank and trunk. The upper left chest wall is tender to palpation and bony crepitus is present. There are decreased breath sounds over both lung bases. Cardiac examination shows no murmurs, rubs, or gallops. The abdomen is soft and nontender. Focused assessment with sonography for trauma is negative. An x-ray of the chest shows nondisplaced fractures of the left 4th and 5th ribs, with clear lung fields bilaterally. Which of the following is the most appropriate next step in management?
- A. Internal fixation
- B. Admission and surveillance in the intensive care unit
- C. Prophylactic antibiotic therapy
- D. Adequate analgesia and conservative management (Correct Answer)
- E. Continuous positive airway pressure
Local anesthesia and nerve blocks Explanation: ***Adequate analgesia and conservative management***
- The patient has **nondisplaced rib fractures** with clear lung fields and stable vitals, indicating that conservative management with **adequate analgesia** is the most appropriate initial step.
- Pain control is crucial to prevent complications such as **pneumonia** and **atelectasis** by allowing the patient to breathe deeply and cough effectively.
*Internal fixation*
- **Internal fixation** is generally reserved for patients with severe rib fractures, such as **flail chest**, significant displacement, or those who fail conservative management, which is not the case here.
- This patient's fractures are **nondisplaced**, and he is hemodynamically stable without signs of respiratory compromise requiring surgical intervention.
*Admission and surveillance in the intensive care unit*
- Admission to the **intensive care unit (ICU)** is typically indicated for patients with **flail chest**, severe respiratory distress, or significant associated injuries, which are absent in this patient.
- While rib fractures can be serious, stable patients with **nondisplaced fractures** do not automatically require ICU admission; a general medical ward or even outpatient management (depending on overall stability and pain control) might be sufficient.
*Prophylactic antibiotic therapy*
- There is currently **no evidence of infection** (e.g., fever, elevated white blood cell count, purulent sputum) to warrant prophylactic antibiotic therapy.
- Rib fractures themselves, without an open wound or lung contusion leading to pneumonia, do not routinely require **antibiotics**.
*Continuous positive airway pressure*
- **Continuous positive airway pressure (CPAP)** is used for respiratory support in conditions like **acute respiratory failure** or **sleep apnea**, or in severe chest wall injuries like flail chest causing significant respiratory compromise.
- This patient has an **oxygen saturation of 96%** on room air and mild shortness of breath, indicating he does not currently require CPAP.
More Local anesthesia and nerve blocks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.