General anesthesia principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for General anesthesia principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
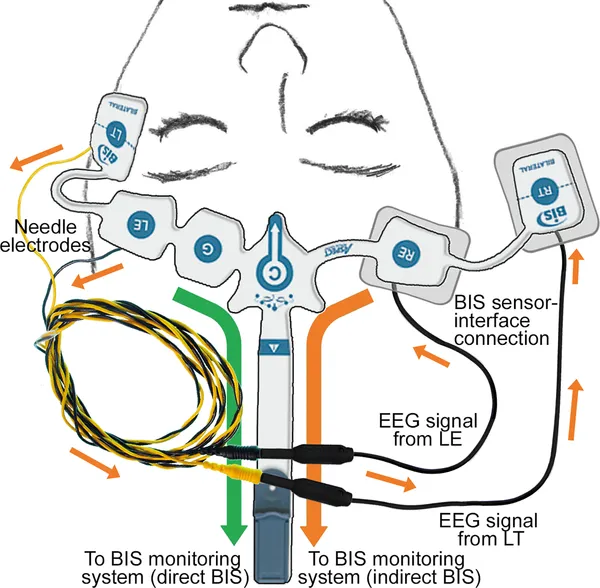
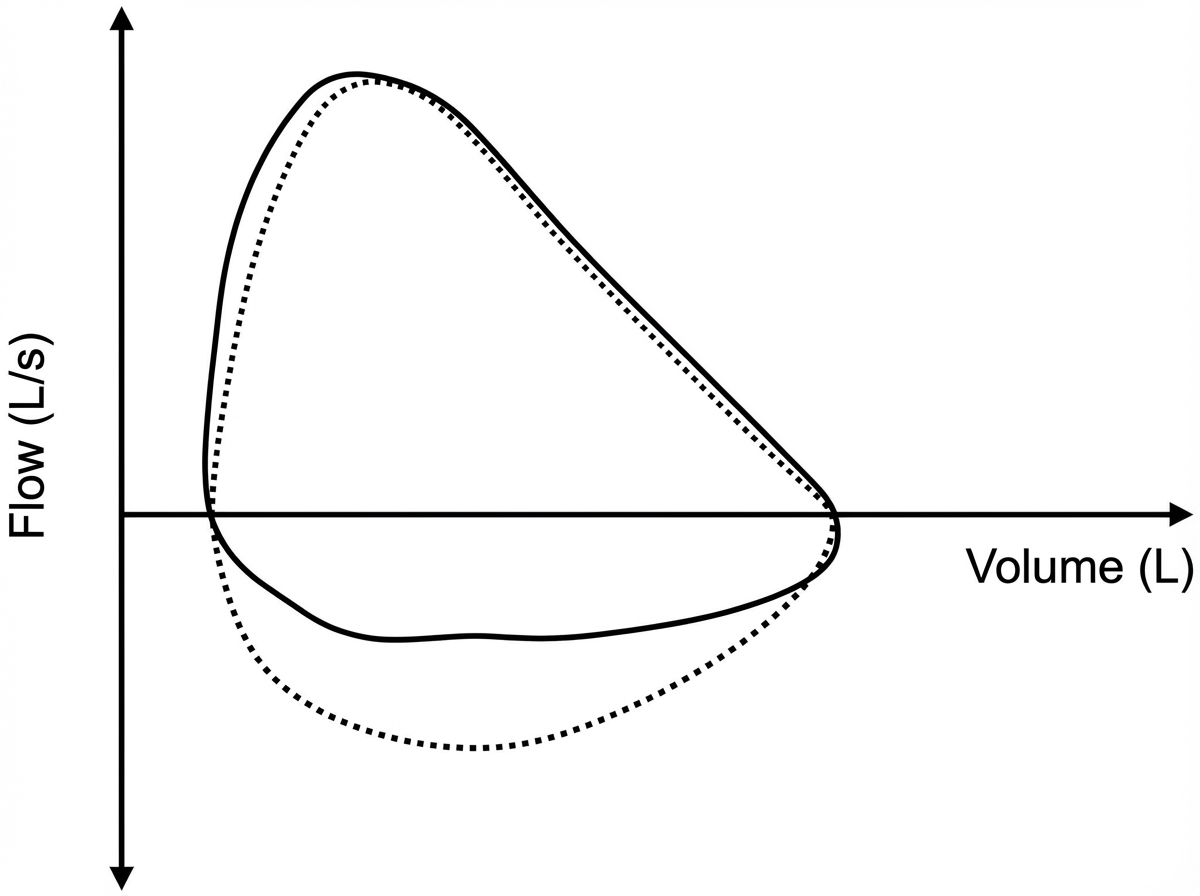
General anesthesia principles US Medical PG Question 1: Five minutes after arriving in the postoperative care unit following total knee replacement under general anesthesia, a 55-year-old woman is acutely short of breath. The procedure was uncomplicated. Postoperatively, prophylactic treatment with cefazolin was begun and the patient received morphine and ketorolac for pain management. She has generalized anxiety disorder. Her only other medication is escitalopram. She has smoked one pack of cigarettes daily for 25 years. Her temperature is 37°C (98.6°F), pulse is 108/min, respirations are 26/min, and blood pressure is 95/52 mm Hg. A flow-volume loop obtained via pulmonary function testing is shown. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Decreased central respiratory drive
- B. Neuromuscular blockade
- C. Bronchial hyperresponsiveness
- D. Rupture of an alveolar bleb
- E. Type I hypersensitivity reaction (Correct Answer)
General anesthesia principles Explanation: ***Type I hypersensitivity reaction***
- The patient's acute shortness of breath, **tachycardia (pulse 108/min)**, **hypotension (95/52 mm Hg)**, and tachypnea (respirations 26/min) immediately post-surgery are highly suggestive of **anaphylaxis**, which is a severe, systemic type I hypersensitivity reaction.
- The sudden onset shortly after general anesthesia and initiation of prophylactic cefazolin points to a potential allergic reaction to a medication administered during this period (e.g., **antibiotics**, **neuromuscular blockers**, anesthetics).
*Decreased central respiratory drive*
- This would typically lead to **bradypnea** or hypopnea rather than the tachypnea seen in this patient.
- While opioids like morphine can depress respiratory drive, the patient's respiratory rate of 26/min indicates an *increased* drive.
*Neuromuscular blockade*
- Residual neuromuscular blockade would cause respiratory muscle weakness, leading to **shallow breathing** and potentially hypoventilation, but not typically the acute onset of shortness of breath with tachypnea and systemic hemodynamic instability observed here.
- The immediate onset of symptoms also points away from persistent effects of intraoperative neuromuscular blockers, which are usually reversed before emergence.
*Bronchial hyperresponsiveness*
- While the patient is a smoker, which can predispose to respiratory issues, **bronchial hyperresponsiveness** (e.g., asthma exacerbation) typically presents with **wheezing**, prolonged expiration, and often hypoxemia, which are not described.
- The severe hypotension and acute onset of systemic symptoms are not typical features of an isolated asthma flare-up.
*Rupture of an alveolar bleb*
- A ruptured bleb can cause a **pneumothorax**, leading to sudden shortness of breath and chest pain.
- However, it would not typically cause **systemic hypotension** or tachycardia to this degree without other signs of tension pneumothorax (e.g., tracheal deviation, absent breath sounds).
General anesthesia principles US Medical PG Question 2: A 59-year-old woman is scheduled to undergo a right hip total arthroplasty for severe hip osteoarthritis that has failed conservative management. She has never had surgery before. She has a history of major depressive disorder and takes sertraline daily and ibuprofen occasionally for pain. Her mother died of breast cancer and her father died from a myocardial infarction. She has a brother who had an adverse reaction following anesthesia, but she does not know details of the event. In the operating room, the anesthesiologist administers isoflurane and succinylcholine. Two minutes later, the patient develops hypercarbia and hypertonicity of her bilateral upper and lower extremities. Her temperature is 103.7°F (39.8°C), blood pressure is 155/95 mmHg, pulse is 115/min, and respirations are 20/min.
A medication with which of the following mechanisms of action is most strongly indicated for this patient?
- A. Muscarinic antagonist
- B. Antihistamine
- C. Ryanodine receptor antagonist (Correct Answer)
- D. Cholinesterase inhibitor
- E. Dopamine receptor agonist
General anesthesia principles Explanation: ***Ryanodine receptor antagonist***
- The patient's presentation with **hyperthermia**, **hypercarbia**, and **muscle rigidity** after exposure to isoflurane and succinylcholine is highly indicative of **malignant hyperthermia (MH)**.
- **Dantrolene**, a **ryanodine receptor antagonist**, is the primary treatment for MH as it blocks the release of calcium from the sarcoplasmic reticulum, thereby reducing muscle contraction and heat production.
*Muscarinic antagonist*
- **Muscarinic antagonists** like atropine block the action of acetylcholine at muscarinic receptors and are used to treat **bradycardia** or reduce secretions.
- They would not address the underlying pathophysiology of malignant hyperthermia, which involves uncontrolled calcium release from the sarcoplasmic reticulum.
*Antihistamine*
- **Antihistamines** block histamine receptors and are used to treat **allergic reactions** or reduce nausea and vomiting.
- They have no role in the management of malignant hyperthermia, which is not an allergic response.
*Cholinesterase inhibitor*
- **Cholinesterase inhibitors** increase acetylcholine levels at the neuromuscular junction and are used to reverse **neuromuscular blockade** or treat **myasthenia gravis**.
- Administering a cholinesterase inhibitor would likely intensify muscle contraction and rigidity, worsening the patient's condition in malignant hyperthermia.
*Dopamine receptor agonist*
- **Dopamine receptor agonists** are primarily used to treat **Parkinson's disease** or as **vasopressors** in critical care.
- They have no direct therapeutic effect on the severe muscle rigidity and hypermetabolic state characteristic of malignant hyperthermia.
General anesthesia principles US Medical PG Question 3: Two hours after undergoing elective cholecystectomy with general anesthesia, a 41-year-old woman is evaluated for decreased mental status. BMI is 36.6 kg/m2. Respirations are 18/min and blood pressure is 126/73 mm Hg. Physical examination shows the endotracheal tube in normal position. She does not respond to sternal rub and gag reflex is absent. Arterial blood gas analysis on room air shows normal PO2 and PCO2 levels. Which of the following anesthetic properties is the most likely cause of these findings?
- A. Low blood solubility
- B. High lipid solubility (Correct Answer)
- C. Low brain-blood partition coefficient
- D. High minimal alveolar concentration
- E. Low cytochrome P450 activity
General anesthesia principles Explanation: ***High lipid solubility***
- Anesthetics with **high lipid solubility** accumulate in **adipose tissue** and are slowly released, prolonging their effect, especially in obese patients.
- The patient's **obesity (BMI 36.6 kg/m2)** contributes to a larger reservoir for lipid-soluble drugs, leading to delayed recovery and decreased mental status.
*Low blood solubility*
- **Low blood solubility** implies a rapid equilibrium between the lungs and the blood, leading to a **faster onset and offset** of anesthetic action.
- This property would result in a quicker recovery from anesthesia, which contradicts the patient's prolonged unconsciousness.
*Low brain-blood partition coefficient*
- A **low brain-blood partition coefficient** means the anesthetic does not accumulate significantly in brain tissue relative to blood.
- Agents with this property equilibrate quickly and leave the brain rapidly upon discontinuation, resulting in **fast recovery**, which is inconsistent with the patient's persistent decreased mental status.
*High minimal alveolar concentration*
- **High minimal alveolar concentration (MAC)** means that a higher concentration of the anesthetic gas is required to produce immobility in 50% of patients.
- A high MAC describes the **potency** of an anesthetic and does not directly explain prolonged recovery or decreased mental status in an obese patient, but rather indicates that a larger dose or concentration was needed to achieve anesthesia.
*Low cytochrome P450 activity*
- **Low cytochrome P450 activity** would lead to slower metabolism of drugs that are primarily cleared by this system, potentially prolonging their effects.
- While relevant for some drugs, the primary issue for inhaled anesthetics is their **physical distribution and elimination**, not typically metabolic clearance via Cytochrome P450 enzymes.
General anesthesia principles US Medical PG Question 4: A 29-year-old man is being monitored at the hospital after cutting open his left wrist. He has a long-standing history of unipolar depressive disorder and multiple trials of antidepressants. The patient expresses thoughts of self-harm and does not deny suicidal intent. A course of electroconvulsive therapy is suggested. His medical history is not significant for other organic illness. Which of the following complications of this therapy is this patient at greatest risk for?
- A. Acute kidney injury
- B. Acute coronary syndrome
- C. Anterograde amnesia
- D. Intracranial hemorrhage
- E. Retrograde amnesia (Correct Answer)
General anesthesia principles Explanation: ***Retrograde amnesia***
- **Retrograde amnesia**, specifically memory loss for events occurring prior to the treatment, is a common and often transient side effect of **electroconvulsive therapy (ECT)**.
- While generally temporary, it can be distressing for patients and is a significant consideration when recommending ECT, especially in patients with otherwise healthy brains.
*Acute kidney injury*
- **Acute kidney injury (AKI)** is not a typical direct complication of **ECT**.
- While fluid and electrolyte imbalances or certain medications used during ECT (e.g., muscle relaxants) could theoretically impact renal function in predisposed individuals, it is not a primary concern in a patient with no significant history of organic illness.
*Acute coronary syndrome*
- **Acute coronary syndrome (ACS)** is a potential risk associated with the physiological stress of **ECT**, which can include transient **hypertension** and **tachycardia**.
- However, in a 29-year-old with no significant medical history, the risk is considerably lower compared to older patients or those with pre-existing cardiovascular disease.
*Anterograde amnesia*
- **Anterograde amnesia**, the inability to form new memories after the treatment, is typically less common and usually milder than retrograde amnesia following **ECT**.
- While some patients may experience transient difficulty recalling new information immediately post-ECT, it is usually less pronounced than the impact on remote memories.
*Intracranial hemorrhage*
- **Intracranial hemorrhage** is an extremely rare and severe complication of **ECT**, typically associated with pre-existing cerebral vascular abnormalities or uncontrolled hypertension during the procedure.
- In a young patient with no organic illness, the risk of this complication is exceedingly low.
General anesthesia principles US Medical PG Question 5: A 28-year-old man comes to the emergency department for an injury sustained while doing construction. Physical examination shows a long, deep, irregular laceration on the lateral aspect of the left forearm with exposed fascia. Prior to surgical repair of the injury, a brachial plexus block is performed using a local anesthetic. Shortly after the nerve block is performed, he complains of dizziness and then loses consciousness. His radial pulse is faint and a continuous cardiac monitor shows a heart rate of 24/min. Which of the following is the most likely mechanism of action of the anesthetic that was administered?
- A. Activation of acetylcholine receptors
- B. Inactivation of ryanodine receptors
- C. Inactivation of sodium channels (Correct Answer)
- D. Activation of GABA receptors
- E. Inactivation of potassium channels
General anesthesia principles Explanation: ***Inactivation of sodium channels***
- Local anesthetics primarily work by reversibly blocking **voltage-gated sodium channels** in nerves.
- This prevents the influx of sodium ions, inhibiting the generation and propagation of **action potentials**, thus blocking pain signals.
- The clinical presentation of dizziness, loss of consciousness, and bradycardia represents systemic toxicity from intravascular absorption of the local anesthetic.
*Activation of acetylcholine receptors*
- Activation of **nicotinic or muscarinic acetylcholine receptors** is the primary mechanism of action for neuromuscular stimulants or parasympathomimetics, not local anesthetics.
- This would typically lead to muscle contraction or increased parasympathetic activity rather than analgesia and local nerve block.
*Inactivation of ryanodine receptors*
- Inactivation of **ryanodine receptors** primarily affects calcium release from the sarcoplasmic reticulum in muscle cells, crucial for excitation-contraction coupling.
- This mechanism is associated with drugs like dantrolene used for malignant hyperthermia, not local anesthetics.
*Activation of GABA receptors*
- Activation of **GABA-A receptors** is the primary mechanism of action for benzodiazepines and barbiturates, leading to widespread CNS depression and sedation.
- While systemic absorption of local anesthetics can cause CNS effects (as seen in toxicity), their primary therapeutic mechanism for nerve block is sodium channel inactivation, not GABA receptor activation.
*Inactivation of potassium channels*
- Inactivation of **potassium channels** would typically prolong repolarization and increase neuronal excitability or cause arrhythmias, depending on the specific channel.
- This is not the mechanism of action for local anesthetics, which prevent depolarization by blocking sodium channel activation.
General anesthesia principles US Medical PG Question 6: A 23-year-old man is brought to the emergency department by ambulance following a motor vehicle accident. He was pinned between 2 cars for several hours. The patient has a history of asthma. He uses an albuterol inhaler intermittently. The patient was not the driver, and admits to having a few beers at a party prior to the accident. His vitals in the ambulance are stable. Upon presentation to the emergency department, the patient is immediately brought to the operating room for evaluation and surgical intervention. It is determined that the patient’s right leg has a Gustilo IIIC injury in the mid-shaft of the tibia with a severely comminuted fracture. The patient’s left leg suffered a similar injury but with damage to the peroneal nerve. The anesthesiologist begins to induce anesthesia. Which of the following agents would be contraindicated in this patient?
- A. Halothane
- B. Propofol
- C. Etomidate
- D. Succinylcholine (Correct Answer)
- E. Neostigmine
General anesthesia principles Explanation: ***Succinylcholine***
- Given the history of the patient being pinned between two cars for several hours, there is a significant risk of **rhabdomyolysis** and subsequent hyperkalemia.
- **Succinylcholine**, a depolarizing neuromuscular blocker, can cause a sudden and significant release of potassium from muscle cells, leading to **life-threatening hyperkalemia** in patients with rhabdomyolysis or crush injuries.
*Halothane*
- While **halothane** has been associated with **malignant hyperthermia**, the patient's history does not directly suggest an increased risk for this condition here.
- It also has a bronchodilating effect, which could be beneficial for a patient with a history of **asthma**.
*Propofol*
- **Propofol** is a commonly used intravenous anesthetic for induction and maintenance, providing rapid onset and recovery.
- There are generally no specific contraindications for propofol in a patient with a crush injury or asthma.
*Etomidate*
- **Etomidate** is an intravenous anesthetic agent known for its **cardiovascular stability**, making it a good choice for hemodynamically unstable patients.
- It can cause adrenal suppression, but this is usually a concern with prolonged infusions, not a single induction dose.
*Neostigmine*
- **Neostigmine** is an acetylcholinesterase inhibitor used to reverse the effects of non-depolarizing neuromuscular blockers.
- It is not an induction agent and would not be used at the beginning of anesthesia induction.
General anesthesia principles US Medical PG Question 7: A 17-year-old boy is brought to the emergency department by his brother after losing consciousness 1 hour ago. The brother reports that the patient was skateboarding outside when he fell on the ground and started to have generalized contractions. There was also some blood coming from his mouth. The contractions stopped after about 1 minute, but he remained unconscious for a few minutes afterward. He has never had a similar episode before. There is no personal or family history of serious illness. He does not smoke or drink alcohol. He does not use illicit drugs. He takes no medications. On arrival, he is confused and oriented only to person and place. He cannot recall what happened and reports diffuse muscle ache, headache, and fatigue. He appears pale. His temperature is 37°C (98.6°F), pulse is 80/min, and blood pressure is 130/80 mm Hg. There is a small wound on the left side of the tongue. A complete blood count and serum concentrations of electrolytes, urea nitrogen, and creatinine are within the reference ranges. Toxicology screening is negative. An ECG shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Electroencephalography
- B. Lumbar puncture
- C. Lorazepam therapy
- D. Reassurance and follow-up
- E. CT scan of the head (Correct Answer)
General anesthesia principles Explanation: ***CT scan of the head***
- Given the **first-time seizure** in an adolescent, especially with a history of head trauma (falling while skateboarding) and subsequent confusion, a **CT scan of the head** is crucial to rule out acute structural lesions like hemorrhage, mass, or edema.
- It is vital for identifying **life-threatening causes** of seizure that require immediate intervention, such as an **intracranial hematoma** or **mass lesion**, which could have been precipitated or exacerbated by the fall.
*Electroencephalography*
- **EEG** is appropriate for later evaluation to diagnose and classify seizure disorders, but it is not the *most appropriate initial step* in the emergency setting for a first-time seizure with a possible traumatic etiology.
- An EEG might be normal shortly after a seizure, and it does not rule out acute structural brain pathology that requires urgent management.
*Lumbar puncture*
- A **lumbar puncture** is indicated if there's suspicion of meningoencephalitis (e.g., fever, nuchal rigidity, immunocompromised status), which are not prominent features in this patient.
- The patient's vital signs are stable, and there are no signs of infection, making this a less urgent initial diagnostic step compared to imaging.
*Lorazepam therapy*
- **Lorazepam** is a benzodiazepine used to terminate ongoing seizures (**status epilepticus**), but this patient's generalized contractions have already stopped.
- Administering lorazepam when the seizure has resolved is unnecessary and would only cause further sedation.
*Reassurance and follow-up*
- While reassurance is part of patient care, it is *insufficient* as the sole next step for a **first-time seizure** episode in an adolescent, especially with features suggesting a possible underlying acute cause.
- A thorough diagnostic workup, beginning with neuroimaging, is necessary to ensure there is no serious underlying pathology before considering discharge and follow-up.
General anesthesia principles US Medical PG Question 8: A 55-year-old man with chronic pain on high-dose opioids (120 mg oral morphine equivalents daily) requires major spine surgery. Intraoperatively, he requires escalating doses of fentanyl with poor pain control. Postoperatively, his pain remains severe (10/10) despite maximum conventional multimodal analgesia including IV hydromorphone PCA, acetaminophen, and ketorolac. He becomes increasingly agitated and tachycardic. Evaluate the most comprehensive pain management strategy addressing the underlying pathophysiology.
- A. Increase PCA opioid dose to match home requirements plus surgical pain needs
- B. Transition to methadone for better mu-receptor coverage
- C. Ketamine infusion to address opioid-induced hyperalgesia and NMDA receptor sensitization (Correct Answer)
- D. Epidural analgesia with local anesthetic and low-dose opioid
- E. Regional nerve blocks with liposomal bupivacaine
General anesthesia principles Explanation: ***Ketamine infusion to address opioid-induced hyperalgesia and NMDA receptor sensitization***
- The patient exhibits **opioid-induced hyperalgesia (OIH)**, where high-dose opioids paradoxically increase pain sensitivity through **NMDA receptor** activation and central sensitization.
- **Ketamine** is an NMDA receptor antagonist that directly targets the underlying pathophysiology to reverse **central sensitization** and reduce the "wind-up" phenomenon.
*Increase PCA opioid dose to match home requirements plus surgical pain needs*
- Simply increasing the opioid dose in a patient with **OIH** can exacerbate the pain sensitization rather than alleviate it.
- This strategy fails to address the down-regulation of **mu-receptors** and the neuroplastic changes associated with chronic high-dose opioid use.
*Transition to methadone for better mu-receptor coverage*
- While **methadone** has NMDA antagonist properties, a rapid transition in the acute postoperative setting is pharmacokinetically complex and lacks the immediate efficacy of a **low-dose ketamine infusion**.
- Methadone titration is challenging due to its long **half-life** and risk of delayed respiratory depression in an agitated, acutely painful patient.
*Epidural analgesia with local anesthetic and low-dose opioid*
- While neuraxial techniques are normally effective, **major spine surgery** often complicates or precludes the placement of an epidural due to surgical site constraints or dural integrity.
- This approach may provide regional relief but does not systemically address the **centralized hyperalgesia** caused by chronic high-dose opioid therapy.
*Regional nerve blocks with liposomal bupivacaine*
- **Regional blocks** for extensive spine surgery may provide inadequate coverage for the broad dermatomal distribution involved in major spinal procedures.
- These blocks target **peripheral nerves** and do not address the **NMDA-mediated sensitization** in the central nervous system that is driving this patient's severe pain.
General anesthesia principles US Medical PG Question 9: A 70-year-old man with severe aortic stenosis (valve area 0.6 cm², mean gradient 55 mmHg) develops acute cholecystitis requiring surgery. He is symptomatic with exertional angina and dyspnea. Cardiology recommends TAVR before surgery, but the patient has signs of gallbladder perforation. The surgical team debates timing of interventions. Evaluate the optimal management strategy weighing cardiac and surgical risks.
- A. Emergency cholecystectomy under general anesthesia with careful hemodynamic monitoring
- B. Medical management of cholecystitis with antibiotics, TAVR in 6 weeks, then cholecystectomy
- C. Percutaneous cholecystostomy tube followed by TAVR, then delayed cholecystectomy (Correct Answer)
- D. Combined TAVR and cholecystectomy in one procedure
- E. Open cholecystectomy under epidural anesthesia to avoid general anesthesia risks
General anesthesia principles Explanation: ***Percutaneous cholecystostomy tube followed by TAVR, then delayed cholecystectomy***
- Severe, symptomatic **aortic stenosis (AS)** represents an extremely high perioperative risk for major non-cardiac surgery; a **percutaneous cholecystostomy** provides rapid source control for the gallbladder under local anesthesia without the hemodynamic stress of general anesthesia.
- This staged approach stabilizes the surgical emergency first, allowing for **Transcatheter Aortic Valve Replacement (TAVR)** to be performed under safer conditions before the patient undergoes a definitive cholecystectomy.
*Emergency cholecystectomy under general anesthesia with careful hemodynamic monitoring*
- The perioperative mortality risk for patients with **symptomatic severe AS** undergoing non-cardiac surgery is unacceptably high due to the inability to increase **cardiac output** in response to surgical stress.
- Induction of general anesthesia and **positive pressure ventilation** can lead to sudden, fatal drops in systemic vascular resistance and preload that the stenotic valve cannot accommodate.
*Medical management of cholecystitis with antibiotics, TAVR in 6 weeks, then cholecystectomy*
- Signs of **gallbladder perforation** constitute a surgical emergency that cannot be managed with antibiotics alone as it will likely lead to **septic shock**.
- Delaying definitive treatment for the gallbladder for 6 weeks in the presence of a perforation would likely result in patient death before cardiac optimization could occur.
*Combined TAVR and cholecystectomy in one procedure*
- Performing a **combined procedure** unnecessarily prolongs anesthesia time and increases the risk of complications such as **bleeding** from the anticoagulation required for TAVR.
- The inflammatory state from the acute cholecystitis and potential sepsis would significantly increase the risk of **TAVR complications**, including valve thrombosis or migration.
*Open cholecystectomy under epidural anesthesia to avoid general anesthesia risks*
- **Neuraxial anesthesia** (spinal or epidural) is generally **contraindicated** in severe aortic stenosis because it can cause rapid sympatholysis and severe **hypotension**.
- An open surgical approach is more invasive and causes more physiological stress than a percutaneous drain, which is the safer initial strategy for an unstable cardiac patient.
General anesthesia principles US Medical PG Question 10: A 42-year-old woman with a history of multiple anesthetic complications presents for elective surgery. Previous records indicate awareness during general anesthesia twice, prolonged paralysis after succinylcholine requiring 6 hours of ventilation, and a sibling with fatal anesthetic complication involving hyperthermia and rhabdomyolysis. Evaluate the comprehensive anesthetic plan that addresses all potential complications.
- A. Genetic testing before proceeding with any anesthetic
- B. Total intravenous anesthesia with propofol and remifentanil, avoid succinylcholine and volatile agents, use rocuronium with sugammadex reversal (Correct Answer)
- C. Standard general anesthesia with dantrolene prophylaxis
- D. Volatile anesthetic with BIS monitoring, avoid all muscle relaxants
- E. Regional anesthesia only without any general anesthetic agents
General anesthesia principles Explanation: ***Total intravenous anesthesia with propofol and remifentanil, avoid succinylcholine and volatile agents, use rocuronium with sugammadex reversal***
- **Total intravenous anesthesia (TIVA)** using propofol and remifentanil avoids **volatile anesthetics** and **succinylcholine**, which are mandatory triggers for **malignant hyperthermia (MH)** mentioned in the family history.
- Avoiding **succinylcholine** prevents prolonged paralysis due to suspected **pseudocholinesterase deficiency**, while **rocuronium** with **sugammadex** provides safe neuromuscular blockade and reliable reversal.
*Genetic testing before proceeding with any anesthetic*
- While **genetic testing** for **RYR1** or **BCHE** mutations is helpful, it is not a comprehensive "anesthetic plan" and would delay necessary elective surgery.
- Negative genetic results do not fully rule out **malignant hyperthermia** susceptibility; clinical precautions must be taken regardless.
*Standard general anesthesia with dantrolene prophylaxis*
- **Dantrolene prophylaxis** is no longer recommended; the standard of care is the strict avoidance of triggering agents like **isoflurane** or **sevoflurane**.
- Using standard anesthesia would involve **volatile agents**, which are contraindicated due to the high risk of **malignant hyperthermia** suggested by the sibling's death.
*Volatile anesthetic with BIS monitoring, avoid all muscle relaxants*
- **Volatile anesthetics** are absolute contraindications in patients at risk for **malignant hyperthermia**, regardless of monitoring techniques used.
- Avoiding all muscle relaxants may lead to poor surgical conditions, whereas **non-depolarizing agents** like **rocuronium** are safe in these patients.
*Regional anesthesia only without any general anesthetic agents*
- While **regional anesthesia** is a safe alternative, it may be insufficient depending on the surgical site or complexity of the procedure.
- A history of **anesthesia awareness** indicates a need for a controlled general anesthetic plan if surgery is not amenable to a simple block.
More General anesthesia principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.