Small bowel obstruction US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Small bowel obstruction. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Small bowel obstruction US Medical PG Question 1: A 69-year-old male presents to the Emergency Department with bilious vomiting that started within the past 24 hours. His medical history is significant for hypertension, hyperlipidemia, and a myocardial infarction six months ago. His past surgical history is significant for a laparotomy 20 years ago for a perforated diverticulum. Most recently he had some dental work done and has been on narcotic pain medicine for the past week. He reports constipation and obstipation. He is afebrile with a blood pressure of 146/92 mm Hg and a heart rate of 116/min. His abdominal exam reveals multiple well-healed scars with distension but no tenderness. An abdominal/pelvic CT scan reveals dilated small bowel with a transition point to normal caliber bowel distally. When did the cause of his pathology commence?
- A. One week ago
- B. Six months ago
- C. 20 years ago (Correct Answer)
- D. At birth
- E. 24 hours ago
Small bowel obstruction Explanation: ***20 years ago***
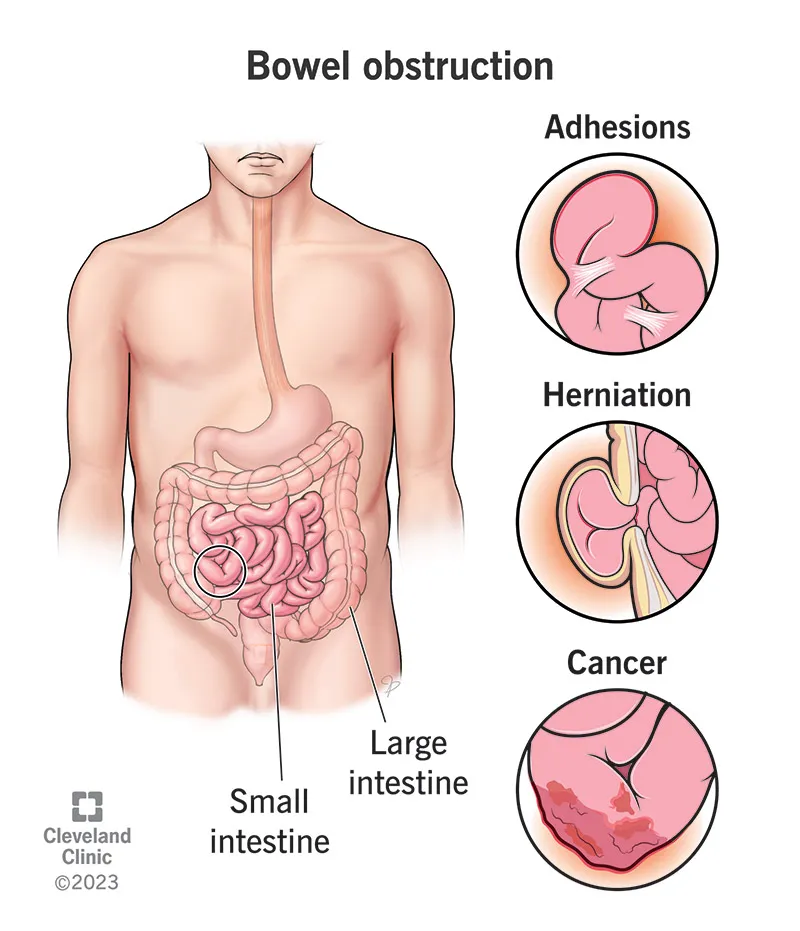
- The patient's history of a **laparotomy 20 years ago** for a perforated diverticulum is the most likely cause of his current small bowel obstruction. **Adhesions** from prior abdominal surgery are the leading cause of small bowel obstruction.
- The CT scan finding of **dilated small bowel** with a **transition point** confirms a mechanical obstruction, and the operative scarring supports adhesions as the etiology.
*One week ago*
- While **narcotic pain medicine** can cause constipation and ileus, it typically leads to a more diffuse distention without a clear transition point characteristic of a mechanical obstruction.
- The development of a clear transition point on CT after only one week of narcotic use makes a mechanical obstruction from adhesions more likely than a pure narcotic-induced ileus.
*Six months ago*
- A **myocardial infarction** six months ago is not directly related to the development of a small bowel obstruction.
- While cardiac events can sometimes lead to mesenteric ischemia, the CT findings of a transition point are more indicative of a mechanical obstruction rather than ischemia.
*At birth*
- Congenital conditions causing small bowel obstruction, such as **atresia** or **malrotation**, typically present in infancy or early childhood.
- Given the patient's age and history of prior abdominal surgery, a congenital cause is highly unlikely.
*24 hours ago*
- The onset of symptoms within the past 24 hours describes the **acute presentation** of the obstruction, not its underlying cause.
- The obstruction itself developed over time due to a predisposing factor from his past medical history.
Small bowel obstruction US Medical PG Question 2: A 76-year-old female is brought to the emergency department after being found unresponsive in her room at her nursing facility. Past medical history is significant for Alzheimer's disease, hypertension, and diabetes. Surgical history is notable for an open cholecystectomy at age 38 and multiple cesarean sections. On arrival, she is non-responsive but breathing by herself, and her vital signs are T 102.9 F, HR 123 bpm, BP 95/64, RR 26/min, and SaO2 97% on 6L nasal cannula. On physical exam the patient has marked abdominal distension and is tympanic to percussion. Laboratory studies are notable for a lactic acidosis. An upright abdominal radiograph and CT abdomen/pelvis with contrast are shown in Figures A and B respectively. She is started on IV fluids and a nasogastric tube is placed to suction which returns green bilious fluid. Repeat vitals 1 hour later are T 101F, HR 140 bpm, BP 75/44, RR 30/min, and SaO2 is 100% on the ventilator after she is intubated for airway concerns. What is the next best step in management?
- A. Sigmoidoscopy, attempted derotation and rectal tube placement
- B. Continue IV fluid hydration, nasogastric suction, NPO
- C. Pneumatic enema
- D. Immediate laparotomy and surgical management (Correct Answer)
- E. Therapy with levofloxacin and metronidazole
Small bowel obstruction Explanation: ***Immediate laparotomy and surgical management***
- The patient presents with **signs of shock** (hypotension, tachycardia, tachypnea, fever, lactic acidosis) and **peritoneal signs** (marked abdominal distension, tympany) along with imaging findings (not provided but implied by the clinical picture) consistent with **bowel obstruction complicated by ischemia or perforation**. **Laparotomy** is urgently needed to address the underlying surgical emergency.
- Given the patient's deteriorating vital signs despite initial resuscitation, and the likelihood of **severe bowel compromise**, medical management or less invasive procedures are insufficient and would delay definitive treatment.
*Sigmoidoscopy, attempted derotation and rectal tube placement*
- This approach is typically used for **uncomplicated sigmoid volvulus** in a stable patient without signs of perforation or peritonitis.
- Given the patient's **septic shock** and **lactic acidosis**, there is a high suspicion of bowel ischemia or perforation, making endoscopic derotation contraindicated and dangerous.
*Continue IV fluid hydration, nasogastric suction, NPO*
- While important initial steps for any bowel obstruction, these measures alone are **insufficient** given the patient's rapidly deteriorating condition and evidence of **organ damage** (lactic acidosis suggests tissue hypoperfusion/ischemia).
- These are supportive measures, not definitive treatment for a **surgical emergency** like complicated bowel obstruction.
*Pneumatic enema*
- **Pneumatic enema** is primarily used for the reduction of **intussusception**, usually in pediatric patients.
- It is **not indicated** for the management of suspected bowel obstruction with signs of ischemia or perforation in an elderly patient and could be harmful.
*Therapy with levofloxacin and metronidazole*
- While **antibiotics** are crucial in managing septic shock due to an abdominal source, they are an **adjunctive treatment** and not the primary step for a surgical emergency.
- Antibiotics alone will not resolve the underlying mechanical obstruction or address compromised bowel, which requires **surgical intervention**.
Small bowel obstruction US Medical PG Question 3: A 68-year-old woman is brought to the emergency department with intense abdominal pain for the past 2 hours. She has had 1 episode of bloody diarrhea recently. She has an 18-year history of diabetes mellitus. She was diagnosed with hypertension and ischemic heart disease 6 years ago. She is fully alert and oriented. Her temperature is 37.5°C (99.5°F), blood pressure is 145/90 mm Hg, pulse is 78/min, and respirations are 14/min. Abdominal examination shows mild generalized abdominal tenderness without guarding or rebound tenderness. An abdominal plain X-ray shows no abnormalities. Abdominal CT reveals colonic wall thickening and pericolonic fat stranding in the splenic curvature. Bowel rest, intravenous hydration, and IV antibiotics are initiated. Which of the following is the most important diagnostic evaluation at this time?
- A. Angiography
- B. Gastrografin-enhanced X-ray
- C. Laparotomy
- D. Inpatient observation
- E. Sigmoidoscopy (Correct Answer)
Small bowel obstruction Explanation: ***Sigmoidoscopy***
- The patient's presentation with acute abdominal pain, bloody diarrhea, history of cardiovascular disease, and CT findings consistent with **colonic wall thickening** and **pericolonic fat stranding** strongly suggests **ischemic colitis**.
- **Flexible sigmoidoscopy** allows for direct visualization of the colonic mucosa to confirm the diagnosis, assess the extent and severity of ischemia, and rule out other causes of colitis, such as inflammatory bowel disease or infection.
*Angiography*
- While angiography can identify mesenteric arterial occlusion, it is generally reserved for cases of acute mesenteric ischemia involving the superior mesenteric artery, which typically presents with more severe pain out of proportion to physical exam findings and less clear CT findings of colitis.
- In cases of ischemic colitis, where the primary concern is mucosal ischemia rather than immediate large vessel occlusion, angiography is usually not the first-line diagnostic.
*Gastrografin-enhanced X-ray*
- This study (also known as a **Gastrografin swallow or enema**) is primarily used to evaluate for **perforations** or **obstructions**, or to assess lumen integrity.
- It does not provide the mucosal detail necessary to diagnose or assess the severity of **ischemic colitis**, and the contrast agent itself could potentially exacerbate an inflamed bowel.
*Laparotomy*
- **Laparotomy** (surgical exploration) is an invasive procedure reserved for cases with signs of peritonitis, bowel perforation, or severe, unresponsive ischemia requiring surgical intervention.
- Given the patient's stable vital signs, mild tenderness, and lack of guarding or rebound, immediate surgical exploration is not warranted without further diagnostic steps.
*Inpatient observation*
- While inpatient observation is part of the initial management (bowel rest, IV fluids, antibiotics), it is not a **diagnostic evaluation** itself.
- The question asks for the most important diagnostic evaluation to determine the underlying cause and guide further management.
Small bowel obstruction US Medical PG Question 4: A 54-year-old man comes to the physician because of diarrhea that has become progressively worse over the past 4 months. He currently has 4–6 episodes of foul-smelling stools per day. Over the past 3 months, he has had fatigue and a 5-kg (11-lb) weight loss. He returned from Bangladesh 6 months ago after a year-long business assignment. He has osteoarthritis and hypertension. Current medications include amlodipine and naproxen. He appears pale and malnourished. His temperature is 37.3°C (99.1°F), pulse is 76/min, and blood pressure is 140/86 mm Hg. Examination shows pale conjunctivae and dry mucous membranes. Angular stomatitis and glossitis are present. The abdomen is distended but soft and nontender. Rectal examination shows no abnormalities. Laboratory studies show:
Hemoglobin 8.9 g/dL
Leukocyte count 4100/mm3
Platelet count 160,000/mm3
Mean corpuscular volume 110 μm3
Serum
Na+ 133 mEq/L
Cl- 98 mEq/l
K+ 3.3 mEq/L
Creatinine 1.1 mg/dL
IgA 250 mg/dL
Anti-tissue transglutaminase, IgA negative
Stool culture and studies for ova and parasites are negative. Test of the stool for occult blood is negative. Fecal fat content is 22 g/day (N < 7). Fecal lactoferrin is negative and elastase is within normal limits. Which of the following is the most appropriate next step in diagnosis?
- A. CT scan of the abdomen
- B. IgG against deamidated gliadin peptide
- C. Schilling test
- D. Enteroscopy
- E. PAS-stained biopsy of small bowel (Correct Answer)
Small bowel obstruction Explanation: ***PAS-stained biopsy of small bowel***
- The patient's history of travel to Bangladesh, chronic diarrhea, malabsorption (weight loss, fatigue, elevated fecal fat, macrocytic anemia), and negative celiac serology (anti-tissue transglutaminase IgA) are highly suggestive of **Whipple's disease**.
- **Periodic Acid-Schiff (PAS) staining** of a small bowel biopsy is the gold standard for diagnosing Whipple's disease, revealing **PAS-positive macrophages** containing *Tropheryma whipplei*.
*CT scan of the abdomen*
- While a CT scan can identify structural abnormalities or masses, it is not the most direct diagnostic test for **malabsorptive conditions** like Whipple's disease.
- It would likely show non-specific findings such as **bowel wall thickening** or **lymphadenopathy**, but not the definitive histological changes.
*IgG against deamidated gliadin peptide*
- This test is used to diagnose **celiac disease**, but the patient's IgA anti-tissue transglutaminase was already negative, and this IgG test is typically performed when IgA deficiency is suspected or in young children.
- Given the strong suspicion of an infectious etiology due to travel history and systemic symptoms, focusing solely on celiac serology is less appropriate as the first next step.
*Schilling test*
- The Schilling test is an **obsolete test** that was historically used to assess **vitamin B12 absorption** and differentiate causes of B12 deficiency (pernicious anemia, bacterial overgrowth, or pancreatic insufficiency).
- This test is **no longer performed in clinical practice** due to unavailability of radioactive B12; modern evaluation uses serum B12, methylmalonic acid, and homocysteine levels.
- While the patient has macrocytic anemia, the test would not directly address the underlying cause of fat malabsorption and systemic symptoms present.
*Enteroscopy*
- Enteroscopy allows for visualization and biopsy of the small bowel beyond the reach of a standard upper endoscopy.
- While useful for obtaining biopsies, simply performing an enteroscopy without knowing what to look for or what specific stain to request (referring to PAS) on the biopsy would be less targeted than ordering a **PAS-stained biopsy** specifically.
Small bowel obstruction US Medical PG Question 5: A 75-year-old man is brought to the emergency department after 2 days of severe diffuse abdominal pain, nausea, vomiting, and lack of bowel movements, which has led him to stop eating. He has a history of type-2 diabetes mellitus, hypertension, and chronic obstructive pulmonary disease. Upon admission, his vital signs are within normal limits and physical examination shows diffuse abdominal tenderness, distention, lack of bowel sounds, and an empty rectal ampulla. After initial fluid therapy and correction of moderate hypokalemia, the patient's condition shows mild improvement. His abdominal plain film is taken and shown. Which of the following is the most appropriate concomitant approach?
- A. Exploratory surgery
- B. Initiate pain management with morphine
- C. Initiate intravenous metoclopramide
- D. Gastrografin enema
- E. Nasogastric decompression (Correct Answer)
Small bowel obstruction Explanation: ***Nasogastric decompression***
- The patient exhibits symptoms consistent with **bowel obstruction** (diffuse abdominal pain, distention, absent bowel sounds, empty rectal ampulla), which can lead to significant fluid and gas accumulation. **Nasogastric decompression** is crucial to relieve pressure, prevent aspiration, and stabilize the patient.
- This intervention helps manage symptoms, reduces the risk of complications, and provides time for further diagnostic workup while addressing fluid and electrolyte imbalances.
*Exploratory surgery*
- While surgery may be indicated for complete bowel obstruction, it is usually reserved for cases that fail conservative management or show signs of **strangulation** or **perforation**.
- Without evidence of these acute complications and given the patient's mild improvement after initial therapy, immediate surgery is not the most appropriate first step.
*Initiate pain management with morphine*
- While pain management is important, **opioids** like morphine can actually **reduce bowel motility** and worsen a bowel obstruction.
- Addressing the underlying obstruction through decompression should be prioritized before initiating pain medication that could exacerbate the condition.
*Initiate intravenous metoclopramide*
- **Metoclopramide** is a **prokinetic agent** that increases gastrointestinal motility.
- In a suspected bowel obstruction, stimulating motility can increase intraluminal pressure and potentially worsen the condition or increase the risk of perforation, making it contraindicated.
*Gastrografin enema*
- A **Gastrografin enema** is typically used to diagnose and sometimes treat **distal colonic obstructions**, or as a therapeutic trial for **meconium ileus** in infants.
- Given the diffuse abdominal pain and an empty rectal ampulla suggesting a more proximal or severe obstruction, an enema may not be appropriate and could even be dangerous if there's a risk of perforation.
Small bowel obstruction US Medical PG Question 6: A 55-year-old woman comes to the emergency department because of a 24-hour history of severe lower abdominal pain. She has had two episodes of nonbloody vomiting today and has been unable to keep down food or fluids. She has not had a bowel movement since the day before. She has hypertension, hyperlipidemia, and osteoarthritis. She had a cholecystectomy 5 years ago. She has smoked one pack of cigarettes daily for the last 20 years. Current medications include chlorthalidone, atorvastatin, and naproxen. Her temperature is 38.8°C (101.8°F), pulse is 102/min, respirations are 20/min, and blood pressure is 118/78 mm Hg. She is 1.68 m (5 ft 6 in) tall and weighs 94.3 kg (207.9 lbs); BMI is 33.4 kg/m2. Abdominal examination shows a soft abdomen with hypoactive bowel sounds. There is moderate left lower quadrant tenderness. A tender mass is palpable on digital rectal examination. There is no guarding or rebound tenderness. Laboratory studies show:
Leukocyte count 17,000/mm3
Hemoglobin 13.3 g/dl
Hematocrit 40%
Platelet count 188,000/mm3
Serum
Na+ 138 mEq/L
K+ 4.1 mEq/L
Cl- 101 mEq/L
HCO3- 22 mEq/L
Urea Nitrogen 18.1 mg/dl
Creatinine 1.1 mg/dl
Which of the following is most appropriate to confirm the diagnosis?
- A. Abdominal x-ray
- B. Abdominal ultrasound
- C. Exploratory laparotomy
- D. Flexible sigmoidoscopy
- E. CT scan of the abdomen with contrast (Correct Answer)
Small bowel obstruction Explanation: ***CT scan of the abdomen with contrast***
- A CT scan with contrast is the **gold standard** for diagnosing diverticulitis,
especially given the patient's acute presentation, fever, leukocytosis, and
localized left lower quadrant tenderness. It can visualize **diverticula**,
wall thickening, inflammation, and potential complications like abscesses.
- The patient's presentation with acute, severe lower
abdominal pain, fever, leukocytosis, and a palpable tender mass on
rectal exam suggests **acute diverticulitis**, making a CT scan the most
appropriate diagnostic next step.
*Abdominal x-ray*
- An abdominal X-ray can detect **free air** (suggesting
perforation) or **bowel obstruction**, but it is generally *not sensitive
or specific enough* to diagnose diverticulitis or its complications.
- It would likely miss key findings of inflammation or abscess
formation associated with diverticulitis.
*Abdominal ultrasound*
- While useful for some abdominal conditions, ultrasound often has
**limited views** of the colon due to **bowel gas** and is less effective
at detecting deep-seated inflammation or abscesses in diverticulitis compared to CT.
- Its diagnostic utility for diverticulitis is generally *lower* than
CT, especially in obese patients where visualization can be challenging.
*Exploratory laparotomy*
- This is an **invasive surgical procedure** used for diagnosis and
treatment when other methods have failed or there is clear evidence of a
surgical emergency (e.g., massive bleeding, perforation with diffuse
peritonitis).
- It is *not the initial diagnostic step* for suspected diverticulitis;
less invasive imaging is always performed first.
*Flexible sigmoidoscopy*
- Flexible sigmoidoscopy is **contraindicated** in acute diverticulitis
due to the high **risk of perforation** of an inflamed and fragile colon.
- Endoscopic procedures are typically performed after acute inflammation
has subsided, usually several weeks later, to assess the extent of
diverticular disease and rule out other pathologies.
Small bowel obstruction US Medical PG Question 7: A 55-year-old man presents to the emergency department with nausea and vomiting. The patient states that he has felt nauseous for the past week and began vomiting last night. He thought his symptoms would resolve but decided to come in when his symptoms worsened. He feels that his symptoms are exacerbated with large fatty meals and when he drinks alcohol. His wife recently returned from a cruise with symptoms of vomiting and diarrhea. The patient has a past medical history of poorly managed diabetes, constipation, anxiety, dyslipidemia, and hypertension. His temperature is 99.5°F (37.5°C), blood pressure is 197/128 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 95% on room air. Physical exam reveals a systolic murmur heard loudest along the left upper sternal border. Abdominal exam reveals an obese, tympanitic and distended abdomen with a 3 cm scar in the right lower quadrant. Vascular exam reveals weak pulses in the lower extremities. Which of the following is the most likely diagnosis?
- A. Enteric nervous system damage
- B. Twisting of the bowel
- C. Adhesions (Correct Answer)
- D. Norovirus
- E. Impacted stool
Small bowel obstruction Explanation: ***Adhesions***
- The patient's history of a 3 cm scar in the right lower quadrant suggests a prior abdominal surgery, which is the most common cause of **intra-abdominal adhesions**.
- **Adhesions** can lead to **small bowel obstruction**, causing symptoms like nausea, vomiting, abdominal distension, and tympany, which are all present in this patient.
*Enteric nervous system damage*
- Poorly managed diabetes can cause **diabetic gastroparesis**, which involves damage to the **enteric nervous system** leading to delayed gastric emptying.
- While it can cause nausea and vomiting, it doesn't typically present with significant abdominal distension or tympany, which are indicative of a mechanical obstruction.
*Twisting of the bowel*
- **Volvulus**, or twisting of the bowel, causes acute abdominal pain, distension, and often complete obstruction.
- While it's a possibility for bowel obstruction, the presence of a surgical scar and gradual worsening of symptoms over a week makes **adhesions** a more likely cause in this scenario.
*Norovirus*
- **Norovirus** is a common cause of acute gastroenteritis, characterized by abrupt onset of vomiting and diarrhea, often with a rapid resolution.
- Although his wife has similar symptoms, the patient's symptoms have been ongoing for a week, are exacerbated by fatty meals, and include abdominal distension, which is inconsistent with typical norovirus infection.
*Impacted stool*
- **Fecal impaction** can cause constipation, abdominal pain, and sometimes paradoxical diarrhea.
- While the patient has a history of constipation, the significant **tympanic distension** and persistent vomiting suggest a mechanical obstruction rather than just impacted stool.
Small bowel obstruction US Medical PG Question 8: A 73-year-old man presents to the emergency department complaining of abdominal pain with nausea and vomiting, stating that he “can’t keep anything down”. He states that the pain has been gradually getting worse over the past 2 months, saying that, at first, it was present only an hour after he ate but now is constant. He also says that he has been constipated for the last 2 weeks, which has also been getting progressively worse. His last bowel movement was 4 days ago which was normal. He states that he cannot pass flatus. The patient’s past medical history is significant for hypertension and an episode of pneumonia last year. The patient is afebrile and his pulse is 105/min. On physical examination, the patient is uncomfortable. His lungs are clear to auscultation bilaterally. His abdomen is visibly distended and diffusely tender with tympany on percussion. A contrast CT scan of the abdomen shows dilated loops of small bowel with collapsed large bowel. Which of the following is the most likely cause of this patient’s condition?
- A. Incarcerated hernia
- B. Crohn's disease
- C. Diverticulitis
- D. Adhesions
- E. Mass effect from a tumor (Correct Answer)
Small bowel obstruction Explanation: ***Mass effect from a tumor***
- The patient's **progressive symptoms** over two months, including worsening abdominal pain initially post-prandial but now constant, progressive constipation, and inability to pass flatus, strongly suggest a **gradually developing obstruction**.
- In a **73-year-old patient**, the **progressive course** and age make **colorectal cancer** a primary concern for mechanical bowel obstruction.
- The **CT findings** of dilated small bowel loops with collapsed distal large bowel indicate a **transition point likely at the level of the distal ileum/ileocecal junction or proximal colon**, consistent with a mass causing mechanical obstruction. With a competent ileocecal valve, a proximal colonic mass can lead to retrograde small bowel dilation.
- The **gradual two-month progression** is highly characteristic of a **growing neoplasm** causing progressive luminal narrowing.
*Incarcerated hernia*
- An incarcerated hernia typically presents with more **acute and severe localized pain**, often associated with a **palpable bulge** at common hernia sites (inguinal, femoral, umbilical, or ventral).
- While it can cause small bowel obstruction, the **gradual onset and steady progression over two months** are atypical for hernia incarceration, which usually develops more acutely.
*Crohn's disease*
- Crohn's disease is characterized by **chronic transmural inflammation** of the GI tract, often presenting with recurrent abdominal pain, diarrhea, weight loss, and sometimes strictures leading to obstruction.
- However, the patient's **age (73)** with **new-onset symptoms** and **no prior inflammatory history** make Crohn's disease unlikely, as it typically presents in younger patients (teens to 30s) with a chronic relapsing-remitting course.
*Diverticulitis*
- Diverticulitis typically presents with **acute localized left lower quadrant pain**, fever, and leukocytosis due to inflammation of colonic diverticula.
- While chronic diverticulitis can lead to strictures, it would more likely cause **large bowel obstruction** rather than the small bowel dilation pattern seen here, and the **absence of fever** and **two-month progressive course** are less typical.
*Adhesions*
- Adhesions are the **most common cause of small bowel obstruction overall**, especially in patients with a **history of prior abdominal or pelvic surgery**.
- However, this patient has **no mentioned surgical history**, and adhesions typically cause **acute or intermittent obstructive episodes** rather than the **steady two-month progressive course** characteristic of a growing malignant mass.
Small bowel obstruction US Medical PG Question 9: A 32-year-old man comes to the emergency department because of recurrent episodes of vomiting for 1 day. He has had over 15 episodes of bilious vomiting. During this period he has had cramping abdominal pain but has not had a bowel movement or passed flatus. He does not have fever or diarrhea. He was diagnosed with Crohn disease at the age of 28 years which has been well controlled with oral mesalamine. He underwent a partial small bowel resection for midgut volvulus at birth. His other medications include vitamin B12, folic acid, loperamide, ferrous sulfate, and vitamin D3. He appears uncomfortable and his lips are parched. His temperature is 37.1°C (99.3°F), pulse is 103/min, and blood pressure is 104/70 mm Hg. The abdomen is distended, tympanitic, and tender to palpation over the periumbilical area and the right lower quadrant. Rectal examination is unremarkable. A CT scan of the abdomen shows multiple dilated loops of small bowel with a transition zone in the mid to distal ileum. After 24 hours of conservative management with IV fluid resuscitation, nasogastric bowel decompression, promethazine, and analgesia, his condition does not improve and a laparotomy is scheduled. During the laparotomy, two discrete strictures are noted in the mid-ileum, around 20 cm apart. Which of the following is the most appropriate next step in management?
- A. Small bowel resection with ileostomy
- B. Abdominal closure and start palliative care
- C. Small bowel resection and primary anastomosis
- D. Strictureplasty of individual strictures (Correct Answer)
- E. Ileocolectomy
Small bowel obstruction Explanation: ***Strictureplasty of individual strictures***
- This patient presents with **multiple strictures** in the mid-ileum causing a small bowel obstruction in the setting of **Crohn's disease**. Strictureplasty is the preferred surgical approach for *short, multiple (up to four), or recurrent Crohn's disease strictures* as it preserves bowel length.
- While small bowel resection is an option, **strictureplasty** is favored in Crohn's disease to *avoid short bowel syndrome*, especially if multiple strictures are present, as seen here.
*Small bowel resection with ileostomy*
- An ileostomy is typically created when a primary anastomosis is not safe due to high risk of leak (e.g., severe inflammation, peritonitis, patient instability) or when there is extensive disease not amenable to strictureplasty with primary anastomosis.
- Performing an ileostomy when primary anastomosis is possible unnecessarily creates a stoma, which can lead to complications and impact quality of life.
*Abdominal closure and start palliative care*
- This patient, while acutely unwell, has a surgically correctable cause for his obstruction and is not described as having an incurable or end-stage condition necessitating only palliative care.
- Palliative care would be considered for patients with widespread untreatable disease or severe comorbidities, which is not indicated here given the localized, treatable strictures.
*Small bowel resection and primary anastomosis*
- While small bowel resection is a valid treatment for isolated, non-recurrent strictures, strictureplasty is generally preferred in Crohn's disease when multiple strictures are present.
- **Resection of multiple segments** can lead to significant **short bowel syndrome**, especially in a patient with a history of prior small bowel resection, making strictureplasty a more bowel-sparing and appropriate choice.
*Ileocolectomy*
- **Ileocolectomy** involves resection of the terminal ileum and a portion of the colon. This would be indicated if the disease involves the *ileocecal valve region* or the *colon*, which is not the case in this patient, whose strictures are in the mid-ileum.
- This procedure is excessive for mid-ileal strictures and would result in unnecessary removal of healthy bowel given the location of the strictures.
Small bowel obstruction US Medical PG Question 10: An institutionalized 65-year-old man is brought to the emergency department because of abdominal pain and distension for 12 hours. The pain was acute in onset and is a cramping-type pain associated with nausea, vomiting, and constipation. He has a history of chronic constipation and has used laxatives for years. There is no history of inflammatory bowel disease in his family. He has not been hospitalized recently. There is no recent history of weight loss or change in bowel habits. On physical examination, the patient appears ill. The abdomen is distended with tenderness mainly in the left lower quadrant and is tympanic on percussion. The blood pressure is 110/79 mm Hg, heart rate is 100/min, the respiratory rate is 20/min, and the temperature is 37.2°C (99.0°F). The CBC shows an elevated white blood cell count. The plain abdominal X-ray is shown in the accompanying image. What is the most likely cause of his condition?
- A. Sigmoid volvulus (Correct Answer)
- B. Intussusception
- C. Acute diverticulitis
- D. Toxic megacolon
- E. Colon cancer
Small bowel obstruction Explanation: ***Sigmoid volvulus***
- The patient’s symptoms of acute **abdominal pain**, distension, and cramping strongly indicate **sigmoid volvulus**, often seen in chronic constipation and institutionalized patients.
- Physical examination revealing **tenderness in the left lower quadrant** and a tympanic abdomen supports the diagnosis of bowel obstruction typically caused by **volvulus**.
*Intussusception*
- Generally presents with **currant jelly stools** and is more common in children; the acute symptoms here are less typical.
- It often involves a **lead point** or associated conditions like **polyps** or tumors, which are not indicated in this case.
*Acute diverticulitis*
- Usually associated with **localized pain** in the left lower quadrant but would present with fever and changes in bowel habits, which the patient lacks.
- Typically shows **peritoneal signs** and may have complications like abscess or perforation, not indicated here.
*Toxic megacolon*
- Commonly associated with underlying **inflammatory bowel disease** or infections, not indicated in this patient with no recent history of **IBD**.
- Symptoms would include severe **diarrhea** and abdominal pain, which do not fit the current acute cramping and constipation pattern.
*Colon cancer*
- While it can cause abdominal symptoms, it presents more insidiously with **weight loss** or **change in bowel habits**, none of which are reported here.
- The acute presentation and findings do not align with a malignancy, which would often be chronic in nature.
More Small bowel obstruction US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.