Mesenteric ischemia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mesenteric ischemia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Mesenteric ischemia US Medical PG Question 1: A 57-year-old man presents with 2 days of severe, generalized, abdominal pain that is worse after meals. He is also nauseated and reports occasional diarrhea mixed with blood. Apart from essential hypertension, his medical history is unremarkable. His vital signs include a temperature of 36.9°C (98.4°F), blood pressure of 145/92 mm Hg, and an irregularly irregular pulse of 105/min. Physical examination is only notable for mild periumbilical tenderness. Which of the following is the most likely diagnosis?
- A. Diverticular disease
- B. Acute pancreatitis
- C. Gastroenteritis
- D. Crohn's disease
- E. Acute mesenteric ischemia (Correct Answer)
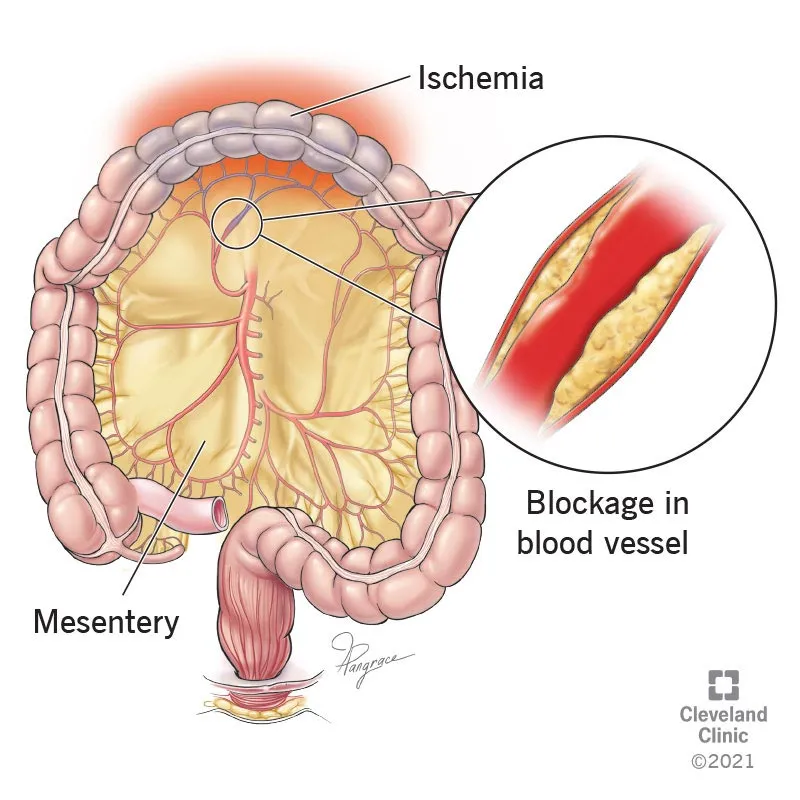
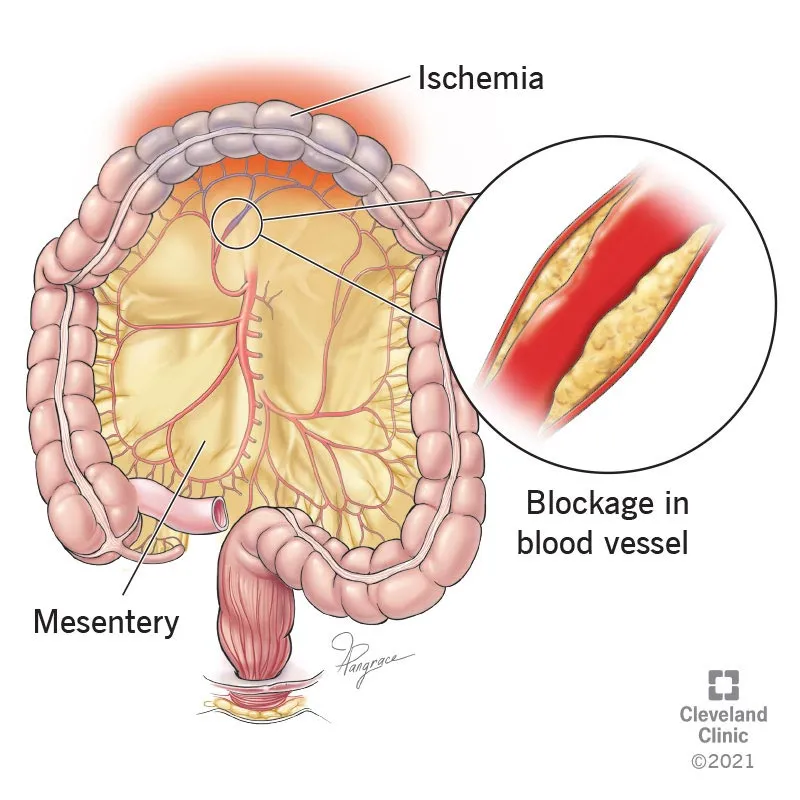
Mesenteric ischemia Explanation: ***Acute mesenteric ischemia***
- The patient's presentation with **severe, generalized abdominal pain worse after meals**, along with **bloody diarrhea** and **irregularly irregular pulse** (suggesting **atrial fibrillation**), is highly indicative of acute mesenteric ischemia.
- Atrial fibrillation can lead to **emboli** that occlude mesenteric arteries, causing rapid onset of **ischemic bowel injury** with disproportionate pain and often minimal findings on physical exam.
*Diverticular disease*
- While diverticulitis can cause abdominal pain, it is typically localized to the **left lower quadrant** and often associated with fever and leukocytosis, which are absent here.
- **Diverticular bleeding** usually presents as painless rectal bleeding, not severe, diffuse abdominal pain with ischemic features.
*Acute pancreatitis*
- Characterized by severe **epigastric pain radiating to the back**, often associated with nausea and vomiting, but not typically with bloody diarrhea.
- Elevated **lipase** and **amylase** levels are diagnostic markers, and an irregularly irregular pulse is not a direct symptom.
*Gastroenteritis*
- Often causes diffuse abdominal pain, nausea, vomiting, and diarrhea, but the pain is rarely as severe or disproportionate to physical findings as described.
- **Bloody diarrhea** can occur, but the rapid onset of severe pain, particularly in the context of possible **embolic source** (atrial fibrillation), makes ischemia more likely.
*Crohn's disease*
- A chronic inflammatory bowel disease presenting with **abdominal pain**, **diarrhea** (often bloody), and weight loss, developing over weeks to months.
- The acute, severe onset of symptoms in this patient does not fit the typical chronic presentation of Crohn's disease.
Mesenteric ischemia US Medical PG Question 2: A 68-year-old woman is brought to the emergency department with intense abdominal pain for the past 2 hours. She has had 1 episode of bloody diarrhea recently. She has an 18-year history of diabetes mellitus. She was diagnosed with hypertension and ischemic heart disease 6 years ago. She is fully alert and oriented. Her temperature is 37.5°C (99.5°F), blood pressure is 145/90 mm Hg, pulse is 78/min, and respirations are 14/min. Abdominal examination shows mild generalized abdominal tenderness without guarding or rebound tenderness. An abdominal plain X-ray shows no abnormalities. Abdominal CT reveals colonic wall thickening and pericolonic fat stranding in the splenic curvature. Bowel rest, intravenous hydration, and IV antibiotics are initiated. Which of the following is the most important diagnostic evaluation at this time?
- A. Angiography
- B. Gastrografin-enhanced X-ray
- C. Laparotomy
- D. Inpatient observation
- E. Sigmoidoscopy (Correct Answer)
Mesenteric ischemia Explanation: ***Sigmoidoscopy***
- The patient's presentation with acute abdominal pain, bloody diarrhea, history of cardiovascular disease, and CT findings consistent with **colonic wall thickening** and **pericolonic fat stranding** strongly suggests **ischemic colitis**.
- **Flexible sigmoidoscopy** allows for direct visualization of the colonic mucosa to confirm the diagnosis, assess the extent and severity of ischemia, and rule out other causes of colitis, such as inflammatory bowel disease or infection.
*Angiography*
- While angiography can identify mesenteric arterial occlusion, it is generally reserved for cases of acute mesenteric ischemia involving the superior mesenteric artery, which typically presents with more severe pain out of proportion to physical exam findings and less clear CT findings of colitis.
- In cases of ischemic colitis, where the primary concern is mucosal ischemia rather than immediate large vessel occlusion, angiography is usually not the first-line diagnostic.
*Gastrografin-enhanced X-ray*
- This study (also known as a **Gastrografin swallow or enema**) is primarily used to evaluate for **perforations** or **obstructions**, or to assess lumen integrity.
- It does not provide the mucosal detail necessary to diagnose or assess the severity of **ischemic colitis**, and the contrast agent itself could potentially exacerbate an inflamed bowel.
*Laparotomy*
- **Laparotomy** (surgical exploration) is an invasive procedure reserved for cases with signs of peritonitis, bowel perforation, or severe, unresponsive ischemia requiring surgical intervention.
- Given the patient's stable vital signs, mild tenderness, and lack of guarding or rebound, immediate surgical exploration is not warranted without further diagnostic steps.
*Inpatient observation*
- While inpatient observation is part of the initial management (bowel rest, IV fluids, antibiotics), it is not a **diagnostic evaluation** itself.
- The question asks for the most important diagnostic evaluation to determine the underlying cause and guide further management.
Mesenteric ischemia US Medical PG Question 3: A 63-year-old man is brought to the emergency department for the evaluation of severe abdominal pain that started suddenly 1 hour ago while he was having a barbecue with his family. The pain is located in the middle of his abdomen and he describes it as 9 out of 10 in intensity. The patient feels nauseated and has vomited twice. He has also had a loose bowel movement. He was diagnosed with hypertension 2 years ago and was started on hydrochlorothiazide. He stopped taking his pills 1 week ago because of several episodes of heart racing and dizziness that he attributes to his medication. The patient has smoked one pack of cigarettes daily for the last 40 years. He is in severe distress. His temperature is 37.6°C (99.7°F), pulse is 120/min, respirations are 16/min, and blood pressure is 130/90 mm Hg. Cardiac examination shows an irregularly irregular rhythm. Bowel sounds are normal. The abdomen is soft and nontender. The remainder of the physical examination shows no abnormalities. Laboratory studies show:
Hemoglobin 16.8 g/dL
Leukocyte count 13,000/mm3
Platelet count 340,000/mm3
Prothrombin time 13 seconds
Partial thromboplastin time 38 seconds
Lactate (venous) 2.4 mEq/L (N=0.5 - 2.2 mEq/L)
Serum
Urea Nitrogen 15 mg/dL
Creatinine 1.2 mg/dL
Lactate dehydrogenase
105 U/L
CT angiography is performed and the diagnosis is confirmed. Which of the following is the most appropriate definitive management of this patient?
- A. Anticoagulation with heparin
- B. MR angiography
- C. Colonoscopy
- D. Piperacillin/tazobactam administration
- E. Balloon angioplasty and stenting (Correct Answer)
Mesenteric ischemia Explanation: ***Balloon angioplasty and stenting***
- This patient presents with **acute mesenteric ischemia** due to an **embolic occlusion** (suggested by irregularly irregular rhythm indicating **atrial fibrillation** and sudden onset of severe abdominal pain out of proportion to physical findings).
- CT angiography has confirmed the diagnosis, and the patient shows **no signs of peritonitis** (soft, nontender abdomen) or bowel necrosis, making him an ideal candidate for **endovascular revascularization**.
- **Balloon angioplasty with stenting** or **catheter-directed thrombolysis** represents the **definitive management** to restore mesenteric blood flow and prevent bowel infarction in patients diagnosed early without peritoneal signs.
- Endovascular therapy has become increasingly preferred over open surgical embolectomy when feasible, offering lower morbidity and mortality with comparable efficacy in selected patients.
*Anticoagulation with heparin*
- While **immediate anticoagulation with heparin** is an essential **initial measure** to prevent clot propagation, it is **not definitive management**.
- Heparin should be started promptly but does **not restore blood flow** or remove the embolic occlusion; it serves as a bridge to definitive revascularization.
- All patients with acute mesenteric ischemia require revascularization (endovascular or surgical) in addition to anticoagulation.
*MR angiography*
- **CT angiography has already confirmed the diagnosis**, making additional imaging with MR angiography unnecessary and wasteful of critical time.
- In acute mesenteric ischemia, every minute counts—**"time is bowel"**—and delays in revascularization increase the risk of irreversible bowel necrosis.
*Colonoscopy*
- Colonoscopy evaluates the **colonic mucosa** and is used for lower GI bleeding, polyp surveillance, or inflammatory bowel disease.
- It has **no role in acute mesenteric ischemia**, which typically involves the **small bowel** supplied by the superior mesenteric artery, and provides no therapeutic benefit for vascular occlusion.
*Piperacillin/tazobactam administration*
- Broad-spectrum antibiotics may be considered as **adjunctive therapy** if bowel necrosis or translocation of bacteria is suspected.
- However, this patient has no peritoneal signs, fever, or other evidence of perforation or sepsis, and antibiotics do **not address the underlying vascular occlusion**.
- The priority is **urgent revascularization** to restore blood flow; antibiotics alone will not prevent bowel infarction.
Mesenteric ischemia US Medical PG Question 4: A 52-year-old woman complains of intermittent diffuse abdominal pain that becomes worse after eating meals and several episodes of diarrhea, the last of which was bloody. These symptoms have been present for the previous 6 months but have worsened recently. She has had significant weight loss since the onset of symptoms. Her past medical history includes systemic lupus erythematosus (SLE), which has been difficult to manage medically. Vital signs include a blood pressure of 100/70 mm Hg, temperature of 37.1°C (98.8 °F), and pulse of 95/min. On physical examination, the patient appears to be in severe pain, and there is mild diffuse abdominal tenderness. Which of the following is the most likely diagnosis?
- A. Ischemic bowel disease (Correct Answer)
- B. Small bowel obstruction
- C. Acute pancreatitis
- D. Gastroenteritis
- E. Ulcerative colitis
Mesenteric ischemia Explanation: ***Ischemic bowel disease***
- The patient's history of **diffuse abdominal pain worsening after meals** (postprandial pain or "abdominal angina"), **bloody diarrhea**, and **significant weight loss** is highly suggestive of **chronic mesenteric ischemia**.
- Her history of **systemic lupus erythematosus (SLE)**, which can cause **vasculitis** and **hypercoagulability**, increases the risk of mesenteric artery thrombosis or emboli, leading to bowel ischemia.
*Small bowel obstruction*
- This typically presents with **colicky abdominal pain**, **vomiting**, and **abdominal distension**, often with obstipation.
- While it can cause pain, it does not typically lead to **bloody diarrhea** or chronic postprandial worsening of symptoms.
*Acute pancreatitis*
- Characterized by **severe epigastric pain** radiating to the back, often associated with nausea and vomiting, and elevated lipase/amylase.
- It does not typically present with **bloody diarrhea** or a chronic history of symptoms worsening after eating.
*Gastroenteritis*
- Usually presents with **acute onset** of nausea, vomiting, diarrhea, and fever, often resolving within a few days to a week.
- The **chronic nature** (6 months) of symptoms, significant weight loss, and the specific pattern of postprandial pain make gastroenteritis unlikely.
*Ulcerative colitis*
- While it causes **bloody diarrhea** and abdominal pain, it typically involves the colon and rectum, and pain is less commonly described as diffuse and worsening specifically after meals due to ischemia.
- The primary symptoms are usually **tenesmus**, frequent bowel movements, and rectal bleeding, and it does not typically present with the specific "abdominal angina" associated with mesenteric ischemia.
Mesenteric ischemia US Medical PG Question 5: A 51-year-old man with a recent diagnosis of peptic ulcer disease currently treated with an oral proton pump inhibitor twice daily presents to the urgent care center complaining of acute abdominal pain which began suddenly less than 2 hours ago. On physical exam, you find his abdomen to be mildly distended, diffusely tender to palpation, and positive for rebound tenderness. Given the following options, what is the next best step in patient management?
- A. Serum gastrin level
- B. Urgent CT abdomen and pelvis (Correct Answer)
- C. H. pylori testing
- D. Abdominal radiographs
- E. Upper endoscopy
Mesenteric ischemia Explanation: ***Urgent CT abdomen and pelvis***
- The sudden onset of severe abdominal pain, diffuse tenderness, and **rebound tenderness** in a patient with a history of peptic ulcer disease (PUD) suggests a **perforated ulcer**, which is a surgical emergency.
- A CT scan is the **most sensitive imaging modality** for detecting **free air** (pneumoperitoneum) and can confirm the diagnosis with >95% sensitivity, helping to localize the perforation and identify complications such as abscess formation.
- CT also helps evaluate alternative diagnoses in the acute abdomen and provides detailed anatomic information for surgical planning.
*Serum gastrin level*
- This test is primarily used in the diagnosis of **Zollinger-Ellison syndrome**, a rare condition characterized by gastrinomas leading to severe, refractory PUD.
- It is not indicated in an acute emergency setting with signs of perforation, as it would delay critical diagnostic imaging and management.
*H. pylori testing*
- **_H. pylori_ infection** is a common cause of PUD, but testing for it is part of routine initial management or follow-up for chronic disease.
- Testing would not address the immediate life-threatening complication of suspected perforation and would delay definitive diagnosis.
*Abdominal radiographs*
- An upright chest X-ray or abdominal radiograph can detect **free air under the diaphragm** in cases of perforation and is a reasonable initial imaging test.
- However, plain radiographs have lower sensitivity (75-80%) compared to CT scan and may miss smaller perforations or provide insufficient information about the location and extent of injury.
- In modern practice with readily available CT, cross-sectional imaging is preferred for its superior diagnostic accuracy in evaluating the acute abdomen.
*Upper endoscopy*
- **Upper endoscopy** is a valuable diagnostic and therapeutic tool for stable PUD but is **absolutely contraindicated** in cases of suspected or confirmed hollow viscus perforation.
- Introducing an endoscope with air insufflation could worsen the perforation and lead to further contamination of the peritoneal cavity, increasing morbidity and mortality.
Mesenteric ischemia US Medical PG Question 6: A 32-year-old man is brought to the emergency department after a skiing accident. The patient had been skiing down the mountain when he collided with another skier who had stopped suddenly in front of him. He is alert but complaining of pain in his chest and abdomen. He has a past medical history of intravenous drug use and peptic ulcer disease. He is a current smoker. His temperature is 97.4°F (36.3°C), blood pressure is 77/53 mmHg, pulse is 127/min, and respirations are 13/min. He has a GCS of 15 and bilateral shallow breath sounds. His abdomen is soft and distended with bruising over the epigastrium. He is moving all four extremities and has scattered lacerations on his face. His skin is cool and delayed capillary refill is present. Two large-bore IVs are placed in his antecubital fossa, and he is given 2L of normal saline. His FAST exam reveals fluid in Morison's pouch. Following the 2L normal saline, his temperature is 97.5°F (36.4°C), blood pressure is 97/62 mmHg, pulse is 115/min, and respirations are 12/min.
Which of the following is the best next step in management?
- A. Diagnostic peritoneal lavage
- B. Emergency laparotomy (Correct Answer)
- C. Upper gastrointestinal endoscopy
- D. Close observation
- E. Diagnostic laparoscopy
Mesenteric ischemia Explanation: ***Emergency laparotomy***
- The patient remains **hemodynamically unstable** (BP 97/62 mmHg, HR 115/min after 2L IV fluids) with evidence of **intra-abdominal fluid on FAST exam** (fluid in Morison's pouch).
- This clinical picture indicates active intra-abdominal hemorrhage requiring **immediate surgical intervention** to identify and control the source of bleeding.
*Diagnostic peritoneal lavage*
- **Diagnostic peritoneal lavage (DPL)** has largely been replaced by the focused abdominal sonography for trauma (FAST) exam and CT scans.
- While it can detect intra-abdominal bleeding, it is **invasive** and would delay definitive treatment in a hemodynamically unstable patient with positive FAST.
*Upper gastrointestinal endoscopy*
- This procedure is primarily for diagnosing and treating **upper gastrointestinal bleeding** or mucosal abnormalities.
- It is **not indicated** for evaluating traumatic intra-abdominal hemorrhage or hemodynamic instability following blunt abdominal trauma.
*Close observation*
- Close observation is appropriate for **hemodynamically stable patients** with blunt abdominal trauma and minor injuries or equivocal findings.
- This patient's persistent hypotension, tachycardia, and positive FAST findings rule out observation as a safe or appropriate next step.
*Diagnostic laparoscopy*
- **Diagnostic laparoscopy** is a minimally invasive surgical procedure used to evaluate the abdominal cavity.
- While it can be diagnostic, it is generally **contraindicated in hemodynamically unstable patients** as it can prolong the time to definitive hemorrhage control if a major injury is found.
Mesenteric ischemia US Medical PG Question 7: A 74-year-old man presents to the emergency department with sudden onset of abdominal pain that is most felt around the umbilicus. The pain began 16 hours ago and has no association with meals. He has not been vomiting, but he has had several episodes of bloody loose bowel movements. He was hospitalized 1 week ago for an acute myocardial infarction. He has had diabetes mellitus for 35 years and hypertension for 20 years. He has smoked 15–20 cigarettes per day for the past 40 years. His temperature is 36.9°C (98.4°F), blood pressure is 95/65 mm Hg, and pulse is 95/min. On physical examination, the patient is in severe pain, there is a mild periumbilical tenderness, and a bruit is heard over the epigastric area. Which of the following is the most likely diagnosis?
- A. Acute mesenteric ischemia (Correct Answer)
- B. Chronic mesenteric ischemia
- C. Colonic ischemia
- D. Irritable bowel syndrome
- E. Peptic ulcer disease
Mesenteric ischemia Explanation: ***Acute mesenteric ischemia***
- The sudden onset of severe, **periumbilical abdominal pain** out of proportion to physical exam findings in a patient with significant **atherosclerotic risk factors** (recent MI, diabetes, hypertension, smoking) is highly suggestive of acute mesenteric ischemia.
- **Bloody loose bowel movements** (due to mucosal sloughing) and the presence of an **epigastric bruit** further support the diagnosis of arterial occlusion to the bowel.
*Chronic mesenteric ischemia*
- This typically presents with **postprandial abdominal pain** (abdominal angina) and **weight loss** due to fear of eating.
- The patient's pain is sudden in onset, not associated with meals, and severe, which is characteristic of acute ischemia.
*Colonic ischemia*
- While it can cause bloody diarrhea, colonic ischemia typically presents with pain localized to the **left or right lower quadrants** and is often less severe than the pain described here.
- The patient's risk factors and abrupt, severe periumbilical pain point away from isolated colonic involvement.
*Irritable bowel syndrome*
- This is a **functional gastrointestinal disorder** characterized by chronic abdominal pain, bloating, and altered bowel habits (constipation, diarrhea, or both).
- It does not present with sudden, severe pain, bloody stools, or in the context of acute cardiovascular events and associated risk factors.
*Peptic ulcer disease*
- This typically causes **epigastric pain** that can be burning or gnawing, often relieved or exacerbated by food, and may cause melena or hematemesis.
- The patient's severe, diffuse periumbilical pain, bloody stools (not melena), and recent MI are not typical for peptic ulcer disease.
Mesenteric ischemia US Medical PG Question 8: A 64-year-old woman has progressively worsening abdominal pain 5 hours after an open valve replacement with cardiopulmonary bypass. The pain is crampy and associated with an urge to defecate. The patient reports having had 2 bloody bowel movements in the last hour. Her operation was complicated by significant intraoperative blood loss, which prolonged the operation and necessitated 2 transfusions of red blood cells. She has hypercholesterolemia and type 2 diabetes mellitus. The patient received prophylactic perioperative antibiotics and opioid pain management during recovery. Her temperature is 37.9°C (98.9°F), pulse is 95/min, and blood pressure is 115/69 mm Hg. Examination shows a soft abdomen with mild tenderness to palpation in the left quadrants but no rebound tenderness or guarding. Bowel sounds are decreased. Rectal examination shows blood on the examining finger. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Embolization of superior mesenteric artery
- B. Atherosclerotic narrowing of the intestinal vessels
- C. Small outpouchings in the sigmoid wall
- D. Infection with Clostridioides difficile
- E. Decreased blood flow to the splenic flexure (Correct Answer)
Mesenteric ischemia Explanation: ***Decreased blood flow to the splenic flexure***
- This patient's symptoms are highly suggestive of **ischemic colitis**, which often affects the **splenic flexure** due to its "watershed" area vulnerability. **Cardiopulmonary bypass** and significant **intraoperative blood loss** (leading to hypotension and hypoperfusion) are major risk factors for this condition.
- The presentation with **crampy abdominal pain**, **urgent defecation**, and **bloody bowel movements** shortly after cardiac surgery points to colonic ischemia.
*Embolization of superior mesenteric artery*
- While an acute **SMA embolism** could cause severe abdominal pain and bloody stools, it typically presents with **more diffuse and severe abdominal tenderness**, often with marked tenderness disproportionate to examination findings early on, and rapid progression to peritonitis.
- The patient's history of valvular disease and hypercholesterolemia increases the risk of embolization, but the **mild tenderness confined to left quadrants** and decreased bowel sounds are less typical of an acute SMA occlusion.
*Atherosclerotic narrowing of the intestinal vessels*
- This describes **chronic mesenteric ischemia**, which typically causes **postprandial abdominal pain** (intestinal angina) and weight loss, not acute abdominal pain and bloody diarrhea in the immediate postoperative period.
- While the patient has risk factors for atherosclerosis (hypercholesterolemia, diabetes), the acute onset of symptoms following cardiac surgery points to an acute ischemic event rather than chronic narrowing.
*Small outpouchings in the sigmoid wall*
- This refers to **diverticulitis** or **diverticular bleeding**. While diverticular bleeding can cause painless or painful bleeding, and diverticulitis can cause abdominal pain, the acute onset post-cardiac surgery in the setting of hypoperfusion makes ischemic colitis a more likely diagnosis.
- Diverticulitis typically presents with **localized left lower quadrant pain**, fever, and leukocytosis, but the systemic context of recent cardiac surgery and hypoperfusion strongly favors ischemia.
*Infection with Clostridioides difficile*
- **_Clostridioides difficile_ infection** typically causes **watery diarrhea**, often after antibiotic use, and usually takes several days to develop symptoms after exposure or antibiotic initiation.
- Although the patient received perioperative antibiotics, the onset of symptoms within hours of surgery and the presence of **frank bloody stools** are less characteristic of _C. difficile_ infection, which is more commonly associated with non-bloody diarrhea.
Mesenteric ischemia US Medical PG Question 9: A 74-year-old man is brought to the emergency department after he had copious amounts of blood-stained stools. Minutes later, he turned sweaty, felt light-headed, and collapsed into his wife’s arms. Upon admission, he is found to have a blood pressure of 78/40 mm Hg, a pulse of 140/min, and oxygen saturation of 98%. His family history is relevant for both gastric and colorectal cancer. His personal history is relevant for hypertension, for which he takes amlodipine. After an initial successful resuscitation with intravenous fluids, which of the following should be the first step in approaching this case?
- A. Radionuclide imaging
- B. Mesenteric angiography
- C. Upper endoscopy (Correct Answer)
- D. Colonoscopy
- E. Nasogastric lavage
Mesenteric ischemia Explanation: ***Upper endoscopy***
- After **initial hemodynamic stabilization** (as stated in the question), **early upper endoscopy** is the recommended first-line approach for patients with acute GI bleeding.
- **Upper GI sources** must be ruled out first, even in patients presenting with hematochezia (blood-stained stools), as **10-15% of cases** with bright red blood per rectum originate from an upper GI source.
- Upper endoscopy is both **diagnostic and therapeutic**, allowing for immediate intervention (banding, sclerotherapy, thermal coagulation, clipping) if a bleeding source is identified.
- **Current ACG/ASGE guidelines** recommend endoscopy **within 24 hours** (ideally within 12 hours) after resuscitation in patients with acute upper GI bleeding.
- The degree of **hemodynamic instability** in this patient (BP 78/40, HR 140) suggests a brisk bleed more consistent with an upper GI source.
*Nasogastric lavage*
- NG lavage has **low sensitivity (42-84%)** for upper GI bleeding and can miss up to 15% of cases.
- It is **no longer routinely recommended** by current guidelines as it delays definitive diagnosis and treatment without providing therapeutic benefit.
- Modern practice favors proceeding directly to endoscopy after stabilization rather than performing NG lavage first.
*Radionuclide imaging*
- **Tagged RBC scan** is useful for **intermittent or slow bleeding** (0.1-0.5 mL/min) when endoscopy is non-diagnostic.
- Not appropriate as the **first step** in an acute, massive bleed requiring immediate source localization and potential intervention.
- Provides localization but no therapeutic capability.
*Mesenteric angiography*
- Indicated for **active, brisk bleeding** (>0.5-1 mL/min) when endoscopy fails to identify the source or when immediate therapeutic embolization is needed.
- Can be both diagnostic and therapeutic but is typically a **second-line intervention** after endoscopy.
- Requires active bleeding at the time of the procedure to visualize the source.
*Colonoscopy*
- **Colonoscopy** is the appropriate diagnostic tool for **lower GI bleeding** after upper GI sources have been excluded.
- Should be performed **after upper endoscopy** rules out an upper source, particularly in patients with this degree of hemodynamic compromise.
- Requires adequate bowel preparation for optimal visualization, which may delay diagnosis.
Mesenteric ischemia US Medical PG Question 10: A newborn boy born vaginally to a healthy 37-year-old G3P1 from a pregnancy complicated by hydramnios fails to pass meconium after 24 hours of life. The vital signs are within normal limits for his age. The abdomen is distended, the anus is patent, and the rectal examination reveals pale mucous with non-pigmented meconium. Based on a barium enema, the boy is diagnosed with sigmoid colonic atresia. Disruption of which structure during fetal development could lead to this anomaly?
- A. Inferior mesenteric artery (Correct Answer)
- B. Superior mesenteric artery
- C. Vitelline duct
- D. Cloaca
- E. Celiac artery
Mesenteric ischemia Explanation: ***Inferior mesenteric artery***
- **Sigmoid colonic atresia**, as observed in this case, results from an ischemic event affecting the segment of the bowel supplied by the **inferior mesenteric artery** during fetal development.
- Interruption of blood flow to this region can lead to subsequent **atresia** as the affected part of the intestine necroses and is reabsorbed.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies the midgut structures, including the small intestine and parts of the large intestine up to the transverse colon.
- Disruption of the superior mesenteric artery would typically lead to atresias higher up in the **gastrointestinal tract**, such as jejunal or ileal atresias, not sigmoid colonic atresia.
*Vitelline duct*
- The **vitelline duct** (also known as the omphalomesenteric duct) connects the midgut to the yolk sac during early fetal development.
- Persistent patency or partial obliteration of the vitelline duct can lead to anomalies like **Meckel's diverticulum** or vitelline cysts, which are distinct from colonic atresia.
*Cloaca*
- The **cloaca** is a common cavity for the digestive, urinary, and reproductive tracts during early embryonic development.
- Defects in cloacal development lead to complex malformations involving these systems, such as **imperforate anus** or persistent cloaca, rather than isolated colonic atresia with a patent anus.
*Celiac artery*
- The **celiac artery** supplies the foregut structures, including the stomach, duodenum, liver, and spleen.
- Disruption of the celiac artery during fetal development would result in malformations of these upper gastrointestinal organs, not the sigmoid colon.
More Mesenteric ischemia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.