Large bowel obstruction US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Large bowel obstruction. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
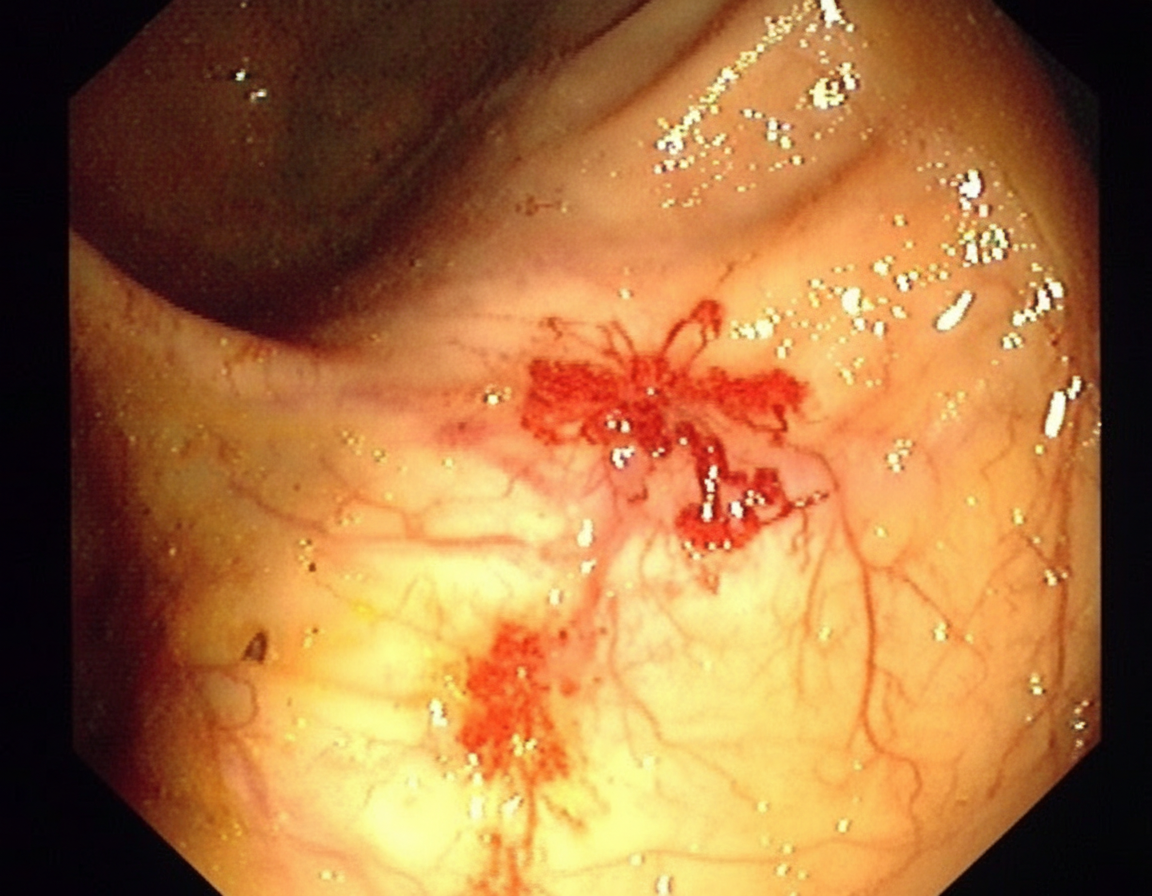
Large bowel obstruction US Medical PG Question 1: A 70-year-old man comes to the clinic for generalized fatigue. He says that he is more tired than before and has difficulty catching his breath while walking upstairs. He feels tired quickly doing his usual activity such as gardening and shopping. He does not have any symptoms of fever, change in bowel habits, abdominal pain, rectal bleeding, or weight loss. His appetite is normal. His last colonoscopy was done 10 years ago and it was normal. His blood pressure is 116/74 and heart rate is 87/min. On physical examination, his conjunctivae are pale. A routine blood test shows iron deficiency anemia with hemoglobin of 10 gm/dL. His stool is positive for occult blood. He is then sent for a colonoscopy (image is shown). What is the most likely diagnosis for the above condition?
- A. Colon cancer
- B. Angiodysplasia (Correct Answer)
- C. Intestinal obstruction
- D. Hereditary hemorrhagic telangiectasia
- E. Diverticulitis
Large bowel obstruction Explanation: ***Angiodysplasia***
- The patient's presentation with **iron deficiency anemia**, **generalized fatigue**, **dyspnea on exertion**, and **positive fecal occult blood** in an elderly individual is highly suggestive of chronic gastrointestinal blood loss. The colonoscopy image would likely show the characteristic vascular malformations of angiodysplasia.
- **Angiodysplasia** is a common cause of GI bleeding in the elderly, often occurring in the **right colon**. These lesions are fragile and prone to intermittent, painless bleeding leading to iron deficiency anemia.
*Colon cancer*
- While **colon cancer** can cause iron deficiency anemia and positive fecal occult blood, the patient's lack of other alarm symptoms such as **weight loss**, **change in bowel habits**, or **abdominal pain** makes it less likely, especially with a normal colonoscopy 10 years prior (though a new lesion is possible).
- The colonoscopy image would typically show a **polypoid mass** or ulcerated lesion, not the distinct vascular malformations characteristic of angiodysplasia.
*Intestinal obstruction*
- **Intestinal obstruction** would primarily present with symptoms like **nausea**, **vomiting**, **abdominal distension**, and **constipation**, which are not reported by the patient.
- It is not a direct cause of **chronic GI blood loss** leading to iron deficiency anemia, although some causes of obstruction (like a tumor) could also bleed.
*Hereditary hemorrhagic telangiectasia*
- **Hereditary hemorrhagic telangiectasia (HHT)**, or **Osler-Weber-Rendu syndrome**, is characterized by widespread **mucocutaneous telangiectasias** and recurrent bleeding from various sites, including the GI tract.
- However, HHT is a genetic disorder usually presenting with symptoms **earlier in life** and affecting multiple organs; there are no signs of other affected systems or mucocutaneous lesions mentioned.
*Diverticulitis*
- **Diverticulitis** typically presents with acute **left lower quadrant abdominal pain**, **fever**, and changes in bowel habits, which are absent in this patient.
- While **diverticulosis** (the presence of diverticula) can cause significant GI bleeding, **diverticulitis** refers to inflammation or infection of the diverticula, not directly chronic, occult bleeding leading to anemia in this context without other symptoms.
Large bowel obstruction US Medical PG Question 2: A 60-year-old patient presents to the urgent care clinic with complaints of pain and abdominal distention for the past several weeks. The pain began with a change in bowel habits 3 months ago, and he gradually defecated less until he became completely constipated, which led to increasing pain and distention. He also mentions that he has lost weight during this period, even though he has not changed his diet. When asked about his family history, the patient reveals that his brother was diagnosed with colorectal cancer at 65 years of age. An abdominal radiograph and CT scan were done which confirmed the diagnosis of obstruction. Which of the following locations in the digestive tract are most likely involved in this patient’s disease process?
- A. Small bowel
- B. Ascending colon
- C. Rectum
- D. Sigmoid colon (Correct Answer)
- E. Cecum
Large bowel obstruction Explanation: ***Sigmoid colon***
- This patient's symptoms—**progressive constipation, abdominal distention, weight loss**, and a family history of colorectal cancer—strongly suggest a **colorectal malignancy** causing obstruction.
- The **sigmoid colon** is the most common site for colorectal cancer, especially those presenting with obstructive symptoms due to its narrower lumen compared to the proximal colon.
*Small bowel*
- While small bowel obstruction can cause similar symptoms, **primary small bowel cancers are rare** and typically present differently, often with episodes of partial obstruction.
- The history of a **change in bowel habits preceding complete constipation** is more indicative of a colonic mass.
*Ascending colon*
- Cancers in the **right colon (ascending and cecum)** tend to present with symptoms like **iron deficiency anemia, fatigue, and occult bleeding**, rather than obstruction, due to its wider lumen and more fluid stool.
- **Obstruction is less common** as an initial presentation in this location.
*Rectum*
- Rectal cancers often cause **changes in bowel habits, tenesmus, and hematochezia** (bright red blood per rectum).
- While obstruction can occur, the sigmoid colon is a more frequent site for tumors causing **progressive obstructive symptoms** as described.
*Cecum*
- Similar to the ascending colon, cancers in the **cecum** are more likely to present with **anemia and vague abdominal discomfort** rather than overt obstruction.
- The **wider diameter** of the cecum allows tumors to grow quite large before causing obstructive symptoms.
Large bowel obstruction US Medical PG Question 3: A 68-year-old woman is brought to the emergency department with intense abdominal pain for the past 2 hours. She has had 1 episode of bloody diarrhea recently. She has an 18-year history of diabetes mellitus. She was diagnosed with hypertension and ischemic heart disease 6 years ago. She is fully alert and oriented. Her temperature is 37.5°C (99.5°F), blood pressure is 145/90 mm Hg, pulse is 78/min, and respirations are 14/min. Abdominal examination shows mild generalized abdominal tenderness without guarding or rebound tenderness. An abdominal plain X-ray shows no abnormalities. Abdominal CT reveals colonic wall thickening and pericolonic fat stranding in the splenic curvature. Bowel rest, intravenous hydration, and IV antibiotics are initiated. Which of the following is the most important diagnostic evaluation at this time?
- A. Angiography
- B. Gastrografin-enhanced X-ray
- C. Laparotomy
- D. Inpatient observation
- E. Sigmoidoscopy (Correct Answer)
Large bowel obstruction Explanation: ***Sigmoidoscopy***
- The patient's presentation with acute abdominal pain, bloody diarrhea, history of cardiovascular disease, and CT findings consistent with **colonic wall thickening** and **pericolonic fat stranding** strongly suggests **ischemic colitis**.
- **Flexible sigmoidoscopy** allows for direct visualization of the colonic mucosa to confirm the diagnosis, assess the extent and severity of ischemia, and rule out other causes of colitis, such as inflammatory bowel disease or infection.
*Angiography*
- While angiography can identify mesenteric arterial occlusion, it is generally reserved for cases of acute mesenteric ischemia involving the superior mesenteric artery, which typically presents with more severe pain out of proportion to physical exam findings and less clear CT findings of colitis.
- In cases of ischemic colitis, where the primary concern is mucosal ischemia rather than immediate large vessel occlusion, angiography is usually not the first-line diagnostic.
*Gastrografin-enhanced X-ray*
- This study (also known as a **Gastrografin swallow or enema**) is primarily used to evaluate for **perforations** or **obstructions**, or to assess lumen integrity.
- It does not provide the mucosal detail necessary to diagnose or assess the severity of **ischemic colitis**, and the contrast agent itself could potentially exacerbate an inflamed bowel.
*Laparotomy*
- **Laparotomy** (surgical exploration) is an invasive procedure reserved for cases with signs of peritonitis, bowel perforation, or severe, unresponsive ischemia requiring surgical intervention.
- Given the patient's stable vital signs, mild tenderness, and lack of guarding or rebound, immediate surgical exploration is not warranted without further diagnostic steps.
*Inpatient observation*
- While inpatient observation is part of the initial management (bowel rest, IV fluids, antibiotics), it is not a **diagnostic evaluation** itself.
- The question asks for the most important diagnostic evaluation to determine the underlying cause and guide further management.
Large bowel obstruction US Medical PG Question 4: A 47-year-old woman presents to the emergency department with abdominal pain. The patient states that she felt this pain come on during dinner last night. Since then, she has felt bloated, constipated, and has been vomiting. Her current medications include metformin, insulin, levothyroxine, and ibuprofen. Her temperature is 99.0°F (37.2°C), blood pressure is 139/79 mmHg, pulse is 95/min, respirations are 12/min, and oxygen saturation is 98% on room air. On physical exam, the patient appears uncomfortable. Abdominal exam is notable for hypoactive bowel sounds, abdominal distension, and diffuse tenderness in all four quadrants. Cardiac and pulmonary exams are within normal limits. Which of the following is the best next step in management?
- A. Metoclopramide
- B. Nasogastric tube, NPO, and IV fluids (Correct Answer)
- C. Stool guaiac
- D. Emergency surgery
- E. IV antibiotics and steroids
Large bowel obstruction Explanation: ***Nasogastric tube, NPO, and IV fluids***
- The patient's symptoms (abdominal pain, bloating, constipation, vomiting, distension, and hypoactive bowel sounds) are highly suggestive of a **bowel obstruction**.
- **Nasogastric tube decompression** relieves pressure, **NPO status** prevents further bowel distension, and **intravenous fluids** address dehydration and electrolyte imbalances, stabilizing the patient for further evaluation.
*Metoclopramide*
- This is a **prokinetic agent** that increases gastrointestinal motility.
- Using it in the context of a suspected bowel obstruction could worsen the condition by increasing pressure against the obstruction and potentially leading to **perforation**.
*Stool guaiac*
- A stool guaiac test detects the presence of **occult blood in the stool**, which is useful for evaluating gastrointestinal bleeding.
- While it can be part of a complete workup, it is not the immediate priority for a patient presenting with symptoms of **acute bowel obstruction** requiring stabilization.
*Emergency surgery*
- While surgery may ultimately be required for a bowel obstruction, it is not the immediate first step unless there are clear signs of **perforation**, **ischemia**, or **strangulation**, which are not specified here.
- Initial management involves **stabilization** with NG decompression, NPO, and IV fluids.
*IV antibiotics and steroids*
- **IV antibiotics** are indicated for suspected infection (e.g., appendicitis, diverticulitis with perforation), but the primary presentation here is mechanical obstruction, not infection.
- **Steroids** are typically used for inflammatory conditions or adrenal insufficiency, neither of which is indicated given the patient's symptoms.
Large bowel obstruction US Medical PG Question 5: An 82-year-old woman presents with 2 months of foul-smelling, greasy diarrhea. She says that she also has felt very tired recently and has had some associated bloating and flatus. She denies any recent abdominal pain, nausea, melena, hematochezia, or vomiting. She also denies any history of recent travel and states that her home has city water. Which of the following tests would be most appropriate to initially work up the most likely diagnosis in this patient?
- A. Fecal fat test (Correct Answer)
- B. Tissue transglutaminase antibody test
- C. Stool O&P
- D. Stool guaiac test
- E. CT of the abdomen with oral contrast
Large bowel obstruction Explanation: ***Fecal fat test***
- The patient's symptoms of **foul-smelling, greasy diarrhea**, along with **fatigue, bloating, and flatus**, strongly suggest **malabsorption**, specifically **steatorrhea** (excess fat in stool).
- A **fecal fat test** (e.g., Sudan stain or 72-hour quantitative stool fat collection) directly assesses fat malabsorption and would be the most appropriate initial diagnostic test.
*Tissue transglutaminase antibody test*
- This test is used to screen for **celiac disease**, which can cause malabsorption symptoms.
- While celiac disease is a possibility, a fecal fat test is a more general and appropriate initial step to confirm fat malabsorption before looking for specific causes.
*Stool O&P*
- Stands for **Stool Ova and Parasites**, used to detect parasitic infections like **Giardia** or **Cryptosporidium**, which can cause diarrhea.
- However, the absence of recent travel, city water, and the prominent greasy nature of the stool make this less likely as the primary initial investigation compared to confirming malabsorption.
*Stool guaiac test*
- This test detects **occult blood in stool**.
- The patient denies **melena or hematochezia**, and there are no signs pointing to gastrointestinal bleeding, making this test irrelevant for her presenting symptoms.
*CT of the abdomen with oral contrast*
- A CT scan with contrast might be used to investigate structural abnormalities or inflammation if other tests confirm malabsorption or point to a specific organ pathology (e.g., pancreatitis, Crohn's disease).
- It's an imaging study and generally not the most appropriate *initial* test for evaluating the described symptoms of malabsorption.
Large bowel obstruction US Medical PG Question 6: A 5-year-old girl is brought to a medical office for evaluation of persistent abdominal pain that has worsened over the past 24 hours. The mother states that the girl often has constipation which has worsened over the last 3 days. The mother denies that the girl has had bloody stools. The girl has not had a bowel movement or passed flatulence in 72 hours. She has vomited 3 times since last night and refuses to eat. She has no significant medical history, including no history of surgeries. On exam, there are no abdominal masses; however, the upper abdomen is distended and tympanic. What is the most likely underlying cause of the girl’s symptoms?
- A. Duodenal atresia
- B. Malrotation of the gut (Correct Answer)
- C. Pyloric stenosis
- D. Meckel’s diverticulum
- E. Volvulus
Large bowel obstruction Explanation: ***Malrotation of the gut***
- The question asks for the **underlying cause** of symptoms in a 5-year-old presenting with her **first episode** of acute bowel obstruction and **no prior surgical history**. **Malrotation** is the congenital anatomical abnormality that predisposes to **midgut volvulus**.
- **Malrotation** occurs when the bowel fails to rotate properly during fetal development, leaving the mesentery on a narrow pedicle. This anatomical defect is the underlying cause that makes volvulus possible.
- While volvulus (twisting) is the acute mechanical event causing obstruction, **malrotation is the underlying anatomical defect** being asked for in the question.
- The presentation of **abdominal pain**, **vomiting**, **abdominal distension**, inability to pass **flatus or stool** for 72 hours, and **tympanic upper abdomen** indicates acute bowel obstruction from midgut volvulus occurring on the background of malrotation.
*Volvulus*
- **Volvulus** (twisting of the bowel) is the **acute complication** that occurs, not the underlying cause.
- Volvulus is the mechanism of obstruction, but it occurs because of the underlying anatomical defect (malrotation).
- The question specifically asks for "underlying cause" - volvulus is the acute event, while malrotation is the predisposing anatomical abnormality.
*Duodenal atresia*
- **Duodenal atresia** is a congenital complete obstruction that presents in the **neonatal period** with vomiting (bilious), the classic "double bubble" sign, and feeding intolerance.
- This would have been diagnosed much earlier than 5 years of age and is not compatible with this presentation.
*Pyloric stenosis*
- **Pyloric stenosis** presents with **non-bilious projectile vomiting** in infants between **2 to 6 weeks of age**, not in a 5-year-old child.
- Physical exam classically reveals an **olive-shaped mass** in the epigastrium and visible gastric peristaltic waves.
*Meckel's diverticulum*
- **Meckel's diverticulum** most commonly presents with **painless rectal bleeding** (from ectopic gastric mucosa causing ulceration) following the "rule of 2s."
- While it can cause obstruction via intussusception or serve as a lead point, it is not the most likely underlying cause of this presentation in a 5-year-old with acute complete bowel obstruction and no prior symptoms.
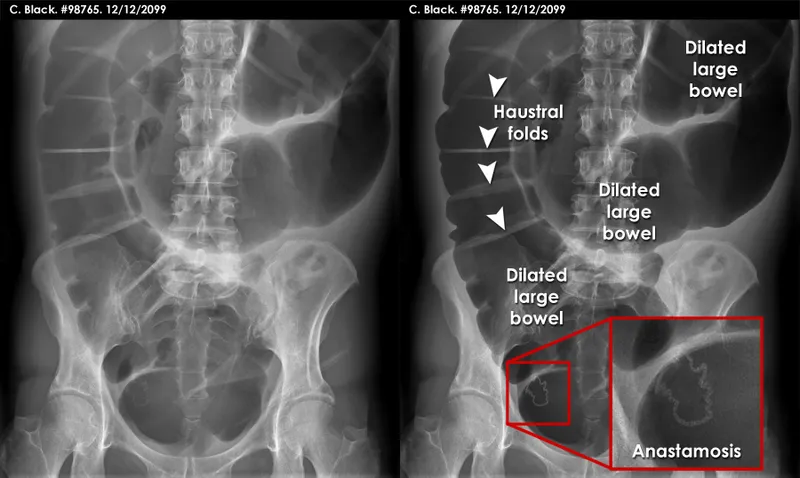
Large bowel obstruction US Medical PG Question 7: An institutionalized 65-year-old man is brought to the emergency department because of abdominal pain and distension for 12 hours. The pain was acute in onset and is a cramping-type pain associated with nausea, vomiting, and constipation. He has a history of chronic constipation and has used laxatives for years. There is no history of inflammatory bowel disease in his family. He has not been hospitalized recently. There is no recent history of weight loss or change in bowel habits. On physical examination, the patient appears ill. The abdomen is distended with tenderness mainly in the left lower quadrant and is tympanic on percussion. The blood pressure is 110/79 mm Hg, heart rate is 100/min, the respiratory rate is 20/min, and the temperature is 37.2°C (99.0°F). The CBC shows an elevated white blood cell count. The plain abdominal X-ray is shown in the accompanying image. What is the most likely cause of his condition?
- A. Sigmoid volvulus (Correct Answer)
- B. Intussusception
- C. Acute diverticulitis
- D. Toxic megacolon
- E. Colon cancer
Large bowel obstruction Explanation: ***Sigmoid volvulus***
- The patient’s symptoms of acute **abdominal pain**, distension, and cramping strongly indicate **sigmoid volvulus**, often seen in chronic constipation and institutionalized patients.
- Physical examination revealing **tenderness in the left lower quadrant** and a tympanic abdomen supports the diagnosis of bowel obstruction typically caused by **volvulus**.
*Intussusception*
- Generally presents with **currant jelly stools** and is more common in children; the acute symptoms here are less typical.
- It often involves a **lead point** or associated conditions like **polyps** or tumors, which are not indicated in this case.
*Acute diverticulitis*
- Usually associated with **localized pain** in the left lower quadrant but would present with fever and changes in bowel habits, which the patient lacks.
- Typically shows **peritoneal signs** and may have complications like abscess or perforation, not indicated here.
*Toxic megacolon*
- Commonly associated with underlying **inflammatory bowel disease** or infections, not indicated in this patient with no recent history of **IBD**.
- Symptoms would include severe **diarrhea** and abdominal pain, which do not fit the current acute cramping and constipation pattern.
*Colon cancer*
- While it can cause abdominal symptoms, it presents more insidiously with **weight loss** or **change in bowel habits**, none of which are reported here.
- The acute presentation and findings do not align with a malignancy, which would often be chronic in nature.
Large bowel obstruction US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Large bowel obstruction Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Large bowel obstruction US Medical PG Question 9: A 75-year-old man is brought to the emergency department after 2 days of severe diffuse abdominal pain, nausea, vomiting, and lack of bowel movements, which has led him to stop eating. He has a history of type-2 diabetes mellitus, hypertension, and chronic obstructive pulmonary disease. Upon admission, his vital signs are within normal limits and physical examination shows diffuse abdominal tenderness, distention, lack of bowel sounds, and an empty rectal ampulla. After initial fluid therapy and correction of moderate hypokalemia, the patient's condition shows mild improvement. His abdominal plain film is taken and shown. Which of the following is the most appropriate concomitant approach?
- A. Exploratory surgery
- B. Initiate pain management with morphine
- C. Initiate intravenous metoclopramide
- D. Gastrografin enema
- E. Nasogastric decompression (Correct Answer)
Large bowel obstruction Explanation: ***Nasogastric decompression***
- The patient exhibits symptoms consistent with **bowel obstruction** (diffuse abdominal pain, distention, absent bowel sounds, empty rectal ampulla), which can lead to significant fluid and gas accumulation. **Nasogastric decompression** is crucial to relieve pressure, prevent aspiration, and stabilize the patient.
- This intervention helps manage symptoms, reduces the risk of complications, and provides time for further diagnostic workup while addressing fluid and electrolyte imbalances.
*Exploratory surgery*
- While surgery may be indicated for complete bowel obstruction, it is usually reserved for cases that fail conservative management or show signs of **strangulation** or **perforation**.
- Without evidence of these acute complications and given the patient's mild improvement after initial therapy, immediate surgery is not the most appropriate first step.
*Initiate pain management with morphine*
- While pain management is important, **opioids** like morphine can actually **reduce bowel motility** and worsen a bowel obstruction.
- Addressing the underlying obstruction through decompression should be prioritized before initiating pain medication that could exacerbate the condition.
*Initiate intravenous metoclopramide*
- **Metoclopramide** is a **prokinetic agent** that increases gastrointestinal motility.
- In a suspected bowel obstruction, stimulating motility can increase intraluminal pressure and potentially worsen the condition or increase the risk of perforation, making it contraindicated.
*Gastrografin enema*
- A **Gastrografin enema** is typically used to diagnose and sometimes treat **distal colonic obstructions**, or as a therapeutic trial for **meconium ileus** in infants.
- Given the diffuse abdominal pain and an empty rectal ampulla suggesting a more proximal or severe obstruction, an enema may not be appropriate and could even be dangerous if there's a risk of perforation.
Large bowel obstruction US Medical PG Question 10: A 55-year-old man presents to the emergency department with nausea and vomiting. The patient states that he has felt nauseous for the past week and began vomiting last night. He thought his symptoms would resolve but decided to come in when his symptoms worsened. He feels that his symptoms are exacerbated with large fatty meals and when he drinks alcohol. His wife recently returned from a cruise with symptoms of vomiting and diarrhea. The patient has a past medical history of poorly managed diabetes, constipation, anxiety, dyslipidemia, and hypertension. His temperature is 99.5°F (37.5°C), blood pressure is 197/128 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 95% on room air. Physical exam reveals a systolic murmur heard loudest along the left upper sternal border. Abdominal exam reveals an obese, tympanitic and distended abdomen with a 3 cm scar in the right lower quadrant. Vascular exam reveals weak pulses in the lower extremities. Which of the following is the most likely diagnosis?
- A. Enteric nervous system damage
- B. Twisting of the bowel
- C. Adhesions (Correct Answer)
- D. Norovirus
- E. Impacted stool
Large bowel obstruction Explanation: ***Adhesions***
- The patient's history of a 3 cm scar in the right lower quadrant suggests a prior abdominal surgery, which is the most common cause of **intra-abdominal adhesions**.
- **Adhesions** can lead to **small bowel obstruction**, causing symptoms like nausea, vomiting, abdominal distension, and tympany, which are all present in this patient.
*Enteric nervous system damage*
- Poorly managed diabetes can cause **diabetic gastroparesis**, which involves damage to the **enteric nervous system** leading to delayed gastric emptying.
- While it can cause nausea and vomiting, it doesn't typically present with significant abdominal distension or tympany, which are indicative of a mechanical obstruction.
*Twisting of the bowel*
- **Volvulus**, or twisting of the bowel, causes acute abdominal pain, distension, and often complete obstruction.
- While it's a possibility for bowel obstruction, the presence of a surgical scar and gradual worsening of symptoms over a week makes **adhesions** a more likely cause in this scenario.
*Norovirus*
- **Norovirus** is a common cause of acute gastroenteritis, characterized by abrupt onset of vomiting and diarrhea, often with a rapid resolution.
- Although his wife has similar symptoms, the patient's symptoms have been ongoing for a week, are exacerbated by fatty meals, and include abdominal distension, which is inconsistent with typical norovirus infection.
*Impacted stool*
- **Fecal impaction** can cause constipation, abdominal pain, and sometimes paradoxical diarrhea.
- While the patient has a history of constipation, the significant **tympanic distension** and persistent vomiting suggest a mechanical obstruction rather than just impacted stool.
More Large bowel obstruction US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.