Diverticulitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diverticulitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diverticulitis US Medical PG Question 1: A 46-year-old woman comes to the emergency department because of intermittent abdominal pain and vomiting for 2 days. The abdominal pain is colicky and diffuse. The patient's last bowel movement was 3 days ago. She has had multiple episodes of upper abdominal pain that radiates to her scapulae and vomiting over the past 3 months; her symptoms subsided after taking ibuprofen. She has coronary artery disease, type 2 diabetes mellitus, gastroesophageal reflux disease, and osteoarthritis of both knees. Current medications include aspirin, atorvastatin, rabeprazole, insulin, and ibuprofen. She appears uncomfortable. Her temperature is 39°C (102.2°F), pulse is 111/min, and blood pressure is 108/68 mm Hg. Examination shows dry mucous membranes. The abdomen is distended and tympanitic with diffuse tenderness; bowel sounds are high-pitched. Rectal examination shows a collapsed rectum. Her hemoglobin concentration is 13.8 g/dL, leukocyte count is 14,400/mm3, and platelet count is 312,000/mm3. An x-ray of the abdomen is shown. Which of the following is the most likely cause of this patient's findings?
- A. Cecal torsion
- B. Viscus perforation
- C. Colonic diverticular inflammation
- D. Cholecystoenteric fistula (Correct Answer)
- E. Bowel infarction
Diverticulitis Explanation: ***Cholecystoenteric fistula***
- The patient's history of recurrent upper abdominal pain radiating to the scapula, responsive to NSAIDs, is highly suggestive of **biliary colic** due to **cholelithiasis**.
- The diffuse colicky pain, vomiting, distended abdomen with high-pitched bowel sounds, and particularly the **pneumobilia** (air in the biliary tree, visible as branching lucency in the hepatic area on X-ray, indicated by red arrows) along with signs of **small bowel obstruction** (dilated small bowel loops and air-fluid levels, indicated by green arrows), are classic features of **gallstone ileus** resulting from a cholecystoenteric fistula.
*Cecal torsion*
- While cecal torsion can cause a large bowel obstruction with colicky pain and distension, it typically presents with a **dilated cecum** and a characteristic "coffee-bean" appearance on X-ray, often without pneumobilia.
- The history of recurrent biliary pain and the presence of pneumobilia are not typical for cecal torsion.
*Viscus perforation*
- A viscus perforation would likely cause **sudden, severe onset abdominal pain**, signs of peritonitis, and usually **free air under the diaphragm** on an upright chest X-ray.
- While the patient has diffuse tenderness, the X-ray findings do not show free intraperitoneal air; instead, they show pneumobilia and small bowel obstruction.
*Colonic diverticuli inflammation*
- **Diverticulitis** typically presents with **left lower quadrant pain**, fever, and changes in bowel habits, though diffuse pain can occur with complications.
- It does not explain the history of recurrent upper abdominal pain radiating to the scapula or the radiologic findings of pneumobilia and small bowel obstruction.
*Bowel infarction*
- Bowel infarction often presents with **severe, disproportionate abdominal pain** (pain out of proportion to exam findings), bloody diarrhea, and signs of sepsis.
- While the patient has some signs of systemic inflammation (fever, leukocytosis), the X-ray findings of pneumobilia and typical small bowel obstruction, without signs of portal venous gas or extensive bowel wall thickening, make infarction less likely as the primary cause.
Diverticulitis US Medical PG Question 2: A 3-day-old newborn is brought to the physician because of abdominal distention, inconsolable crying, and 3 episodes of bilious vomiting since the previous evening. He was delivered at home at 40 weeks' gestation by a trained midwife. He has not passed meconium. Physical examination shows abdominal distention, a tight anal sphincter, and an explosive passage of air and feces on removal of the examining finger. Abnormal development of which of the following best explains this patient's condition?
- A. Submucosa and muscularis externa (Correct Answer)
- B. Epithelium and submucosa
- C. Muscularis mucosae and lamina propria
- D. Muscularis mucosae and serosa
- E. Epithelium and lamina propria
Diverticulitis Explanation: ***Submucosa and muscularis externa***
- This patient's symptoms (abdominal distention, bilious vomiting, failure to pass meconium, tight anal sphincter with explosive stool passage) are classic for **Hirschsprung disease**.
- Hirschsprung disease is characterized by the absence of **ganglion cells** in the myenteric (Auerbach's) plexus (located between the inner circular and outer longitudinal layers of the muscularis externa) and the submucosal (Meissner's) plexus (located in the submucosa) of the distal colon.
*Epithelium and submucosa*
- The **epithelium** is involved in absorption and secretion, and its primary dysfunction would typically lead to diarrhea or malabsorption, not an obstructive picture like this.
- While the submucosa contains Meissner's plexus, the lack of ganglion cells in the muscularis externa's Auerbach's plexus is equally crucial to the pathophysiology of Hirschsprung disease.
*Muscularis mucosae and lamina propria*
- The **muscularis mucosae** is a thin layer that causes folding of the mucosa, while the **lamina propria** is connective tissue supporting the epithelium; neither is directly implicated in the primary pathology of Hirschsprung disease which involves neural crest cell migration.
- Absence of ganglion cells in these layers would not explain the severe motility disorder observed in Hirschsprung disease involving the entire bowel wall.
*Muscularis mucosae and serosa*
- The **serosa** is the outermost connective tissue layer and is not directly involved in the intrinsic innervation or motility problems seen in Hirschsprung disease.
- Dysfunction of the muscularis mucosae alone would not result in the functional obstruction due to absent peristalsis.
*Epithelium and lamina propria*
- The **epithelium** and **lamina propria** are primarily involved in the digestive and absorptive functions of the gut, and their abnormal development would not typically cause the characteristic features of Hirschsprung disease, which is a neurodevelopmental disorder of the gut.
- The core issue in Hirschsprung disease lies in the neural plexuses controlling motility, not the mucosal lining.
Diverticulitis US Medical PG Question 3: A 68-year-old man presents to the emergency department with left lower quadrant abdominal pain and fever for 1 day. He states during this time frame he has had weight loss and a decreased appetite. The patient had surgery for a ruptured Achilles tendon 1 month ago and is still recovering but is otherwise generally healthy. His temperature is 102°F (38.9°C), blood pressure is 154/94 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam is remarkable for an uncomfortable and thin man with left lower quadrant abdominal tenderness without rebound findings. Fecal occult test for blood is positive. Laboratory studies are ordered as seen below.
Hemoglobin: 10 g/dL
Hematocrit: 30%
Leukocyte count: 3,500/mm^3 with normal differential
Platelet count: 157,000/mm^3
Which of the following is the most appropriate next step in management?
- A. Ceftriaxone and metronidazole
- B. Ciprofloxacin and metronidazole
- C. Colonoscopy
- D. CT abdomen (Correct Answer)
- E. MRI abdomen
Diverticulitis Explanation: ***CT abdomen***
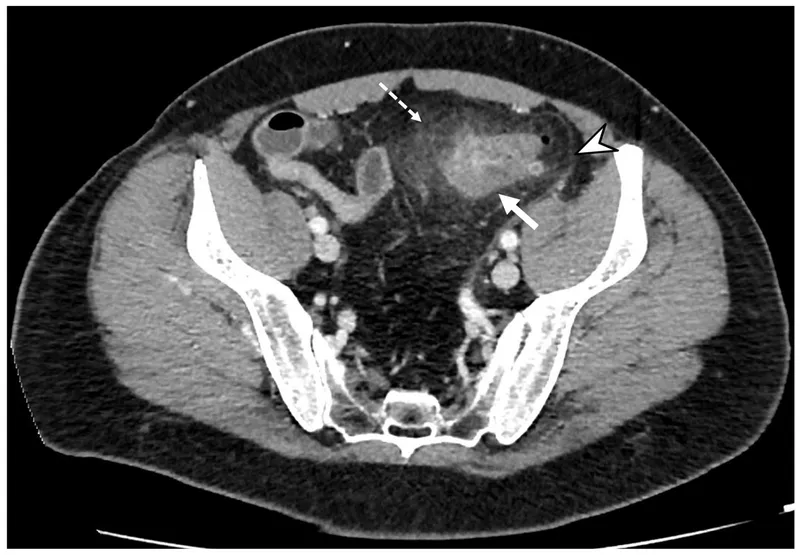
- A **CT scan of the abdomen and pelvis** is the most appropriate initial diagnostic step for acute left lower quadrant pain with fever, leukopenia, and a positive fecal occult blood test, as it can efficiently evaluate for **diverticulitis**, bowel perforation, or **colonic malignancy**.
- The patient's presentation with constitutional symptoms like **weight loss and decreased appetite** in an older male, along with signs of anemia and occult blood, raises concern for **colorectal cancer**, making imaging a critical next step to differentiate potential etiologies.
*Ceftriaxone and metronidazole*
- While this is a common antibiotic regimen for suspected **diverticulitis**, it should not be initiated without definitive imaging, especially given the patient's concerning systemic symptoms and signs of **anemia and occult bleeding**, which could indicate a more serious underlying condition.
- Empirical antibiotic therapy without a clear diagnosis could delay the identification of conditions like **colorectal cancer** or abscess, which require different management strategies.
*Ciprofloxacin and metronidazole*
- This is also a typical antibiotic combination for uncomplicated **diverticulitis**; however, giving antibiotics without confirmation of the diagnosis via imaging is inappropriate in this case due to the patient's **systemic symptoms** and signs of **GI bleeding**.
- Without imaging to rule out intestinal perforation or malignancy, starting antibiotics could mask symptoms or delay crucial diagnostic and therapeutic interventions.
*Colonoscopy*
- A **colonoscopy** is indicated to investigate the **positive fecal occult blood** and rule out colorectal malignancy, but it is generally *contraindicated* in the acute setting of suspected diverticulitis due to the risk of **perforation**.
- Imaging (like CT) should always precede colonoscopy when acute abdominal pain and inflammation are present to assess for safety and guide the timing of endoscopy.
*MRI abdomen*
- While **MRI provides excellent soft tissue delineation**, it is typically not the first-line imaging modality for acute abdominal pain presentations in the emergency department.
- **CT scans are faster, more readily available**, and provide comprehensive imaging of the bowel, mesentery, and surrounding structures, making them superior for initial evaluation of acute abdominal conditions like diverticulitis or perforation.
Diverticulitis US Medical PG Question 4: A 70-year-old man with a history of chronic constipation presents to the emergency department with a two-day history of left lower quadrant abdominal pain. He is found to have a temperature of 100.8F, BP 140/90, HR 85, and RR 16. On physical examination, he is tender to light palpation in the left lower quadrant and exhibits voluntary guarding. Rectal examination reveals heme-positive stool. Laboratory values are unremarkable except for a WBC count of 12,500 with a left shift. Which of the following tests would be most useful in the diagnosis of this patient's disease?
- A. Abdominal x-ray
- B. Abdominal CT (Correct Answer)
- C. Emergent colonoscopy
- D. Left lower quadrant ultrasound
- E. Lipase
Diverticulitis Explanation: ***Abdominal CT***
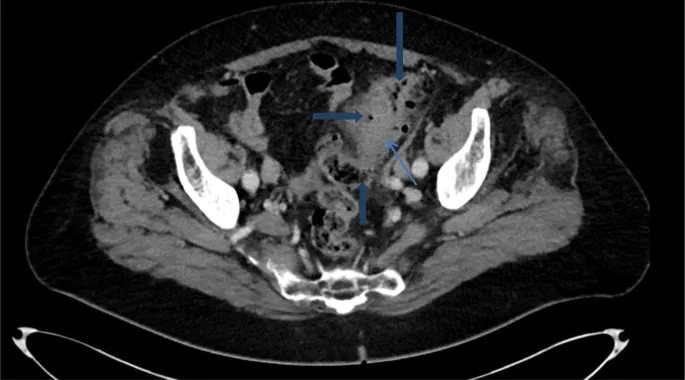
- **CT scan** is the most accurate imaging modality for diagnosing **diverticulitis**, identifying bowel wall thickening, inflammation, and complications such as abscess formation.
- It effectively differentiates diverticulitis from other causes of **left lower quadrant pain** and can guide intervention if necessary.
*Abdominal x-ray*
- An **abdominal x-ray** is generally not useful for diagnosing **diverticulitis** as it provides limited soft tissue detail.
- It may identify free air in cases of perforation, but it is not sensitive or specific for diverticular inflammation.
*Emergent colonoscopy*
- **Colonoscopy** is generally contraindicated in acute **diverticulitis** due to the risk of **perforation** of the inflamed colon.
- It is typically performed after recovery from an acute episode (usually 4-6 weeks later) to rule out underlying malignancy or other inflammatory bowel conditions.
*Left lower quadrant ultrasound*
- While **ultrasound** can identify diverticulitis, its diagnostic accuracy is highly **operator-dependent** and can be limited by bowel gas.
- It is often less sensitive than CT, particularly for deeper structures or in obese patients, making **CT** the preferred initial imaging study.
*Lipase*
- **Lipase** is a marker for **pancreatitis** and is not relevant for the diagnosis of **diverticulitis**.
- The patient's symptoms are localized to the left lower quadrant and are not suggestive of pancreatic inflammation.
Diverticulitis US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Diverticulitis Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Diverticulitis US Medical PG Question 6: A 65-year-old man comes to the physician because of abdominal pain and bloody, mucoid diarrhea for 3 days. He has been taking over-the-counter supplements for constipation over the past 6 months. He was diagnosed with type 2 diabetes mellitus 15 years ago. He has smoked one pack of cigarettes daily for 35 years. His current medications include metformin. His temperature is 38.4°C (101.1°F), pulse is 92/min, and blood pressure is 134/82 mm Hg. Examination of the abdomen shows no masses. Palpation of the left lower abdomen elicits tenderness. A CT scan of the abdomen is shown. Which of the following is the most likely underlying cause of the patient's condition?
- A. Focal weakness of the colonic muscularis layer (Correct Answer)
- B. Twisting of the sigmoid colon around its mesentery
- C. Transmural inflammation of the terminal ileum
- D. Infiltrative growth in the descending colon
- E. Decreased perfusion to mesenteric blood vessel
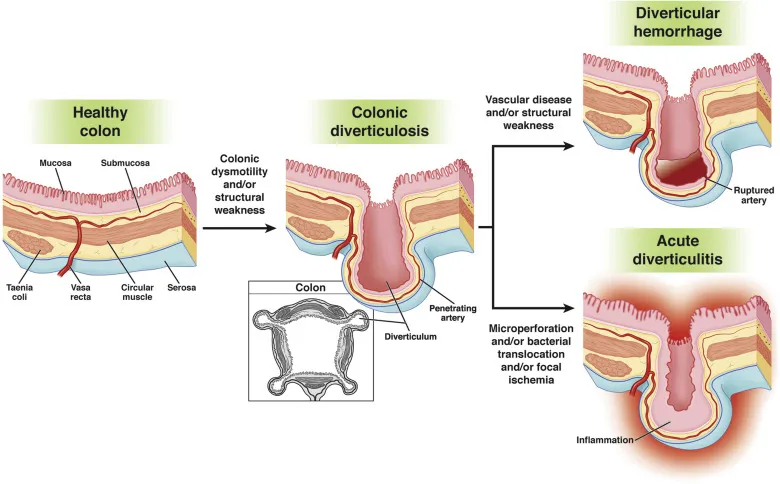
Diverticulitis Explanation: **Focal weakness of the colonic muscularis layer**
- The patient's symptoms of **abdominal pain**, **bloody, mucoid diarrhea**, and **left lower abdominal tenderness** are classic for **diverticulitis**, which occurs when small pouches (diverticula) in the colon become inflamed or infected. Diverticula form due to **focal weakness in the colonic muscularis layer**, often at points where blood vessels penetrate the muscle wall.
- **Constipation** and a history of **smoking** are risk factors for diverticular disease, contributing to increased intraluminal pressure and the formation of diverticula.
*Twisting of the sigmoid colon around its mesentery*
- This describes a **sigmoid volvulus**, which presents with acute onset of **severe abdominal pain**, distension, and obstipation (complete absence of stool and gas).
- While a volvulus can cause bloody stools due to ischemia, the clinical presentation and likely CT findings (not provided, but inferred to show diverticula) are inconsistent with this condition, and the described symptoms point more towards inflammation.
*Transmural inflammation of the terminal ileum*
- This suggests **Crohn's disease**, which can cause abdominal pain and diarrhea. However, Crohn's disease typically affects the **terminal ileum** and has a more chronic course, often with weight loss, perianal disease, and extraintestinal manifestations.
- Bloody, mucoid diarrhea is less typical for Crohn's unless there is severe colonic involvement, and the acute onset and tenderness in the left lower quadrant point away from isolated terminal ileitis.
*Infiltrative growth in the descending colon*
- An **infiltrative growth** (e.g., colorectal cancer) can cause changes in bowel habits, abdominal pain, and bloody stools. However, it usually presents with more **chronic symptoms** and weight loss.
- The acute inflammatory picture presented (fever, tenderness, mucoid diarrhea) is less characteristic of an uncomplicated infiltrative growth without obstruction or perforation.
*Decreased perfusion to mesenteric blood vessel*
- This describes **ischemic colitis**, which causes acute abdominal pain, bloody diarrhea, and tenderness. While it's a possibility, especially in older patients with vascular risk factors (diabetes, smoking), the description of **mucoid diarrhea** and the strong association with a history of constipation and symptoms pointing to localized inflammation (tenderness in left lower abdomen suggesting sigmoid/descending colon involvement) make **diverticulitis** a more likely primary cause in this context unless imaging strongly suggests ischemia.
- Ischemic colitis often presents with more severe, diffuse abdominal pain often out of proportion to physical exam findings initially.
Diverticulitis US Medical PG Question 7: A 75-year-old man presents to the emergency department for abdominal pain. The patient states the pain started this morning and has been worsening steadily. He decided to come to the emergency department when he began vomiting. The patient has a past medical history of obesity, diabetes, alcohol abuse, and hypertension. His current medications include captopril, insulin, metformin, sodium docusate, and ibuprofen. His temperature is 104.0°F (40°C), blood pressure is 160/97 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Abdominal exam reveals left lower quadrant tenderness. Cardiac exam reveals a crescendo systolic murmur heard best by the right upper sternal border. Lab values are ordered and return as below.
Hemoglobin: 15 g/dL
Hematocrit: 42%
Leukocyte count: 19,500 cells/mm^3 with normal differential
Platelet count: 226,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 24 mEq/L
BUN: 22 mg/dL
Glucose: 144 mg/dL
Creatinine: 1.2 mg/dL
Ca2+: 9.8 mg/dL
Which of the following is the most accurate test for this patient's condition?
- A. Colonoscopy
- B. Sigmoidoscopy
- C. Amylase and lipase levels
- D. Barium enema
- E. CT scan (Correct Answer)
Diverticulitis Explanation: ***CT scan***
- The patient presents with classic symptoms of **diverticulitis**, including **left lower quadrant pain**, **fever**, and **leukocytosis**. A **CT scan with oral and IV contrast** is the most accurate diagnostic test to identify diverticular inflammation, abscess formation, or perforation.
- A CT scan can also help rule out other causes of abdominal pain and guide further management, such as the need for percutaneous drainage of an abscess.
*Colonoscopy*
- **Colonoscopy is contraindicated during an acute episode of diverticulitis** due to the risk of **perforation** of an inflamed colon.
- It may be considered **6-8 weeks after resolution of acute diverticulitis** to investigate for other pathologies such as malignancy.
*Sigmoidoscopy*
- Similar to colonoscopy, **sigmoidoscopy is generally avoided in acute diverticulitis** because of the risk of **perforation** of the inflamed bowel from instrumentation.
- Its diagnostic yield in acute settings is also limited compared to CT imaging.
*Amylase and lipase levels*
- These tests are primarily used to diagnose **pancreatitis**, which typically presents with **epigastric pain radiating to the back**, often associated with elevated enzyme levels.
- While vomiting is present, the **left lower quadrant tenderness and fever** point away from pancreatitis as the primary diagnosis.
*Barium enema*
- **Barium enema is generally contraindicated in acute diverticulitis** due to the risk of **perforation** and the introduction of barium into the peritoneum, which can cause severe peritonitis.
- It has largely been replaced by **CT scanning** for its superior safety profile and diagnostic accuracy in acute abdominal conditions.
Diverticulitis US Medical PG Question 8: A 67-year-old man presents to the emergency department with abdominal pain that started 1 hour ago. The patient has a past medical history of diabetes and hypertension as well as a 40 pack-year smoking history. His blood pressure is 107/58 mmHg, pulse is 130/min, respirations are 23/min, and oxygen saturation is 98% on room air. An abdominal ultrasound demonstrates focal dilation of the aorta with peri-aortic fluid. Which of the following is the best next step in management?
- A. Serial annual abdominal ultrasounds
- B. Emergent surgical intervention (Correct Answer)
- C. Administer labetalol
- D. Counsel the patient in smoking cessation
- E. Urgent surgery within the next day
Diverticulitis Explanation: ***Emergent surgical intervention***
- The patient's presentation with acute **abdominal pain**, **hypotension**, and **tachycardia** combined with ultrasound findings of focal aortic dilation and peri-aortic fluid strongly suggests a **ruptured abdominal aortic aneurysm (AAA)**.
- A ruptured AAA is a life-threatening emergency requiring immediate surgical repair to prevent further hemorrhage and death.
*Serial annual abdominal ultrasounds*
- This approach is appropriate for asymptomatic patients with smaller, stable AAAs (typically <5.5 cm) to monitor for growth.
- In this case, the patient is symptomatic with signs of rupture, making surveillance an inappropriate and dangerous management strategy.
*Administer labetalol*
- Medications like labetalol are used to control blood pressure in conditions like aortic dissection or to slow the progression of AAAs, but they are contraindicated in hypotensive patients with a ruptured AAA.
- In this patient, labetalol would worsen the existing hypotension and could lead to cardiovascular collapse.
*Counsel the patient in smoking cessation*
- Smoking cessation is a crucial long-term intervention to reduce the risk of AAA expansion and rupture.
- While important, it does not address the immediate, life-threatening emergency of a ruptured AAA.
*Urgent surgery within the next day*
- Waiting until the next day for surgery in a patient with a suspected ruptured AAA is unacceptable.
- The patient's hemodynamic instability (hypotension, tachycardia) indicates active bleeding, and any delay significantly increases morbidity and mortality.
Diverticulitis US Medical PG Question 9: A 47-year-old woman is brought to the emergency department by her husband with the complaints of severe abdominal pain and discomfort. The pain began 2 days earlier, she describes it as radiating to her back and is associated with nausea. Her past medical history is significant for similar episodes of pain after fatty meals that resolved on its own. She drinks socially and has a 15 pack-year smoking history. Her pulse is 121/min, blood pressure is 121/71 mm Hg, and her temperature is 103.1°F (39.5°C). She has tenderness in the right upper quadrant and epigastrium with guarding and rebound tenderness. Bowel sounds are hypoactive. Part of a CBC is given below. What is the next best step in the management of this patient?
Hb%: 11 gm/dL
Total count (WBC): 13,400/mm3
Differential count:
Neutrophils: 80%
Lymphocytes: 15%
Monocytes: 5%
ESR: 45 mm/hr
C-reactive protein: 9.9 mg/dL (Normal < 3.0 mg/dL)
- A. Serum lipase levels
- B. Ultrasound of the gallbladder (Correct Answer)
- C. Erect abdominal X-ray
- D. Upper GI endoscopy
- E. Ultrasound of the appendix
Diverticulitis Explanation: ***Ultrasound of the gallbladder***
- The patient presents with classic symptoms of **acute cholecystitis**, including severe right upper quadrant pain radiating to the back, fever, leukocytosis, and a history of similar pain after fatty meals.
- An ultrasound of the gallbladder is the **gold standard** for diagnosing cholecystitis, as it can visualize gallstones, gallbladder wall thickening, pericholecystic fluid, and sonographic Murphy's sign.
*Serum lipase levels*
- While pancreatic involvement can occur, **serum lipase** is primarily used to diagnose **pancreatitis**, which typically presents with more severe epigastric pain and may or may not involve gallstones.
- The clinical picture here is more suggestive of cholecystitis, where gallbladder imaging is the priority.
*Erect abdominal X-ray*
- An **erect abdominal X-ray** is useful for detecting **free air under the diaphragm** in cases of bowel perforation or to assess for bowel obstruction.
- It is not the primary diagnostic tool for cholecystitis, as gallstones are often radiolucent and it does not provide detailed information about the gallbladder wall or surrounding structures.
*Upper GI endoscopy*
- **Upper GI endoscopy** is indicated for evaluating **esophageal, gastric, or duodenal pathologies**, such as ulcers, gastritis, or tumors.
- While peptic ulcer disease can cause epigastric pain, the patient's symptoms, especially the radiation to the back, fever, and history of pain after fatty meals, are more consistent with gallbladder disease, making endoscopy a less immediate diagnostic step.
*Ultrasound of the appendix*
- An **ultrasound of the appendix** is primarily used to diagnose **appendicitis**, which typically presents with periumbilical pain migrating to the right lower quadrant.
- The patient's pain is localized to the right upper quadrant and epigastrium, making appendicitis highly unlikely.
Diverticulitis US Medical PG Question 10: A 24-year-old woman recently noticed a mass in her left breast. The examination shows a 4-cm mass in the left upper quadrant. The mass is firm, mobile, and has well-defined margins. She complains of occasional tenderness. There is no lymphatic involvement. Mammography showed a dense lesion. What is the most likely cause?
- A. Phyllodes tumor
- B. Invasive ductal carcinoma (IDC)
- C. Inflammatory carcinoma
- D. Ductal carcinoma in situ (DCIS)
- E. Fibroadenoma (Correct Answer)
Diverticulitis Explanation: ***Fibroadenoma***
- The patient's age (24 years old) and the description of the mass as **firm, mobile, with well-defined margins** are classic features of a fibroadenoma.
- Fibroadenomas are **benign stromal and epithelial tumors** of the breast, often presenting as non-tender or occasionally tender masses, especially common in younger women.
*Phyllodes tumor*
- While also a fibroepithelial tumor, phyllodes tumors tend to grow **rapidly** and can reach **larger sizes** (often >5 cm), with some having malignant potential.
- They are typically seen in **older women** (perimenopausal or postmenopausal) compared to the patient's age.
*Invasive ductal carcinoma (IDC)*
- IDC often presents as a **hard, irregular, fixed mass** with **poorly defined margins**, which is contrary to the description of a mobile, well-defined mass.
- Although it can occur at this age, it is less likely given the benign-appearing physical characteristics of the mass.
*Inflammatory carcinoma*
- This is an aggressive form of breast cancer characterized by **rapid onset of redness, warmth, swelling**, and a "peau d'orange" appearance due to lymphatic involvement, none of which are described.
- It does not typically present as a mobile, well-defined mass.
*Ductal carcinoma in situ (DCIS)*
- DCIS is a **non-invasive** carcinoma where atypical cells are confined to the breast ducts and usually presents as **microcalcifications on mammography**, often without a palpable mass.
- When it does present as a palpable mass, it is typically not mobile with well-defined margins.
More Diverticulitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.