Acute cholecystitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute cholecystitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute cholecystitis US Medical PG Question 1: Three days after undergoing coronary artery bypass surgery, a 72-year-old man has severe right upper quadrant pain, fever, nausea, and vomiting. He has type 2 diabetes mellitus, benign prostatic hyperplasia, peripheral vascular disease, and chronic mesenteric ischemia. He had smoked one pack of cigarettes daily for 30 years but quit 10 years ago. He drinks 8 cans of beer a week. His preoperative medications include metformin, aspirin, simvastatin, and finasteride. His temperature is 38.9°C (102°F), pulse is 102/min, respirations are 18/min, and blood pressure is 110/60 mmHg. Auscultation of the lungs shows bilateral inspiratory crackles. Cardiac examination shows no murmurs, rubs or gallops. Abdominal examination shows soft abdomen with tenderness and sudden inspiratory arrest upon palpation in the right upper quadrant. There is no rebound tenderness or guarding. Laboratory studies show the following:
Hemoglobin 13.1 g/dL
Hematocrit 42%
Leukocyte count 15,700/mm3
Segmented neutrophils 65%
Bands 10%
Lymphocytes 20%
Monocytes 3%
Eosinophils 1%
Basophils 0.5%
AST 40 U/L
ALT 100 U/L
Alkaline phosphatase 85 U/L
Total bilirubin 1.5 mg/dL
Direct 0.9 mg/dL
Amylase 90 U/L
Abdominal ultrasonography shows a distended gallbladder, thickened gallbladder wall with pericholecystic fluid, and no stones. Which of the following is the most appropriate next step in management?
- A. Intravenous heparin therapy followed by embolectomy
- B. Careful observation with serial abdominal examinations
- C. Endoscopic retrograde cholangiopancreatography with papillotomy
- D. Intravenous piperacillin-tazobactam therapy and percutaneous cholecystostomy (Correct Answer)
- E. Immediate cholecystectomy
Acute cholecystitis Explanation: ***Intravenous piperacillin-tazobactam therapy and percutaneous cholecystostomy***
- The patient presents with **acalculous cholecystitis**, characterized by severe RUQ pain, fever, leukocytosis, elevated transaminases, and ultrasonographic findings of a distended gallbladder with a thickened wall and pericholecystic fluid, but no stones.
- Given his comorbid conditions (diabetes, PVD, recent CABG) and the severity of his illness, empirical **broad-spectrum antibiotics** (like piperacillin-tazobactam) along with image-guided **percutaneous cholecystostomy** for gallbladder decompression are the most appropriate management, avoiding the high risks of immediate surgery.
*Intravenous heparin therapy followed by embolectomy*
- This approach is indicated for **acute mesenteric ischemia with embolism**, which can present with severe abdominal pain and signs of hypoperfusion.
- While the patient has chronic mesenteric ischemia, his current symptoms and imaging findings are more consistent with cholecystitis, and there is no clear evidence of acute embolic event requiring embolectomy.
*Careful observation with serial abdominal examinations*
- This patient exhibits signs of a severe inflammatory process (fever, leukocytosis, RUQ tenderness, elevated LFTs, and sonographic findings of severe inflammation) and systemic illness, making **conservative observation insufficient** and potentially dangerous.
- **Acalculous cholecystitis** is a serious condition with a high risk of complications like perforation and sepsis, especially in critically ill patients, and requires prompt intervention.
*Endoscopic retrograde cholangiopancreatography with papillotomy*
- **ERCP with papillotomy** is indicated for conditions like **choledocholithiasis** (common bile duct stones) or **cholangitis**, which cause biliary obstruction.
- The ultrasound shows **no stones** and features specific to cholecystitis rather than common bile duct obstruction, making ERCP inappropriate as an initial step.
*Immediate cholecystectomy*
- While cholecystectomy is the definitive treatment for cholecystitis, immediate open or laparoscopic cholecystectomy in a critically ill patient with **acalculous cholecystitis** after recent CABG carries a **very high morbidity and mortality risk**.
- **Percutaneous cholecystostomy** offers a safer, less invasive alternative for source control and stabilizes the patient before potential delayed definitive surgery if needed, once the patient's condition improves.
Acute cholecystitis US Medical PG Question 2: Ten days after undergoing emergent colectomy for a ruptured bowel that she sustained in a motor vehicle accident, a 59-year-old woman has abdominal pain. During the procedure, she was transfused 3 units of packed red blood cells. She is currently receiving total parenteral nutrition. Her temperature is 38.9°C (102.0°F), pulse is 115/min, and blood pressure is 100/60 mm Hg. Examination shows tenderness to palpation in the right upper quadrant of the abdomen. Bowel sounds are hypoactive. Serum studies show:
Aspartate aminotransferase 142 U/L
Alanine aminotransferase 86 U/L
Alkaline phosphatase 153 U/L
Total bilirubin 1.5 mg/dL
Direct bilirubin 1.0 mg/dL
Amylase 20 U/L
Which of the following is the most likely diagnosis?
- A. Hemolytic transfusion reaction
- B. Acalculous cholecystitis (Correct Answer)
- C. Acute cholecystitis (calculous)
- D. Small bowel obstruction
- E. Acute pancreatitis
Acute cholecystitis Explanation: ***Acalculous cholecystitis***
- This patient's clinical picture of **fever**, **RUQ tenderness**, **leukocytosis**, and mildly elevated liver enzymes in the setting of recent **major surgery**, **trauma**, and **total parenteral nutrition (TPN)** is highly suggestive of **acalculous cholecystitis**.
- **Acalculous cholecystitis** often occurs in critically ill patients due to gallbladder stasis, ischemia, and inflammation, usually without the presence of stones.
*Hemolytic transfusion reaction*
- While the patient received blood transfusions, a **hemolytic transfusion reaction** typically presents with fever, chills, flank pain, and **hemoglobinuria**, none of which are explicitly mentioned.
- Liver enzyme elevations can occur, but the significant RUQ tenderness and absence of signs of hemolysis make it less likely.
*Acute cholecystitis (calculous)*
- **Acute cholecystitis with gallstones** typically presents with similar symptoms to acalculous cholecystitis (pain, fever), but requires the presence of gallstones causing obstruction.
- The clinical context of critical illness, recent surgery, and TPN use points more towards acalculous inflammation rather than stone-related disease.
*Small bowel obstruction*
- **Small bowel obstruction** would present with more pronounced **abdominal distention**, **vomiting**, and often **high-pitched bowel sounds** followed by absent sounds, which is not the primary picture here.
- Although bowel sounds are hypoactive, the focal RUQ tenderness and liver enzyme changes are not typical of a primary small bowel obstruction.
*Acute pancreatitis*
- **Acute pancreatitis** is usually characterized by **severe epigastric pain** radiating to the back, and significantly elevated **amylase** and **lipase** levels.
- The patient's amylase is normal, and lipase is not mentioned but usually tracks with amylase in pancreatitis.
Acute cholecystitis US Medical PG Question 3: A 52-year-old woman presents to the urgent care center with several hours of worsening abdominal discomfort with radiation to the back. The patient also complains of malaise, chills, nausea, and vomiting. Social history is notable for alcoholism. On physical exam, she is febrile to 39.5°C (103.1°F), and she is diffusely tender to abdominal palpation. Complete blood count is notable for 13,500 white blood cells, bilirubin 2.1, lipase 842, and amylase 3,210. Given the following options, what is the most likely diagnosis?
- A. Choledocholithiasis
- B. Ascending cholangitis
- C. Gallstone pancreatitis (Correct Answer)
- D. Cholelithiasis
- E. Acute cholecystitis
Acute cholecystitis Explanation: ***Gallstone pancreatitis***
- The patient presents with classic symptoms of **acute pancreatitis**: severe abdominal pain radiating to the back, nausea, vomiting, and markedly elevated **lipase (842)** and **amylase (3,210)**.
- The **key differentiating feature** is the elevated **bilirubin (2.1 mg/dL)**, which indicates biliary obstruction from a gallstone passing through or obstructing the ampulla of Vater.
- **Gallstone pancreatitis** is the most common cause of acute pancreatitis in women, and the combination of pancreatitis with hyperbilirubinemia strongly suggests a biliary etiology rather than alcoholic pancreatitis (which typically does not cause elevated bilirubin).
- While the patient has a history of alcoholism, the elevated bilirubin makes **gallstone pancreatitis** the most likely diagnosis.
*Choledocholithiasis*
- This refers to a stone in the **common bile duct**, which can cause biliary obstruction and elevated bilirubin.
- However, choledocholithiasis alone does not explain the **markedly elevated lipase and amylase**, which indicate pancreatic inflammation.
- Choledocholithiasis may be present as part of the pathophysiology, but the clinical picture is acute pancreatitis caused by the stone (gallstone pancreatitis).
*Ascending cholangitis*
- This serious bile duct infection presents with **Charcot's triad** (fever, jaundice, right upper quadrant pain) or **Reynolds' pentad** (adds altered mental status and hypotension).
- While the patient is febrile, she lacks **jaundice**, hypotension, or altered mental status.
- The **extremely elevated lipase and amylase** point to pancreatitis rather than cholangitis as the primary process.
*Cholelithiasis*
- This simply means **gallstones in the gallbladder**, which are often asymptomatic.
- The patient's acute presentation with fever, systemic symptoms, and markedly elevated pancreatic enzymes indicates a complication of gallstones (pancreatitis), not just their presence.
*Acute cholecystitis*
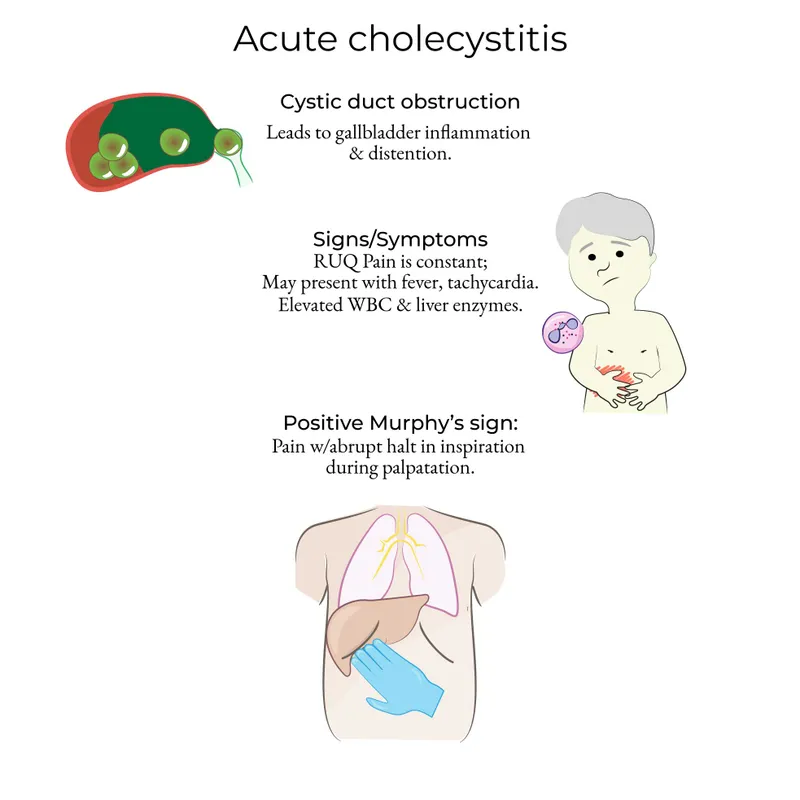
- This is **gallbladder inflammation**, typically presenting with right upper quadrant pain, fever, positive Murphy's sign, and leukocytosis.
- The **diffuse abdominal tenderness** (not localized to RUQ), pain radiating to the back, and **extremely elevated lipase and amylase** are characteristic of pancreatitis, not cholecystitis.
- Acute cholecystitis does not cause such dramatic elevations in pancreatic enzymes.
Acute cholecystitis US Medical PG Question 4: A 45-year-old woman comes to the emergency department because of right upper abdominal pain and nausea that have become progressively worse since eating a large meal 8 hours ago. She has had intermittent pain similar to this before, but it has never lasted this long. She has a history of hypertension and type 2 diabetes mellitus. She does not smoke or drink alcohol. Current medications include metformin and enalapril. Her temperature is 38.5°C (101.3°F), pulse is 90/min, and blood pressure is 130/80 mm Hg. The abdomen is soft, and bowel sounds are normal. The patient has sudden inspiratory arrest during right upper quadrant palpation. Laboratory studies show a leukocyte count of 13,000/mm3. Serum alkaline phosphatase, total bilirubin, amylase, and aspartate aminotransferase levels are within the reference ranges. Imaging is most likely to show which of the following findings?
- A. Dilated common bile duct with intrahepatic biliary dilatation
- B. Enlargement of the pancreas with peripancreatic fluid
- C. Gallstone in the cystic duct (Correct Answer)
- D. Gas in the gallbladder wall
- E. Decreased echogenicity of the liver
Acute cholecystitis Explanation: ***Gallstone in the cystic duct***
- The patient's presentation with **right upper quadrant pain** after a fatty meal, **nausea**, **fever**, **leukocytosis**, and a positive **Murphy's sign** (inspiratory arrest during palpation) is highly suggestive of **acute cholecystitis**.
- **Acute cholecystitis** is most commonly caused by an obstructing gallstone in the **cystic duct**, leading to inflammation of the gallbladder.
*Dilated common bile duct with intrahepatic biliary dilatation*
- This finding suggests **choledocholithiasis** (gallstone in the common bile duct) or another obstruction of the common bile duct, which would typically cause **elevated bilirubin** and **alkaline phosphatase**.
- These laboratory values are **within normal limits** for this patient, making choledocholithiasis less likely.
*Enlargement of the pancreas with peripancreatic fluid*
- These findings are characteristic of **acute pancreatitis**, which would present with elevated **amylase** and **lipase**.
- The patient's **amylase level is normal**, ruling out acute pancreatitis as the primary diagnosis.
*Gas in the gallbladder wall*
- This indicates **emphysematous cholecystitis**, a severe form of acute cholecystitis typically seen in elderly or immunocompromised patients, often with diabetes.
- While the patient has diabetes, the overall clinical picture does not specifically point to this more advanced and rare complication, and it's not the *most likely* initial finding for typical acute cholecystitis.
*Decreased echogenicity of the liver*
- Decreased echogenicity of the liver is typically associated with conditions like **fatty liver disease** or **hepatitis**.
- While the patient has risk factors for fatty liver (type 2 diabetes), this finding does not explain her acute symptoms of right upper quadrant pain, fever, and Murphy's sign, which point towards gallbladder pathology.
Acute cholecystitis US Medical PG Question 5: A 58-year-old woman comes to the emergency department because of a 2-day history of worsening upper abdominal pain. She reports nausea and vomiting, and is unable to tolerate oral intake. She appears uncomfortable. Her temperature is 38.1°C (100.6°F), pulse is 92/min, respirations are 18/min, and blood pressure is 132/85 mm Hg. Examination shows yellowish discoloration of her sclera. Her abdomen is tender in the right upper quadrant. There is no abdominal distention or organomegaly. Laboratory studies show:
Hemoglobin 13 g/dL
Leukocyte count 16,000/mm3
Serum
Urea nitrogen
25 mg/dL
Creatinine 2 mg/dL
Alkaline phosphatase 432 U/L
Alanine aminotransferase 196 U/L
Aspartate transaminase 207 U/L
Bilirubin
Total 3.8 mg/dL
Direct 2.7 mg/dL
Lipase 82 U/L (N = 14–280)
Ultrasound of the right upper quadrant shows dilated intrahepatic and extrahepatic bile ducts and multiple hyperechoic spheres within the gallbladder. The pancreas is not well visualized. Intravenous fluid resuscitation and antibiotic therapy with ceftriaxone and metronidazole is begun. Twelve hours later, the patient appears acutely ill and is not oriented to time. Her temperature is 39.1°C (102.4°F), pulse is 105/min, respirations are 22/min, and blood pressure is 112/82 mm Hg. Which of the following is the most appropriate next step in management?
- A. Abdominal CT scan
- B. Laparoscopic cholecystectomy
- C. Endoscopic retrograde cholangiopancreatography (Correct Answer)
- D. Extracorporeal shock wave lithotripsy
- E. Percutaneous cholecystostomy
Acute cholecystitis Explanation: ***Endoscopic retrograde cholangiopancreatography***
- The patient exhibits signs of **cholangitis** (fever, jaundice, RUQ pain), complicated by **sepsis** and **altered mental status**, necessitating urgent biliary decompression.
- **ERCP** allows for direct visualization of the biliary tree, removal of stones, and stent placement to relieve obstruction.
*Abdominal CT scan*
- While CT can provide more detailed anatomical information, it is not the most immediate or definitive therapeutic intervention for acute biliary obstruction and sepsis.
- **Delaying definitive biliary decompression** for imaging could worsen the patient's rapidly deteriorating clinical status.
*Laparoscopic cholecystectomy*
- **Cholecystectomy** is indicated for symptomatic gallstones, but in the setting of acute cholangitis, especially with increasing severity and signs of sepsis, it carries a higher risk.
- The primary and most urgent goal is to **decompress the obstructed biliary system**, which cholecystectomy alone may not achieve if the obstruction is in the common bile duct.
*Extracorporeal shock wave lithotripsy*
- **ESWL** is generally used for breaking up gallstones or kidney stones but is not suitable for the urgent management of **obstructive cholangitis with sepsis**.
- It does not provide immediate biliary decompression and is typically considered for less acute biliary issues or specific stone types.
*Percutaneous cholecystostomy*
- **PCD** involves placing a drain into the gallbladder percutaneously to decompress the gallbladder, often used in critically ill patients with acute cholecystitis who are not surgical candidates.
- However, the primary issue here is **common bile duct obstruction and cholangitis**, not just cholecystitis, so PCD would not address the main problem of biliary outflow obstruction.
Acute cholecystitis US Medical PG Question 6: An 82-year-old woman visits her primary care provider complaining of a vague cramping pain on the right side of her abdomen for the past 6 hours. She is also nauseated and had an episode of vomiting earlier today and two episodes yesterday. Past medical history includes third-degree heart block, gastroesophageal reflux disease, hypertension, hypothyroidism and chronic cholecystitis with cholelithiasis. She is not a good candidate for cholecystectomy due to cardiac disease and is treated with analgesics and ursodeoxycholic acid. Her medications include chlorthalidone, omeprazole, levothyroxine, and occasional naproxen for pain. Vitals are normal. A supine abdominal X-ray reveals air in the gallbladder and biliary tree, small bowel obstruction, and a large radiolucent gallstone impacted in the small bowel. What is the most likely diagnosis?
- A. Cholecystitis
- B. Small bowel perforation
- C. Choledocolithiasis
- D. Gallstone ileus (Correct Answer)
- E. Primary biliary cholangitis
Acute cholecystitis Explanation: ***Gallstone ileus***
- The presence of **air in the gallbladder and biliary tree** (**pneumobilia**), signs of **small bowel obstruction**, and a **large radiolucent gallstone impacted in the small bowel** are the classic features of gallstone ileus, known as **Rigler's triad**.
- This condition occurs when a gallstone erodes through the gallbladder wall into the small intestine, causing obstruction.
*Cholecystitis*
- While the patient has a history of chronic cholecystitis with cholelithiasis, the described **radiographic findings** (pneumobilia, small bowel obstruction) are not typical for uncomplicated acute cholecystitis.
- Acute cholecystitis would typically present with **right upper quadrant pain**, fever, and nausea/vomiting, often with gallbladder wall thickening and pericholecystic fluid on imaging.
*Small bowel perforation*
- Small bowel perforation would typically present with **acute, severe abdominal pain**, signs of peritonitis, and potentially **free air under the diaphragm** on abdominal radiographs.
- While there is small bowel obstruction, the other specific findings of gallstone ileus (pneumobilia, impacted gallstone) differentiate this from a simple perforation.
*Choledocolithiasis*
- This involves the presence of gallstones in the **common bile duct**, leading to symptoms like **jaundice**, cholangitis, or pancreatitis.
- The imaging findings of **air in the gallbladder and biliary tree** and a **small bowel obstruction** with an impacted stone are not characteristic of choledocholithiasis.
*Primary biliary cholangitis*
- This is a **chronic autoimmune liver disease** affecting the small bile ducts, presenting with fatigue, pruritus, and elevated liver enzymes, particularly **alkaline phosphatase**.
- It does not involve gallstone impaction in the small bowel or present with acute small bowel obstruction.
Acute cholecystitis US Medical PG Question 7: Fourteen days after a laparoscopic cholecystectomy for cholelithiasis, a 45-year-old woman comes to the emergency department because of persistent episodic epigastric pain for 3 days. The pain radiates to her back, occurs randomly throughout the day, and is associated with nausea and vomiting. Each episode lasts 30 minutes to one hour. Antacids do not improve her symptoms. She has hypertension and fibromyalgia. She has smoked 1–2 packs of cigarettes daily for the past 10 years and drinks 4 cans of beer every week. She takes lisinopril and pregabalin. She appears uncomfortable. Her temperature is 37°C (98.6° F), pulse is 84/min, respirations are 14/min, and blood pressure is 127/85 mm Hg. Abdominal examination shows tenderness to palpation in the upper quadrants without rebound or guarding. Bowel sounds are normal. The incisions are clean, dry, and intact. Serum studies show:
AST 80 U/L
ALT 95 U/L
Alkaline phosphatase 213 U/L
Bilirubin, total 1.3 mg/dL
Direct 0.7 mg/dL
Amylase 52 U/L
Abdominal ultrasonography shows dilation of the common bile duct and no gallstones. Which of the following is the most appropriate next step in management?
- A. Counseling on alcohol cessation
- B. Endoscopic retrograde cholangiopancreatography (Correct Answer)
- C. Proton pump inhibitor therapy
- D. CT scan of the abdomen
- E. Reassurance and follow-up in 4 weeks
Acute cholecystitis Explanation: ***Endoscopic retrograde cholangiopancreatography***
- The patient's symptoms (epigastric pain radiating to the back, nausea, vomiting, elevated liver enzymes, and **common bile duct (CBD) dilation** on ultrasound after cholecystectomy) are highly suggestive of **postcholecystectomy syndrome**, specifically due to a retained or de novo **CBD stone** or **sphincter of Oddi dysfunction**.
- **ERCP** is both diagnostic and therapeutic in this setting, allowing for visualization of the bile ducts, stone extraction (if present), or sphincterotomy.
*Counseling on alcohol cessation*
- While **alcohol cessation** is beneficial for overall health, especially with a history of alcohol use, it is not the most immediate or appropriate next step for the acute and severe symptoms presented.
- The patient's symptoms are more indicative of a **biliary obstruction** rather than alcohol-related chronic pancreatitis or liver disease, given the acute onset post-surgery.
*Proton pump inhibitor therapy*
- **PPI therapy** is used for acid-related disorders such as GERD or peptic ulcers, which typically present with burning epigastric pain that improves with antacids.
- This patient's pain radiates to the back, is associated with nausea and vomiting, does not improve with antacids, and has abnormal imaging/labs (CBD dilation, elevated liver enzymes), ruling out a simple acid-related issue.
*CT scan of the abdomen*
- An abdominal **CT scan** could provide more detailed imaging but is generally less effective than ERCP for evaluating **biliary duct pathology** and is not therapeutic.
- Given the ultrasound findings of **CBD dilation** and the patient's symptoms, a more invasive but definitive diagnostic and therapeutic procedure is warranted.
*Reassurance and follow-up in 4 weeks*
- The patient is experiencing severe, persistent symptoms with abnormal liver enzymes and imaging findings indicating **biliary obstruction** post-cholecystectomy.
- **Reassurance and delayed follow-up** would be inappropriate and could lead to worsening of her condition, including cholangitis or pancreatitis if left untreated.
Acute cholecystitis US Medical PG Question 8: A 45-year-old woman comes to the emergency department complaining of abdominal pain for the past day. The pain is situated in the right upper quadrant, colicky, 8/10, and radiates to the tip of the right shoulder with no aggravating or relieving factors. The pain is associated with nausea but no vomiting. She tried to take over-the-counter antacids which relieved her pain to a certain extent, but not entirely. She does not smoke cigarettes or drink alcohol. She has no past medical illness. Her father died of pancreatic cancer at the age of 75, and her mother has diabetes controlled with medications. Temperature is 38°C (100.4°F), blood pressure is 125/89 mm Hg, pulse is 104/min, respiratory rate is 20/min, and BMI is 29 kg/m2. On abdominal examination, her abdomen is tender to shallow and deep palpation of the right upper quadrant.
Laboratory test
Complete blood count
Hemoglobin 13 g/dL
WBC 15,500/mm3
Platelets 145,000/mm3
Basic metabolic panel
Serum Na+ 137 mEq/L
Serum K+ 3.6 mEq/L
Serum Cl- 95 mEq/L
Serum HCO3- 25 mEq/L
BUN 10 mg/dL
Serum creatinine 0.8 mg/dL
Liver function test
Total bilirubin 1.3 mg/dL
AST 52 U/L
ALT 60 U/L
Ultrasonography of the abdomen shows normal findings. What is the best next step in management of this patient?
- A. Emergency cholecystectomy
- B. CT scan
- C. Reassurance and close follow up
- D. Cholescintigraphy (Correct Answer)
- E. Percutaneous cholecystostomy
Acute cholecystitis Explanation: ***Cholescintigraphy***
- The patient presents with **right upper quadrant pain**, fever, **leukocytosis**, and elevated liver enzymes, pointing towards **acute cholecystitis**. Despite a normal ultrasound, cholescintigraphy (HIDA scan) is the gold standard for diagnosing acute cholecystitis when imaging is equivocal.
- Cholescintigraphy can assess the **patency of the cystic duct**, which is often obstructed in acute cholecystitis, by observing whether the gallbladder fills with tracer.
*Emergency cholecystectomy*
- **Acute cholecystitis** usually requires cholecystectomy, but it's typically performed **after confirmation** of the diagnosis, often after a period of stabilization with antibiotics and fluids, not immediately as an emergency for this stable patient.
- There is no evidence of severe complications such as **gallbladder perforation** or gangrene that would necessitate immediate emergency surgery without further diagnostic confirmation.
*CT scan*
- A **CT scan** is not the primary imaging modality for acute cholecystitis as it is **less sensitive** than ultrasound or cholescintigraphy for detecting gallbladder inflammation and cystic duct obstruction.
- While CT can identify complications such as abscess formation or perforation, the initial diagnostic work-up should focus on confirming the inflammation of the gallbladder itself.
*Reassurance and close follow up*
- The patient's symptoms (severe **colicky pain**, fever, **leukocytosis**, elevated liver enzymes) indicate an **acute inflammatory process** requiring active medical management and diagnosis, not mere reassurance.
- Delaying appropriate diagnosis and treatment for acute cholecystitis can lead to severe complications like gallbladder perforation, sepsis, or cholangitis.
*Percutaneous cholecystostomy*
- **Percutaneous cholecystostomy** is generally reserved for patients with acute cholecystitis who are **too unstable for surgery**, or in cases where surgical risk is very high.
- The patient is hemodynamically stable and does not have contraindications for surgery, making a definitive surgical approach (after diagnosis) preferable over a temporizing measure.
Acute cholecystitis US Medical PG Question 9: A 47-year-old woman is brought to the emergency department by her husband with the complaints of severe abdominal pain and discomfort. The pain began 2 days earlier, she describes it as radiating to her back and is associated with nausea. Her past medical history is significant for similar episodes of pain after fatty meals that resolved on its own. She drinks socially and has a 15 pack-year smoking history. Her pulse is 121/min, blood pressure is 121/71 mm Hg, and her temperature is 103.1°F (39.5°C). She has tenderness in the right upper quadrant and epigastrium with guarding and rebound tenderness. Bowel sounds are hypoactive. Part of a CBC is given below. What is the next best step in the management of this patient?
Hb%: 11 gm/dL
Total count (WBC): 13,400/mm3
Differential count:
Neutrophils: 80%
Lymphocytes: 15%
Monocytes: 5%
ESR: 45 mm/hr
C-reactive protein: 9.9 mg/dL (Normal < 3.0 mg/dL)
- A. Serum lipase levels
- B. Ultrasound of the gallbladder (Correct Answer)
- C. Erect abdominal X-ray
- D. Upper GI endoscopy
- E. Ultrasound of the appendix
Acute cholecystitis Explanation: ***Ultrasound of the gallbladder***
- The patient presents with classic symptoms of **acute cholecystitis**, including severe right upper quadrant pain radiating to the back, fever, leukocytosis, and a history of similar pain after fatty meals.
- An ultrasound of the gallbladder is the **gold standard** for diagnosing cholecystitis, as it can visualize gallstones, gallbladder wall thickening, pericholecystic fluid, and sonographic Murphy's sign.
*Serum lipase levels*
- While pancreatic involvement can occur, **serum lipase** is primarily used to diagnose **pancreatitis**, which typically presents with more severe epigastric pain and may or may not involve gallstones.
- The clinical picture here is more suggestive of cholecystitis, where gallbladder imaging is the priority.
*Erect abdominal X-ray*
- An **erect abdominal X-ray** is useful for detecting **free air under the diaphragm** in cases of bowel perforation or to assess for bowel obstruction.
- It is not the primary diagnostic tool for cholecystitis, as gallstones are often radiolucent and it does not provide detailed information about the gallbladder wall or surrounding structures.
*Upper GI endoscopy*
- **Upper GI endoscopy** is indicated for evaluating **esophageal, gastric, or duodenal pathologies**, such as ulcers, gastritis, or tumors.
- While peptic ulcer disease can cause epigastric pain, the patient's symptoms, especially the radiation to the back, fever, and history of pain after fatty meals, are more consistent with gallbladder disease, making endoscopy a less immediate diagnostic step.
*Ultrasound of the appendix*
- An **ultrasound of the appendix** is primarily used to diagnose **appendicitis**, which typically presents with periumbilical pain migrating to the right lower quadrant.
- The patient's pain is localized to the right upper quadrant and epigastrium, making appendicitis highly unlikely.
Acute cholecystitis US Medical PG Question 10: A 30-year-old woman, gravida 1, para 0, at 30 weeks' gestation is brought to the emergency department because of progressive upper abdominal pain for the past hour. The patient vomited once on her way to the hospital. She said she initially had dull, generalized stomach pain about 6 hours prior, but now the pain is located in the upper abdomen and is more severe. There is no personal or family history of any serious illnesses. She is sexually active with her husband. She does not smoke or drink alcohol. Medications include folic acid and a multivitamin. Her temperature is 38.5°C (101.3°F), pulse is 100/min, and blood pressure is 130/80 mm Hg. Physical examination shows right upper quadrant tenderness. The remainder of the examination shows no abnormalities. Laboratory studies show a leukocyte count of 12,000/mm3. Urinalysis shows mild pyuria. Which of the following is the most appropriate definitive treatment in the management of this patient?
- A. Laparoscopic removal of ovarian cysts
- B. Cefoxitin and azithromycin
- C. Appendectomy
- D. Cholecystectomy (Correct Answer)
- E. Intramuscular ceftriaxone followed by cephalexin
Acute cholecystitis Explanation: ***Cholecystectomy***
- The patient's presentation (fever, RUQ pain, leukocytosis, vomiting) is classic for **acute cholecystitis** in pregnancy, which requires **cholecystectomy** as the definitive treatment.
- **Laparoscopic cholecystectomy** is safe during pregnancy and is the **preferred definitive treatment** for acute cholecystitis, ideally performed in the second trimester but can be done in the third trimester when indicated.
- While conservative management with antibiotics and supportive care can be attempted initially, cholecystectomy remains the definitive treatment and is increasingly performed during pregnancy to avoid recurrent symptoms and complications.
- The mild pyuria is likely secondary to adjacent inflammation rather than a primary UTI.
*Laparoscopic removal of ovarian cysts*
- Ovarian cysts typically present with **pelvic or lower abdominal pain**, not RUQ tenderness.
- The clinical picture with fever, leukocytosis, and RUQ pain strongly suggests biliary pathology, not ovarian pathology.
*Cefoxitin and azithromycin*
- This regimen is used for **pelvic inflammatory disease (PID)**, which presents with lower abdominal/pelvic pain, cervical motion tenderness, and vaginal discharge.
- The patient's RUQ localization and fever pattern do not support PID as the primary diagnosis.
*Intramuscular ceftriaxone followed by cephalexin*
- This regimen treats **gonorrhea/chlamydia** or uncomplicated UTIs.
- While mild pyuria is present, the dominant clinical features (fever, RUQ pain, leukocytosis) point to cholecystitis, not a primary genitourinary infection.
- Antibiotics alone would not provide definitive treatment for acute cholecystitis.
*Appendectomy*
- **Appendicitis** in pregnancy typically causes **RLQ pain** (though it can migrate superiorly in the third trimester due to uterine displacement).
- The distinct **RUQ localization** with the classic triad of fever, RUQ pain, and leukocytosis makes cholecystitis far more likely than appendicitis.
More Acute cholecystitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.