Acute appendicitis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute appendicitis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute appendicitis US Medical PG Question 1: A 1-year-old boy is brought to the emergency room by his parents because of inconsolable crying and diarrhea for the past 6 hours. As the physician is concerned about acute appendicitis, she consults the literature base. She finds a paper with a table that summarizes data regarding the diagnostic accuracy of multiple clinical findings for appendicitis:
Clinical finding Sensitivity Specificity
Abdominal guarding (in children of all ages) 0.70 0.85
Anorexia (in children of all ages)
0.75 0.50
Abdominal rebound (in children ≥ 5 years of age) 0.85 0.65
Vomiting (in children of all ages) 0.40 0.63
Fever (in children from 1 month to 2 years of age) 0.80 0.80
Based on the table, the absence of which clinical finding would most accurately rule out appendicitis in this patient?
- A. Guarding
- B. Vomiting
- C. Anorexia
- D. Fever (Correct Answer)
- E. Rebound
Acute appendicitis Explanation: ***Fever***
- To **rule out** a diagnosis, a finding with **high sensitivity** is desired. A high sensitivity means that if the disease is present, the test result will almost always be positive. Therefore, a negative test result (absence of the finding) in a highly sensitive test makes the presence of the disease unlikely.
- Fever has a sensitivity of **0.80**, which means it is present in 80% of patients with appendicitis in the 1 month to 2 years age group. While 0.80 isn't extremely high, among the options applicable to this age group, it is the highest sensitivity for a "rule out" purpose. The absence of fever would therefore be the most useful finding to rule out appendicitis.
*Guarding*
- Guarding has a sensitivity of **0.70**, meaning it is present in 70% of appendicitis cases. While it's a useful sign, its sensitivity is lower than fever for ruling out the condition.
- Its higher specificity (0.85) means that its presence makes appendicitis more likely, but its absence is less helpful for ruling it out compared to a highly sensitive finding.
*Vomiting*
- Vomiting has a sensitivity of **0.40**, which is very low. This means that 60% of patients with appendicitis do not experience vomiting.
- Therefore, the absence of vomiting is not a reliable indicator to rule out appendicitis, as many appendicitis cases occur without it.
*Anorexia*
- Anorexia has a sensitivity of **0.75**. While higher than vomiting and guarding, it is still lower than fever (0.80) in the relevant age group for ruling out appendicitis.
- Its low specificity (0.50) indicates it's a common symptom even in children without appendicitis, making its presence less diagnostic and its absence less useful for ruling out.
*Rebound*
- The table states that abdominal rebound data is for children **≥ 5 years of age**. The patient is 1 year old.
- Therefore, this clinical finding's diagnostic accuracy is not applicable to the given patient's age and cannot be used for diagnosis or ruling out appendicitis.
Acute appendicitis US Medical PG Question 2: A 12-year-old boy is brought to the emergency department late at night by his worried mother. She says he has not been feeling well since this morning after breakfast. He skipped both lunch and dinner. He complains of abdominal pain as he points towards his lower abdomen but says that the pain initially started at the center of his belly. His mother adds that he vomited once on the way to the hospital. His past medical history is noncontributory and his vaccinations are up to date. His temperature is 38.1°C (100.6°F), pulse is 98/min, respirations are 20/min, and blood pressure is 110/75 mm Hg. Physical examination reveals right lower quadrant tenderness. The patient is prepared for laparoscopic abdominal surgery. Which of the following structures is most likely to aid the surgeons in finding the source of this patient's pain and fever?
- A. McBurney's point
- B. Linea Semilunaris
- C. Transumbilical plane
- D. Arcuate line
- E. Teniae coli (Correct Answer)
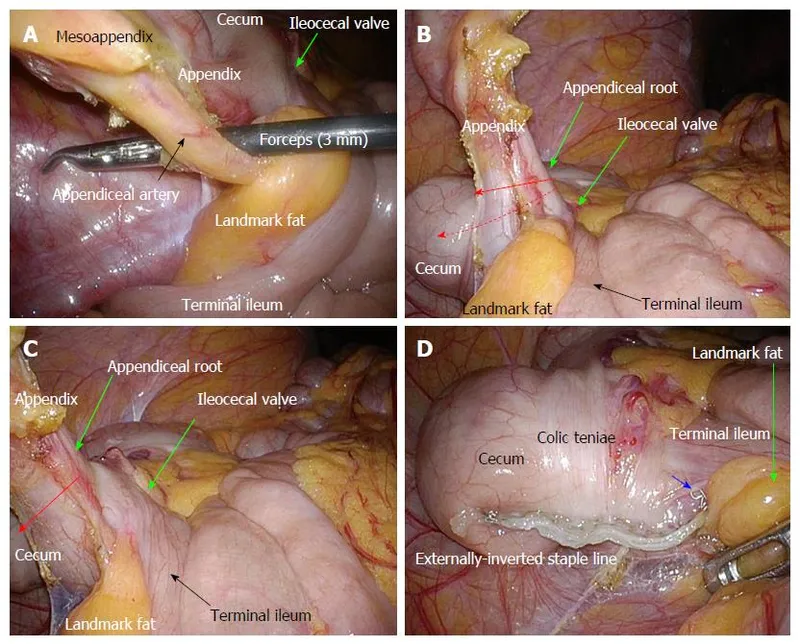
Acute appendicitis Explanation: ***Teniae coli***
- The **teniae coli** are three distinct longitudinal bands of smooth muscle that run along the length of the large intestine, converging at the base of the appendix. They serve as reliable anatomical landmarks for locating the appendix during surgery.
- Given the patient's symptoms (periumbilical pain migrating to the right lower quadrant, fever, vomiting, and right lower quadrant tenderness), **acute appendicitis** is highly suspected, making the teniae coli crucial for surgical identification of the inflamed appendix.
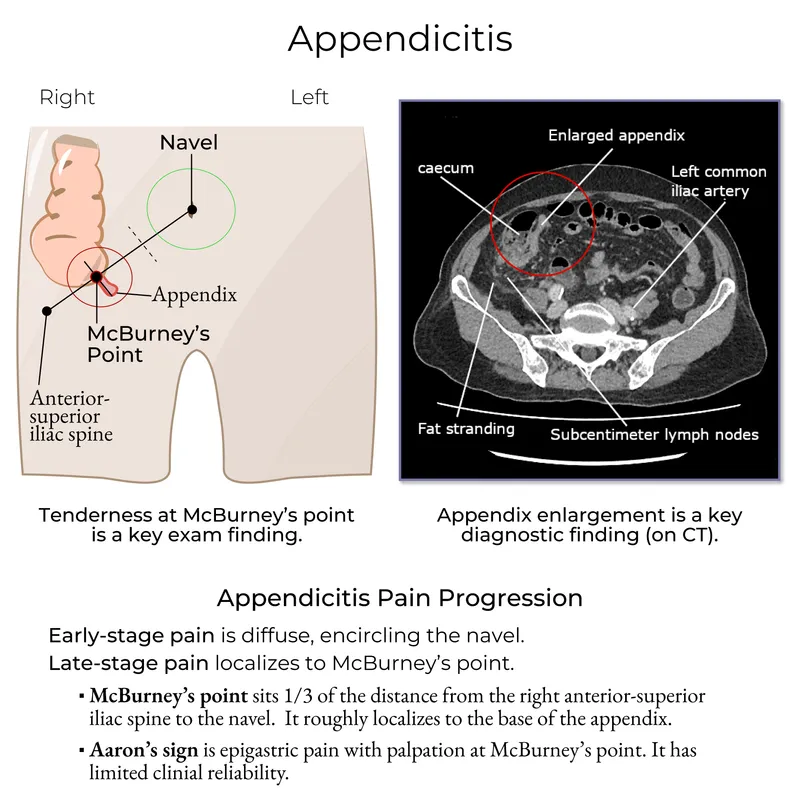
*McBurney's point*
- **McBurney's point** is a clinical landmark on the abdominal wall, two-thirds of the way from the umbilicus to the right anterior superior iliac spine, that often corresponds to the base of the appendix. It is used to elicit tenderness during physical examination.
- While tenderness at McBurney's point is a strong indicator of appendicitis, it is a **surface landmark** for diagnosis and not an internal anatomical structure that aids the surgeon in _finding_ the appendix during a laparoscopic procedure.
*Linea Semilunaris*
- The **linea semilunaris** is the curved tendinous intersection found at the lateral border of the rectus abdominis muscle, extending from the costal margin to the pubic tubercle.
- It defines the lateral extent of the rectus sheath but has **no direct anatomical relationship** to the appendix or its surgical identification.
*Transumbilical plane*
- The **transumbilical plane** is an imaginary horizontal plane passing through the umbilicus. It is used in topographical anatomy for abdominal segmentation.
- It is a **surface and arbitrary anatomical plane** for regional description, not an internal structure that guides surgical access to or identification of the appendix.
*Arcuate line*
- The **arcuate line** is a crescent-shaped anatomical landmark located on the posterior wall of the rectus sheath, inferior to the umbilicus, marking the transition where the aponeuroses of the transverse abdominis and internal oblique muscles pass anterior to the rectus abdominis.
- This line is relevant to the integrity of the rectus sheath but is **anatomically distant from the appendix** and does not assist in its surgical localization.
Acute appendicitis US Medical PG Question 3: A 19-year-old man comes to the emergency department because of abdominal pain, nausea, and vomiting for 4 hours. Initially, the pain was dull and located diffusely around his umbilicus, but it has now become sharper and moved towards his lower right side. He has no history of serious illness and takes no medications. His temperature is 38.2°C (100.7°F) and blood pressure is 123/80 mm Hg. Physical examination shows severe right lower quadrant tenderness without rebound or guarding; bowel sounds are decreased. His hemoglobin concentration is 14.2 g/dL, leukocyte count is 12,000/mm3, and platelet count is 280,000/mm3. Abdominal ultrasonography shows a dilated noncompressible appendix with distinct wall layers and echogenic periappendiceal fat. Intravenous fluid resuscitation is begun. Which of the following is the most appropriate next step in management?
- A. Prescribe oral amoxicillin and clavulanic acid
- B. Perform laparoscopic appendectomy (Correct Answer)
- C. Perform percutaneous drainage
- D. Perform interval appendectomy
- E. Begin bowel rest and nasogastric aspiration
Acute appendicitis Explanation: ***Perform laparoscopic appendectomy***
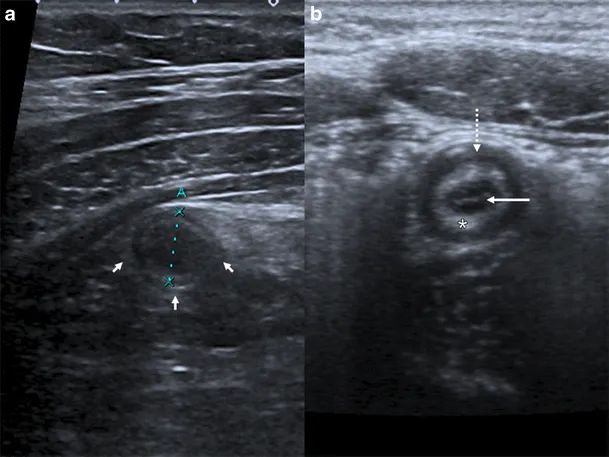
- The patient presents with classic symptoms of **acute appendicitis**, including periumbilical pain migrating to the right lower quadrant, localized tenderness, fever, and leukocytosis.
- Abdominal ultrasonography showing a **dilated noncompressible appendix** with echogenic periappendiceal fat further confirms the diagnosis, making surgical removal the most appropriate and definitive treatment.
*Prescribe oral amoxicillin and clavulanic acid*
- While antibiotics are often given pre-operatively, they are not the definitive treatment for **acute appendicitis**, especially with clear imaging findings.
- Relying solely on antibiotics in this scenario would risk **perforation** and increased morbidity.
*Perform percutaneous drainage*
- Percutaneous drainage is typically reserved for **appendiceal abscesses** or phlegmons, especially if the patient is unstable or the inflammation is walled off.
- There is no mention of an abscess in this patient's presentation or imaging, making surgical removal of the inflamed appendix the primary treatment.
*Perform interval appendectomy*
- **Interval appendectomy** is considered for patients who initially respond to conservative antibiotic management for an appendiceal mass or phlegmon.
- Since this patient has acute symptoms with clear ultrasound findings of appendicitis without mention of an abscess that would necessitate conservative management, immediate surgical intervention is indicated.
*Begin bowel rest and nasogastric aspiration*
- Bowel rest and nasogastric aspiration are indicated for conditions like **bowel obstruction** or severe **pancreatitis** to decompress the gastrointestinal tract.
- These measures do not address the underlying inflammation and obstruction of acute appendicitis and would delay definitive treatment, increasing the risk of complications.
Acute appendicitis US Medical PG Question 4: A 68-year-old woman is brought to the emergency department with intense abdominal pain for the past 2 hours. She has had 1 episode of bloody diarrhea recently. She has an 18-year history of diabetes mellitus. She was diagnosed with hypertension and ischemic heart disease 6 years ago. She is fully alert and oriented. Her temperature is 37.5°C (99.5°F), blood pressure is 145/90 mm Hg, pulse is 78/min, and respirations are 14/min. Abdominal examination shows mild generalized abdominal tenderness without guarding or rebound tenderness. An abdominal plain X-ray shows no abnormalities. Abdominal CT reveals colonic wall thickening and pericolonic fat stranding in the splenic curvature. Bowel rest, intravenous hydration, and IV antibiotics are initiated. Which of the following is the most important diagnostic evaluation at this time?
- A. Angiography
- B. Gastrografin-enhanced X-ray
- C. Laparotomy
- D. Inpatient observation
- E. Sigmoidoscopy (Correct Answer)
Acute appendicitis Explanation: ***Sigmoidoscopy***
- The patient's presentation with acute abdominal pain, bloody diarrhea, history of cardiovascular disease, and CT findings consistent with **colonic wall thickening** and **pericolonic fat stranding** strongly suggests **ischemic colitis**.
- **Flexible sigmoidoscopy** allows for direct visualization of the colonic mucosa to confirm the diagnosis, assess the extent and severity of ischemia, and rule out other causes of colitis, such as inflammatory bowel disease or infection.
*Angiography*
- While angiography can identify mesenteric arterial occlusion, it is generally reserved for cases of acute mesenteric ischemia involving the superior mesenteric artery, which typically presents with more severe pain out of proportion to physical exam findings and less clear CT findings of colitis.
- In cases of ischemic colitis, where the primary concern is mucosal ischemia rather than immediate large vessel occlusion, angiography is usually not the first-line diagnostic.
*Gastrografin-enhanced X-ray*
- This study (also known as a **Gastrografin swallow or enema**) is primarily used to evaluate for **perforations** or **obstructions**, or to assess lumen integrity.
- It does not provide the mucosal detail necessary to diagnose or assess the severity of **ischemic colitis**, and the contrast agent itself could potentially exacerbate an inflamed bowel.
*Laparotomy*
- **Laparotomy** (surgical exploration) is an invasive procedure reserved for cases with signs of peritonitis, bowel perforation, or severe, unresponsive ischemia requiring surgical intervention.
- Given the patient's stable vital signs, mild tenderness, and lack of guarding or rebound, immediate surgical exploration is not warranted without further diagnostic steps.
*Inpatient observation*
- While inpatient observation is part of the initial management (bowel rest, IV fluids, antibiotics), it is not a **diagnostic evaluation** itself.
- The question asks for the most important diagnostic evaluation to determine the underlying cause and guide further management.
Acute appendicitis US Medical PG Question 5: A 42-year-old man presents to the emergency department with abdominal pain. The patient was at home watching television when he experienced sudden and severe abdominal pain that prompted him to instantly call emergency medical services. The patient has a past medical history of obesity, smoking, alcoholism, hypertension, and osteoarthritis. His current medications include lisinopril and ibuprofen. His temperature is 98.5°F (36.9°C), blood pressure is 120/97 mmHg, pulse is 130/min, respirations are 22/min, and oxygen saturation is 97% on room air. The patient is in an antalgic position on the stretcher. His abdomen is rigid and demonstrates rebound tenderness and hypoactive bowel sounds. What is the next best step in management?
- A. CT of the abdomen
- B. Urgent laparoscopy
- C. NPO, IV fluids, and analgesics
- D. Urgent laparotomy (Correct Answer)
- E. Abdominal radiograph
Acute appendicitis Explanation: ***Urgent laparotomy***
- The patient's presentation with **sudden, severe abdominal pain**, a **rigid abdomen**, **rebound tenderness**, and **hypoactive bowel sounds** indicates **acute peritonitis**, most likely from a **perforated viscus**.
- In a patient with **frank peritonitis** and clinical signs of perforation, the diagnosis is **made clinically** based on physical examination findings.
- **Urgent laparotomy** (exploratory surgery) is the definitive management and should not be delayed for imaging when peritonitis is obvious.
- The patient's risk factors (NSAID use, alcoholism) further support peptic ulcer perforation as the likely etiology.
*CT of the abdomen*
- While CT scan is highly sensitive for identifying perforation and can provide anatomic detail, it is **not necessary when the diagnosis of peritonitis is clinically evident**.
- In a patient with **obvious peritonitis**, obtaining a CT scan would **delay definitive surgical treatment** without changing management.
- CT is more appropriate for stable patients with **uncertain diagnosis** or equivocal physical findings, not for those with frank peritonitis.
*Urgent laparoscopy*
- **Laparoscopy** can be used diagnostically and therapeutically in selected cases of abdominal emergencies.
- However, in a patient with diffuse peritonitis and suspected perforation, **laparotomy** is generally preferred over laparoscopy as it provides better exposure, faster source control, and easier peritoneal lavage.
- Laparoscopy may be considered in stable patients with localized findings, but this patient has signs of diffuse peritonitis.
*NPO, IV fluids, and analgesics*
- These are **essential supportive measures** and should be initiated immediately as part of resuscitation.
- However, they are **adjunctive** to definitive surgical management and do not constitute the "next best step" in a patient requiring emergency surgery.
- These measures should be initiated concurrently while preparing for urgent laparotomy.
*Abdominal radiograph*
- An **upright chest X-ray** or **abdominal radiograph** can show **free air under the diaphragm** (pneumoperitoneum) in cases of perforation.
- However, it is **only 50-70% sensitive**, meaning it misses many perforations.
- In a patient with **clinical peritonitis**, the absence of free air on X-ray does **not rule out perforation** and should not delay surgery.
- Imaging should not delay surgical intervention when peritonitis is clinically evident.
Acute appendicitis US Medical PG Question 6: A 75-year-old man presents to the emergency department for abdominal pain. The patient states the pain started this morning and has been worsening steadily. He decided to come to the emergency department when he began vomiting. The patient has a past medical history of obesity, diabetes, alcohol abuse, and hypertension. His current medications include captopril, insulin, metformin, sodium docusate, and ibuprofen. His temperature is 104.0°F (40°C), blood pressure is 160/97 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Abdominal exam reveals left lower quadrant tenderness. Cardiac exam reveals a crescendo systolic murmur heard best by the right upper sternal border. Lab values are ordered and return as below.
Hemoglobin: 15 g/dL
Hematocrit: 42%
Leukocyte count: 19,500 cells/mm^3 with normal differential
Platelet count: 226,000/mm^3
Serum:
Na+: 139 mEq/L
Cl-: 101 mEq/L
K+: 4.4 mEq/L
HCO3-: 24 mEq/L
BUN: 22 mg/dL
Glucose: 144 mg/dL
Creatinine: 1.2 mg/dL
Ca2+: 9.8 mg/dL
Which of the following is the most accurate test for this patient's condition?
- A. Colonoscopy
- B. Sigmoidoscopy
- C. Amylase and lipase levels
- D. Barium enema
- E. CT scan (Correct Answer)
Acute appendicitis Explanation: ***CT scan***
- The patient presents with classic symptoms of **diverticulitis**, including **left lower quadrant pain**, **fever**, and **leukocytosis**. A **CT scan with oral and IV contrast** is the most accurate diagnostic test to identify diverticular inflammation, abscess formation, or perforation.
- A CT scan can also help rule out other causes of abdominal pain and guide further management, such as the need for percutaneous drainage of an abscess.
*Colonoscopy*
- **Colonoscopy is contraindicated during an acute episode of diverticulitis** due to the risk of **perforation** of an inflamed colon.
- It may be considered **6-8 weeks after resolution of acute diverticulitis** to investigate for other pathologies such as malignancy.
*Sigmoidoscopy*
- Similar to colonoscopy, **sigmoidoscopy is generally avoided in acute diverticulitis** because of the risk of **perforation** of the inflamed bowel from instrumentation.
- Its diagnostic yield in acute settings is also limited compared to CT imaging.
*Amylase and lipase levels*
- These tests are primarily used to diagnose **pancreatitis**, which typically presents with **epigastric pain radiating to the back**, often associated with elevated enzyme levels.
- While vomiting is present, the **left lower quadrant tenderness and fever** point away from pancreatitis as the primary diagnosis.
*Barium enema*
- **Barium enema is generally contraindicated in acute diverticulitis** due to the risk of **perforation** and the introduction of barium into the peritoneum, which can cause severe peritonitis.
- It has largely been replaced by **CT scanning** for its superior safety profile and diagnostic accuracy in acute abdominal conditions.
Acute appendicitis US Medical PG Question 7: A 55-year-old man presents to the emergency department with nausea and vomiting. The patient states that he has felt nauseous for the past week and began vomiting last night. He thought his symptoms would resolve but decided to come in when his symptoms worsened. He feels that his symptoms are exacerbated with large fatty meals and when he drinks alcohol. His wife recently returned from a cruise with symptoms of vomiting and diarrhea. The patient has a past medical history of poorly managed diabetes, constipation, anxiety, dyslipidemia, and hypertension. His temperature is 99.5°F (37.5°C), blood pressure is 197/128 mmHg, pulse is 100/min, respirations are 17/min, and oxygen saturation is 95% on room air. Physical exam reveals a systolic murmur heard loudest along the left upper sternal border. Abdominal exam reveals an obese, tympanitic and distended abdomen with a 3 cm scar in the right lower quadrant. Vascular exam reveals weak pulses in the lower extremities. Which of the following is the most likely diagnosis?
- A. Enteric nervous system damage
- B. Twisting of the bowel
- C. Adhesions (Correct Answer)
- D. Norovirus
- E. Impacted stool
Acute appendicitis Explanation: ***Adhesions***
- The patient's history of a 3 cm scar in the right lower quadrant suggests a prior abdominal surgery, which is the most common cause of **intra-abdominal adhesions**.
- **Adhesions** can lead to **small bowel obstruction**, causing symptoms like nausea, vomiting, abdominal distension, and tympany, which are all present in this patient.
*Enteric nervous system damage*
- Poorly managed diabetes can cause **diabetic gastroparesis**, which involves damage to the **enteric nervous system** leading to delayed gastric emptying.
- While it can cause nausea and vomiting, it doesn't typically present with significant abdominal distension or tympany, which are indicative of a mechanical obstruction.
*Twisting of the bowel*
- **Volvulus**, or twisting of the bowel, causes acute abdominal pain, distension, and often complete obstruction.
- While it's a possibility for bowel obstruction, the presence of a surgical scar and gradual worsening of symptoms over a week makes **adhesions** a more likely cause in this scenario.
*Norovirus*
- **Norovirus** is a common cause of acute gastroenteritis, characterized by abrupt onset of vomiting and diarrhea, often with a rapid resolution.
- Although his wife has similar symptoms, the patient's symptoms have been ongoing for a week, are exacerbated by fatty meals, and include abdominal distension, which is inconsistent with typical norovirus infection.
*Impacted stool*
- **Fecal impaction** can cause constipation, abdominal pain, and sometimes paradoxical diarrhea.
- While the patient has a history of constipation, the significant **tympanic distension** and persistent vomiting suggest a mechanical obstruction rather than just impacted stool.
Acute appendicitis US Medical PG Question 8: A 68-year-old man presents to the emergency department with left lower quadrant abdominal pain and fever for 1 day. He states during this time frame he has had weight loss and a decreased appetite. The patient had surgery for a ruptured Achilles tendon 1 month ago and is still recovering but is otherwise generally healthy. His temperature is 102°F (38.9°C), blood pressure is 154/94 mmHg, pulse is 90/min, respirations are 15/min, and oxygen saturation is 98% on room air. Physical exam is remarkable for an uncomfortable and thin man with left lower quadrant abdominal tenderness without rebound findings. Fecal occult test for blood is positive. Laboratory studies are ordered as seen below.
Hemoglobin: 10 g/dL
Hematocrit: 30%
Leukocyte count: 3,500/mm^3 with normal differential
Platelet count: 157,000/mm^3
Which of the following is the most appropriate next step in management?
- A. Ceftriaxone and metronidazole
- B. Ciprofloxacin and metronidazole
- C. Colonoscopy
- D. CT abdomen (Correct Answer)
- E. MRI abdomen
Acute appendicitis Explanation: ***CT abdomen***
- A **CT scan of the abdomen and pelvis** is the most appropriate initial diagnostic step for acute left lower quadrant pain with fever, leukopenia, and a positive fecal occult blood test, as it can efficiently evaluate for **diverticulitis**, bowel perforation, or **colonic malignancy**.
- The patient's presentation with constitutional symptoms like **weight loss and decreased appetite** in an older male, along with signs of anemia and occult blood, raises concern for **colorectal cancer**, making imaging a critical next step to differentiate potential etiologies.
*Ceftriaxone and metronidazole*
- While this is a common antibiotic regimen for suspected **diverticulitis**, it should not be initiated without definitive imaging, especially given the patient's concerning systemic symptoms and signs of **anemia and occult bleeding**, which could indicate a more serious underlying condition.
- Empirical antibiotic therapy without a clear diagnosis could delay the identification of conditions like **colorectal cancer** or abscess, which require different management strategies.
*Ciprofloxacin and metronidazole*
- This is also a typical antibiotic combination for uncomplicated **diverticulitis**; however, giving antibiotics without confirmation of the diagnosis via imaging is inappropriate in this case due to the patient's **systemic symptoms** and signs of **GI bleeding**.
- Without imaging to rule out intestinal perforation or malignancy, starting antibiotics could mask symptoms or delay crucial diagnostic and therapeutic interventions.
*Colonoscopy*
- A **colonoscopy** is indicated to investigate the **positive fecal occult blood** and rule out colorectal malignancy, but it is generally *contraindicated* in the acute setting of suspected diverticulitis due to the risk of **perforation**.
- Imaging (like CT) should always precede colonoscopy when acute abdominal pain and inflammation are present to assess for safety and guide the timing of endoscopy.
*MRI abdomen*
- While **MRI provides excellent soft tissue delineation**, it is typically not the first-line imaging modality for acute abdominal pain presentations in the emergency department.
- **CT scans are faster, more readily available**, and provide comprehensive imaging of the bowel, mesentery, and surrounding structures, making them superior for initial evaluation of acute abdominal conditions like diverticulitis or perforation.
Acute appendicitis US Medical PG Question 9: A 12-year-old boy is brought to the emergency room by his mother with complaints of abdominal pain and fever that started 24 hours ago. On further questioning, the mother says that her son vomited twice and has constipation that started approximately 1 and one-half days ago. The medical history is benign. The vital signs are as follows: heart rate 103/min, respiratory rate of 20/min, temperature 38.7°C (101.66°F), and blood pressure 109/69 mm Hg. On physical examination, there is severe right lower quadrant abdominal tenderness on palpation. Which of the following is the most likely cause for this patient’s symptoms?
- A. Luminal obstruction due to a fecalith (Correct Answer)
- B. Ascending infection of the urinary tract
- C. Telescoping of bowel segment causing intestinal obstruction
- D. Twisting of testes on its axis, hampering the blood supply
- E. Immune-mediated vasculitis associated with IgA deposition
Acute appendicitis Explanation: ***Luminal obstruction due to a fecalith***
- The classic presentation of **appendicitis** in a 12-year-old boy, including **abdominal pain**, fever, vomiting, constipation, and **right lower quadrant tenderness**, is most commonly caused by **luminal obstruction** due to a **fecalith**.
- This obstruction leads to inflammation, bacterial overgrowth, and edema of the appendix, resulting in the described symptoms.
- Other causes of appendiceal luminal obstruction include **lymphoid hyperplasia** and, less commonly, parasites or tumors.
*Ascending infection of the urinary tract*
- While urinary tract infections (UTIs) can cause fever and abdominal pain, the **severe, localized right lower quadrant tenderness** and specific progression of symptoms (vomiting, constipation) are less typical than for appendicitis.
- UTIs are usually associated with **dysuria, frequency, and urgency**, which are not mentioned here.
*Telescoping of bowel segment causing intestinal obstruction*
- This describes **intussusception**, which typically presents in **younger children (6 months to 3 years)** with **colicky abdominal pain**, vomiting, and **currant jelly stools**.
- While it can cause abdominal pain and vomiting, the **age of the patient**, **localized right lower quadrant tenderness**, and absence of classic signs make appendicitis more likely.
*Twisting of testes on its axis, hampering the blood supply*
- This describes **testicular torsion**, which presents with **sudden, severe scrotal pain**, swelling, and tenderness, sometimes with referred abdominal pain.
- The primary complaint of **abdominal pain** with associated vomiting, fever, and right lower quadrant tenderness makes appendicitis a more likely diagnosis.
*Immune-mediated vasculitis associated with IgA deposition*
- This refers to **Henoch-Schönlein purpura (HSP)**, which typically presents with a **palpable purpuric rash** on the lower extremities and buttocks, **arthralgia**, abdominal pain, and sometimes renal involvement.
- The absence of a rash and key features of HSP makes this diagnosis less likely than appendicitis.
Acute appendicitis US Medical PG Question 10: A 16-year-old boy presents to the emergency department with abdominal pain and tenderness. The pain began approximately 2 days ago in the area just above his umbilicus and was crampy in nature. Earlier this morning, the pain moved laterally to his right lower abdomen. At that time, the pain in the right lower quadrant became severe and constant and woke him up from sleep. He decided to come to the hospital. The patient is nauseous and had a low-grade fever of 37.8°C (100.1°F). Other vitals are normal. Upon physical examination, the patient has rebound tenderness but a negative psoas sign while the remaining areas of his abdomen are non-tender. His rectal exam is normal. Laboratory tests show a white cell count of 15,000/mm3. Urinalysis and other laboratory findings were negative. What conclusion can be drawn about the nerves involved in the transmission of this patient’s pain during the physical exam?
- A. His pain is transmitted bilaterally by somatic afferent nerve fibers of the abdomen.
- B. His pain is transmitted by somatic afferent nerve fibers located in the right flank.
- C. His pain is transmitted by the pelvic nerves.
- D. His pain is transmitted by right somatic nerve fibers. (Correct Answer)
- E. His pain is mainly transmitted by the right splanchnic nerve.
Acute appendicitis Explanation: ***His pain is transmitted by right somatic nerve fibers.***
- The **migration of pain from the periumbilical region to the right lower quadrant** and becoming **severe and constant** indicates parietal peritoneal irritation.
- **Somatic nerve fibers** innervate the parietal peritoneum and are responsible for transmitting **sharp, localized pain** typically associated with appendicitis in the right lower quadrant.
*His pain is transmitted bilaterally by somatic afferent nerve fibers of the abdomen.*
- While **visceral pain** from the initial appendiceal inflammation can be perceived bilaterally in the periumbilical region due to **bilateral innervation of visceral organs**, the **localized right lower quadrant pain** signifies involvement of **unilaterally innervated parietal peritoneum**.
- The physical exam findings of **rebound tenderness** strongly suggest **localized peritoneal inflammation**, which is transmitted by **unilateral somatic nerves** at the site of inflammation, not bilaterally across the abdomen.
*His pain is transmitted by somatic afferent nerve fibers located in the right flank.*
- The **right flank** refers to the lateral aspect of the abdomen, while the pain is specifically localized to the **right lower quadrant**.
- Although somatic nerves are involved, stating "right flank" is **too broad and imprecise** given the very specific localization of the pain to the right lower quadrant where the inflamed appendix is typically situated.
*His pain is transmitted by the pelvic nerves.*
- **Pelvic nerves** primarily carry parasympathetic fibers and visceral afferent fibers from pelvic organs, not the somatic pain from the parietal peritoneum in the right lower quadrant.
- Pain from **pelvic organs** or **pelvic peritoneum** would be transmitted via these nerves, but the localized pain here is distinctly higher than typical pelvic organ pain.
*His pain is mainly transmitted by the right splanchnic nerve.*
- **Splanchnic nerves** primarily carry **visceral afferent fibers** responsible for the dull, poorly localized, initial periumbilical pain of appendicitis.
- They do not transmit the **sharp, well-localized somatic pain** associated with parietal peritoneal irritation, which is characteristic of the pain migrating to the right lower quadrant.
More Acute appendicitis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.