Withdrawal management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Withdrawal management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Withdrawal management US Medical PG Question 1: A 20-year-old female presents to student health at her university for excessive daytime sleepiness. She states that her sleepiness has caused her to fall asleep in all of her classes for the last semester, and that her grades are suffering as a result. She states that she normally gets 7 hours of sleep per night, and notes that when she falls asleep during the day, she immediately starts having dreams. She denies any cataplexy. A polysomnogram and a multiple sleep latency test rule out obstructive sleep apnea and confirm her diagnosis. She is started on a daytime medication that acts both by direct neurotransmitter release and reuptake inhibition. What other condition can this medication be used to treat?
- A. Obsessive-compulsive disorder
- B. Bulimia
- C. Attention-deficit hyperactivity disorder (Correct Answer)
- D. Tourette syndrome
- E. Alcohol withdrawal
Withdrawal management Explanation: ***Attention-deficit hyperactivity disorder***
- The patient's presentation is consistent with **narcolepsy type 2 (without cataplexy)**, given the excessive daytime sleepiness, short latency to REM sleep (immediate dreaming), and exclusion of sleep apnea. The medication described, acting via **direct neurotransmitter release and reuptake inhibition**, is characteristic of a stimulant like **methylphenidate** or an amphetamine-based drug.
- These stimulants are commonly used as first-line treatment for **attention-deficit hyperactivity disorder (ADHD)** due to their effects on dopamine and norepinephrine in the brain, improving focus and reducing impulsivity.
*Obsessive-compulsive disorder*
- **Obsessive-compulsive disorder (OCD)** is typically treated with selective serotonin reuptake inhibitors (SSRIs) or cognitive behavioral therapy.
- Stimulants are not indicated for OCD and may even worsen anxiety symptoms in some individuals.
*Bulimia*
- **Bulimia nervosa** is often managed with a combination of psychotherapy (e.g., cognitive behavioral therapy) and antidepressants like fluoxetine.
- Stimulants are not a primary treatment for bulimia and could potentially exacerbate some symptoms or risks due to their appetite-suppressing effects.
*Tourette syndrome*
- **Tourette syndrome** involves motor and vocal tics and is often treated with alpha-2 adrenergic agonists (e.g., guanfacine, clonidine) or dopamine receptor blocking agents.
- Stimulants generally are not used for Tourette syndrome as they can sometimes worsen tics.
*Alcohol withdrawal*
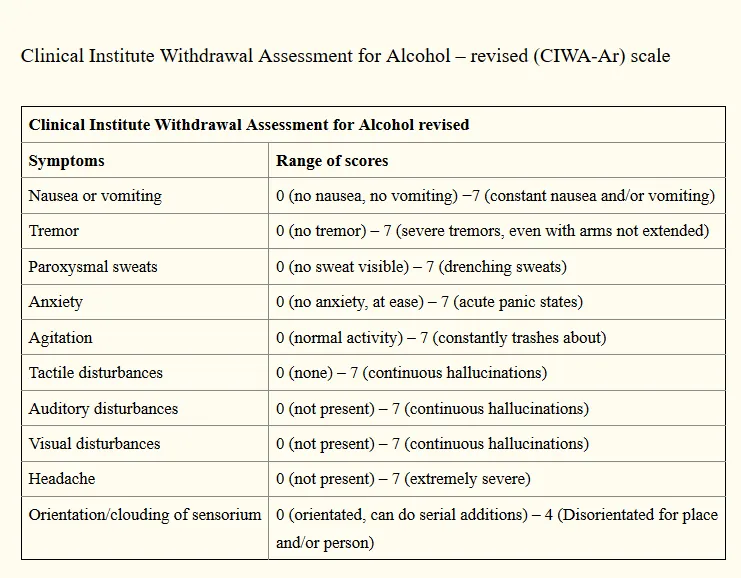
- **Alcohol withdrawal** is a medical emergency managed with benzodiazepines to prevent seizures and delirium tremens.
- Stimulants are contraindicated in alcohol withdrawal as they can increase seizure risk and cardiac complications.
Withdrawal management US Medical PG Question 2: A 53-year-old woman presented to her PCP with one week of difficulty falling asleep, despite having good sleep hygiene. She denies changes in her mood, weight loss, and anhedonia. She has had difficulty concentrating and feels tired throughout the day. Recently, she was fired from her previous job. What medication would be most helpful for this patient?
- A. Citalopram
- B. Diphenhydramine
- C. Quetiapine
- D. Diazepam
- E. Zolpidem (Correct Answer)
Withdrawal management Explanation: ***Zolpidem***
- This patient presents with **insomnia** characterized by **difficulty falling asleep**, which is the primary indication for zolpidem.
- Zolpidem is a **non-benzodiazepine GABA-A receptor agonist** that acts quickly to induce sleep, making it effective for sleep onset insomnia.
*Citalopram*
- **Citalopram** is an **SSRI** primarily used for treating depression and anxiety disorders, which are not explicitly indicated as primary issues for this patient.
- While it can sometimes help with sleep in depressed patients, its **onset of action is slow** (weeks), and it is not a first-line agent for acute insomnia.
*Diphenhydramine*
- **Diphenhydramine** is an **antihistamine** with sedative properties, often used for occasional insomnia, but it can lead to significant **daytime sedation, anticholinergic side effects**, and is generally not recommended for chronic use.
- The patient's presentation suggests a need for more targeted and potentially long-term management beyond an over-the-counter antihistamine.
*Quetiapine*
- **Quetiapine** is an **antipsychotic** medication that is sometimes used off-label for insomnia due to its sedative effects, but it carries significant **side effects** like metabolic syndrome, orthostatic hypotension, and tardive dyskinesia.
- It is generally **not recommended as a first-line treatment for insomnia** without co-occurring psychiatric conditions like bipolar disorder or schizophrenia.
*Diazepam*
- **Diazepam** is a **benzodiazepine** that can be used for insomnia, but it has a **long half-life** leading to daytime sedation and a **high potential for dependence and abuse**.
- Its use should be limited to short-term treatment of severe insomnia and is generally avoided in patients who deny mood changes and anhedonia, suggesting a less complex underlying issue.
Withdrawal management US Medical PG Question 3: A 30-year-old man is brought to the emergency department by the police after starting a fight at a local bar. He has several minor bruises and he appears agitated. He talks incessantly about his future plans. He reports that he has no history of disease and that he is "super healthy" and "never felt better". His temperature is 38.0°C (100.4°F), pulse is 110/min, respirations are 16/min, and blood pressure is 155/80 mm Hg. On physical examination reveals a euphoric and diaphoretic man with slightly dilated pupils. An electrocardiogram is obtained and shows tachycardia with normal sinus rhythm. A urine toxicology screen is positive for cocaine. The patient is held in the ED for observation. Which of the following symptoms can the patient expect to experience as he begins to withdraw from cocaine?
- A. Psychosis
- B. Seizures
- C. Lacrimation
- D. Increased appetite (Correct Answer)
- E. Increased sympathetic stimulation
Withdrawal management Explanation: ***Increased appetite***
- **Cocaine withdrawal** is characterized by a "crash" phase, which includes severe fatigue, **dysphoria**, and increased appetite, often leading to binge eating as the body attempts to replenish depleted neurotransmitters.
- This symptom, combined with **hypersomnia** and a reduction in pleasure, represents a rebound effect from the intense stimulation caused by cocaine use.
*Psychosis*
- While acute cocaine intoxication can induce **psychotic symptoms** like paranoia and hallucinations, psychosis is not a typical feature of the *withdrawal* phase.
- Instead, the withdrawal period is often marked by a decrease in stimulation, leading to symptoms like depression and anhedonia rather than further agitation or psychosis.
*Seizures*
- **Seizures** are a potential complication of acute cocaine intoxication due to its stimulant effects on the central nervous system, but they are generally not a primary symptom of uncomplicated **cocaine withdrawal**.
- Withdrawal is more commonly associated with a state of brain hyperexcitability that manifests as cravings and dysphoria, not typically grand mal seizures.
*Lacrimation*
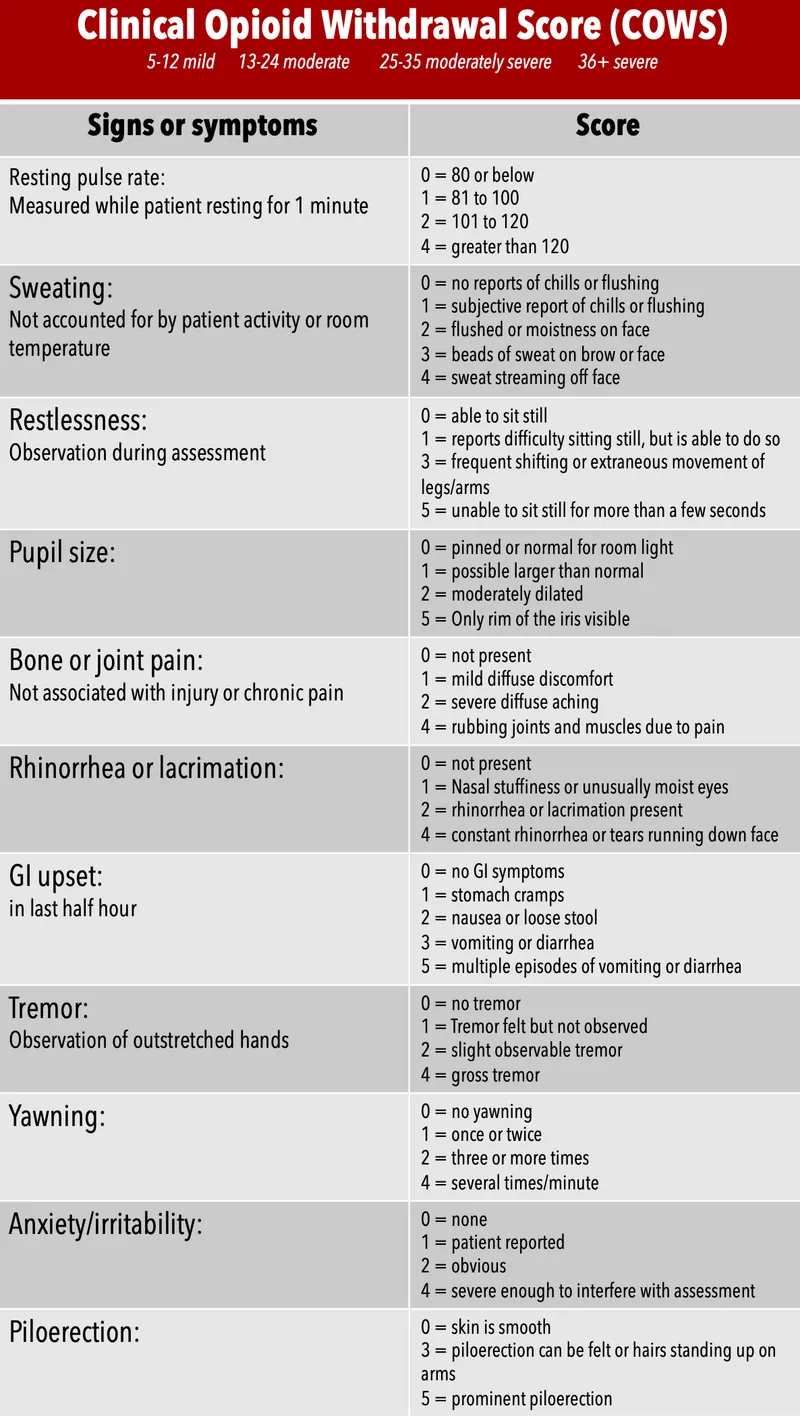
- **Lacrimation** (tearing) is a common symptom of **opioid withdrawal**, often accompanied by rhinorrhea, muscle aches, and piloerection.
- These **cholinergic rebound** symptoms are not characteristic of cocaine withdrawal, which primarily involves dopaminergic and noradrenergic system dysregulation.
*Increased sympathetic stimulation*
- Acute cocaine use directly causes increased sympathetic stimulation, resulting in **tachycardia**, **hypertension**, and dilated pupils, as seen in this patient.
- **Cocaine withdrawal**, conversely, leads to a *decrease* in sympathetic tone, often accompanied by fatigue, bradycardia, and a general depressive state, as the body rebounds from overstimulation.
Withdrawal management US Medical PG Question 4: A 28-year-old woman comes to the physician because of an 8-hour history of painful leg cramping, a runny nose, and chills. She has also had diarrhea and abdominal pain. She appears irritable and yawns frequently. Her pulse is 115/min. Examination shows cool, damp skin with piloerection. The pupils are 7 mm in diameter and equal in size. Bowel sounds are hyperactive. Deep tendon reflexes are 3+ bilaterally. Withdrawal from which of the following substances is most likely the cause of this patient's symptoms?
- A. Barbiturate
- B. Heroin (Correct Answer)
- C. Gamma-hydroxybutyric acid
- D. Cocaine
- E. Alcohol
Withdrawal management Explanation: ***Heroin***
- The constellation of symptoms including **painful muscle cramps**, **runny nose**, **chills**, **diarrhea**, **abdominal pain**, **irritability**, **frequent yawning**, **tachycardia**, **cool and damp skin with piloerection** ("goosebumps"), **dilated pupils**, **hyperactive bowel sounds**, and **hyperreflexia** is highly characteristic of **opioid withdrawal**.
- **Heroin** is a potent opioid, and its withdrawal syndrome presents with these classic signs of autonomic hyperactivity and generalized discomfort.
*Barbiturate*
- **Barbiturate withdrawal** can cause anxiety, seizures, and delirium, but it typically presents with **CNS hyperexcitability** (tremors, seizures, hallucinations) rather than the pronounced autonomic symptoms and pain described.
- While some symptoms like anxiety and tachycardia might overlap, the specific combination of **piloerection**, **dilated pupils**, and **hyperactive bowels** points away from barbiturate withdrawal.
*Gamma-hydroxybutyric acid*
- **GHB withdrawal** can manifest as anxiety, insomnia, tremors, and psychosis, but it does not typically cause the prominent **gastrointestinal distress**, **piloerection**, and **rhinorrhoea** seen in this patient.
- It’s more associated with **seizures** and **delirium tremens-like symptoms** in severe cases.
*Cocaine*
- **Cocaine withdrawal** is often characterized by **dysphoria**, fatigue, increased appetite, and psychomotor retardation, reflecting a **"crash"** after stimulant use.
- It does not typically involve the autonomic hyperactivity signs like **rhinorrhoea**, **piloerection**, or **dilated pupils** described, and the prominent physical symptoms (cramping, diarrhea) are absent.
*Alcohol*
- **Alcohol withdrawal** can cause tremors, anxiety, tachycardia, and seizures, and in severe cases, delirium tremens; however, **piloerection**, **dilated pupils**, and pronounced **gastrointestinal symptoms** (diarrhea, abdominal pain) as the primary presentation are less typical.
- The time course and specific cluster of symptoms strongly favor opioid withdrawal over alcohol withdrawal.
Withdrawal management US Medical PG Question 5: A 45-year-old man has a history of smoking 1 pack per day and drinking a six-pack of beer daily over the last ten years. He is admitted to the medical floor after undergoing a cholecystectomy. One day after the surgery, the patient states that he feels anxious and that his hands are shaking. While being checked for a clean surgical site, the patient starts shaking vigorously and loses consciousness. The patient groans and falls to the floor. His arms and legs begin to jerk rapidly and rhythmically. This episode lasts for almost five minutes, and the patient's airway, breathing, and circulation are stabilized per seizure protocol. What is the best next step for this patient?
- A. Antibiotics
- B. Morphine
- C. Chest radiograph
- D. Urinalysis
- E. Lorazepam (Correct Answer)
Withdrawal management Explanation: ***Lorazepam***
- The patient exhibits classic signs of **alcohol withdrawal syndrome**, including anxiety, tremors, and a generalized tonic-clonic seizure, which is a medical emergency.
- **Benzodiazepines** like lorazepam are the first-line treatment for alcohol withdrawal seizures due to their ability to potentiate **GABA** (gamma-aminobutyric acid) and stabilize neuronal hyperactivity.
*Antibiotics*
- There is no clinical indication for infection in this patient's presentation; the symptoms are clearly related to **alcohol withdrawal**.
- Administering antibiotics without evidence of infection contributes to **antibiotic resistance** and potential side effects.
*Morphine*
- **Opioids** like morphine can depress the respiratory system and do not address the underlying pathophysiology of alcohol withdrawal seizures.
- Administering morphine could worsen the patient's condition by masking symptoms or increasing the risk of respiratory compromise.
*Chest radiograph*
- A chest radiograph is primarily used to evaluate **pulmonary pathology** like pneumonia or aspiration, which are not the immediate concerns given the seizure and alcohol history.
- While aspiration is a risk during seizures, the immediate priority is to stop the ongoing seizure and address the underlying cause.
*Urinalysis*
- A urinalysis is used to detect urinary tract infections, kidney disease, or metabolic abnormalities, none of which are suggested by the patient's acute presentation of seizures and withdrawal symptoms.
- While it may be part of a broader workup, it is not the most urgent next step for an ongoing or recent seizure due to alcohol withdrawal.
Withdrawal management US Medical PG Question 6: A 36-year-old man is admitted to the hospital for treatment of burn wounds on his upper extremities. Analgesic therapy with an opioid drug is begun. Shortly after, the patient develops chills, diaphoresis, nausea, and abdominal pain. On further questioning, the patient reports that he has been smoking opium at home to help him ""deal with the depression and pain.” This patient was most likely given which of the following opioid drugs?
- A. Butorphanol (Correct Answer)
- B. Oxycodone
- C. Morphine
- D. Fentanyl
- E. Hydrocodone
Withdrawal management Explanation: ***Butorphanol***
- **Butorphanol** is a **mixed opioid agonist-antagonist** that acts as a **kappa (κ) receptor agonist** and **mu (μ) receptor antagonist/partial agonist**.
- In opioid-dependent patients who use **mu receptor agonists** (like opium), butorphanol can precipitate **acute opioid withdrawal** by displacing full agonists from mu receptors and blocking their effects.
- The patient's symptoms of chills, diaphoresis, nausea, and abdominal pain are classic signs of **acute opioid withdrawal syndrome**.
*Oxycodone*
- **Oxycodone** is a **full mu opioid receptor agonist** and would not precipitate withdrawal in an opioid-dependent patient.
- Administering oxycodone would provide continued mu receptor stimulation, potentially alleviating withdrawal symptoms or maintaining the patient's opioid dependence.
*Morphine*
- **Morphine** is a **full mu opioid receptor agonist** and would not cause withdrawal in an opioid-dependent individual.
- It would continue to stimulate mu opioid receptors, providing analgesia and preventing withdrawal symptoms.
*Fentanyl*
- **Fentanyl** is a potent **full mu opioid receptor agonist** and would provide continued opioid receptor stimulation.
- Its administration would prevent withdrawal and provide effective analgesia in an opioid-tolerant patient.
*Hydrocodone*
- **Hydrocodone** is a **full mu opioid receptor agonist** and would not induce withdrawal symptoms.
- Like other full agonists, it would continue mu receptor activation, providing analgesia without precipitating withdrawal.
Withdrawal management US Medical PG Question 7: A 38-year-old male is admitted to the hospital after a motor vehicle accident in which he sustained a right diaphyseal femur fracture. His medical history is significant for untreated hypertension. He reports smoking 1 pack of cigarettes per day and drinking 1 liter of bourbon daily. On hospital day 1, he undergoes open reduction internal fixation of his fracture with a femoral intramedullary nail. At what time after the patient's last drink is he at greatest risk for suffering from life-threatening effects of alcohol withdrawal?
- A. 24-48 hours
- B. 1 week
- C. Less than 24 hours
- D. 48-72 hours (Correct Answer)
- E. 5-6 days
Withdrawal management Explanation: ***48-72 hours***
- The most severe and life-threatening symptoms of alcohol withdrawal, such as **delirium tremens (DTs)**, typically manifest within **48 to 72 hours** after the last drink.
- This period is characterized by **autonomic hyperactivity**, profound confusion, hallucinations, and seizures.
*24-48 hours*
- This period may see the onset of more severe withdrawal symptoms like **hallucinations** (alcoholic hallucinosis) and **generalized tonic-clonic seizures**.
- While serious, these symptoms are generally less life-threatening than the full-blown delirium tremens that follows.
*1 week*
- By one week, if left untreated, patients would likely already have experienced the peak severity of withdrawal.
- While some mild symptoms might persist or resolve, the highest risk for acute, life-threatening events has usually passed.
*Less than 24 hours*
- Within this early timeframe, symptoms are usually milder, including **tremors, anxiety, nausea, vomiting, and insomnia**.
- These are considered "minor withdrawal symptoms" and are not typically life-threatening.
*5-6 days*
- By 5-6 days, patients who are going to develop **delirium tremens** would generally have already experienced its onset.
- The peak of severe withdrawal symptoms is usually within the 48-72 hour window, and by day 5-6, symptoms might be resolving or the patient would be in a critical state with established DTs.
Withdrawal management US Medical PG Question 8: A mother presents to the family physician with her 16-year-old son. She explains, "There's something wrong with him doc. His grades are getting worse, he's cutting class, he's gaining weight, and his eyes are often bloodshot." Upon interviewing the patient apart from his mother, he seems withdrawn and angry at times when probed about his social history. The patient denies abuse and sexual history. What initial test should be sent to rule out the most likely culprit of this patient's behavior?
- A. Complete blood count
- B. Sexually transmitted infection (STI) testing
- C. Blood culture
- D. Urine toxicology screen (Correct Answer)
- E. Slit lamp examination
Withdrawal management Explanation: ***Urine toxicology screen***
- The patient's presentation with **declining grades**, **cutting class**, **weight gain**, **bloodshot eyes**, and **irritability** are classic signs of **substance abuse** in an adolescent.
- A **urine toxicology screen** is the most appropriate initial test to detect common illicit substances, especially given the clear signs pointing towards drug use.
*Slit lamp examination*
- This test is used to examine the **anterior segment of the eye**, including the conjunctiva, cornea, iris, and lens.
- While the patient has **bloodshot eyes**, this specific test would be more relevant for ruling out ocular infections or injuries, not for diagnosing the underlying cause of systemic behavioral changes.
*Complete blood count*
- A **complete blood count (CBC)** measures different components of the blood, such as red blood cells, white blood cells, and platelets.
- A CBC is a general health indicator and while it can detect infections or anemia, it is not specific or sensitive enough to identify the cause of the behavioral changes described.
*Sexually transmitted infection (STI) testing*
- Although the patient denies sexual history, all adolescents presenting with certain risk factors or symptoms may warrant STI testing in a broader health assessment.
- However, in this scenario, the primary cluster of symptoms (poor grades, cutting class, bloodshot eyes, irritability) points more directly to substance abuse than to an STI.
*Blood culture*
- A **blood culture** is used to detect the presence of bacteria or other microorganisms in the bloodstream, indicating a systemic infection (sepsis).
- The patient's symptoms are not indicative of an acute bacterial bloodstream infection, and a blood culture would not be the initial test for the presented behavioral changes.
Withdrawal management US Medical PG Question 9: A 30-year-old man presents to his family physician admitting to using heroin. He says he started using about 6-months ago when his back pain medication ran out. At first, he says he would borrow his wife’s Percocet but, eventually, that ran out and he had to find a different source. Since then, he has been having more and more issues related to his heroin use, and it has started to affect his work and home life. He is concerned that, if he continues like this, he might end up in real trouble. He denies sharing needles and is sincerely interested in quitting. He recalls trying to quit last month but recounts how horrible the withdrawal symptoms were. Because of this and the strong cravings, he relapsed shortly after his initial attempt. Methadone maintenance therapy is prescribed. Which of the following would most likely be the most important benefit of this new treatment plan in this patient?
- A. Decreases methadone dependence
- B. Euphoria without the side effects
- C. Prevention of withdrawal symptoms and reduced cravings (Correct Answer)
- D. Reduced risk of hepatitis B and C transmission
- E. Improved interpersonal relationships
Withdrawal management Explanation: ***Prevention of withdrawal symptoms and reduced cravings***
- **Methadone maintenance therapy** is a long-acting μ-opioid receptor agonist that prevents withdrawal symptoms and reduces cravings—this is the **primary therapeutic benefit** and mechanism of action.
- By providing a stable, long-acting opioid, methadone eliminates the cycle of withdrawal and drug-seeking behavior that characterizes heroin addiction.
- This patient's previous quit attempt failed specifically due to **"horrible withdrawal symptoms"** and **strong cravings**, making this the most directly relevant benefit for his situation.
- All other benefits of methadone maintenance (improved functioning, better relationships, reduced risk behaviors) are **secondary consequences** that stem from this primary pharmacological effect.
- Evidence-based guidelines consistently identify withdrawal prevention and craving reduction as the core therapeutic goals of opioid agonist therapy.
*Improved interpersonal relationships*
- While this is an important **downstream benefit** of successful methadone maintenance, it is an indirect consequence rather than the primary therapeutic effect.
- Improved relationships result FROM the stabilization achieved through withdrawal prevention and craving reduction, not as a direct pharmacological action.
- Though clinically meaningful, this represents a **psychosocial outcome** rather than the most important direct benefit of the medication itself.
*Decreases methadone dependence*
- This is **incorrect**—methadone itself is an opioid agonist and patients on maintenance therapy develop **physical dependence** on methadone.
- The goal is to substitute unstable illicit opioid use (heroin) with stable, medically supervised opioid therapy (methadone), not to eliminate opioid dependence immediately.
- Methadone maintenance is harm reduction, not abstinence-based treatment initially.
*Euphoria without the side effects*
- Methadone is **not intended to produce euphoria**—it is administered at stable doses to maintain normal functioning without intoxication.
- Its slow onset and long duration of action when taken orally minimize the "rush" or euphoric effects associated with rapid-acting opioids like heroin.
- The goal is stabilization and normal functioning, not achieving a "high."
*Reduced risk of hepatitis B and C transmission*
- This is a valuable **harm reduction benefit**, particularly for those who inject drugs and share needles.
- However, this patient specifically **denies sharing needles**, making this less relevant to his individual case.
- More importantly, this is a secondary benefit that occurs as a result of reduced injection drug use, which itself results from the primary effect of withdrawal prevention and craving reduction.
Withdrawal management US Medical PG Question 10: A 23-year-old woman is admitted to the inpatient psychiatry unit after her boyfriend reported she was “acting funny and refusing to talk.” The patient’s boyfriend states that he came home from work and found the patient sitting up in bed staring at the wall. When he said her name or waved his hand in front of her, she did not respond. When he tried to move her, she would remain in whatever position she was placed. The patient’s temperature is 99°F (37.2°C), blood pressure is 122/79 mmHg, pulse is 68/min, and respirations are 12/min with an oxygen saturation of 98% O2 on room air. During the physical exam, the patient is lying on the bed with her left arm raised and pointing at the ceiling. She resists any attempt to change her position. The patient remains mute and ignores any external stimuli. The patient’s medical history is significant for depression. She was recently switched from phenelzine to fluoxetine. Which of the following is the best initial therapy?
- A. Electroconvulsive therapy
- B. Lorazepam (Correct Answer)
- C. Haloperidol
- D. Cyproheptadine
- E. Benztropine
Withdrawal management Explanation: **Lorazepam**
- The patient presents with classic symptoms of **catatonia**, including **mutism**, **waxy flexibility**, and **posturing**, following a medication change from phenelzine (MAOI) to fluoxetine (SSRI), which could potentially precipitate catatonia or serotonin syndrome.
- **Benzodiazepines**, particularly lorazepam, are the **first-line treatment** for catatonia, often showing a rapid and dramatic response.
*Electroconvulsive therapy*
- While **ECT** is a highly effective treatment for severe catatonia, especially when unresponsive to benzodiazepines, it is typically considered a **second-line intervention** or for cases involving medical instability.
- Given the strong initial efficacy and safety profile of benzodiazepines, they are preferred as the first step before proceeding to ECT.
*Haloperidol*
- **Antipsychotics** like haloperidol are generally **contraindicated** in catatonia, as they can sometimes worsen the symptoms or even induce **neuroleptic malignant syndrome (NMS)**, which shares some features with severe catatonia.
- NMS is a serious condition with high mortality, and introducing an antipsychotic in a catatonic patient could be dangerous.
*Cyproheptadine*
- **Cyproheptadine** is a **serotonin antagonist** used primarily in the treatment of **serotonin syndrome**, which involves symptoms like hyperthermia, agitation, and hyperreflexia.
- While the medication change could raise suspicion for serotonin syndrome, the clinical picture of **waxy flexibility, mutism, and posturing** is much more indicative of catatonia, for which cyproheptadine is not an effective treatment.
*Benztropine*
- **Benztropine** is an **anticholinergic medication** primarily used to treat **extrapyramidal symptoms (EPS)** caused by antipsychotics, such as **dystonia** or **parkinsonism**.
- The patient's symptoms are not indicative of EPS, and benztropine has no role in the treatment of catatonia.
More Withdrawal management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.