Stimulant use disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Stimulant use disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Stimulant use disorders US Medical PG Question 1: A 32-year-old man is brought to the emergency department because he was found stumbling in the street heedless of oncoming traffic. On arrival, he is found to be sluggish and has slow and sometimes incoherent speech. He is also drowsy and falls asleep several times during questioning. Chart review shows that he has previously been admitted after getting a severe cut during a bar fight. Otherwise, he is known to be intermittently homeless and has poorly managed diabetes. Serum testing reveals the presence of a substance that increases the duration of opening for an important channel. Which of the following symptoms may be seen if the most likely substance in this patient is abruptly discontinued?
- A. Tremors
- B. Insomnia
- C. Delayed delirium
- D. Piloerection
- E. Seizures (Correct Answer)
Stimulant use disorders Explanation: ***Seizures***
- This patient presents with symptoms of **central nervous system (CNS) depression** (sluggish, incoherent speech, drowsiness) and a history suggestive of **substance abuse** (homelessness, bar fight).
- The key clue is that the substance **increases the duration of opening** of the GABA-A receptor channel, which specifically describes **barbiturates** (benzodiazepines increase the **frequency** of opening, not duration).
- Abrupt discontinuation of barbiturates can lead to life-threatening **withdrawal seizures** due to CNS hyperexcitability when GABAergic inhibition is suddenly removed [1].
- This is the most critical and potentially fatal complication of barbiturate withdrawal.
*Tremors*
- While **tremors** can occur during withdrawal from CNS depressants, they are a less severe symptom compared to seizures.
- Tremors are common in withdrawal syndromes but do not represent the most life-threatening risk in acute barbiturate withdrawal.
*Insomnia*
- **Insomnia** is a common symptom of withdrawal from CNS depressants due to rebound CNS hyperactivity [1].
- However, compared to seizures, insomnia is not life-threatening and is a less critical feature of barbiturate withdrawal.
*Delayed delirium*
- **Delirium** can occur during severe withdrawal, particularly **delirium tremens** in alcohol withdrawal.
- While delirium may develop, the most immediate and severe risk for barbiturate withdrawal is seizures, which can occur within hours to days of cessation.
*Piloerection*
- **Piloerection** (goosebumps) is a classic symptom of **opioid withdrawal**, resulting from sympathetic nervous system activation.
- This symptom is **not** characteristic of withdrawal from barbiturates or other GABAergic substances, making it an incorrect choice.
Stimulant use disorders US Medical PG Question 2: A 24-year-old graduate student is brought to the emergency department by her boyfriend because of chest pain that started 90 minutes ago. Her boyfriend says she has been taking medication to help her study for an important exam and has not slept in several days. On examination, she is diaphoretic, agitated, and attempts to remove her IV lines and ECG leads. Her temperature is 37.6°C (99.7°F), pulse is 128/min, and blood pressure is 163/97 mmHg. Her pupils are dilated. The most appropriate next step in management is the administration of which of the following?
- A. Lorazepam (Correct Answer)
- B. Ketamine
- C. Haloperidol
- D. Activated charcoal
- E. Dantrolene
Stimulant use disorders Explanation: ***Lorazepam***
- This patient presents with symptoms highly suggestive of **sympathomimetic toxicity** (agitation, tachycardia, hypertension, dilated pupils, diaphoresis) likely due to stimulant abuse for studying. **Benzodiazepines** like lorazepam are the first-line treatment to manage agitation, tachycardia, and hypertension in this setting.
- Lorazepam helps by **calming the central nervous system** and reducing the sympathetic overdrive, thereby mitigating the cardiovascular and neurological effects of stimulant toxicity.
*Ketamine*
- Ketamine is a **dissociative anesthetic** that typically increases heart rate and blood pressure, which would exacerbate the patient's existing sympathetic hyperactivity and cardiovascular instability.
- It is not indicated for the management of stimulant-induced agitation or catecholamine surge.
*Haloperidol*
- Haloperidol is an **antipsychotic** that can prolong the **QT interval** and potentially lower the seizure threshold, effects that can be dangerous in stimulant toxicity.
- It does not directly address the underlying sympathetic overdrive and can worsen hyperthermia with its anticholinergic properties.
*Activated charcoal*
- Activated charcoal is used to **prevent absorption** of toxins from the gastrointestinal tract, but it is typically only effective if given within 1-2 hours of ingestion. This patient's symptoms started 90 minutes ago, implying some absorption has already occurred, and her agitated state makes oral administration risky if airway protection is not ensured.
- It is also contraindicated in patients with an unprotected airway due to the risk of aspiration, and benzodiazepines are needed first to control agitation and protect the airway.
*Dantrolene*
- Dantrolene is a **skeletal muscle relaxant** used primarily to treat **malignant hyperthermia** and **neuroleptic malignant syndrome**.
- While this patient has some signs of hyperthermia, dantrolene is not the first-line treatment for stimulant-induced hyperthermia, which is primarily managed by controlling agitation and sympathetic overdrive with benzodiazepines and external cooling.
Stimulant use disorders US Medical PG Question 3: A 23-year-old man is brought to the emergency department by the police for impaired cognition and agitation after being struck in the head at a local nightclub. The patient refuses to respond to questions and continues to be markedly agitated. An alcoholic smell is noted. His temperature is 36.9°C (98.4°F), pulse is 104/min, respirations are 24/min, and blood pressure is 148/95 mm Hg. He is confused and oriented only to person. Neurological examination shows miosis and nystagmus but is quickly aborted after the patient tries to attack several members of the care team. CT scan of the head shows no abnormalities. Ingestion of which of the following substances most likely explains this patient's symptoms?
- A. Lysergic acid diethylamide
- B. Phencyclidine (Correct Answer)
- C. Alcohol
- D. Heroin
- E. Methamphetamine
Stimulant use disorders Explanation: ***Phencyclidine***
- **Phencyclidine (PCP)** intoxication is characterized by a combination of severe **agitation**, **aggression**, impaired cognition, nystagmus (vertical or horizontal), and miotic pupils, which precisely matches the patient's presentation.
- The patient's violent behavior and refusal to cooperate with examination despite an initial head injury also align with the dissociative and stimulant effects of PCP.
*Lysergic acid diethylamide*
- **LSD** typically causes hallucinations, altered perceptions, and dilated pupils (**mydriasis**), rather than the miotic pupils and marked aggression seen in this patient.
- While agitation can occur with LSD, the extreme violence and neurological signs like nystagmus point away from it as the primary cause.
*Alcohol*
- While alcohol can cause impaired cognition and agitation, the presence of **miosis** and **nystagmus** in this agitated state, especially given the degree of disorientation and aggression, is more characteristic of other substances.
- The "alcoholic smell" could be a red herring or co-ingestion, but the overall clinical picture is not solely attributable to acute alcohol intoxication.
*Heroin*
- **Heroin (opioid)** overdose typically causes **sedation**, respiratory depression, and pinpoint pupils (**miosis**), which is contrary to the agitation, aggression, and elevated vital signs described.
- The patient's high blood pressure and pulse are inconsistent with opioid effects.
*Methamphetamine*
- **Methamphetamine** intoxication leads to agitation, paranoia, and elevated vital signs (tachycardia, hypertension), but typically causes **mydriasis (dilated pupils)**, not miosis.
- Although agitation and aggression are significant features, the pupillary findings help differentiate it from PCP.
Stimulant use disorders US Medical PG Question 4: A 55-year-old woman comes to the physician because of involuntary hand movements that improve with alcohol consumption. Physical examination shows bilateral hand tremors that worsen when the patient is asked to extend her arms out in front of her. The physician prescribes a medication that is associated with an increased risk of bronchospasms. This drug has which of the following immediate effects on the cardiovascular system?
Stroke volume | Heart rate | Peripheral vascular resistance
- A. ↓ ↓ ↓
- B. ↓ ↓ ↑ (Correct Answer)
- C. ↓ ↑ ↑
- D. ↑ ↑ ↑
- E. ↑ ↑ ↓
Stimulant use disorders Explanation: ***↓ ↓ ↑***
- This patient likely has **essential tremor**, which is characterized by **bilateral hand tremors** that improve with alcohol and worsen with intention (postural tremor). The prescribed medication is a **beta-blocker** (e.g., propranolol), which is associated with an increased risk of bronchospasms due to blocking **beta-2 receptors** in the airways.
- Beta-blockers **decrease heart rate** (negative chronotropic effect) and **stroke volume** (negative inotropic effect) by blocking beta-1 receptors in the heart, reducing cardiac output.
- **Peripheral vascular resistance increases** acutely due to: (1) **unopposed alpha-1 adrenergic tone** in blood vessels (loss of beta-2 mediated vasodilation), and (2) baroreceptor-mediated reflex vasoconstriction in response to decreased cardiac output. This helps maintain blood pressure despite reduced cardiac output.
*↓ ↓ ↓*
- While beta-blockers decrease **heart rate** and **stroke volume**, peripheral vascular resistance does not decrease acutely. A decrease in all three parameters would cause severe hypotension.
- The loss of beta-2 receptor-mediated vasodilation and baroreceptor reflexes lead to increased, not decreased, peripheral vascular resistance.
*↓ ↑ ↑*
- Beta-blockers **decrease heart rate** through beta-1 blockade, not increase it. This is their primary cardiac mechanism of action.
- An increase in heart rate would be expected with sympathomimetic drugs or anticholinergics, not beta-blockers.
*↑ ↑ ↑*
- This combination indicates increased cardiovascular activity, which is the opposite effect of **beta-blockers**.
- Beta-blockers reduce heart rate and stroke volume by blocking beta-1 receptors; they do not increase these parameters.
- This pattern would suggest sympathetic activation or administration of an adrenergic agonist.
*↑ ↑ ↓*
- Beta-blockers **decrease** (not increase) both heart rate and stroke volume through beta-1 receptor blockade.
- While decreased peripheral vascular resistance occurs with vasodilators, beta-blockers acutely **increase** PVR due to unopposed alpha-adrenergic tone.
Stimulant use disorders US Medical PG Question 5: A 25-year-old man is brought to the emergency department by police for aggressive behavior. The patient is combative and shouts sexually aggressive remarks at the nursing staff. While obtaining the patient’s vitals, it is noted that he has markedly dilated pupils. His temperature is 98.2°F (36.8°C), pulse is 112/min, blood pressure is 130/70 mmHg, respirations are 18/min, and oxygen saturation is 98% on room air. Urine toxicology is obtained and sent off. Physical exam is notable for an energetic patient with dilated pupils and increased sweating. The patient spends the night in the emergency department. In the morning the patient is withdrawn and has a notable depressed affect. He apologizes for his behavior the previous night and states that he is concerned about his problem and wants help. Which of the following is appropriate management of this patient?
- A. Medical detoxification program
- B. Motivational interviewing session
- C. Discharge with outpatient follow-up
- D. Psychiatric evaluation and assessment
- E. Referral to substance abuse treatment program (Correct Answer)
Stimulant use disorders Explanation: ***Referral to substance abuse treatment program***
- The patient exhibits classic features of **stimulant intoxication** (aggression, dilated pupils, tachycardia, sweating) followed by the typical **"crash" phase** with withdrawal and depressed affect, most consistent with cocaine or amphetamine use.
- Most importantly, the patient **expresses desire for help** the next morning—this represents a **critical window of opportunity** for intervention while motivation is high.
- **Stimulant withdrawal is not medically dangerous** and does not require medical detoxification (unlike alcohol or benzodiazepine withdrawal), so the patient can be directly referred to a substance abuse treatment program.
- **Immediate referral** is the standard of care to capitalize on the patient's readiness for change, as delaying treatment risks losing motivation and potential relapse.
*Medical detoxification program*
- Medical detoxification is **not indicated for stimulant use disorder** because stimulant withdrawal, while uncomfortable (fatigue, depression, increased appetite, vivid dreams), is **not medically dangerous** and has no life-threatening complications.
- Unlike alcohol or benzodiazepine withdrawal, there are **no medications required** for stimulant withdrawal management, and symptoms are self-limited.
- The patient is already past the acute intoxication phase and does not require medical detoxification before entering treatment.
*Motivational interviewing session*
- While motivational interviewing is a valuable evidence-based technique to enhance intrinsic motivation for behavior change, it is typically **a component within a comprehensive treatment program** rather than standalone definitive management.
- The patient has **already expressed motivation** ("concerned about his problem and wants help"), so the priority is to act on this motivation with immediate treatment referral rather than further motivational work.
*Discharge with outpatient follow-up*
- Simply discharging with outpatient follow-up is **insufficient** and risks losing the patient during this critical window of motivation.
- Patients with substance use disorders often have **poor follow-up rates** when not immediately connected to treatment, and motivation can wane quickly after the acute consequences resolve.
- More structured and immediate intervention is needed given the severity of the presentation and expressed desire for help.
*Psychiatric evaluation and assessment*
- While psychiatric comorbidities are common in patients with substance use disorders and should eventually be assessed, this is **not the immediate priority** when a patient is requesting help for substance abuse.
- Comprehensive psychiatric evaluation can be performed **within the substance abuse treatment program** where co-occurring disorders can be addressed simultaneously.
- The primary presenting problem is substance use, and immediate treatment engagement takes precedence.
Stimulant use disorders US Medical PG Question 6: A 19-year-old man presents to a psychiatrist for the management of substance abuse. He reports that he started using the substance 2 years ago and that he smokes it after sprinkling it on his cigarette. He describes that after smoking the substance, he feels excited and as if he does not belong to himself. He also reports that when he is in his room, he sees vivid colors on the walls after using the substance; if he listens to his favorite music, he clearly sees colors and shapes in front of his eyes. There is no history of alcohol or nicotine abuse. The psychiatrist goes through his medical records and notes that he had presented with acute substance intoxication 1 month prior. At that point, his clinical features included delusions, amnesia, generalized erythema of his skin, tachycardia, hypertension, dilated pupils, dysarthria, and ataxia. Which of the following signs is also most likely to have been present on physical examination while the man was intoxicated with the substance?
- A. Increased sensitivity to pain
- B. Excessive perspiration
- C. Hyporeflexia
- D. Generalized hypotonia
- E. Nystagmus (Correct Answer)
Stimulant use disorders Explanation: ***Nystagmus***
- The patient's symptoms of **dissociation** ("feels as if he does not belong to himself"), **visual hallucinations** (seeing vivid colors and shapes), delusions, amnesia, tachycardia, hypertension, dilated pupils, dysarthria, and ataxia are highly characteristic of **phencyclidine (PCP) intoxication**.
- **Nystagmus**, particularly **horizontal and vertical nystagmus**, is a classic and frequently observed sign in PCP intoxication due to its effects on the **cerebellum** and vestibular system.
*Increased sensitivity to pain*
- PCP is known for its **analgesic** and **anesthetic** properties, leading to **decreased sensitivity to pain**, not increased.
- This effect contributes to the potential for self-injurious behavior during intoxication.
*Excessive perspiration*
- While other stimulants can cause diaphoresis, PCP intoxication more typically presents with **dry skin** or normal perspiration despite **hyperthermia** as it interferes with cholinergic thermoregulation.
- The described **generalized erythema** suggests **vasodilation**, but **dry skin** is more often associated with the anticholinergic effects that can accompany PCP.
*Hyporeflexia*
- PCP intoxication commonly causes **hyperreflexia** and **spasticity**, not hyporeflexia, due to its excitatory effects on the **central nervous system**.
- **Muscle rigidity** and **seizures** are also possible, further indicating CNS excitation.
*Generalized hypotonia*
- PCP typically leads to **increased muscle tone** and **rigidity**, not generalized hypotonia.
- The patient's presentation with **ataxia** and **dysarthria** suggests cerebellar involvement, but this usually manifests with motor incoordination rather than widespread flaccidity.
Stimulant use disorders US Medical PG Question 7: A 65-year old man comes to the emergency department because of altered mental status for 1 day. He has had headaches, severe nausea, vomiting, and diarrhea for 2 days. He has a history of hypertension, insomnia, and bipolar disorder. His medications include lisinopril, fluoxetine, atorvastatin, lithium, olanzapine, and alprazolam. His temperature is 37.2 °C (99.0 °F), pulse is 90/min, respirations are 22/min, and blood pressure is 102/68 mm Hg. He is somnolent and confused. His mucous membranes are dry. Neurological examination shows dysarthria, decreased muscle strength throughout, and a coarse tremor of the hands bilaterally. The remainder of the examination shows no abnormalities. In addition to IV hydration and electrolyte supplementation, which of the following is the next best step in management?
- A. Bowel irrigation
- B. Intravenous diazepam
- C. Oral cyproheptadine
- D. Intravenous dantrolene
- E. Hemodialysis (Correct Answer)
Stimulant use disorders Explanation: ***Hemodialysis***
- This patient presents with symptoms consistent with **severe lithium toxicity** (altered mental status, somnolence, confusion, dysarthria, decreased muscle strength, coarse tremor) likely exacerbated by dehydration due to nausea, vomiting, and diarrhea.
- **Hemodialysis** is indicated for severe lithium toxicity, especially when plasma lithium levels are very high (>4.0 mEq/L), there are signs of cerebellar toxicity or seizures, or if renal impairment prevents adequate lithium excretion.
*Bowel irrigation*
- **Whole-bowel irrigation** is primarily used for large ingestions of sustained-release or enteric-coated medications, or substances not adsorbed by activated charcoal.
- It is generally *not* effective for removing lithium, as lithium is rapidly and completely absorbed from the gastrointestinal tract.
*Intravenous diazepam*
- **Benzodiazepines** like diazepam are useful for managing seizures or severe agitation associated with drug toxicities but do not address the underlying cause of lithium toxicity by removing the drug from the body.
- While agitation and seizures might occur in severe lithium toxicity, the primary initial step in severe cases is to remove the excess lithium.
*Oral cyproheptadine*
- **Cyproheptadine** is an antihistamine with antiserotonergic properties, used in the treatment of **serotonin syndrome**.
- This patient's clinical presentation is classic for **lithium toxicity**, not serotonin syndrome, although fluoxetine can contribute to serotonin syndrome, the tremor and neurological picture coupled with lithium use points to lithium toxicity.
*Intravenous dantrolene*
- **Dantrolene** is a muscle relaxant primarily used for conditions like **neuroleptic malignant syndrome** (NMS) or malignant hyperthermia due to its direct action on skeletal muscle.
- It is not indicated for treating the central nervous system effects or removal of lithium in lithium toxicity.
Stimulant use disorders US Medical PG Question 8: A 24-year-old man is brought to the emergency department by his roommates for aggressive and unusual behavior. His roommates state that he has been under a lot of stress lately from his final exams and has been more reclusive. They state that this evening he was very irritable and was yelling at his computer prior to breaking it, followed by him spending several hours at the gym. His temperature is 101°F (38.3°C), blood pressure is 137/98 mmHg, pulse is 120/min, respirations are 23/min, and oxygen saturation is 99% on room air. Physical exam is notable for an irritable young man. Cardiopulmonary exam is notable for tachycardia and bilateral clear breath sounds. Neurological exam reveals dilated pupils. The patient is notably diaphoretic and speaks very rapidly during the physical exam and is aggressive. He is given haloperidol, diphenhydramine, and diazepam for sedation and placed in soft restraints. His symptoms resolved over the next 10 hours in the emergency department. Which of the following is the most likely diagnosis?
- A. Cocaine intoxication (Correct Answer)
- B. Phencyclidine intoxication
- C. Schizophrenia
- D. Caffeine intoxication
- E. Lisdexamfetamine intoxication
Stimulant use disorders Explanation: ***Cocaine intoxication***
- The patient's presentation with **agitation, aggression, dilated pupils, tachycardia, hypertension, diaphoresis, and rapid speech** is highly consistent with stimulant intoxication, especially **cocaine**.
- The **rapid resolution of symptoms over 10 hours** supports cocaine intoxication, as cocaine has a short half-life (~1 hour) with effects typically resolving within a few hours after cessation.
*Phencyclidine intoxication*
- While PCP can cause aggression, agitation, and dilated pupils, it is classically associated with **nystagmus (horizontal or vertical)**, which is not mentioned here.
- PCP intoxication often presents with **dissociative symptoms** and a severe level of unpredictable violence or bizarre behavior not fully described.
*Schizophrenia*
- The **acute onset of symptoms** in a previously functioning individual, particularly with a clear trigger (stress), is less typical for schizophrenia, which usually has a more insidious prodromal phase.
- The **rapid and complete resolution** of symptoms within hours strongly argues against a primary psychotic disorder like schizophrenia, which requires longer-term treatment.
*Caffeine intoxication*
- While high doses of caffeine can cause **tachycardia, anxiety, and agitation**, it rarely leads to the severe **aggression and property damage** described in this case.
- The degree of physical symptoms like **dilated pupils, hypertension, and significant diaphoresis** would be unusually severe for typical caffeine intoxication.
*Lisdexamfetamine intoxication*
- Lisdexamfetamine (Vyvanse) is an amphetamine prodrug that shares many symptoms with cocaine intoxication, including **agitation, aggression, dilated pupils, and sympathetic overdrive**.
- However, amphetamines have a **much longer duration of action (8-12+ hours)** compared to cocaine, so complete symptom resolution within 10 hours would be less typical for amphetamine intoxication, which often requires longer observation periods.
Stimulant use disorders US Medical PG Question 9: A 28-year-old man is brought to the emergency department after he was found half dressed and incoherent in the middle of the road. In the emergency department he states that he has not slept for 36 hours and that he has incredible ideas that will make him a billionaire within a few months. He also states that secret agents from Russia are pursuing him and that he heard one of them speaking through the hospital intercom. His past medical history is significant only for a broken arm at age 13. On presentation, his temperature is 102.2°F (39°C), blood pressure is 139/88 mmHg, pulse is 112/min, and respirations are 17/min. Physical exam reveals pupillary dilation and psychomotor agitation. Which of the following mechanisms is most likely responsible for this patient's symptoms?
- A. N-methyl-D-aspartate receptor antagonist
- B. Gamma-aminobutyric acid receptor agonist
- C. Increased biogenic amine release (Correct Answer)
- D. 5-HT receptor agonist
- E. Opioid receptor agonist
Stimulant use disorders Explanation: ***Increased biogenic amine release***
- The patient exhibits a classic constellation of symptoms consistent with **stimulant intoxication**, including **psychomotor agitation**, **pupillary dilation**, **tachycardia**, **hyperthermia**, **insomnia**, **grandiosity**, and **paranoia**.
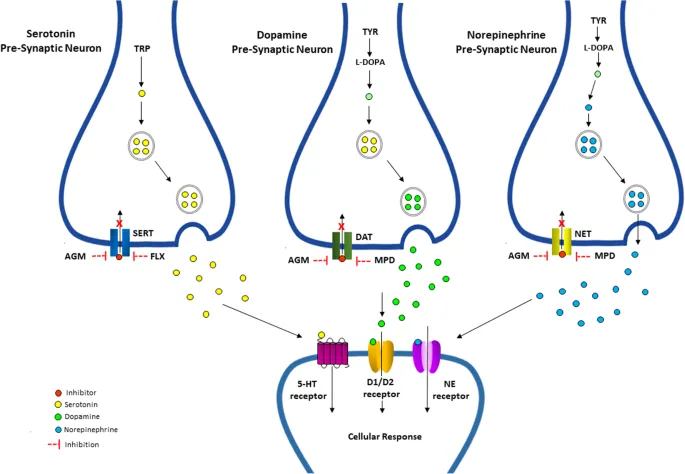
- Stimulants like **amphetamines** and **cocaine** primarily exert their effects by increasing the release and inhibiting the reuptake of **biogenic amines** (dopamine, norepinephrine, serotonin) in the brain, leading to an exaggerated sympathetic response and altered mental status.
*N-methyl-D-aspartate receptor antagonist*
- **NMDA receptor antagonists** (e.g., phencyclidine - PCP, ketamine) are associated with dissociative symptoms, nystagmus, and sometimes aggression, but generally do not present with the prominent **hyperthermia** and grandiosity seen here.
- While they can cause psychotic symptoms, the specific combination of signs points more strongly to **stimulant intoxication**.
*Gamma-aminobutyric acid receptor agonist*
- **GABA receptor agonists** (e.g., benzodiazepines, barbiturates) cause **CNS depression**, sedation, respiratory depression, and ataxia.
- These effects are contrary to the patient's presentation of **agitation**, **increased heart rate**, and **hyperthermia**.
*5-HT receptor agonist*
- While drugs like **LSD** and **MDMA** (ecstasy) act as 5-HT receptor agonists and can cause hallucinations and altered perception, the prominent **paranoia**, **grandiosity**, and **significant hyperthermia** in this scenario are more characteristic of stimulant toxicity, which involves a broader increase in biogenic amine release beyond just serotonin.
- MDMA, in particular, can cause hyperthermia, but the full clinical picture is more suggestive of traditional stimulants.
*Opioid receptor agonist*
- **Opioid receptor agonists** (e.g., heroin, morphine) typically cause **CNS depression**, **miosis** (pinpoint pupils), respiratory depression, and sedation.
- These effects are the **opposite** of the patient's symptoms of pupillary dilation, agitation, and hyperthermia.
Stimulant use disorders US Medical PG Question 10: A 22-year-old man presents to the emergency department with anxiety. The patient states that he is very anxious and has not been able to take his home anxiety medications. He is requesting to have his home medications administered. The patient has a past medical history of anxiety and depression. His current medications include clonazepam, amitriptyline, and lorazepam. Notably, the patient has multiple psychiatric providers who currently care for him. His temperature is 99.2°F (37.3°C), blood pressure is 130/85 mmHg, pulse is 112/min, respirations are 22/min, and oxygen saturation is 100% on room air. Physical exam is notable for an anxious, sweating, and tremulous young man who becomes more confused during his stay in the emergency department. Which of the following should be given to this patient?
- A. Diazepam (Correct Answer)
- B. Sodium bicarbonate
- C. Flumazenil
- D. Supportive therapy and monitoring
- E. Midazolam
Stimulant use disorders Explanation: ***Diazepam***
- This patient presents with classic **benzodiazepine withdrawal syndrome**: anxiety, tremors, sweating, tachycardia, tachypnea, and progressive confusion after being unable to take his home benzodiazepines (clonazepam and lorazepam).
- Benzodiazepine withdrawal is a **medical emergency** that can progress to seizures, delirium, and death if untreated.
- **Diazepam** is the preferred treatment due to its **long half-life**, which provides smooth, sustained benzodiazepine receptor activity and prevents withdrawal progression.
- The autonomic instability (elevated pulse and respiratory rate) and neurological symptoms (tremors, confusion) require immediate benzodiazepine administration, not just supportive care.
*Supportive therapy and monitoring*
- While monitoring is important, **supportive care alone is inadequate** for benzodiazepine withdrawal with autonomic instability and confusion.
- Untreated benzodiazepine withdrawal can rapidly progress to **seizures, severe delirium, and cardiovascular collapse**.
- The objective signs (tachycardia, tremors, sweating, confusion) indicate physiological withdrawal, not simply anxiety or drug-seeking behavior.
- Active treatment with benzodiazepines is the **standard of care** to prevent life-threatening complications.
*Sodium bicarbonate*
- Sodium bicarbonate treats **metabolic acidosis** or specific overdoses (e.g., tricyclic antidepressants, aspirin).
- There is no indication of acidosis or TCA toxicity in this presentation; the patient has withdrawal symptoms, not overdose.
*Flumazenil*
- Flumazenil is a benzodiazepine antagonist that **reverses benzodiazepine effects** in acute overdose.
- It is **absolutely contraindicated** in patients with chronic benzodiazepine use or dependence, as it can precipitate **severe withdrawal, seizures, and status epilepticus**.
- This patient needs benzodiazepine administration, not reversal.
*Midazolam*
- While midazolam is a benzodiazepine that could treat withdrawal acutely, its **short half-life** makes it less ideal for managing withdrawal syndrome.
- **Diazepam or chlordiazepoxide** (long-acting agents) are preferred for withdrawal management as they provide sustained coverage and smoother tapering.
- Midazolam would require frequent redosing and carries higher risk of rebound withdrawal.
More Stimulant use disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.