Alcohol use disorder US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Alcohol use disorder. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Alcohol use disorder US Medical PG Question 1: One hour after undergoing an uncomplicated laparoscopic appendectomy, a 22-year-old man develops agitation and restlessness. He also has tremors, diffuse sweating, headache, and nausea with dry heaves. One liter of lactated ringer's was administered during the surgery and he had a blood loss of approximately 100 mL. His urine output was 100 mL. His pain has been controlled with intravenous morphine. He was admitted to the hospital 3 days ago and has not eaten in 18 hours. He has no history of serious illness. He is a junior in college. His mother has Hashimoto's thyroiditis. He has experimented with intravenous illicit drugs. He drinks 3 beers and 2 glasses of whiskey daily during the week and more on the weekends with his fraternity. He appears anxious. His temperature is 37.4°C (99.3°F), pulse is 120/min, respirations are 19/min, and blood pressure is 142/90 mm Hg. He is alert and fully oriented but keeps asking if his father, who is not present, can leave the room. Mucous membranes are moist and the skin is warm. Cardiac examination shows tachycardia and regular rhythm. The lungs are clear to auscultation. His abdomen has three port sites with clean and dry bandages. His hands tremble when his arms are extended with fingers spread apart. Which of the following is the most appropriate next step in management?
- A. Administer intravenous lorazepam (Correct Answer)
- B. Administer 5% dextrose in 1/2 normal saline
- C. Administer intravenous naloxone
- D. Administer intravenous propranolol
- E. Administer intravenous dexamethasone
Alcohol use disorder Explanation: ***Administer intravenous lorazepam***
- The patient's symptoms (agitation, restlessness, tremors, sweating, tachycardia, hypertension, and anxiety) occurring post-surgery in a patient with a history of heavy alcohol use are highly suggestive of alcohol withdrawal syndrome.
- Benzodiazepines like lorazepam are the first-line treatment for alcohol withdrawal due to their sedative, anxiolytic, and anticonvulsant properties, which can prevent progression to more severe complications like seizures or delirium tremens.
*Administer 5% dextrose in 1/2 normal saline*
- This solution is primarily used to address dehydration and provide some caloric support, but it does not directly manage the neuroexcitatory symptoms of alcohol withdrawal.
- While supportive care including fluids is important, addressing the underlying alcohol withdrawal is the immediate priority.
*Administer intravenous naloxone*
- Naloxone is an opioid antagonist used to reverse opioid overdose.
- The patient's symptoms are inconsistent with opioid overdose; in fact, he is experiencing agitation and autonomic hyperactivity, which are the opposite of opioid effects.
*Administer intravenous propranolol*
- Propranolol is a beta-blocker that can help control some autonomic symptoms like tachycardia and hypertension, but it does not address the underlying neuroexcitability or prevent seizures associated with alcohol withdrawal.
- It should not be used as monotherapy for alcohol withdrawal and should be given cautiously, often after benzodiazepines, especially in patients with respiratory concerns.
*Administer intravenous dexamethasone*
- Dexamethasone is a potent corticosteroid used for anti-inflammatory or immunosuppressive effects and in conditions like cerebral edema or adrenal insufficiency.
- It has no role in the management of alcohol withdrawal syndrome.
Alcohol use disorder US Medical PG Question 2: A 42-year-old homeless man is brought to the emergency room after he was found unconscious in a park. He has alcohol on his breath and is known to have a history of chronic alcoholism. A noncontrast CT scan of the head is normal. The patient is treated for acute alcohol intoxication and admitted to the hospital. The next day, the patient demands to be released. His vital signs are a pulse 120/min, a respiratory rate 22/min, and blood pressure 136/88 mm Hg. On physical examination, the patient is confused, agitated, and sweating profusely, particularly from his palms. Generalized pallor is present. What is the mechanism of action of the drug recommended to treat this patient’s most likely condition?
- A. It decreases the duration of GABA-gated chloride channel opening.
- B. It increases the duration of GABA-gated chloride channel opening.
- C. It activates the GABA receptors by binding at the GABA binding site.
- D. It decreases the frequency of GABA-gated chloride channel opening.
- E. It increases the frequency of GABA-gated chloride channel opening. (Correct Answer)
Alcohol use disorder Explanation: ***It increases the frequency of GABA-gated chloride channel opening.***
- The patient's symptoms (agitation, confusion, sweating, tachycardia, elevated blood pressure) 24 hours after acute alcohol intoxication, in a chronic alcoholic, are highly suggestive of **alcohol withdrawal syndrome**, likely progressing towards **delirium tremens**.
- **Benzodiazepines** are the first-line treatment for alcohol withdrawal. They act by **increasing the frequency of GABA-gated chloride channel opening**, leading to increased chloride influx, hyperpolarization, and reduced neuronal excitability, thus counteracting the CNS hyperexcitability of alcohol withdrawal.
*It decreases the duration of GABA-gated chloride channel opening.*
- Some drugs, like certain **antiepileptics** (e.g., lamotrigine), can modulate GABA indirectly or affect other ion channels, but this is not the primary mechanism of action for benzodiazepines.
- Decreasing the duration of GABA-gated chloride channel opening would further contribute to neuronal excitation, worsening the alcohol withdrawal symptoms.
*It increases the duration of GABA-gated chloride channel opening.*
- This mechanism is characteristic of **barbiturates**, not benzodiazepines. While barbiturates can also be used for severe alcohol withdrawal, benzodiazepines are generally preferred due to a wider therapeutic index and lower risk of respiratory depression.
- Barbiturates have a higher potential for sedation and overdose than benzodiazepines.
*It activates the GABA receptors by binding at the GABA binding site.*
- **GABA itself** binds to the GABA binding site on the receptor. Benzodiazepines are **allosteric modulators**; they bind to a different site on the GABA-A receptor, not the GABA binding site.
- Direct activation of the GABA binding site by an exogenous substance is not the primary mechanism of action of drugs used for alcohol withdrawal.
*It decreases the frequency of GABA-gated chloride channel opening.*
- Decreasing the frequency of GABA-gated chloride channel opening would lead to reduced inhibitory signaling and increased neuronal excitability, which would exacerbate the symptoms of alcohol withdrawal.
- This mechanism is not associated with drugs used to treat alcohol withdrawal.
Alcohol use disorder US Medical PG Question 3: A 26-year-old man with a history of alcoholism presents to the emergency department with nausea, vomiting, and right upper quadrant pain. Serum studies show AST and ALT levels >5000 U/L. A suicide note is found in the patient's pocket. The most appropriate initial treatment for this patient has which of the following mechanisms of action?
- A. Glutathione substitute (Correct Answer)
- B. Competitive inhibitor of alcohol dehydrogenase
- C. Opioid receptor antagonist
- D. GABA receptor competitive antagonist
- E. Heavy metal chelator
Alcohol use disorder Explanation: ***Glutathione substitute***
- This patient's presentation with **elevated AST/ALT** levels and a **suicide note** strongly suggests **acetaminophen overdose**, which depletes hepatic glutathione stores.
- **N-acetylcysteine (NAC)**, the antidote for acetaminophen overdose, acts as a **glutathione substitute** and precursor, replenishing hepatic glutathione and aiding in the detoxification pathway of acetaminophen's toxic metabolite.
*Competitive inhibitor of alcohol dehydrogenase*
- This describes **fomepizole**, used to treat **methanol** or **ethylene glycol poisoning**, not acetaminophen overdose.
- While the patient has a history of alcoholism, the extremely high transaminase levels point away from typical alcohol-induced liver injury and towards a different toxin.
*Opioid receptor antagonist*
- This describes **naloxone** or **naltrexone**, which are used to reverse **opioid overdose** or block opioid effects.
- The symptoms described (nausea, vomiting, RUQ pain, high transaminases) are not typical of opioid overdose.
*GABA receptor competitive antagonist*
- This describes **flumazenil**, the antidote for **benzodiazepine overdose**.
- While benzodiazepines can be used in suicide attempts, the clinical picture, specifically the profound liver injury, is not characteristic of benzodiazepine toxicity.
*Heavy metal chelator*
- This category includes drugs like **dimercaprol** or **EDTA**, used to treat poisoning by **heavy metals** such as lead, mercury, or arsenic.
- There is no clinical indication for heavy metal poisoning in this scenario; the symptoms and lab findings are inconsistent with such exposures.
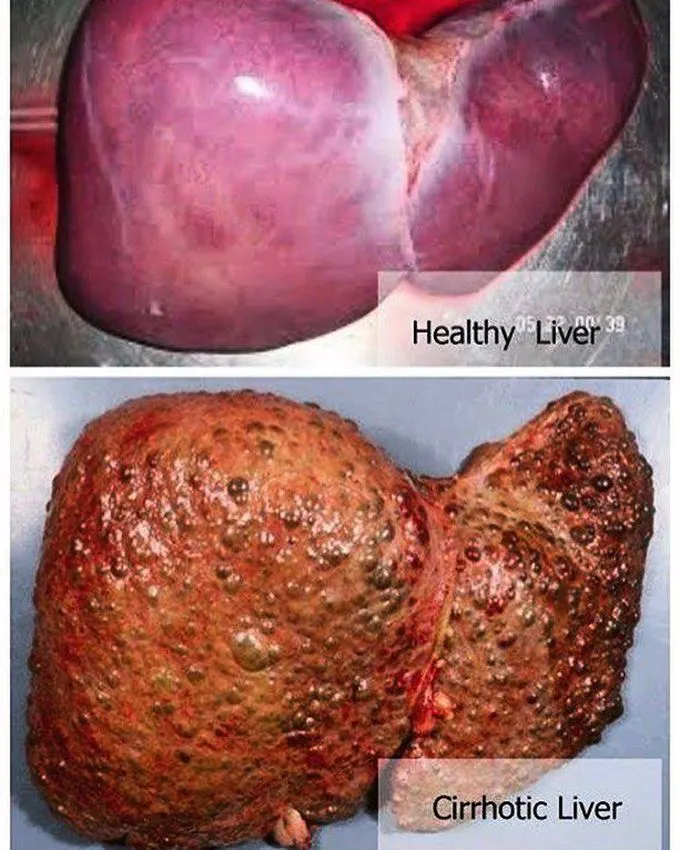
Alcohol use disorder US Medical PG Question 4: A 40-year-old homeless man is brought to the emergency department after police found him in the park lying on the ground with a minor cut at the back of his head. He is confused with slurred speech and fails a breathalyzer test. Pupils are normal in size and reactive to light. A bolus of intravenous dextrose, thiamine, and naloxone is given in the emergency department. The cut on the head is sutured. Blood and urine are drawn for toxicology screening. The blood-alcohol level comes out to be 200 mg/dL. Liver function test showed an AST of 320 U/L, ALT of 150 U/L, gamma-glutamyl transferase of 100 U/L, and total and direct bilirubin level are within normal limits. Which additional physical examination finding is most likely to be present in this patient?
- A. Pin point pupil
- B. Vertical nystagmus
- C. Ataxic gait (Correct Answer)
- D. Increased appetite
- E. High blood pressure
Alcohol use disorder Explanation: ***Ataxic gait***
- Chronic alcohol abuse, suggested by elevated AST, ALT, and GGT levels, leads to **cerebellar degeneration** which manifests as an **ataxic gait**.
- **Alcohol intoxication** itself can cause disequilibrium and staggering, contributing to an ataxic presentation.
*Pin point pupil*
- **Pinpoint pupils** are typically associated with **opioid intoxication** or pontine hemorrhage, neither of which is indicated here.
- The patient's pupils are specifically noted as **normal in size and reactive to light**, ruling out this finding.
*Vertical nystagmus*
- **Vertical nystagmus** is often a sign of **brainstem dysfunction** or certain drug toxicities (e.g., phencyclidine, phenytoin), rather than typical alcohol intoxication or chronic alcoholic effects.
- While nystagmus can occur with alcohol, it's more commonly horizontal; vertical nystagmus would suggest a different or additional pathology.
*Increased appetite*
- **Increased appetite** is not a characteristic symptom of acute alcohol intoxication or chronic alcoholism.
- Chronic alcoholics often experience **malnutrition** and **decreased appetite** due to the metabolic effects of alcohol and associated organ damage.
*High blood pressure*
- While chronic alcoholism can lead to **hypertension** over time, acute alcohol intoxication typically causes **vasodilation and hypotension**.
- This patient's presentation with acute intoxication would more likely involve a lower, rather than higher, blood pressure.
Alcohol use disorder US Medical PG Question 5: A 48-year-old man is brought to the emergency department by his wife 20 minutes after she witnessed him vigorously shaking for about 1 minute. During this episode, he urinated on himself. He feels drowsy and has nausea. He has a history of chronic alcoholism; he has been drinking 15 beers daily for the past 3 days. Before this time, he drank 8 beers daily. His last drink was 2 hours ago. He appears lethargic. His vital signs are within normal limits. Physical and neurologic examinations show no other abnormalities. On mental status examination, he is confused and not oriented to time. Laboratory studies show:
Hematocrit 44.0%
Leukocyte count 12,000/mm3
Platelet count 320,000/mm3
Serum
Na+ 112 mEq/L
Cl- 75 mEq/L
K+ 3.8 mEq/L
HCO3- 13 mEq/L
Urea nitrogen 6 mEq/L
Creatinine 0.6 mg/dL
Albumin 2.1 g/dL
Glucose 80 mg/dL
Urgent treatment for this patient's current condition puts him at increased risk for which of the following adverse events?
- A. Cardiac arrhythmia
- B. Osmotic myelinolysis (Correct Answer)
- C. Cerebral edema
- D. Wernicke encephalopathy
- E. Hyperglycemia
Alcohol use disorder Explanation: **Osmotic myelinolysis**
- The severe **hyponatremia (Na+ 112 mEq/L)** in a chronic alcoholic, likely due to increased ADH from excessive beer intake (beer potomania) and possible malnutrition, places him at risk.
- **Rapid correction** of chronic hyponatremia can cause water to leave brain cells too quickly, leading to **demyelination** of neurons, particularly in the pons.
*Cardiac arrhythmia*
- While severe **electrolyte imbalances** such as hypokalemia or hypomagnesemia can cause cardiac arrhythmias, his potassium is normal, and there's no indication of magnesium deficiency.
- **Alcohol withdrawal** can also cause arrhythmias, but the immediate treatment for his hyponatremia does not directly increase this risk.
*Cerebral edema*
- **Cerebral edema** is a risk of **untreated severe hyponatremia**, where water shifts into brain cells, causing swelling.
- However, the question asks about the risk associated with **urgent treatment** for the condition, which, in this case, would involve raising serum sodium.
*Wernicke encephalopathy*
- **Wernicke encephalopathy** is caused by **thiamine deficiency**, common in chronic alcoholics, and presents with gait ataxia, ophthalmoplegia, and confusion.
- While this patient is at risk, treating hyponatremia does not directly increase the risk of Wernicke encephalopathy; rather, thiamine administration is part of routine care for alcoholics.
*Hyperglycemia*
- **Hyperglycemia** is not a common adverse event of correcting hyponatremia in a patient with a normal blood glucose level.
- Insulin resistance or glucose intolerance might be present in chronic alcoholics, but the urgent treatment for hyponatremia itself does not typically induce hyperglycemia.
Alcohol use disorder US Medical PG Question 6: A 39-year-old man presents to the emergency department for severe abdominal pain. His pain is located in the epigastric region of his abdomen, which he describes as sharp and persistent. His symptoms began approximately 2 days prior to presentation, and he has tried acetaminophen and ibuprofen, which did not improve his symptoms. He feels nauseated and has had 2 episodes of non-bloody, non-bilious emesis. He has a medical history of hypertension and hyperlipidemia for which he is on chlorthalidone and simvastatin. He has smoked 1 pack of cigarettes per day for the last 20 years and drinks 1 pint of vodka per day. On physical exam, there is tenderness to palpation of the upper abdomen, and the patient is noted to have tender hepatomegaly. Serum studies demonstrate:
Amylase: 350 U/L (25-125 U/L)
Lipase: 150 U/L (12-53 U/L)
AST: 305 U/L (8-20 U/L)
ALT: 152 U/L (8-20 U/L)
He is admitted to the hospital and started on intravenous fluids and morphine. Approximately 18 hours after admission the patient reports to feeling anxious, tremulous, and having trouble falling asleep. His blood pressure is 165/105 mmHg and pulse is 140/min. On exam, the patient appears restless and diaphoretic. Which of the following will most likely improve this patient's symptoms?
- A. Chlordiazepoxide
- B. Lorazepam (Correct Answer)
- C. Risperidone
- D. Thiamine
- E. Haloperidol
Alcohol use disorder Explanation: ***Lorazepam***
- The patient is exhibiting symptoms of **alcohol withdrawal**, including anxiety, tremors, restlessness, diaphoresis, hypertension, and tachycardia, which require treatment with a **benzodiazepine**.
- **Lorazepam** is a short-to-intermediate acting benzodiazepine that is preferred in patients with **liver disease** (indicated by elevated AST/ALT and tender hepatomegaly) because it is metabolized by glucuronidation and does not rely on oxidative hepatic metabolism.
*Chlordiazepoxide*
- **Chlordiazepoxide** is a long-acting benzodiazepine primarily metabolized by the **liver's oxidative pathways**, which can accumulate and lead to toxicity in patients with liver dysfunction.
- While effective for alcohol withdrawal, its long half-life and hepatic metabolism make it less ideal for patients with signs of **liver injury** such as this patient with elevated AST/ALT and hepatomegaly.
*Risperidone*
- **Risperidone** is an atypical antipsychotic primarily used to treat **psychosis** or severe agitation, not the core symptoms of alcohol withdrawal.
- It does not address the underlying **neurotransmitter imbalance** (GABAergic hypofunction) characteristic of alcohol withdrawal.
*Thiamine*
- **Thiamine** (vitamin B1) is essential for preventing **Wernicke-Korsakoff syndrome** in patients with chronic alcohol use, and should be administered in this patient.
- However, thiamine does not alleviate the acute symptoms of alcohol withdrawal like anxiety, tremors, or autonomic hyperactivity.
*Haloperidol*
- **Haloperidol** is a potent antipsychotic that can be used for severe agitation or psychotic symptoms, but it **lowers the seizure threshold**, which is particularly dangerous in alcohol withdrawal where seizure risk is already elevated.
- It does not provide the anxiolytic or sedative effects needed to reverse the **GABAergic hypofunction** seen in alcohol withdrawal syndrome.
Alcohol use disorder US Medical PG Question 7: A 33-year-old woman presents with anxiety, poor sleep, and occasional handshaking and sweating for the past 10 months. She says that the best remedy for her symptoms is a “glass of a good cognac” after work. She describes herself as a “moderate drinker”. However, on a more detailed assessment, the patient confesses that she drinks 1–2 drinks per working day and 3–5 drinks on days-off when she is partying. She was once involved in a car accident while being drunk. She works as a financial assistant and describes her job as “demanding”. She is divorced and lives with her 15-year-old daughter. She says that she often hears from her daughter that she should stop drinking. She realizes that the scope of the problem might be larger than she perceives, but she has never tried stopping drinking. She does not feel hopeless, but sometimes she feels guilty because of her behavior. She does not smoke and does not report illicit drugs use. Which of the following medications would be a proper part of the management of this patient?
- A. Topiramate
- B. Naltrexone (Correct Answer)
- C. Amitriptyline
- D. Gabapentin
- E. Disulfiram
Alcohol use disorder Explanation: ***Naltrexone***
- This patient exhibits symptoms consistent with **alcohol use disorder**, including increased tolerance, problematic use despite negative consequences (car accident, daughter's concern), and use to alleviate withdrawal-like symptoms (anxiety, poor sleep, handshaking, sweating). **Naltrexone** helps reduce **craving and pleasurable effects of alcohol** by blocking opioid receptors.
- Given that she has never tried stopping and does not endorse severe withdrawal symptoms requiring inpatient detoxification typically, naltrexone is a suitable first-line pharmacotherapy for **alcohol use disorder** in this context.
*Topiramate*
- While **topiramate** can be used as an off-label treatment for alcohol use disorder, particularly in reducing heavy drinking and cravings, it is generally considered a second-line option.
- Its side effect profile can be more notable (e.g., cognitive slowing, paresthesias) compared to naltrexone, and it's less commonly chosen as an initial monotherapy when other options are available.
*Amitriptyline*
- **Amitriptyline** is a tricyclic antidepressant primarily used for **depression** and some **neuropathic pain** conditions.
- It is not indicated for the treatment of **alcohol use disorder** and could potentially worsen some symptoms or interact with alcohol.
*Gabapentin*
- **Gabapentin** is sometimes used off-label for **alcohol use disorder**, particularly for managing withdrawal symptoms, reducing cravings, and improving sleep.
- However, for a patient who has never attempted cessation and is not in acute withdrawal, but rather is seeking to reduce problematic drinking, naltrexone is generally preferred as a first-line agent.
*Disulfiram*
- **Disulfiram** works by causing an unpleasant physical reaction (nausea, vomiting, flushing, palpitations) when alcohol is consumed.
- It requires strong patient motivation and adherence, as the patient must avoid all alcohol. Given her current struggle with moderation and no prior attempts at abstinence, beginning with disulfiram, which relies on aversive conditioning, might be challenging and is often reserved for highly motivated patients or those who have failed other treatments.
Alcohol use disorder US Medical PG Question 8: A middle aged man is brought in by emergency medical services after being found unconscious, lying on the street next to an empty bottle of vodka. His past medical history is unknown. Upon evaluation, he opens his eyes spontaneously and is able to obey commands. After peripheral access is obtained, IV normal saline and glucose are administered. Suddenly, the patient becomes confused and agitated. Horizontal nystagmus is noted on exam. This acute presentation was likely caused by a deficiency in which of the following?
- A. Vitamin B6
- B. Vitamin B12
- C. Vitamin B1 (Correct Answer)
- D. Vitamin B9
- E. Vitamin A
Alcohol use disorder Explanation: ***Vitamin B1***
- The patient exhibits classic signs of **Wernicke-Korsakoff syndrome**, caused by **thiamine (Vitamin B1) deficiency**, commonly seen in chronic alcoholics.
- The sudden neurological deterioration (confusion, agitation, nystagmus) after intravenous **glucose administration** without prior thiamine repletion is characteristic, as glucose metabolism depletes remaining thiamine reserves.
*Vitamin B6*
- **Pyridoxine (Vitamin B6) deficiency** can cause peripheral neuropathy, sideroblastic anemia, and seizures, but typically not acute encephalopathy or nystagmus exacerbated by glucose.
- It is less commonly associated with acute neurological decline in the context of chronic alcoholism compared to thiamine.
*Vitamin B12*
- **Cobalamin (Vitamin B12) deficiency** can lead to megaloblastic anemia and peripheral neuropathy, and in severe cases, subacute combined degeneration of the spinal cord.
- However, it does not typically present with acute confusion, nystagmus, and agitation, especially not exacerbated by glucose administration.
*Vitamin B9*
- **Folate (Vitamin B9) deficiency** typically causes megaloblastic anemia and, in some cases, neurological symptoms due to high homocysteine levels, but not the acute constellation of symptoms described.
- Like B12 deficiency, it is not acutely worsened by glucose administration.
*Vitamin A*
- **Vitamin A deficiency** can lead to night blindness, xerophthalmia, and immune dysfunction.
- It does not cause acute neurological symptoms such as confusion, agitation, or nystagmus, and is unrelated to glucose metabolism in this context.
Alcohol use disorder US Medical PG Question 9: A 62-year-old man is referred to a gastroenterologist because of difficulty swallowing for the past 5 months. He has difficulty swallowing both solid and liquid foods, but there is no associated pain. He denies any shortness of breath or swelling in his legs. He immigrated from South America 10 years ago. He is a non-smoker and does not drink alcohol. His physical examination is unremarkable. A barium swallow study was ordered and the result is given below. Esophageal manometry confirms the diagnosis. What is the most likely underlying cause of this patient’s condition?
- A. Pharyngoesophageal diverticulum
- B. Chagas disease (Correct Answer)
- C. Esophageal rupture
- D. Gastroesophageal reflux disease
- E. Squamous cell carcinoma of the esophagus
Alcohol use disorder Explanation: ***Chagas disease***
- The patient's history of living in **South America** and presenting with **dysphagia for both solids and liquids** (suggesting a motility disorder), along with the **barium swallow image showing esophageal dilation and a 'bird's beak' appearance** at the gastroesophageal junction, are highly characteristic of achalasia caused by Chagas disease.
- Chagas disease, caused by *Trypanosoma cruzi*, leads to the destruction of **myenteric plexus neurons** in the esophagus, resulting in achalasia (failure of the lower esophageal sphincter to relax) and megaesophagus.
*Pharyngoesophageal diverticulum*
- This typically presents as **Zenker's diverticulum**, causing **difficulty initiating a swallow**, regurgitation of undigested food, and sometimes halitosis, which is different from the described dysphagia for both solids and liquids.
- A Zenker's diverticulum would appear as a **pouch-like protrusion** in the posterior pharynx, not the diffuse esophageal dilation seen in the image.
*Esophageal rupture*
- Esophageal rupture (Boerhaave syndrome) is an acute, life-threatening condition associated with **severe chest pain, vomiting, and crepitus**, not a chronic, progressive dysphagia without pain.
- Imaging would reveal **extravasation of contrast** into the mediastinum or pleural space, not the smooth dilation and distal narrowing observed.
*Gastroesophageal reflux disease*
- While chronic GERD can lead to **strictures** and dysphagia, it typically causes **heartburn**, regurgitation, and sometimes odynophagia, and the dysphagia is usually progressive for solids first.
- The barium swallow would show reflux or a stricture, not the **classic achalasia findings** of a dilated esophagus tapering to a narrow distal segment.
*Squamous cell carcinoma of the esophagus*
- Squamous cell carcinoma usually presents with **progressive dysphagia, initially for solids**, and is often associated with weight loss, smoking, and alcohol use, none of which are present in this patient.
- A tumor would typically appear as an **irregular, focal narrowing or mass** on barium swallow, not the smooth, diffuse dilation seen in this image.
Alcohol use disorder US Medical PG Question 10: A mother presents to the family physician with her 16-year-old son. She explains, "There's something wrong with him doc. His grades are getting worse, he's cutting class, he's gaining weight, and his eyes are often bloodshot." Upon interviewing the patient apart from his mother, he seems withdrawn and angry at times when probed about his social history. The patient denies abuse and sexual history. What initial test should be sent to rule out the most likely culprit of this patient's behavior?
- A. Complete blood count
- B. Sexually transmitted infection (STI) testing
- C. Blood culture
- D. Urine toxicology screen (Correct Answer)
- E. Slit lamp examination
Alcohol use disorder Explanation: ***Urine toxicology screen***
- The patient's presentation with **declining grades**, **cutting class**, **weight gain**, **bloodshot eyes**, and **irritability** are classic signs of **substance abuse** in an adolescent.
- A **urine toxicology screen** is the most appropriate initial test to detect common illicit substances, especially given the clear signs pointing towards drug use.
*Slit lamp examination*
- This test is used to examine the **anterior segment of the eye**, including the conjunctiva, cornea, iris, and lens.
- While the patient has **bloodshot eyes**, this specific test would be more relevant for ruling out ocular infections or injuries, not for diagnosing the underlying cause of systemic behavioral changes.
*Complete blood count*
- A **complete blood count (CBC)** measures different components of the blood, such as red blood cells, white blood cells, and platelets.
- A CBC is a general health indicator and while it can detect infections or anemia, it is not specific or sensitive enough to identify the cause of the behavioral changes described.
*Sexually transmitted infection (STI) testing*
- Although the patient denies sexual history, all adolescents presenting with certain risk factors or symptoms may warrant STI testing in a broader health assessment.
- However, in this scenario, the primary cluster of symptoms (poor grades, cutting class, bloodshot eyes, irritability) points more directly to substance abuse than to an STI.
*Blood culture*
- A **blood culture** is used to detect the presence of bacteria or other microorganisms in the bloodstream, indicating a systemic infection (sepsis).
- The patient's symptoms are not indicative of an acute bacterial bloodstream infection, and a blood culture would not be the initial test for the presented behavioral changes.
More Alcohol use disorder US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.