Sleep-related movement disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sleep-related movement disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sleep-related movement disorders US Medical PG Question 1: A 63-year-old man presents to his primary care physician complaining of excessive daytime sleepiness. He explains that this problem has worsened slowly over the past few years but is now interfering with his ability to play with his grandchildren. He worked previously as an overnight train conductor, but he has been retired for the past 3 years. He sleeps approximately 8-9 hours per night and believes his sleep quality is good; however, his wife notes that he often snores loudly during sleep. He has never experienced muscle weakness or hallucinations. He has also been experiencing headaches in the morning and endorses a depressed mood. His physical exam is most notable for his large body habitus, with a BMI of 34. What is the best description of the underlying mechanism for this patient's excessive daytime sleepiness?
- A. Poor oropharyngeal tone (Correct Answer)
- B. Circadian rhythm sleep-wake disorder
- C. Deficiency of the neuropeptides, orexin-A and orexin-B
- D. Insufficient sleep duration
- E. Psychiatric disorder
Sleep-related movement disorders Explanation: ***Poor oropharyngeal tone***
- This patient's symptoms, including **excessive daytime sleepiness**, loud **snoring**, **morning headaches**, **obesity (BMI 34)**, and depressed mood, are all highly suggestive of **obstructive sleep apnea (OSA)**.
- In OSA, poor oropharyngeal tone, often exacerbated by obesity, leads to the collapse of the upper airway during sleep, causing interrupted breathing and subsequent sleep fragmentation, which manifests as daytime sleepiness.
*Circadian rhythm sleep-wake disorder*
- This disorder typically involves a **misalignment between endogenous sleep-wake rhythms** and external environmental cues, often seen in shift workers or with jet lag.
- While the patient previously worked as an overnight conductor, he has been retired for 3 years, and his symptoms are more aligned with chronic airway obstruction rather than a desynchronized internal clock.
*Deficiency of the neuropeptides, orexin-A and orexin-B*
- A deficiency in **orexin (hypocretin)** is the underlying mechanism for **narcolepsy type 1**, characterized by excessive daytime sleepiness, cataplexy (sudden loss of muscle tone triggered by strong emotions), and sleep paralysis/hypnagogic hallucinations.
- This patient specifically denies muscle weakness or hallucinations, which makes narcolepsy less likely.
*Insufficient sleep duration*
- While insufficient sleep duration can cause excessive daytime sleepiness, the patient reports sleeping approximately **8-9 hours per night**, which is generally considered an adequate duration for adults.
- The loud snoring and other symptoms point towards a **qualitative problem with sleep**, despite seemingly adequate hours.
*Psychiatric disorder*
- While **depressed mood** is present, it is often a **consequence or comorbidity of chronic sleep deprivation** and fragmented sleep rather than the primary cause of the patient's excessive daytime sleepiness and loud snoring.
- Depression alone does not explain the physical signs like snoring and morning headaches without an underlying sleep disorder.
Sleep-related movement disorders US Medical PG Question 2: A 45-year-old woman presents with recent onset movement abnormalities. She says that she noticeably blinks, which is out of her control. She also has spasms of her neck muscles and frequent leg cramps. Past medical history is significant for ovarian cancer, currently being treated with an antineoplastic agent that disrupts microtubule function and an alkylating agent, as well as metoclopramide for nausea. Her blood pressure is 110/65 mm Hg, the respiratory rate is 17/min, the heart rate is 78/min, and the temperature is 36.7°C (98.1°F). Physical examination is within normal limits. Which of the following drugs would be the best treatment for this patient?
- A. Physostigmine
- B. Bethanechol
- C. Benztropine (Correct Answer)
- D. Diazepam
- E. Clozapine
Sleep-related movement disorders Explanation: ***Benztropine***
- This patient presents with symptoms of **drug-induced parkinsonism** or **extrapyramidal symptoms (EPS)**, likely caused by **metoclopramide**, a dopamine receptor antagonist. Benztropine, an **anticholinergic agent**, is effective in blocking cholinergic overactivity in the basal ganglia, which is characteristic of EPS.
- Its mechanism of action helps to restore the balance between **dopamine** and **acetylcholine** in the striatum, thereby alleviating symptoms like dystonia, akathisia, and parkinsonism.
*Physostigmine*
- Physostigmine is an **acetylcholinesterase inhibitor** that increases acetylcholine levels. It is used to reverse anticholinergic toxicity, which is the opposite of the current clinical need.
- Administering physostigmine would worsen the patient's EPS symptoms as it would further imbalance the dopamine-acetylcholine ratio towards cholinergic dominance.
*Bethanechol*
- Bethanechol is a **direct cholinergic agonist** that primarily acts on muscarinic receptors in the bladder and gastrointestinal tract. It is used for urinary retention and gastrointestinal hypomotility.
- This drug would not address the underlying pathophysiology of EPS and could potentially exacerbate cholinergic side effects, rather than resolving movement disorders.
*Diazepam*
- Diazepam is a **benzodiazepine** that enhances the effect of GABA, a major inhibitory neurotransmitter. It is used for anxiety, seizures, and muscle spasms, but it is not a primary treatment for EPS.
- While it might offer some symptomatic relief for muscle spasms, it does not directly target the dopaminergic-cholinergic imbalance responsible for EPS, and it is associated with sedation and dependence.
*Clozapine*
- Clozapine is an **atypical antipsychotic** with potent D4 and serotonin 5-HT2A receptor antagonism, known for its low risk of EPS. It is primarily used for treatment-resistant schizophrenia.
- As an antipsychotic, clozapine is not indicated for the treatment of drug-induced EPS and could potentially introduce new side effects, including agranulocytosis and myocarditis, making it an inappropriate choice for this presentation.
Sleep-related movement disorders US Medical PG Question 3: A 55-year-old woman comes to the physician because of involuntary rhythmic shaking of both hands for several months. More recently, she also noticed involuntary head nodding movements. The shaking seems to improve after having one or two glasses of wine. Her father had similar symptoms starting at the age of 60. Neurologic examination shows a symmetric hand tremor that worsens with voluntary movement of the respective extremity. The most appropriate pharmacotherapy for this patient's symptoms is also recommended for the treatment of which of the following conditions?
- A. Malignant hyperthermia
- B. Restless legs syndrome
- C. Hyperthyroidism (Correct Answer)
- D. Sleepwalking
- E. Motion sickness
Sleep-related movement disorders Explanation: ***Hyperthyroidism***
- The patient presents with **essential tremor**, characterized by **bilateral symmetric hand tremor** that worsens with action, head nodding, and improvement with alcohol. The first-line treatment for essential tremor is **propranolol**, a non-selective beta-blocker.
- Propranolol is also the primary symptomatic treatment for the adrenergic symptoms of **hyperthyroidism**, such as **tachycardia**, tremor, and anxiety, by blocking beta-adrenergic receptors.
*Malignant hyperthermia*
- This is a life-threatening, rare pharmacogenetic disorder triggered by certain anesthetic agents, leading to **skeletal muscle rigidity**, hyperthermia, and metabolic acidosis.
- The primary treatment is **dantrolene**, a muscle relaxant, not propranolol.
*Restless legs syndrome*
- Characterized by an irresistible urge to move the legs, often accompanied by unpleasant sensations, typically worse at rest and in the evening.
- First-line treatments include **dopamine agonists** (e.g., pramipexole, ropinirole) or gabapentin, not propranolol.
*Sleepwalking*
- A type of parasomnia characterized by complex behaviors while partially aroused from NREM sleep, with no memory of the event upon awakening.
- While sometimes managed with low-dose benzodiazepines or antidepressants, propranolol is not a standard treatment.
*Motion sickness*
- Caused by a mismatch between visual and vestibular sensory input, leading to nausea, vomiting, and dizziness.
- Treated with anticholinergic agents like **scopolamine**, or antihistamines such as dimenhydrinate, primarily targeting the vestibular system and central nervous system.
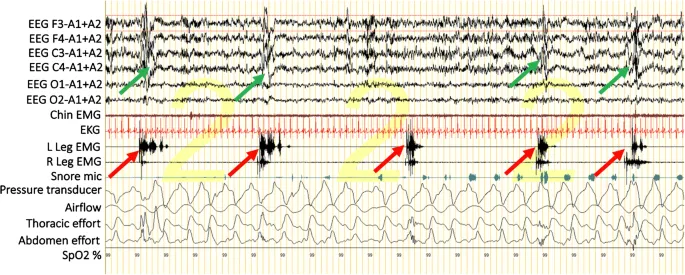
Sleep-related movement disorders US Medical PG Question 4: A 47-year-old man presents with a history of a frequent unpleasant crawling sensation in both of his legs accompanied by an urge to move his legs for the last 6 months. He continuously moves his legs to provide him with partial relief from the unpleasant feelings in his legs. The symptoms are especially severe during the night or while lying down in bed after returning from work. These symptoms occur 3–5 days per week. He also complains of significant daytime fatigue and sleep disturbances on most days of the week. He is advised to take a polysomnography test, which reveals periodic limb movements (PLMs) during his sleep. Which of the following conditions is most associated with secondary restless legs syndrome?
- A. Pulmonary tuberculosis
- B. Vitamin B3 deficiency
- C. Zinc deficiency
- D. Liver failure
- E. Iron deficiency anemia (Correct Answer)
Sleep-related movement disorders Explanation: ***Iron deficiency anemia***
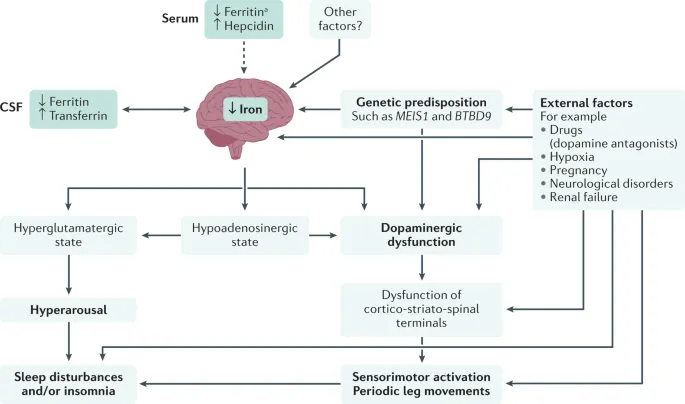
- **Iron deficiency** is a common cause of **secondary Restless Legs Syndrome (RLS)**, as iron is crucial for dopamine synthesis in the brain, which is implicated in RLS pathophysiology.
- Evaluation of RLS often includes testing **serum ferritin levels** to assess iron stores.
*Pulmonary tuberculosis*
- While tuberculosis can cause systemic symptoms and chronic illness, it is **not directly associated** with the pathophysiology of RLS.
- The focus of tuberculosis is on the respiratory system and other organs where the infection manifests.
*Vitamin B3 deficiency*
- **Vitamin B3 deficiency**, or **pellagra**, primarily affects the skin, gastrointestinal tract, and nervous system, causing dermatitis, diarrhea, and dementia.
- It does **not typically present** with or directly cause RLS symptoms.
*Zinc deficiency*
- **Zinc deficiency** can lead to various symptoms like immune dysfunction, hair loss, and skin lesions.
- There is **no established direct link** between zinc deficiency and the development of RLS.
*Liver failure*
- **Liver failure** can cause a range of neurological symptoms such as **encephalopathy** and peripheral neuropathy.
- However, it is **not a primary or common cause** of secondary RLS.
Sleep-related movement disorders US Medical PG Question 5: An 11-year-old boy with a history of attention deficit disorder presents to a general medicine clinic with leg pain. He is accompanied by his mother. He reports dull, throbbing, diffuse pain in his bilateral lower extremities. He reports that the pain feels deep in his muscles. He has awakened several times at night with the pain, and his symptoms tend to be better during the daylight hours. He denies fatigue, fever, or pain in his joints. On physical examination, his vital signs are stable, and he is afebrile. Physical examination reveals full range of motion in the hip and knee joints without pain. He has no joint effusions, erythema, or warmth. What is the next best step in management?
- A. X-ray of the knees
- B. Send ESR and CRP
- C. Reassurance (Correct Answer)
- D. MRI of the knees
- E. Lower extremity venous ultrasound
Sleep-related movement disorders Explanation: ***Reassurance***
- The patient's presentation is classic for **growing pains**, characterized by bilateral, diffuse, deep leg pain, often worse at night and improving with activity or during the day.
- The absence of fever, joint swelling, erythema, tenderness, or gait abnormalities, along with normal physical examination findings, supports this benign diagnosis.
*X-ray of the knees*
- This symptom complex is a **diagnosis of exclusion**; imaging studies like X-rays are typically normal and not indicated unless there are focal pain, limping, or other concerning signs.
- An X-ray would not show any abnormalities related to growing pains and would expose the child to unnecessary radiation.
*Send ESR and CRP*
- **Inflammatory markers** (ESR, CRP) are used to detect conditions like arthritis, osteomyelitis, or malignancy, which would cause systemic symptoms (e.g., fever, fatigue) or localized inflammatory signs.
- In growing pains, these markers are typically normal, and ordering them without other clinical indications is unnecessary.
*MRI of the knees*
- An MRI is highly sensitive for detecting bone and soft tissue pathologies but is generally not indicated for the typical presentation of growing pains.
- It would be considered if there were signs of **osteomyelitis**, **tumors**, or specific internal derangement of the joint, none of which are present here.
*Lower extremity venous ultrasound*
- This test is used to evaluate for **deep vein thrombosis (DVT)**, which typically presents with unilateral leg swelling, warmth, and tenderness.
- The patient's symptoms are bilateral, diffuse, and lack any signs of vascular compromise, making a venous ultrasound inappropriate.
Sleep-related movement disorders US Medical PG Question 6: A 4-year-old African-American girl is brought to the physician because of multiple episodes of bilateral leg pain for 4 months. The pain is crampy in nature, lasts up to an hour, and occurs primarily before her bedtime. Occasionally, she has woken up crying because of severe pain. The pain is reduced when her mother massages her legs. She has no pain while attending school or playing. Her mother has rheumatoid arthritis. The patient's temperature is 37°C (98.6°F), pulse is 90/min and blood pressure is 94/60 mm Hg. Physical examination shows no abnormalities. Her hemoglobin concentration is 12.1 g/dL, leukocyte count is 10,900/mm3 and platelet count is 230,000/mm3. Which of the following is the most appropriate next best step in management?
- A. X-ray of the lower extremities
- B. Reassurance (Correct Answer)
- C. Nafcillin therapy
- D. Antinuclear antibody
- E. Pramipexole therapy
Sleep-related movement disorders Explanation: ***Reassurance***
- The patient presents with classic symptoms of **growing pains**, characterized by bilateral leg pain that occurs primarily at night, improves with massage, and does not interfere with daily activities or cause physical findings.
- Given the benign nature of growing pains and the unremarkable physical examination and laboratory findings, reassurance and symptomatic management (like massage) are the most appropriate next steps.
*X-ray of the lower extremities*
- This is generally not indicated for typical growing pains as they are a diagnosis of exclusion and do not involve bone abnormalities.
- **Radiographs** would only be considered if there were atypical features like unilateral pain, persistent pain, limping, fever, or localized tenderness, which are absent here.
*Nafcillin therapy*
- Nafcillin is an antibiotic used to treat bacterial infections, particularly those caused by **Staphylococcus aureus**.
- There is no indication of a bacterial infection (e.g., fever, localized swelling, redness, elevated inflammatory markers) in this patient, making antibiotic therapy inappropriate.
*Antinuclear antibody*
- An antinuclear antibody (ANA) test is used to screen for **autoimmune diseases** like systemic lupus erythematosus (SLE) or juvenile idiopathic arthritis.
- While the mother has rheumatoid arthritis, the patient's symptoms are inconsistent with an autoimmune condition, lacking joint swelling, morning stiffness, or systemic symptoms, making an ANA screen premature.
*Pramipexole therapy*
- Pramipexole is primarily used to treat **Parkinson's disease** and **restless legs syndrome (RLS)**.
- Although RLS also presents with leg discomfort at night, it typically involves an *unpleasant sensation* and a *compelling urge to move the legs*, which is different from the crampy pain described as growing pains.
Sleep-related movement disorders US Medical PG Question 7: A 77-year-old woman is brought to her primary care provider by her daughter with behavioral changes and an abnormally bad memory for the past few months. The patient’s daughter says she sometimes gets angry and aggressive while at other times she seems lost and stares at her surroundings. Her daughter also reports that she has seen her mother talking to empty chairs. The patient says she sleeps well during the night but still feels sleepy throughout the day. She has no problems getting dressed and maintaining her one bedroom apartment. Past medical history is significant for mild depression and mild osteoporosis. Current medications include escitalopram, alendronic acid, and a multivitamin. The patient is afebrile, and her vital signs are within normal limits. On physical examination, the patient is alert and oriented and sitting comfortably in her chair. A mild left-hand tremor is noted. Muscle strength is 5 out of 5 in the upper and lower extremities bilaterally, but muscle tone is slightly increased. She can perform repetitive alternating movements albeit slowly. She walks with a narrow gait and has mild difficulty turning. Which of the following is the most likely diagnosis in this patient?
- A. Lewy body dementia (Correct Answer)
- B. Alzheimer's disease
- C. Serotonin syndrome
- D. Frontotemporal dementia
- E. Delirium
Sleep-related movement disorders Explanation: ***Lewy body dementia***
- This patient exhibits **fluctuating cognition** (being lost and staring, behavioral changes), **recurrent visual hallucinations** (talking to empty chairs), and spontaneous motor features of **parkinsonism** (mild left-hand tremor, increased muscle tone, slow alternating movements, narrow gait, difficulty turning), all core features of Lewy body dementia.
- The **insidious onset** and progressive decline over months, along with the symptom triad, fit the diagnostic criteria for Lewy body dementia.
*Alzheimer's disease*
- While Alzheimer's involves memory loss and cognitive decline, it is not typically associated with **prominent early visual hallucinations** or **parkinsonian features** at presentation.
- Alzheimer's disease often presents with **memory impairment as the most prominent early symptom**, often preceding other cognitive deficits by years.
*Serotonin syndrome*
- This is an acute drug reaction characterized by a triad of **mental status changes**, **autonomic hyperactivity**, and **neuromuscular abnormalities**, usually developing rapidly after medication changes affecting serotonin levels.
- The patient's symptoms have been present for months, the vital signs are stable, and her medications (escitalopram) have been stable, making an **acute syndrome** like serotonin syndrome unlikely.
*Frontotemporal dementia*
- This type of dementia primarily affects personality, behavior, and language, with **prominent disinhibition or apathy**.
- While behavioral changes are present, the patient's prominent **visual hallucinations** and **parkinsonian features** are not characteristic of frontotemporal dementia.
*Delirium*
- Delirium is characterized by an **acute onset** and fluctuating course of attention and awareness, often triggered by an underlying medical condition, medication, or infection.
- The patient's symptoms have progressed over **several months**, rather than hours or days, and she is afebrile with stable vital signs, making delirium less likely.
Sleep-related movement disorders US Medical PG Question 8: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Sleep-related movement disorders Explanation: ***Medulla***
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Sleep-related movement disorders US Medical PG Question 9: A 33-year-old man presents to a physician with a 3-year history of gradually worsening tics and difficulty walking. He was last seen by the physician 5 years ago for anxiety and has been purchasing anti-anxiety medications from an internet website without a prescription because he cannot afford to pay for the office visits. Now he says his anxiety is somewhat controlled, but the motor difficulties are making it difficult for him to work and socialize. His family history is unknown because his parents died in an automobile accident when he was an infant. He grew up in foster care and was always a bright child. An MRI of the brain is ordered, which shows prominent atrophy of the caudate nucleus. Repeats of which of the following trinucleotides are most likely responsible for this patient’s disorder?
- A. GAA
- B. CGG
- C. CTG
- D. CCG
- E. CAG (Correct Answer)
Sleep-related movement disorders Explanation: ***CAG***
- The constellation of **gradually worsening tics**, **difficulty walking** (motor difficulties), **anxiety**, and **caudate nucleus atrophy** on MRI is pathognomonic for **Huntington's disease (HD)**.
- Huntington's disease is caused by an expansion of **CAG trinucleotide repeats** in the *HTT* gene on chromosome 4, leading to production of mutant huntingtin protein with an abnormally long polyglutamine tract.
- CAG repeats >36 cause HD; normal alleles have <27 repeats.
*GAA*
- An abnormal expansion of **GAA repeats** in the *FXN* gene causes **Friedreich's ataxia**, which presents with progressive gait ataxia, dysarthria, loss of proprioception, and cardiomyopathy.
- Friedreich's ataxia primarily affects the **spinal cord dorsal columns**, **cerebellum**, and **peripheral nerves**, not the caudate nucleus.
- Onset is typically in childhood/adolescence, earlier than this case.
*CGG*
- An increased number of **CGG repeats** in the *FMR1* gene causes **Fragile X syndrome**, the most common inherited cause of intellectual disability.
- Fragile X presents with developmental delay, intellectual disability, autism spectrum features, and characteristic facial features (long face, large ears).
- It does not cause caudate atrophy, adult-onset motor tics, or progressive neurodegeneration.
*CTG*
- An expansion of **CTG repeats** in the *DMPK* gene causes **myotonic dystrophy type 1** (DM1).
- DM1 presents with **myotonia** (delayed muscle relaxation), progressive muscle weakness, cataracts, cardiac conduction defects, and frontal balding.
- It does not cause the prominent tics, chorea, or caudate atrophy characteristic of Huntington's disease.
*CCG*
- **CCG repeats** are not associated with a major trinucleotide repeat disorder that presents with the specific clinical features described.
- This option does not explain the caudate atrophy, progressive motor tics, and neurodegenerative course seen in this patient.
Sleep-related movement disorders US Medical PG Question 10: A 33-year-old man presents to his physician with a 3-year history of gradually worsening tics and difficulty walking. He was last seen by the physician 5 years ago for anxiety, and he has been buying anti-anxiety medications from an internet website without a prescription as he cannot afford to pay for doctor’s visits. Now, the patient notes that his anxiety is somewhat controlled, but motor difficulties are making it difficult for him to work and socialize. Family history is unobtainable as his parents died in an accident when he was an infant. He grew up in foster care and was always a bright child. An MRI of the brain is ordered; it shows prominent atrophy of the caudate nucleus. Repeats of which of the following trinucleotides are most likely responsible for this patient’s disorder?
- A. CCG
- B. CTG
- C. CGG
- D. CAG (Correct Answer)
- E. GAA
Sleep-related movement disorders Explanation: ***CAG***
- The clinical presentation of **worsening tics**, **difficulty walking** (suggesting motor dysfunction), and the MRI finding of **caudate nucleus atrophy** are classic signs of **Huntington's disease**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder caused by an unstable expansion of **CAG trinucleotide repeats** within the *HTT* gene.
*CCG*
- Expansions of **CCG repeats** are associated with conditions like **fragile X-associated tremor/ataxia syndrome (FXTAS)**.
- While FXTAS involves neurological symptoms, the specific presentation of prominent tics and caudate atrophy points more strongly to Huntington's.
*CTG*
- **CTG trinucleotide repeat** expansions are characteristic of **myotonic dystrophy type 1 (DM1)**.
- Myotonic dystrophy primarily manifests with muscle weakness, myotonia, and cataracts, which are not the primary presenting symptoms here.
*CGG*
- Expansions of **CGG repeats** are the genetic basis of **Fragile X syndrome**, the most common inherited cause of intellectual disability.
- While Fragile X syndrome can have neurological features, it typically presents with developmental delay and distinctive physical features, rather than adult-onset tics and caudate atrophy.
*GAA*
- An expansion of **GAA trinucleotide repeats** is responsible for **Friedreich's ataxia**.
- Friedreich's ataxia is characterized by progressive ataxia, dysarthria, and loss of proprioception, which differ from the motor tics and specific caudate atrophy seen in this patient.
More Sleep-related movement disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.