Sleep hygiene and behavioral interventions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sleep hygiene and behavioral interventions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sleep hygiene and behavioral interventions US Medical PG Question 1: A 24-year-old woman presents with a 3-month history of worsening insomnia and anxiety. She says that she has an important college exam in the next few weeks for which she has to put in many hours of work each day. Despite the urgency of her circumstances, she states that she is unable to focus and concentrate, is anxious, irritable and has lost interest in almost all activities. She also says that she has trouble falling asleep and wakes up several times during the night. She claims that this state of affairs has severely hampered her productivity and is a major problem for her, and she feels tired and fatigued all day. She denies hearing voices, abnormal thoughts, or any other psychotic symptoms. The patient asks if there is some form of therapy that can help her sleep better so that she can function more effectively during the day. She claims that the other symptoms of not enjoying anything, irritability, and anxiety are things that she can learn to handle. Which of the following approaches is most likely to address the patients concerns most effectively?
- A. Initiation of risperidone
- B. Psychotherapy only
- C. Trial of bupropion
- D. Phototherapy
- E. Initiation of mirtazapine (Correct Answer)
Sleep hygiene and behavioral interventions Explanation: ***Initiation of mirtazapine***
- The patient exhibits classic symptoms of **major depressive disorder**, including insomnia, anxiety, anhedonia (loss of interest), irritability, and fatigue, all of which would benefit from an antidepressant.
- **Mirtazapine** is particularly effective at lower doses for **insomnia** and **anxiety** due to its potent antihistaminergic properties, making it suitable given her chief complaint about sleep.
*Initiation of risperidone*
- **Risperidone** is an **antipsychotic** medication used for conditions like schizophrenia, bipolar disorder, or severe agitation, which is not indicated here given the absence of psychotic symptoms.
- Its use in this context would expose the patient to unnecessary side effects such as **extrapyramidal symptoms**, **metabolic syndrome**, and hyperprolactinemia.
*Psychotherapy only*
- While psychotherapy, particularly cognitive-behavioral therapy (CBT), is an important component of depression treatment, the severity and acute nature of her symptoms, especially the significant functional impairment and insomnia, suggest that **pharmacotherapy is also warranted** for a more effective and rapid response.
- Relying solely on psychotherapy might delay symptomatic relief, especially for her prominent **sleep disturbance** and **anxiety**.
*Trial of bupropion*
- **Bupropion** is an antidepressant that works primarily on **dopamine** and **norepinephrine** reuptake, and it tends to be **activating**, which could exacerbate the patient's existing **insomnia** and **anxiety**.
- It lacks the sedative properties that would directly address her primary concern regarding difficulty sleeping.
*Phototherapy*
- **Phototherapy** is primarily used for **seasonal affective disorder (SAD)**, which is not suggested by the patient's presentation; her symptoms have been ongoing for 3 months and are linked to significant stressors, not seasonal changes.
- While it can improve mood and sleep in SAD, it would not be the most appropriate or effective initial treatment for a non-seasonal major depressive episode with prominent insomnia and anxiety.
Sleep hygiene and behavioral interventions US Medical PG Question 2: A 15-year-old boy is brought to the physician with excessive daytime sleepiness over the past year. His parents are concerned with his below-average school performance over the last 3 months. He goes to bed around midnight and wakes up at 7 am on school days, but sleeps in late on weekends. He exercises regularly after school. He usually has a light snack an hour before bed. He does not snore or have awakenings during sleep. He has no history of a serious illness and takes no medications. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. He does not smoke or drink alcohol. There is no history of a similar problem in the family. His vital signs are within normal limits. His BMI is 22 kg/m2. Physical examination shows no abnormal findings. Which of the following is the most appropriate recommendation at this time?
- A. Take melatonin before bedtime
- B. Avoid snacks before bedtime
- C. Decrease exercise intensity
- D. Increase nighttime sleep hours (Correct Answer)
- E. Take a nap in the afternoon
Sleep hygiene and behavioral interventions Explanation: ***Increase nighttime sleep hours***
- The patient's pattern of going to bed at midnight and waking at 7 AM on school days, along with sleeping in late on weekends, suggests a **chronic sleep deficit** accumulated during the week. Adolescents typically require 8-10 hours of sleep per night.
- The excessive daytime sleepiness and declining school performance are strong indicators of insufficient sleep, and **prioritizing more sleep during school nights** is the most direct intervention.
*Take melatonin before bedtime*
- Melatonin supplements are typically used for **sleep-onset insomnia** or **circadian rhythm disorders**, neither of which is clearly indicated here.
- There is no evidence presented of difficulty falling asleep; rather, the issue appears to be insufficient duration of sleep due to **late bedtime schedules**.
*Avoid snacks before bedtime*
- While heavy meals before bedtime can disrupt sleep, this patient reports having only a **light snack**, which is unlikely to be the primary cause of his significant daytime sleepiness.
- There is no mention of indigestion or gastrointestinal discomfort after the snack that would point to this as a problem.
*Decrease exercise intensity*
- Regular exercise generally **improves sleep quality**, and there's no indication that the patient's exercise routine is negatively impacting his sleep.
- While very intense exercise too close to bedtime can be disruptive for some, exercise itself is generally beneficial for sleep and overall health; therefore, reducing it would not be a primary recommendation.
*Take a nap in the afternoon*
- While naps can temporarily alleviate daytime sleepiness, they can also **disrupt nighttime sleep patterns** by reducing sleep drive.
- Napping would be treating the symptom rather than the root cause, which is a **chronic lack of sufficient nighttime sleep**.
Sleep hygiene and behavioral interventions US Medical PG Question 3: A 27-year-old man presents to his primary care physician with concerns about poor sleep quality. The patient states that he often has trouble falling asleep and that it is negatively affecting his studies. He is nervous that he is going to fail out of graduate school. He states that he recently performed poorly at a lab meeting where he had to present his research. This has been a recurrent issue for the patient any time he has had to present in front of groups. Additionally, the patient is concerned that his girlfriend is going to leave him and feels the relationship is failing. The patient has a past medical history of irritable bowel syndrome for which he takes fiber supplements. His temperature is 98.9°F (37.2°C), blood pressure is 117/68 mmHg, pulse is 80/min, respirations are 12/min, and oxygen saturation is 98% on room air. Physical exam is within normal limits. Which of the following is the best initial step in management?
- A. Duloxetine
- B. Alprazolam during presentations
- C. Fluoxetine
- D. Cognitive behavioral therapy (Correct Answer)
- E. Propranolol during presentations
Sleep hygiene and behavioral interventions Explanation: ***Cognitive behavioral therapy***
- This patient presents with symptoms highly suggestive of **generalized anxiety disorder (GAD)**, characterized by persistent worry about various life situations (academics, relationships) and difficulty sleeping. **Cognitive behavioral therapy (CBT)** is considered a first-line treatment for GAD, addressing maladaptive thought patterns and behaviors.
- CBT could also address the patient's specific social anxiety related to presentations, by teaching coping mechanisms and restructuring negative thoughts about social situations.
*Duloxetine*
- **Duloxetine** is a **serotonin-norepinephrine reuptake inhibitor (SNRI)**, which is an appropriate pharmacological treatment for GAD. However, initial management for anxiety disorders, especially in a patient expressing concern about medication side effects or preference for non-pharmacological approaches, often prioritizes psychotherapy like CBT.
- While it could be considered, it is typically not the *best initial step* before exploring non-pharmacological options, given the patient's concerns are not immediately life-threatening and psychotherapeutic options have high efficacy.
*Fluoxetine*
- **Fluoxetine** is a **selective serotonin reuptake inhibitor (SSRI)** and is a first-line pharmacological treatment for GAD.
- Similar to duloxetine, while an effective medication, it is not always the *best initial step* as many patients prefer to try psychotherapy first, and it doesn't address the underlying maladaptive thought processes in the same way CBT does.
*Alprazolam during presentations*
- **Alprazolam** is a **benzodiazepine** that provides rapid relief of anxiety symptoms. However, it is primarily used for **acute, short-term anxiety**, not as a long-term solution for generalized anxiety or social anxiety.
- Chronic use of benzodiazepines carries risks of **tolerance, dependence, and withdrawal symptoms**, making it unsuitable as an initial management strategy for persistent anxiety.
*Propranolol during presentations*
- **Propranolol** is a **beta-blocker** that can help manage the **physical symptoms of performance anxiety** (e.g., tremors, palpitations) by blocking adrenergic receptors.
- While helpful for specific situations like presentations for social anxiety, it does not address the underlying cognitive distortions or generalized anxiety disorder, and therefore is not the best initial comprehensive management approach.
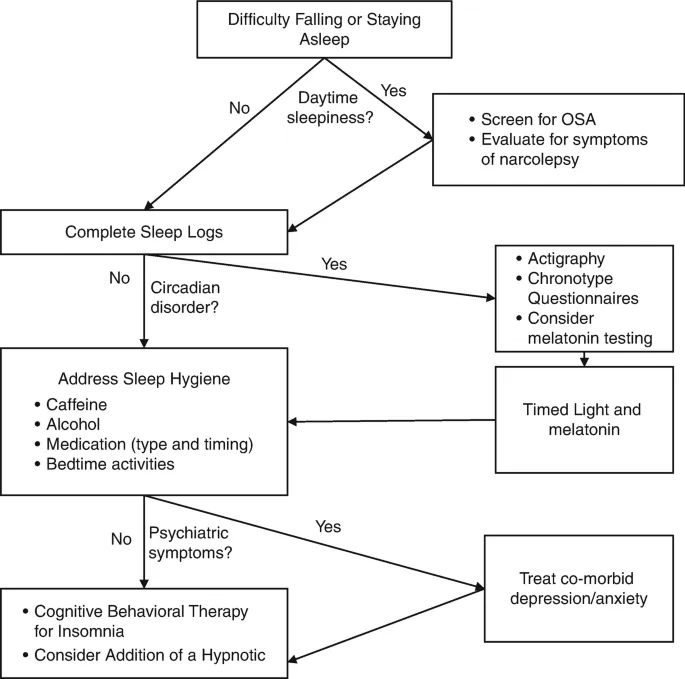
Sleep hygiene and behavioral interventions US Medical PG Question 4: A 62-year-old man presents to his geriatrician due to waking several times during the night and also rising too early in the morning. He says this has worsened over the past 7 months. In the morning, he feels unrefreshed and tired. His medical history is positive for hypertension and benign prostatic hyperplasia. He has never been a smoker. He denies drinking alcohol or caffeine prior to bedtime. Vital signs reveal a temperature of 36.6°C (97.8°F), blood pressure of 130/80 mm Hg, and heart rate of 77/min. Physical examination is unremarkable. After discussing good sleep hygiene with the patient, which of the following is the best next step in the management of this patient’s condition?
- A. Cognitive behavioral therapy for insomnia (CBT-I) (Correct Answer)
- B. Melatonin supplementation
- C. Referral to sleep medicine specialist
- D. Polysomnography
- E. Zolpidem
Sleep hygiene and behavioral interventions Explanation: ***Cognitive behavioral therapy for insomnia (CBT-I)***
- CBT-I is the **first-line treatment** for chronic insomnia according to the American Academy of Sleep Medicine and American College of Physicians guidelines
- After addressing sleep hygiene (already done), CBT-I is the recommended next step before considering pharmacotherapy
- CBT-I has **durable benefits** without the risks of medications, particularly important in elderly patients
- Components include sleep restriction, stimulus control, cognitive restructuring, and relaxation techniques
- In elderly patients, CBT-I avoids medication-related risks such as **falls, cognitive impairment, and dependence**
*Zolpidem*
- While hypnotics like zolpidem may provide short-term symptom relief, they are **not first-line therapy** for chronic insomnia
- The American Geriatrics Society **Beers Criteria** lists benzodiazepines and Z-drugs (including zolpidem) as potentially inappropriate medications in older adults due to increased risk of **falls, fractures, cognitive impairment, and delirium**
- Hypnotics should be reserved for situations where CBT-I is unavailable, ineffective, or when used as a short-term adjunct while implementing behavioral therapy
- If used, they should be prescribed at the **lowest effective dose for the shortest duration**
*Melatonin supplementation*
- Melatonin is most helpful for **circadian rhythm disorders** (e.g., delayed sleep phase syndrome) or **jet lag**
- Limited evidence supports its effectiveness for chronic insomnia with sleep maintenance problems (frequent awakenings and early morning awakening) in elderly patients
- May have a role in patients with documented melatonin deficiency or specific circadian disorders
*Referral to sleep medicine specialist*
- Appropriate if initial interventions (sleep hygiene, CBT-I, limited pharmacotherapy trial) fail
- Indicated when suspecting **primary sleep disorders** such as obstructive sleep apnea, restless legs syndrome, or periodic limb movement disorder
- Not the immediate next step for straightforward chronic insomnia presentation after sleep hygiene counseling
*Polysomnography*
- Polysomnography (sleep study) is indicated when there is clinical suspicion of **sleep-disordered breathing** (sleep apnea), **narcolepsy**, **REM sleep behavior disorder**, or **periodic limb movement disorder**
- This patient's presentation (sleep maintenance insomnia with frequent awakenings and early morning awakening) is most consistent with **primary insomnia**, not a parasomnia or sleep-disordered breathing
- Red flags for sleep apnea (witnessed apneas, loud snoring, gasping, excessive daytime sleepiness, obesity) are absent
- Polysomnography is **not routinely indicated** for the diagnosis of chronic insomnia
Sleep hygiene and behavioral interventions US Medical PG Question 5: A 37-year-old man presents to his primary care physician because he has been experiencing episodes where he wakes up at night gasping for breath. His past medical history is significant for morbid obesity as well as hypertension for which he takes lisinopril. He is diagnosed with sleep apnea and prescribed a continuous positive airway pressure apparatus. In addition, the physician discusses making lifestyle and behavioral changes such as dietary modifications and exercise. The patient agrees to attempt these behavioral changes. Which of the following is most likely to result in improving patient adherence to this plan?
- A. Refer the patient to a peer support group addressing lifestyle changes
- B. Ask the patient to bring a family member to next appointment
- C. Provide follow-up appointments to assess progress in attaining goals (Correct Answer)
- D. Provide appropriate publications for the patient's educational level
- E. Inform the patient of the health consequences of not intervening
Sleep hygiene and behavioral interventions Explanation: ***Provide follow-up appointments to assess progress in attaining goals***
- **Regular follow-up appointments** provide accountability and opportunities to discuss progress, troubleshoot challenges, and reinforce motivation for lifestyle changes
- This approach fosters a **patient-centered relationship** where the physician actively participates in the patient's journey, increasing adherence
- Evidence supports that scheduled follow-up is one of the most effective interventions for improving adherence to chronic disease management plans
*Refer the patient to a peer support group addressing lifestyle changes*
- While peer support can be beneficial for some patients, it is **not universally effective** and might not be suitable for all patients, especially as a primary strategy for adherence
- The effectiveness of such groups varies widely based on the patient's personality and group dynamics, potentially leading to **inconsistent adherence**
*Ask the patient to bring a family member to next appointment*
- Involving family can be supportive, but it may not always be appropriate or desired by the patient and doesn't directly address the patient's individual motivation or challenges
- While family support can enhance adherence, this approach is supplementary rather than primary in effectiveness
*Provide appropriate publications for the patient's educational level*
- Providing educational materials is a good initial step, but information alone is often **insufficient to sustain long-term behavioral changes**
- Without active follow-up and personalized guidance, written materials can be easily forgotten or not fully implemented into daily life
*Inform the patient of the health consequences of not intervening*
- While explaining risks is crucial for informed consent and awareness, relying solely on **fear-based motivation** often has limited long-term effectiveness in promoting sustained behavioral change
- Patients are often aware of potential negative consequences, but this knowledge alone does not provide the practical support or strategies needed for adherence
Sleep hygiene and behavioral interventions US Medical PG Question 6: A 31-year-old woman presents to your office with one week of recurrent fevers. The highest temperature she recorded was 101°F (38.3°C). She recently returned from a trip to Nigeria to visit family and recalls a painful bite on her right forearm at that time. Her medical history is significant for two malarial infections as a child. She is not taking any medications. On physical examination, her temperature is 102.2°F (39°C), blood pressure is 122/80 mmHg, pulse is 80/min, respirations are 18/min, and pulse oximetry is 99% on room air. She has bilateral cervical lymphadenopathy and a visible, enlarged, mobile posterior cervical node. Cardiopulmonary and abdominal examinations are unremarkable. She has an erythematous induration on her right forearm. The most likely cause of this patient's symptoms can be treated with which of the following medications?
- A. Sulfadiazine and pyrimethamine
- B. Atovaquone and azithromycin
- C. Primaquine
- D. Chloroquine
- E. Fexinidazole (Correct Answer)
Sleep hygiene and behavioral interventions Explanation: ***Fexinidazole***
- This patient's symptoms (recurrent fevers, cervical lymphadenopathy, erythematous induration after a trip to Nigeria with a painful bite) are highly suggestive of **African trypanosomiasis (sleeping sickness)**.
- **Fexinidazole** is an oral nitroimidazole derivative approved for treating both first and second-stage human African trypanosomiasis (HAT) caused by *Trypanosoma brucei gambiense*.
*Sulfadiazine and pyrimethamine*
- This combination is primarily used to treat **toxoplasmosis**, an infection caused by the parasite *Toxoplasma gondii*.
- While it can cause fever and lymphadenopathy, the travel history to Nigeria and a "painful bite" are not typical for toxoplasmosis transmission.
*Atovaquone and azithromycin*
- This combination is utilized for treating **Babesiosis**, a tick-borne parasitic infection.
- While Babesiosis can cause fever and fatigue, the characteristic erythematous induration and prominent lymphadenopathy point away from this diagnosis.
*Primaquine*
- **Primaquine** is an antimalarial drug specifically used for the **radical cure of *Plasmodium vivax*** and ***Plasmodium ovale*** malaria, targeting the hypnozoite liver stages.
- Although the patient has a history of malaria and a travel history to an endemic area, the current presentation with distinct lymphadenopathy and skin lesion points away from a straightforward malarial relapse or new infection primarily requiring primaquine as the sole treatment.
*Chloroquine*
- **Chloroquine** is an antimalarial drug, but its use is limited primarily to areas where **chloroquine-sensitive *Plasmodium falciparum*** strains are prevalent.
- While the patient traveled to Nigeria, a region where malaria is endemic, the specific constellation of symptoms, including the bite and lymphadenopathy, is less characteristic of typical malaria than of trypanosomiasis.
Sleep hygiene and behavioral interventions US Medical PG Question 7: A 50-year-old man with severe obstructive sleep apnea (AHI 65 events/hour) and CPAP intolerance despite multiple mask trials undergoes maxillomandibular advancement surgery. Three months post-operatively, he continues to report excessive daytime sleepiness and his bed partner reports persistent snoring. Post-operative polysomnography shows AHI of 28 events/hour. He has a BMI of 38 kg/m² (unchanged from pre-surgery) and crowded posterior pharynx. Evaluate the next management strategy.
- A. Hypoglossal nerve stimulation therapy evaluation
- B. Repeat maxillomandibular advancement with greater advancement distance
- C. Observe for another 3 months as surgical swelling may still be resolving
- D. Revisit CPAP therapy with auto-adjusting pressure settings (Correct Answer)
- E. Proceed directly to tracheostomy for definitive airway management
Sleep hygiene and behavioral interventions Explanation: ***Revisit CPAP therapy with auto-adjusting pressure settings***
- **Maxillomandibular advancement (MMA)** significantly reduced the **Apnea-Hypopnea Index (AHI)** from 65 to 28; while not curative, this anatomical change may lower the **positive airway pressure (PAP)** requirements, potentially improving **patient tolerance**.
- **Auto-CPAP** is the most appropriate next step to determine if the post-surgical airway allows for successful treatment at manageable pressures, especially before considering more invasive options.
*Hypoglossal nerve stimulation therapy evaluation*
- This patient's **BMI of 38 kg/m²** currently exceeds the standard FDA-approved threshold of **35 kg/m²** for **hypoglossal nerve stimulation**.
- Evaluation requires a **Drug-Induced Sleep Endoscopy (DISE)** to check for **concentric palatal collapse**, but primary medical optimization remains the priority.
*Repeat maxillomandibular advancement with greater advancement distance*
- **Revision MMA** carries significantly higher surgical risks, including **nerve injury** and **non-union**, and is generally not indicated when initial surgery was technically successful.
- The persistent **AHI of 28** is more likely due to the patient's **persistent obesity** and soft tissue volume rather than inadequate bony advancement.
*Observe for another 3 months as surgical swelling may still be resolving*
- Three months is typically sufficient for the resolution of **post-operative edema** impacting the airway, and active treatment is needed for **moderate OSA** (AHI 28) and **daytime sleepiness**.
- Delaying management puts the patient at continued risk for **cardiovascular complications** and accidents associated with **excessive sleepiness**.
*Proceed directly to tracheostomy for definitive airway management*
- **Tracheostomy** is the most invasive surgical intervention and is reserved for **life-threatening OSA** where all other medical and surgical options have failed.
- It represents a significant **quality-of-life burden** and should not be considered until less invasive modalities like post-surgical **PAP therapy** are re-attempted.
Sleep hygiene and behavioral interventions US Medical PG Question 8: A 70-year-old man with newly diagnosed Parkinson disease and REM sleep behavior disorder is being considered for treatment. His neurologist is concerned about medication interactions and disease progression. He also has mild cognitive impairment, orthostatic hypotension, and a history of visual hallucinations. Evaluate the optimal therapeutic approach considering his complex medical profile.
- A. Quetiapine for both hallucinations and RBD symptoms
- B. Clonazepam 0.5 mg at bedtime with close monitoring for falls
- C. Rivastigmine to address cognitive impairment and sleep disturbance
- D. Melatonin 3-12 mg at bedtime as first-line therapy (Correct Answer)
- E. Pramipexole dose adjustment to suppress REM sleep
Sleep hygiene and behavioral interventions Explanation: ***Melatonin 3-12 mg at bedtime as first-line therapy***
- **Melatonin** is the preferred first-line treatment for **REM sleep behavior disorder (RBD)** in elderly patients with neurodegeneration due to its excellent safety profile.
- It effectively reduces **dream enactment** with a lower risk of side effects like **excessive sedation** or motor instability compared to other agents.
*Quetiapine for both hallucinations and RBD symptoms*
- While **Quetiapine** is used to manage **visual hallucinations** in Parkinson's, it is not an established or effective therapy for managing **RBD symptoms**.
- It may worsen **orthostatic hypotension** and daytime somnolence, complicating the patient's existing clinical state.
*Clonazepam 0.5 mg at bedtime with close monitoring for falls*
- **Clonazepam** is highly effective for RBD but is generally avoided in patients with **mild cognitive impairment** and **orthostatic hypotension** due to the high risk of **confusion** and **falls**.
- It can also exacerbate **obstructive sleep apnea** or cause significant **morning-after sedation** in the elderly.
*Rivastigmine to address cognitive impairment and sleep disturbance*
- **Rivastigmine**, a cholinesterase inhibitor, is used for **Parkinson disease dementia** but is not the primary treatment for **REM sleep behavior disorder**.
- Although it may help cognitive symptoms, it does not reliably suppress the physical **dream enactment** characteristic of RBD.
*Pramipexole dose adjustment to suppress REM sleep*
- **Dopamine agonists** like **Pramipexole** are known to potentially **worsen RBD** and can significantly increase the frequency of **visual hallucinations**.
- Increasing the dose in this patient would likely exacerbate his **psychosis** and **orthostatic hypotension**.
Sleep hygiene and behavioral interventions US Medical PG Question 9: A 25-year-old medical resident presents with excessive daytime sleepiness and difficulty maintaining wakefulness during lectures. Polysomnography shows normal sleep architecture with a sleep latency of 8 minutes. Multiple Sleep Latency Test (MSLT) shows a mean sleep latency of 4 minutes with 1 sleep-onset REM period (SOREMP). She works rotating shifts, sleeps 4-5 hours on workdays, and has no cataplexy. Evaluation of this clinical scenario suggests which diagnosis best accounts for all findings?
- A. Idiopathic hypersomnia with long sleep time
- B. Narcolepsy type 1 requiring CSF hypocretin measurement
- C. Shift work sleep disorder with circadian misalignment
- D. Narcolepsy type 2 based on objective sleepiness and one SOREMP
- E. Insufficient sleep syndrome related to work schedule (Correct Answer)
Sleep hygiene and behavioral interventions Explanation: ***Insufficient sleep syndrome related to work schedule***
- The patient reports sleeping only **4-5 hours** on workdays, which represents chronic **sleep restriction** compared to the physiological requirement of 7-9 hours.
- **Chronic sleep deprivation** can lead to a shortened mean sleep latency of <8 minutes and single **SOREMPs** on MSLT, making it the most plausible explanation for the findings in a medical resident.
*Idiopathic hypersomnia with long sleep time*
- This condition is characterized by a mean sleep latency of <8 minutes but typically involves **prolonged sleep episodes** (more than 10-11 hours) with significant **sleep drunkenness**.
- The diagnosis requires ruling out **insufficient sleep**, and this patient’s restricted 4-5 hour sleep window directly contradicts the "long sleep time" criteria.
*Narcolepsy type 1 requiring CSF hypocretin measurement*
- **Narcolepsy Type 1** requires the presence of **cataplexy** or low **CSF hypocretin-1** levels, neither of which is suggested by the patient's history.
- The MSLT results in this case only showed **one SOREMP**, whereas Narcolepsy Type 1 diagnosis usually requires **two or more SOREMPs** (or one SOREMP during polysomnography and one during MSLT).
*Shift work sleep disorder with circadian misalignment*
- While the patient works rotating shifts, this disorder specifically involves insomnia or sleepiness that is temporally linked to the **work schedule** causing **circadian misalignment**.
- The primary issue here is the **quantity of sleep** (4-5 hours) rather than the timing of sleep relative to her internal clock, pointing more specifically to insufficient sleep syndrome.
*Narcolepsy type 2 based on objective sleepiness and one SOREMP*
- Diagnostic criteria for **Narcolepsy Type 2** require a mean sleep latency of ≤8 minutes and **two or more SOREMPs**; this patient only had one SOREMP.
- A diagnosis of Narcolepsy Type 2 cannot be made until **insufficient sleep syndrome** is ruled out by ensuring adequate sleep hygiene for at least two weeks prior to testing.
Sleep hygiene and behavioral interventions US Medical PG Question 10: A 40-year-old woman presents with chronic insomnia, taking zolpidem 10 mg nightly for 2 years. Despite medication, she reports difficulty falling asleep, frequent awakenings, and spends significant time in bed worrying about sleep. She naps for 2-3 hours in the afternoon and has an irregular sleep schedule. Her bedroom has a television that she watches until falling asleep. Analysis of perpetuating factors suggests which intervention addresses the core maintaining mechanism of her insomnia?
- A. Polysomnography to identify underlying sleep architecture abnormalities
- B. Switching to a longer-acting benzodiazepine receptor agonist
- C. Gradual tapering of zolpidem with substitution of melatonin
- D. Cognitive behavioral therapy for insomnia (CBT-I) with sleep restriction (Correct Answer)
- E. Adding a sedating antidepressant to the current regimen
Sleep hygiene and behavioral interventions Explanation: ***Cognitive behavioral therapy for insomnia (CBT-I) with sleep restriction***
- This patient exhibits **maladaptive behaviors** such as excessive time in bed, afternoon napping, and conditioned arousal (watching TV in bed) that perpetuate chronic insomnia.
- **CBT-I** is the first-line treatment as it uses **sleep restriction** and **stimulus control** to consolidate sleep and address the underlying cognitive distortions regarding sleep.
*Polysomnography to identify underlying sleep architecture abnormalities*
- **Polysomnography** is generally not indicated for the diagnosis of chronic insomnia unless a breathing disorder or **periodic limb movement disorder** is suspected.
- It does not address the **perpetuating behavioral factors** such as napping and irregular schedules identified in this patient.
*Switching to a longer-acting benzodiazepine receptor agonist*
- Switching to long-acting agents increases the risk of **daytime sedation**, falls, and cognitive impairment without addressing behavioral causes.
- This does not target the **conditioned arousal** or poor sleep hygiene that are maintaining the patient's insomnia.
*Gradual tapering of zolpidem with substitution of melatonin*
- While tapering is often necessary, **melatonin** has limited efficacy for chronic insomnia and does not address the core behavioral issues like excessive time in bed.
- It fails to provide the **cognitive restructuring** needed to manage the patient's anxiety about falling asleep.
*Adding a sedating antidepressant to the current regimen*
- Adding more medication leads to **polypharmacy** and fails to treat the root cause, which is behavioral and cognitive in nature.
- Sedating antidepressants do not improve **sleep efficiency** or consolidate the sleep cycle as effectively as behavioral interventions.
More Sleep hygiene and behavioral interventions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.