Pharmacological management of sleep disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pharmacological management of sleep disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pharmacological management of sleep disorders US Medical PG Question 1: An otherwise healthy 55-year-old woman comes to the physician because of a 7-month history of insomnia. She has difficulty initiating sleep, and her sleep onset latency is normally about 1 hour. She takes melatonin most nights. The physician gives the following recommendations: leave the bedroom when unable to fall asleep within 20 minutes to read or listen to music; return only when sleepy; avoid daytime napping. These recommendations are best classified as which of the following?
- A. Cognitive behavioral therapy
- B. Relaxation
- C. Improved sleep hygiene
- D. Stimulus control therapy (Correct Answer)
- E. Sleep restriction
Pharmacological management of sleep disorders Explanation: ***Stimulus control therapy***
- This therapy focuses on **removing cues** that hinder sleep and **establishing a strong association** between the bed/bedroom and sleep.
- The recommendations (leaving the bedroom when awake, returning only when sleepy, avoiding daytime naps) are classic components of **stimulus control therapy** for insomnia.
*Cognitive behavioral therapy*
- **CBT-I** is a comprehensive approach that includes stimulus control, sleep hygiene, relaxation techniques, and cognitive restructuring.
- While stimulus control is a part of CBT-I, the recommendations provided are specifically designed to address conditioning and are thus best classified as stimulus control therapy.
*Relaxation*
- Relaxation techniques involve methods like **progressive muscle relaxation**, **deep breathing exercises**, or **meditation** to reduce physiological arousal.
- The given recommendations do not directly involve these types of activities but rather focus on changing behaviors around sleep.
*Improved sleep hygiene*
- Sleep hygiene involves practices that promote good sleep, such as maintaining a **regular sleep schedule**, ensuring a **comfortable sleep environment**, and **avoiding caffeine/alcohol** before bed.
- While avoiding daytime naps is related to sleep hygiene, the core recommendations (leaving the bedroom when awake, returning only when sleepy) specifically target conditional associations with the bed, making them more characteristic of stimulus control.
*Sleep restriction*
- Sleep restriction therapy involves **limiting the time spent in bed** to the actual time asleep, with the goal of building up sleep drive and improving sleep efficiency.
- The recommendations given do not specify a fixed reduction in time allowed in bed but rather focus on behavioral responses to wakefulness in bed.
Pharmacological management of sleep disorders US Medical PG Question 2: A 17-year-old man presents to his primary care physician concerned about excessive sleepiness that has persisted his entire life. He notes that he has been having difficulty with his job as a waiter because he often falls asleep suddenly during the day. He also experiences a sensation of dreaming as he goes to sleep even though he still feels awake. He sleeps about 10 hours per day and still feels tired throughout the day. The patient has even reported driving into a tree once as he fell asleep while driving. The patient often stays up late at night working on the computer. Physical exam demonstrates an obese young man who appears tired. His oropharynx demonstrates high palatal ridges and good dental hygiene. Which of the following is the best next step in management?
- A. Recommend scheduling regular naps and more time for sleep at night
- B. Start a selective serotonin reuptake inhibitor
- C. Begin inhibitor of dopamine reuptake
- D. Order sleep study with Multiple Sleep Latency Test (Correct Answer)
- E. Continuous positive airway pressure at night
Pharmacological management of sleep disorders Explanation: ***Order sleep study with Multiple Sleep Latency Test***
- This patient presents with classic symptoms of **narcolepsy**: **excessive daytime sleepiness**, **sudden sleep attacks**, and **hypnagogic hallucinations** (sensation of dreaming while still feeling awake).
- The **Multiple Sleep Latency Test (MSLT)** following overnight **polysomnography** is the **gold standard for diagnosing narcolepsy**. The MSLT measures how quickly the patient falls asleep during daytime nap opportunities and detects **sleep-onset REM periods (SOREMPs)**, which are characteristic of narcolepsy.
- **Diagnosis must precede treatment**: Before initiating pharmacotherapy with controlled substances like modafinil, **definitive diagnosis is required** for both medical/legal standards and insurance approval.
- While the patient has safety concerns (fell asleep driving), the immediate management includes **counseling about driving restrictions** and **ordering diagnostic testing** as the next step.
*Begin inhibitor of dopamine reuptake*
- **Modafinil** or **armodafinil** (dopamine reuptake inhibitors) are first-line treatments for **confirmed narcolepsy** to promote wakefulness and reduce excessive daytime sleepiness.
- However, these medications are **controlled substances** that require a confirmed diagnosis before initiation. Starting treatment without diagnostic confirmation violates standard medical practice and would not be covered by insurance without proper diagnosis codes.
- This would be the appropriate step **after** confirming narcolepsy with sleep study and MSLT.
*Recommend scheduling regular naps and more time for sleep at night*
- While **sleep hygiene** and **scheduled naps** can be adjunctive measures in narcolepsy management, they do not address the underlying pathophysiology and are insufficient as primary management.
- The patient already sleeps 10 hours per day, suggesting that simply increasing sleep time will not resolve the pathological sleepiness.
- This does not provide diagnostic confirmation, which is essential before any treatment plan.
*Start a selective serotonin reuptake inhibitor*
- **SSRIs** or **SNRIs** (like venlafaxine) can be used to treat **cataplexy** (sudden loss of muscle tone triggered by emotions) in narcolepsy patients.
- This patient does not describe clear cataplexy symptoms, and the primary complaint is excessive daytime sleepiness and sleep attacks.
- Like dopamine reuptake inhibitors, SSRIs should only be started **after diagnostic confirmation** of narcolepsy.
*Continuous positive airway pressure at night*
- **CPAP** is the primary treatment for **obstructive sleep apnea (OSA)**, which can cause daytime sleepiness due to fragmented sleep from apneic episodes.
- While this patient is **obese** (a risk factor for OSA) and has **high palatal ridges**, his symptoms of **hypnagogic hallucinations** and **sudden irresistible sleep attacks** are characteristic of **narcolepsy, not OSA**.
- The polysomnography portion of the sleep study will also rule out OSA as a contributing factor, but the primary diagnosis here is narcolepsy.
Pharmacological management of sleep disorders US Medical PG Question 3: A 19-year-old man is seen by his primary care physician. The patient has a history of excessive daytime sleepiness going back several years. He has begun experiencing episodes in which his knees become weak and he drops to the floor when he laughs. He has a history of marijuana use. His family history is notable for hypertension and cardiac disease. His primary care physician refers him for a sleep study, which confirms your suspected diagnosis.
Which of the following is the best first-line pharmacological treatment for this patient?
- A. Zolpidem
- B. Lisdexamfetamine
- C. Modafinil (Correct Answer)
- D. Methylphenidate
- E. Dextroamphetamine
Pharmacological management of sleep disorders Explanation: ***Modafinil***
- This patient presents with symptoms of **narcolepsy** (excessive daytime sleepiness, cataplexy triggered by laughter). **Modafinil** is a non-amphetamine stimulant and a **first-line treatment** for the **excessive daytime sleepiness** component of narcolepsy due to its efficacy in improving wakefulness with a relatively low side effect profile.
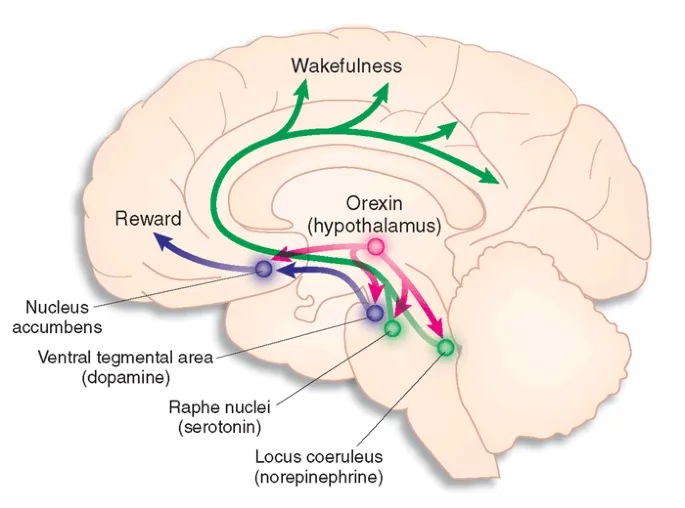
- It works by increasing the release of **monoamines (norepinephrine, dopamine, serotonin)** and histamine, promoting wakefulness without significant cardiovascular effects or abuse potential compared to traditional stimulants.
- **Note:** While modafinil addresses the daytime sleepiness, **cataplexy** would typically require additional treatment with **sodium oxybate** (first-line for cataplexy) or antidepressants (SSRIs, SNRIs, or TCAs).
*Zolpidem*
- **Zolpidem** is a **sedative-hypnotic** primarily used for the short-term treatment of **insomnia**, not for excessive daytime sleepiness or narcolepsy.
- Administering a sedative would worsen the patient's primary complaint of daytime sleepiness.
*Lisdexamfetamine*
- **Lisdexamfetamine** is a **prodrug of dextroamphetamine**, a potent central nervous system stimulant used for **ADHD** and sometimes narcolepsy.
- While effective, it is generally considered a **second-line treatment** for narcolepsy after non-amphetamine stimulants like modafinil, especially given its higher potential for abuse and side effects.
*Methylphenidate*
- **Methylphenidate** is a **central nervous system stimulant** commonly used for **ADHD** and, in some cases, narcolepsy.
- Similar to lisdexamfetamine, it is a stronger stimulant with greater potential for side effects and abuse compared to modafinil, making it a less preferred first-line option.
*Dextroamphetamine*
- **Dextroamphetamine** is a potent **amphetamine stimulant** effective for increasing wakefulness in narcolepsy.
- However, due to its **higher abuse potential**, cardiovascular side effects, and more significant impact on dopamine pathways, it is usually reserved for cases refractory to safer options like modafinil.
Pharmacological management of sleep disorders US Medical PG Question 4: A 53-year-old woman presented to her PCP with one week of difficulty falling asleep, despite having good sleep hygiene. She denies changes in her mood, weight loss, and anhedonia. She has had difficulty concentrating and feels tired throughout the day. Recently, she was fired from her previous job. What medication would be most helpful for this patient?
- A. Citalopram
- B. Diphenhydramine
- C. Quetiapine
- D. Diazepam
- E. Zolpidem (Correct Answer)
Pharmacological management of sleep disorders Explanation: ***Zolpidem***
- This patient presents with **insomnia** characterized by **difficulty falling asleep**, which is the primary indication for zolpidem.
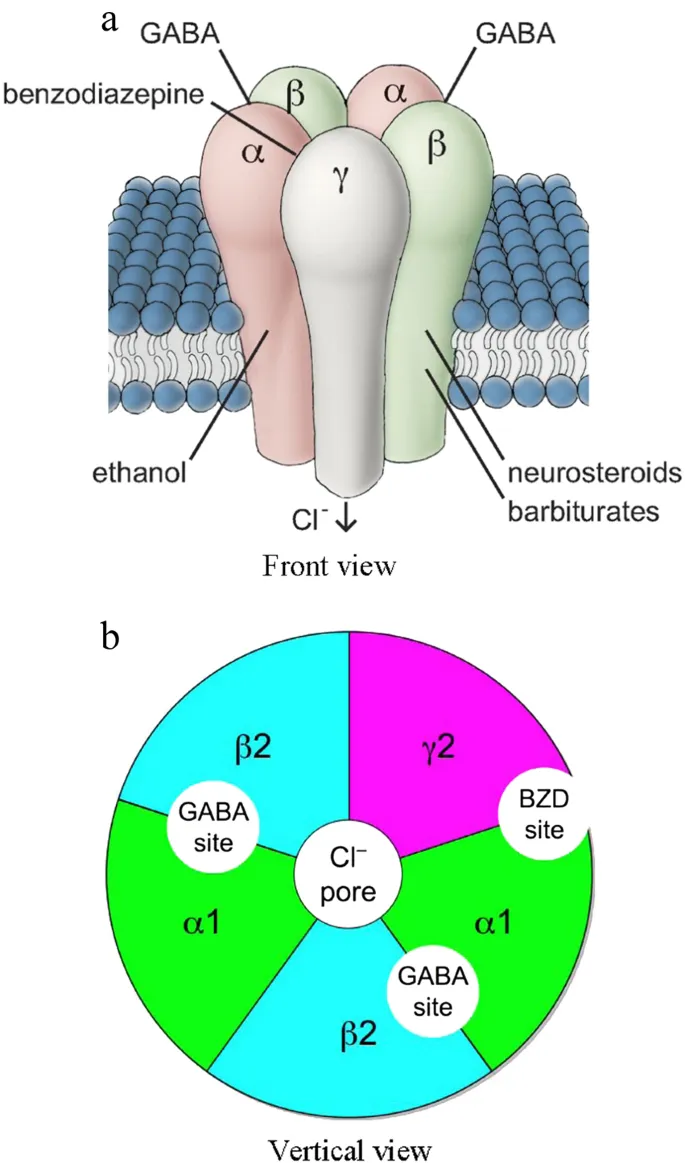
- Zolpidem is a **non-benzodiazepine GABA-A receptor agonist** that acts quickly to induce sleep, making it effective for sleep onset insomnia.
*Citalopram*
- **Citalopram** is an **SSRI** primarily used for treating depression and anxiety disorders, which are not explicitly indicated as primary issues for this patient.
- While it can sometimes help with sleep in depressed patients, its **onset of action is slow** (weeks), and it is not a first-line agent for acute insomnia.
*Diphenhydramine*
- **Diphenhydramine** is an **antihistamine** with sedative properties, often used for occasional insomnia, but it can lead to significant **daytime sedation, anticholinergic side effects**, and is generally not recommended for chronic use.
- The patient's presentation suggests a need for more targeted and potentially long-term management beyond an over-the-counter antihistamine.
*Quetiapine*
- **Quetiapine** is an **antipsychotic** medication that is sometimes used off-label for insomnia due to its sedative effects, but it carries significant **side effects** like metabolic syndrome, orthostatic hypotension, and tardive dyskinesia.
- It is generally **not recommended as a first-line treatment for insomnia** without co-occurring psychiatric conditions like bipolar disorder or schizophrenia.
*Diazepam*
- **Diazepam** is a **benzodiazepine** that can be used for insomnia, but it has a **long half-life** leading to daytime sedation and a **high potential for dependence and abuse**.
- Its use should be limited to short-term treatment of severe insomnia and is generally avoided in patients who deny mood changes and anhedonia, suggesting a less complex underlying issue.
Pharmacological management of sleep disorders US Medical PG Question 5: A 31-year-old man presents to his primary care physician endorsing three months of decreased sleep. He reports an inability to fall asleep; although once asleep, he generally sleeps through the night and wakes up at a desired time. He has instituted sleep hygiene measures, but this has not helped. He has not felt anxious or depressed and is otherwise healthy. You prescribe him a medication that has the potential side effect of priapism. From which of the following locations is the neurotransmitter affected by this medication released?
- A. Locus ceruleus
- B. Substantia nigra
- C. Posterior pituitary
- D. Raphe nucleus (Correct Answer)
- E. Nucleus accumbens
Pharmacological management of sleep disorders Explanation: ***Raphe nucleus***
- The patient's symptoms of **insomnia** without anxiety or depression, despite good sleep hygiene, suggest a potential for prescribing **trazodone**. Trazodone is an antidepressant with **sedating properties** that acts as a serotonin receptor antagonist and reuptake inhibitor.
- The **raphe nucleus** is the primary source of **serotonin** in the brain, and trazodone primarily affects serotonergic pathways, with priapism being a known but rare side effect associated with alpha-1 adrenergic blockade.
*Locus ceruleus*
- The **locus ceruleus** is the main source of **norepinephrine** in the brain, involved in arousal, attention, and stress responses.
- While norepinephrine plays a role in sleep-wake cycles, it is not the primary neurotransmitter targeted by medications commonly associated with priapism for insomnia management in this context.
*Substantia nigra*
- The **substantia nigra** is a brain structure that produces **dopamine** and is primarily involved in motor control, with its degeneration leading to Parkinson's disease.
- This region and its neurotransmitter are not typically associated with the treatment of insomnia or the specific side effect of priapism.
*Posterior pituitary*
- The **posterior pituitary** gland releases **oxytocin** and **vasopressin** (ADH), which are hormones synthesized in the hypothalamus.
- This structure is part of the endocrine system and is not directly involved in the central nervous system pathways targeted by medications for insomnia with the potential for priapism.
*Nucleus accumbens*
- The **nucleus accumbens** is a key component of the **reward pathway** in the brain, primarily utilizing **dopamine** and involved in motivation, pleasure, and addiction.
- While dopamine has some modulatory roles in sleep, it is not the primary target for effective insomnia treatment or associated with the specific side effects mentioned.
Pharmacological management of sleep disorders US Medical PG Question 6: A 62-year-old man presents to his geriatrician due to waking several times during the night and also rising too early in the morning. He says this has worsened over the past 7 months. In the morning, he feels unrefreshed and tired. His medical history is positive for hypertension and benign prostatic hyperplasia. He has never been a smoker. He denies drinking alcohol or caffeine prior to bedtime. Vital signs reveal a temperature of 36.6°C (97.8°F), blood pressure of 130/80 mm Hg, and heart rate of 77/min. Physical examination is unremarkable. After discussing good sleep hygiene with the patient, which of the following is the best next step in the management of this patient’s condition?
- A. Cognitive behavioral therapy for insomnia (CBT-I) (Correct Answer)
- B. Melatonin supplementation
- C. Referral to sleep medicine specialist
- D. Polysomnography
- E. Zolpidem
Pharmacological management of sleep disorders Explanation: ***Cognitive behavioral therapy for insomnia (CBT-I)***
- CBT-I is the **first-line treatment** for chronic insomnia according to the American Academy of Sleep Medicine and American College of Physicians guidelines
- After addressing sleep hygiene (already done), CBT-I is the recommended next step before considering pharmacotherapy
- CBT-I has **durable benefits** without the risks of medications, particularly important in elderly patients
- Components include sleep restriction, stimulus control, cognitive restructuring, and relaxation techniques
- In elderly patients, CBT-I avoids medication-related risks such as **falls, cognitive impairment, and dependence**
*Zolpidem*
- While hypnotics like zolpidem may provide short-term symptom relief, they are **not first-line therapy** for chronic insomnia
- The American Geriatrics Society **Beers Criteria** lists benzodiazepines and Z-drugs (including zolpidem) as potentially inappropriate medications in older adults due to increased risk of **falls, fractures, cognitive impairment, and delirium**
- Hypnotics should be reserved for situations where CBT-I is unavailable, ineffective, or when used as a short-term adjunct while implementing behavioral therapy
- If used, they should be prescribed at the **lowest effective dose for the shortest duration**
*Melatonin supplementation*
- Melatonin is most helpful for **circadian rhythm disorders** (e.g., delayed sleep phase syndrome) or **jet lag**
- Limited evidence supports its effectiveness for chronic insomnia with sleep maintenance problems (frequent awakenings and early morning awakening) in elderly patients
- May have a role in patients with documented melatonin deficiency or specific circadian disorders
*Referral to sleep medicine specialist*
- Appropriate if initial interventions (sleep hygiene, CBT-I, limited pharmacotherapy trial) fail
- Indicated when suspecting **primary sleep disorders** such as obstructive sleep apnea, restless legs syndrome, or periodic limb movement disorder
- Not the immediate next step for straightforward chronic insomnia presentation after sleep hygiene counseling
*Polysomnography*
- Polysomnography (sleep study) is indicated when there is clinical suspicion of **sleep-disordered breathing** (sleep apnea), **narcolepsy**, **REM sleep behavior disorder**, or **periodic limb movement disorder**
- This patient's presentation (sleep maintenance insomnia with frequent awakenings and early morning awakening) is most consistent with **primary insomnia**, not a parasomnia or sleep-disordered breathing
- Red flags for sleep apnea (witnessed apneas, loud snoring, gasping, excessive daytime sleepiness, obesity) are absent
- Polysomnography is **not routinely indicated** for the diagnosis of chronic insomnia
Pharmacological management of sleep disorders US Medical PG Question 7: A 32-year-old man comes to the physician because of generalized fatigue for the past 4 months. He also has difficulty sleeping and concentrating. He says he does not enjoy his hobbies anymore and has stopped attending family events. Mental status examination shows psychomotor retardation and a flat affect along with some evidence of suicidal ideation. His speech is slow in rate and monotone in rhythm. Treatment with fluoxetine is initiated. One month later, he reports significant improvement in his motivation and mood but also delayed ejaculation and occasional anorgasmia. The physician decides to replace his current medication with another agent. It is most appropriate to switch the patient to which of the following drugs?
- A. Venlafaxine
- B. Trazodone
- C. Citalopram
- D. Tranylcypromine
- E. Bupropion (Correct Answer)
Pharmacological management of sleep disorders Explanation: ***Bupropion***
- Bupropion is a **norepinephrine-dopamine reuptake inhibitor** that is associated with a **lower incidence of sexual side effects** compared to SSRIs.
- It would be an appropriate switch for a patient experiencing sexual dysfunction (delayed ejaculation, anorgasmia) secondary to fluoxetine, while still effectively treating depression.
*Venlafaxine*
- Venlafaxine is a **serotonin-norepinephrine reuptake inhibitor (SNRI)**, and like SSRIs, it can also cause **sexual dysfunction** due to its serotonergic activity.
- Switching to venlafaxine would likely not resolve the patient's sexual side effects and might even worsen them.
*Trazodone*
- Trazodone is primarily used off-label for **insomnia** at low doses due to its strong **sedating effects** and antagonism of various receptors (e.g., histamine, alpha-1 adrenergic, serotonin 5-HT2A/C).
- While it has a lower risk of sexual dysfunction than SSRIs, its antidepressant efficacy as monotherapy for major depression is generally considered **weaker** than other first-line options, and its sedating profile might not be ideal given the patient's existing fatigue.
*Citalopram*
- Citalopram is an **SSRI** and belongs to the same class as fluoxetine, sharing similar mechanisms of action and side effect profiles.
- Switching to another SSRI like citalopram would likely result in persistent or similar **sexual dysfunction**, as this is a common class effect of SSRIs.
*Tranylcypromine*
- Tranylcypromine is a **monoamine oxidase inhibitor (MAOI)**, a class of antidepressants typically reserved for **refractory depression** due to their significant drug-drug and food-drug interactions.
- While MAOIs can be effective, they are associated with a much **higher risk of adverse effects** (e.g., hypertensive crisis with tyramine-rich foods) and are generally not a first-line alternative after intolerance to an SSRI, especially when the current issue is sexual dysfunction.
Pharmacological management of sleep disorders US Medical PG Question 8: A 5-year-old boy is brought to the physician by his parents because of 2 episodes of screaming in the night over the past week. The parents report that their son woke up suddenly screaming, crying, and aggressively kicking his legs around both times. The episodes lasted several minutes and were accompanied by sweating and fast breathing. The parents state that they were unable to stop the episodes and that their son simply went back to sleep when the episodes were over. The patient cannot recall any details of these incidents. He has a history of obstructive sleep apnea. He takes no medications. His vital signs are within normal limits. Physical examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Restless legs syndrome
- B. Nightmare disorder
- C. Sleepwalking disorder
- D. Insomnia disorder
- E. Sleep terror disorder (Correct Answer)
Pharmacological management of sleep disorders Explanation: ***Sleep terror disorder***
- This patient's presentation with sudden nocturnal screaming, agitation, autonomic arousal (sweating, fast breathing), and subsequent **amnesia** for the event is classic for **sleep terror disorder**.
- The inability of parents to awaken or comfort the child, followed by the child returning to sleep and having **no recall**, are key diagnostic features.
*Restless legs syndrome*
- Characterized by an irresistible urge to move the legs, often accompanied by uncomfortable sensations, typically occurring or worsening during periods of **rest** or **inactivity**, and partially or totally relieved by movement.
- This condition does not involve screaming, intense fear, or amnesia for a sleep event.
*Nightmare disorder*
- Nightmares are typically **vivid, frightening dreams** from which the individual awakens fully alert and often recalls the dream in detail.
- Unlike sleep terrors, nightmares occur during **REM sleep** (usually later in the night), and the child is usually consolable after waking.
*Sleepwalking disorder*
- Involves complex motor behaviors, such as walking, while still asleep, without full consciousness.
- While it can occur during NREM sleep and involves partial amnesia, it typically **does not feature screaming, intense fear, or significant autonomic arousal** as the predominant symptom.
*Insomnia disorder*
- Defined by persistent difficulty with **sleep initiation, duration, consolidation, or quality**, despite adequate opportunity for sleep, leading to daytime impairment.
- It does not involve acute episodes of screaming or terror during sleep as described.
Pharmacological management of sleep disorders US Medical PG Question 9: A 17-year-old high school student comes to the physician because of a 6-month history of insomnia. On school nights, he goes to bed around 11 p.m. but has had persistent problems falling asleep and instead studies at his desk until he feels sleepy around 2 a.m. He does not wake up in the middle of the night. He is worried that he does not get enough sleep. He has significant difficulties waking up on weekdays and has repeatedly been late to school. At school, he experiences daytime sleepiness and drinks 1–2 cups of coffee in the mornings. He tries to avoid daytime naps. On the weekends, he goes to bed around 2 a.m. and sleeps in until 10 a.m., after which he feels rested. He has no history of severe illness and does not take medication. Which of the following most likely explains this patient's sleep disorder?
- A. Inadequate sleep hygiene
- B. Irregular sleep-wake disorder
- C. Psychophysiologic insomnia
- D. Delayed sleep-wake disorder (Correct Answer)
- E. Advanced sleep-wake disorder
Pharmacological management of sleep disorders Explanation: ***Delayed sleep-wake disorder***
- This patient exhibits a consistent pattern of **delayed sleep onset** and **delayed wake time**, particularly evident on weekends when he can follow his natural circadian rhythm (going to bed at 2 AM and waking at 10 AM).
- The symptoms, including difficulty falling asleep at conventional times, difficulty waking for school, and daytime sleepiness, are classic for **delayed sleep-wake phase disorder**, where an individual's internal clock is misaligned with societal expectations.
*Inadequate sleep hygiene*
- While aspects like studying in bed are **poor sleep hygiene**, the core issue is not simply bad habits but a fundamental misalignment of his **circadian rhythm** as evidenced by his consistent late sleep onset and wake times when allowed.
- The patient's ability to sleep well and feel rested on weekends when he can follow his natural rhythm suggests that hygiene alone isn't the primary cause.
*Irregular sleep-wake disorder*
- This disorder is characterized by a **lack of a discernible sleep-wake rhythm**, with sleep periods fragmented and scattered throughout the 24-hour day.
- The patient, however, demonstrates a clear, albeit delayed, sleep schedule; he sleeps in one consolidated block and feels rested when allowed to do so.
*Psychophysiologic insomnia*
- This condition involves heightened arousal and **anxiety surrounding sleep**, leading to difficulty falling asleep at night and often improved sleep in novel environments or away from home.
- While he expresses worry about not getting enough sleep, his sleep issues are primarily due to a shifted circadian phase, not just anxiety about sleep itself, and he sleeps restfully when allowed to follow his delayed rhythm.
*Advanced sleep-wake disorder*
- This disorder is characterized by a **habitually early sleep onset** and **early morning awakening**, typically several hours earlier than desired or conventional times.
- The patient, in contrast, consistently struggles to fall asleep until very late hours and desires a later wake time.
Pharmacological management of sleep disorders US Medical PG Question 10: A 21-year-old man presents to the clinic complaining of feeling tired during the day. He is concerned as his grades in school have worsened and he does not want to lose his scholarship. Upon further questioning, the patient describes frequently experiencing a dreamlike state before falling asleep and after waking up. He also has frequent nighttime awakenings where he finds himself unable to move. He denies snoring. The patient does not drink alcohol or abuse any other drugs. The patient's BMI is 21 kg/m2, and his vital signs are all within normal limits. What is this patient's diagnosis?
- A. Obstructive sleep apnea (OSA)
- B. Insomnia
- C. Alcohol withdrawal
- D. Delayed sleep phase syndrome (DSPS)
- E. Narcolepsy (Correct Answer)
Pharmacological management of sleep disorders Explanation: ***Narcolepsy***
- The patient's symptoms of **excessive daytime sleepiness**, **hypnagogic/hypnopompic hallucinations** (dreamlike state before falling asleep and after waking up), and **sleep paralysis** (unable to move during nighttime awakenings) are the **classic tetrad of narcolepsy** (cataplexy is the 4th feature, not present here).
- The absence of snoring, normal BMI, and lack of alcohol/drug use rule out other common causes of sleep disturbances, supporting the diagnosis of narcolepsy.
- Narcolepsy is a **chronic sleep-wake disorder** caused by hypothalamic hypocretin (orexin) deficiency.
*Obstructive sleep apnea (OSA)*
- While OSA also causes **daytime sleepiness**, a key feature is **snoring**, which this patient denies.
- OSA is often associated with obesity, but this patient has a **normal BMI of 21 kg/m²**.
- OSA would not explain the hypnagogic hallucinations or sleep paralysis.
*Insomnia*
- Insomnia primarily involves difficulty initiating or maintaining sleep, leading to **insufficient sleep quantity or quality**.
- This patient's symptoms are more specific, including episodes of sleep paralysis and vivid dreamlike states, rather than just general difficulty sleeping.
- The hallmark features of narcolepsy distinguish this from simple insomnia.
*Alcohol withdrawal*
- Alcohol withdrawal can cause **sleep disturbances**, but it is typically accompanied by other symptoms like tremors, anxiety, autonomic hyperactivity, and potentially seizures, none of which are present.
- The patient **explicitly denies drinking alcohol**, making this diagnosis highly unlikely.
*Delayed sleep phase syndrome (DSPS)*
- DSPS is a **circadian rhythm disorder** characterized by a delayed sleep-wake cycle, where individuals fall asleep and wake up later than desired.
- While it can cause daytime fatigue if individuals are forced to wake up early, it does **not** involve the specific symptoms of hypnagogic/hypnopompic hallucinations or sleep paralysis seen in this patient.
- DSPS is primarily a timing issue, not a neurological sleep disorder.
More Pharmacological management of sleep disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.