Parasomnias US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Parasomnias. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Parasomnias US Medical PG Question 1: A 30-year-old woman comes to the physician because of difficulty sleeping. She is afraid of falling asleep and gets up earlier than desired. Four months ago, she was the driver in a car accident that resulted in the death of her unborn child. She has vivid nightmares of the event and reports that she frequently re-experiences the accident. She blames herself for the death of her child, has stopped working as an accountant, avoids driving in cars, and has withdrawn from her parents and close friends. Which of the following is the most likely diagnosis?
- A. Acute stress disorder
- B. Normal grief
- C. Major depressive disorder
- D. Adjustment disorder
- E. Post-traumatic stress disorder (Correct Answer)
Parasomnias Explanation: ***Post-traumatic stress disorder***
- The patient's symptoms, including **re-experiencing the trauma** (nightmares, flashbacks), avoidance behaviors (avoiding driving, withdrawing from social interactions), and negative alterations in cognition and mood (difficulty sleeping, self-blame), persisting for **four months** after a traumatic event, are characteristic of PTSD.
- The severity and chronicity of these symptoms, significantly impacting her daily functioning, align with the diagnostic criteria for PTSD.
*Acute stress disorder*
- This diagnosis also involves exposure to a traumatic event and similar symptoms (intrusive thoughts, negative mood, avoidance) but is diagnosed only when symptoms last for a minimum of **3 days and a maximum of 1 month** after the trauma.
- Since the patient's symptoms have persisted for **four months**, acute stress disorder is ruled out.
*Normal grief*
- While grief is a natural response to loss, the patient's symptoms extend beyond typical grief, involving specific **trauma-related re-experiencing** and **avoidance behaviors** that are not primarily focused on the deceased, but rather on the traumatic event itself.
- Normal grief typically does not involve the severe, persistent avoidance and intrusive symptoms of a traumatic nature seen here.
*Major depressive disorder*
- Although the patient exhibits symptoms that could overlap with depression (difficulty sleeping, withdrawal, loss of interest), the primary driver of her symptoms is the **traumatic event** and its associated re-experiencing and avoidance.
- A diagnosis of MDD would be considered if the depressive symptoms are paramount and not better explained by the trauma response, but in this case, the **trauma-specific symptoms** are central.
*Adjustment disorder*
- This disorder is characterized by the development of emotional or behavioral symptoms in response to an identifiable stressor, occurring within **3 months of the stressor**.
- While a traumatic event could be a stressor, adjustment disorder is diagnosed when the symptoms **do not meet the criteria for another specific mental disorder**, like PTSD, and are generally less severe and pervasive than what is described in this patient.
Parasomnias US Medical PG Question 2: A 17-year-old man presents to his primary care physician concerned about excessive sleepiness that has persisted his entire life. He notes that he has been having difficulty with his job as a waiter because he often falls asleep suddenly during the day. He also experiences a sensation of dreaming as he goes to sleep even though he still feels awake. He sleeps about 10 hours per day and still feels tired throughout the day. The patient has even reported driving into a tree once as he fell asleep while driving. The patient often stays up late at night working on the computer. Physical exam demonstrates an obese young man who appears tired. His oropharynx demonstrates high palatal ridges and good dental hygiene. Which of the following is the best next step in management?
- A. Recommend scheduling regular naps and more time for sleep at night
- B. Start a selective serotonin reuptake inhibitor
- C. Begin inhibitor of dopamine reuptake
- D. Order sleep study with Multiple Sleep Latency Test (Correct Answer)
- E. Continuous positive airway pressure at night
Parasomnias Explanation: ***Order sleep study with Multiple Sleep Latency Test***
- This patient presents with classic symptoms of **narcolepsy**: **excessive daytime sleepiness**, **sudden sleep attacks**, and **hypnagogic hallucinations** (sensation of dreaming while still feeling awake).
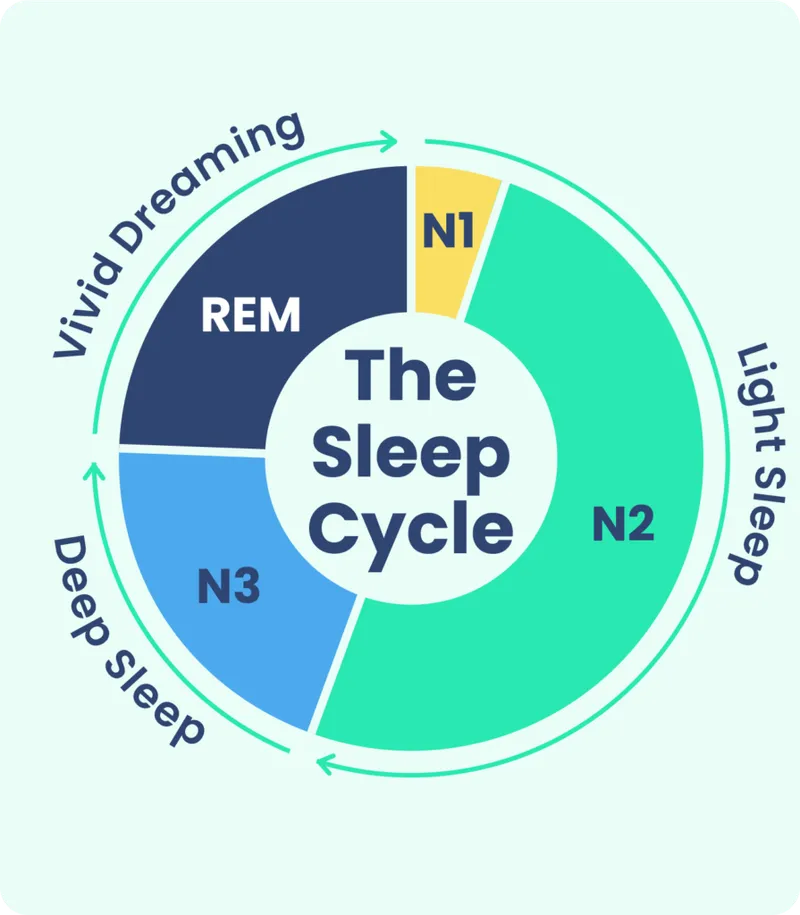
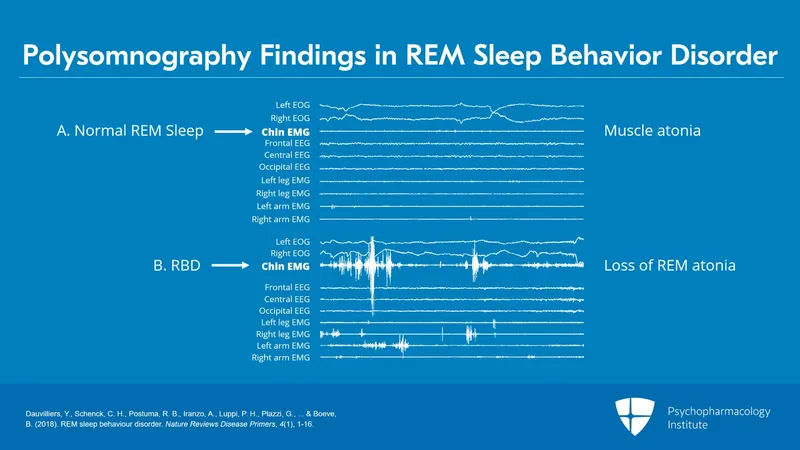
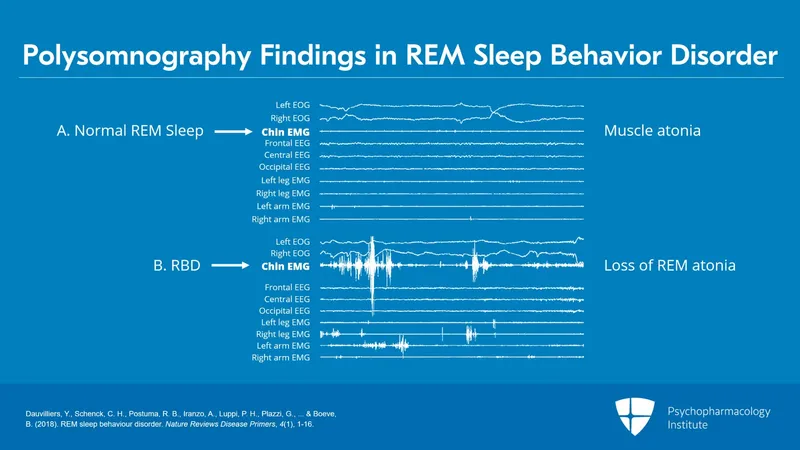
- The **Multiple Sleep Latency Test (MSLT)** following overnight **polysomnography** is the **gold standard for diagnosing narcolepsy**. The MSLT measures how quickly the patient falls asleep during daytime nap opportunities and detects **sleep-onset REM periods (SOREMPs)**, which are characteristic of narcolepsy.
- **Diagnosis must precede treatment**: Before initiating pharmacotherapy with controlled substances like modafinil, **definitive diagnosis is required** for both medical/legal standards and insurance approval.
- While the patient has safety concerns (fell asleep driving), the immediate management includes **counseling about driving restrictions** and **ordering diagnostic testing** as the next step.
*Begin inhibitor of dopamine reuptake*
- **Modafinil** or **armodafinil** (dopamine reuptake inhibitors) are first-line treatments for **confirmed narcolepsy** to promote wakefulness and reduce excessive daytime sleepiness.
- However, these medications are **controlled substances** that require a confirmed diagnosis before initiation. Starting treatment without diagnostic confirmation violates standard medical practice and would not be covered by insurance without proper diagnosis codes.
- This would be the appropriate step **after** confirming narcolepsy with sleep study and MSLT.
*Recommend scheduling regular naps and more time for sleep at night*
- While **sleep hygiene** and **scheduled naps** can be adjunctive measures in narcolepsy management, they do not address the underlying pathophysiology and are insufficient as primary management.
- The patient already sleeps 10 hours per day, suggesting that simply increasing sleep time will not resolve the pathological sleepiness.
- This does not provide diagnostic confirmation, which is essential before any treatment plan.
*Start a selective serotonin reuptake inhibitor*
- **SSRIs** or **SNRIs** (like venlafaxine) can be used to treat **cataplexy** (sudden loss of muscle tone triggered by emotions) in narcolepsy patients.
- This patient does not describe clear cataplexy symptoms, and the primary complaint is excessive daytime sleepiness and sleep attacks.
- Like dopamine reuptake inhibitors, SSRIs should only be started **after diagnostic confirmation** of narcolepsy.
*Continuous positive airway pressure at night*
- **CPAP** is the primary treatment for **obstructive sleep apnea (OSA)**, which can cause daytime sleepiness due to fragmented sleep from apneic episodes.
- While this patient is **obese** (a risk factor for OSA) and has **high palatal ridges**, his symptoms of **hypnagogic hallucinations** and **sudden irresistible sleep attacks** are characteristic of **narcolepsy, not OSA**.
- The polysomnography portion of the sleep study will also rule out OSA as a contributing factor, but the primary diagnosis here is narcolepsy.
Parasomnias US Medical PG Question 3: An 8-year-old girl is brought to the physician by her parents because of difficulty sleeping. One to two times per week for the past 2 months, she has woken up frightened in the middle of the night, yelling and crying. She has not seemed confused after waking up, and she is consolable and able to fall back asleep in her parents' bed. The following day, she seems more tired than usual at school. She recalls that she had a bad dream and looks for ways to delay bedtime in the evenings. She has met all her developmental milestones to date. Physical examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Normal development
- B. Sleep terror disorder
- C. Nightmare disorder (Correct Answer)
- D. Post-traumatic stress disorder
- E. Separation anxiety disorder
Parasomnias Explanation: ***Nightmare disorder***
- The key features supporting **nightmare disorder** are vivid, frightening dreams that lead to waking up, the ability to recall the dream content, being easily consolable, and attempts to avoid bedtime.
- Sleep disturbances, daytime fatigue, and negative emotional responses centered around sleep are characteristic of this disorder.
*Normal development*
- While occasional bad dreams are part of normal development, a frequency of one to two times per week over 2 months, leading to daytime tiredness and bedtime avoidance, suggests a **clinical disorder** exceeding typical developmental experiences.
- The distress caused and impact on daily functioning (tiredness at school) differentiate it from normal, transient nightmares.
*Sleep terror disorder*
- **Sleep terrors** typically involve abrupt awakening with intense fear, screaming, and autonomic arousal, but the individual is usually disoriented, inconsolable, and has no recall of the event upon waking or the next day.
- In this case, the child is consolable and *recalls* having a bad dream, distinguishing it from sleep terrors.
*Post-traumatic stress disorder*
- **PTSD** requires exposure to a traumatic event, which is not mentioned in the vignette.
- While nightmares can be a symptom of PTSD, they are usually accompanied by other symptoms like flashbacks, avoidance behavior, negative alterations in cognition/mood, and hypervigilance related to the trauma.
*Separation anxiety disorder*
- **Separation anxiety disorder** is characterized by excessive fear or anxiety concerning separation from attachment figures.
- Although the child sleeps in her parents' bed, the primary issue is frightening dreams and difficulty sleeping, not anxiety specifically related to separation from her parents.
Parasomnias US Medical PG Question 4: A 20-year-old female presents to student health at her university for excessive daytime sleepiness. She states that her sleepiness has caused her to fall asleep in all of her classes for the last semester, and that her grades are suffering as a result. She states that she normally gets 7 hours of sleep per night, and notes that when she falls asleep during the day, she immediately starts having dreams. She denies any cataplexy. A polysomnogram and a multiple sleep latency test rule out obstructive sleep apnea and confirm her diagnosis. She is started on a daytime medication that acts both by direct neurotransmitter release and reuptake inhibition. What other condition can this medication be used to treat?
- A. Obsessive-compulsive disorder
- B. Bulimia
- C. Attention-deficit hyperactivity disorder (Correct Answer)
- D. Tourette syndrome
- E. Alcohol withdrawal
Parasomnias Explanation: ***Attention-deficit hyperactivity disorder***
- The patient's presentation is consistent with **narcolepsy type 2 (without cataplexy)**, given the excessive daytime sleepiness, short latency to REM sleep (immediate dreaming), and exclusion of sleep apnea. The medication described, acting via **direct neurotransmitter release and reuptake inhibition**, is characteristic of a stimulant like **methylphenidate** or an amphetamine-based drug.
- These stimulants are commonly used as first-line treatment for **attention-deficit hyperactivity disorder (ADHD)** due to their effects on dopamine and norepinephrine in the brain, improving focus and reducing impulsivity.
*Obsessive-compulsive disorder*
- **Obsessive-compulsive disorder (OCD)** is typically treated with selective serotonin reuptake inhibitors (SSRIs) or cognitive behavioral therapy.
- Stimulants are not indicated for OCD and may even worsen anxiety symptoms in some individuals.
*Bulimia*
- **Bulimia nervosa** is often managed with a combination of psychotherapy (e.g., cognitive behavioral therapy) and antidepressants like fluoxetine.
- Stimulants are not a primary treatment for bulimia and could potentially exacerbate some symptoms or risks due to their appetite-suppressing effects.
*Tourette syndrome*
- **Tourette syndrome** involves motor and vocal tics and is often treated with alpha-2 adrenergic agonists (e.g., guanfacine, clonidine) or dopamine receptor blocking agents.
- Stimulants generally are not used for Tourette syndrome as they can sometimes worsen tics.
*Alcohol withdrawal*
- **Alcohol withdrawal** is a medical emergency managed with benzodiazepines to prevent seizures and delirium tremens.
- Stimulants are contraindicated in alcohol withdrawal as they can increase seizure risk and cardiac complications.
Parasomnias US Medical PG Question 5: A 32-year-old man comes to the Veterans Affairs hospital because of difficulty sleeping for the past 9 weeks. He is a soldier who returned from a deployment in Afghanistan 12 weeks ago. Fifteen weeks ago, his unit was ambushed in a deserted street, and a fellow soldier was killed. He wakes up frequently during the night from vivid dreams of this incident. He blames himself for being unable to save his friend. He also has trouble falling asleep and gets up earlier than desired. During this period, he has started to avoid walking in deserted streets. Vital signs are within normal limits. Physical examination shows no abnormalities. He refuses cognitive behavioral therapy and is started on sertraline. Five weeks later, he returns to the physician and complains about persistent nightmares and difficulty sleeping. Which of the following is the most appropriate next step in management?
- A. Prazosin therapy (Correct Answer)
- B. Triazolam therapy
- C. Diazepam therapy
- D. Supportive psychotherapy
- E. Phenelzine therapy
Parasomnias Explanation: ***Prazosin therapy***
- **Prazosin**, an alpha-1 adrenergic antagonist, is effective in reducing **nightmares and sleep disturbances** associated with **post-traumatic stress disorder (PTSD)**, especially when SSRIs are insufficient.
- It works by blocking the effects of norepinephrine, thereby reducing hyperarousal and improving sleep quality in patients with PTSD.
*Triazolam therapy*
- **Triazolam** is a short-acting benzodiazepine primarily used for **insomnia** but is generally not recommended for long-term use due to its potential for **dependence** and withdrawal symptoms.
- While it can help with sleep onset, it does not address the underlying **PTSD-related nightmares** and may worsen the overall sleep architecture.
*Diazepam therapy*
- **Diazepam** is a long-acting benzodiazepine that can provide sedation, but its use in PTSD is **limited due to risks of dependence**, sedation, and cognitive impairment.
- Benzodiazepines like diazepam can also **suppress REM sleep**, which is where nightmares occur, but they don't treat the root cause of the nightmares and are not a first-line therapy for PTSD sleep disturbances.
*Supportive psychotherapy*
- While **psychotherapy is crucial for PTSD**, the patient has already refused **cognitive behavioral therapy (CBT)**, and supportive psychotherapy, while helpful, may not specifically target persistent **nightmares** as effectively as targeted pharmacological interventions when initial SSRI treatment has failed.
- Other forms of psychotherapy like **trauma-focused CBT** or **eye movement desensitization and reprocessing (EMDR)** would be more appropriate for PTSD, but the question asks for the next **management step** for persistent nightmares after an SSRI.
*Phenelzine therapy*
- **Phenelzine** is a **monoamine oxidase inhibitor (MAOI)**, an older class of antidepressants with a **significant side effect profile** and numerous dietary restrictions due to risk of **hypertensive crisis**.
- While MAOIs can be used in refractory depression or anxiety, they are **not a first-line treatment for PTSD** and their risks typically outweigh benefits for sleep disturbances in this context, especially given safer and more targeted options.
Parasomnias US Medical PG Question 6: A 40-year-old man with a past medical history of major depression presents to the clinic. He is interested in joining a research study on depression-related sleep disturbances. He had 2 episodes of major depression within the last 2 years, occurring once during the summer and then during the winter of the other year. He has been non-compliant with medication and has a strong desire to treat his condition with non-pharmacological methods. He would like to be enrolled in this study that utilizes polysomnography to record sleep-wave patterns. Which of the following findings is likely associated with this patient’s psychiatric condition?
- A. Increased REM sleep latency
- B. Associated with a seasonal pattern
- C. Decreased REM sleep latency (Correct Answer)
- D. Increased slow wave sleep
- E. Late morning awakenings
Parasomnias Explanation: ***Decreased REM sleep latency***
- Patients with major depression exhibit characteristic alterations in sleep architecture, most notably a **decreased REM latency** (shortened time from sleep onset to the first REM period).
- Normal REM latency is typically 90 minutes, but in depression it may be reduced to **45-60 minutes or less**.
- This is one of the most **consistent and well-established polysomnographic findings** in major depressive disorder.
- Other REM sleep changes include **increased REM density** (more frequent rapid eye movements) and a shift of REM sleep to the first half of the night.
*Increased REM sleep latency*
- This is the **opposite** of what occurs in depression.
- **Decreased REM sleep latency** (shorter time to reach REM sleep) is the hallmark finding, not increased latency.
- Increased REM latency might be seen in other conditions or with certain medications, but not in untreated major depression.
*Associated with a seasonal pattern*
- While the patient had episodes in summer and winter, the question asks specifically about **polysomnography findings**, not clinical subtypes or patterns.
- Seasonal pattern is a **clinical specifier** for major depressive disorder (as in seasonal affective disorder), not a polysomnographic finding.
- The seasonal pattern itself is a diagnostic feature, not something detected on sleep studies.
*Increased slow wave sleep*
- Depression is associated with **decreased slow-wave sleep (SWS)**, not increased.
- SWS (stage N3, deep sleep) is typically **reduced** in patients with major depression.
- This decrease in restorative deep sleep contributes to the poor sleep quality, daytime fatigue, and cognitive difficulties in depressed patients.
*Late morning awakenings*
- Major depression classically presents with **early morning awakening** (terminal insomnia), not late morning awakening.
- Patients typically wake 2-3 hours earlier than desired and cannot return to sleep.
- Late morning awakenings or hypersomnia may occur in **atypical depression**, but early morning awakening is the more typical pattern in melancholic depression.
Parasomnias US Medical PG Question 7: A 25-year-old male presents to his primary care physician with a chief complaint of anxiety and fatigue. The patient states that during this past week he has had final exams and has been unable to properly study and prepare because he is so exhausted. He states that he has been going to bed early but has been unable to get a good night’s sleep. The patient admits to occasional cocaine and marijuana use. Otherwise, the patient has no significant past medical history and is not taking any medications. On physical exam you note a tired and anxious appearing young man. His neurological exam is within normal limits. The patient states that he fears he will fail his courses if he does not come up with a solution. Which of the following is the best initial step in management?
- A. Polysomnography
- B. Sleep hygiene education (Correct Answer)
- C. Alprazolam
- D. Melatonin
- E. Zolpidem
Parasomnias Explanation: ***Sleep hygiene education***
- This is the **best initial step** because it addresses lifestyle factors that commonly contribute to **insomnia and fatigue**, especially during periods of stress like final exams.
- Helping the patient establish **regular sleep patterns**, avoid stimulants, and create a conducive sleep environment can significantly improve sleep quality without medication.
*Polysomnography*
- This is a diagnostic test typically reserved for when a **primary sleep disorder** like sleep apnea or restless legs syndrome is suspected.
- Given the patient's acute stressor (final exams) and **drug use**, lifestyle interventions should be tried first before pursuing expensive and invasive testing.
*Alprazolam*
- This is a **benzodiazepine** that can be used for acute anxiety or insomnia, but it carries a risk of **dependence, tolerance, and withdrawal**.
- It is not a first-line treatment for a patient experiencing sleep difficulties primarily due to stress and poor sleep habits, and its use should be avoided in those with a history of substance abuse.
*Melatonin*
- Melatonin can be helpful for **circadian rhythm disorders** or jet lag, but its efficacy for primary insomnia is limited and inconsistent.
- While it has fewer side effects than prescription hypnotics, **sleep hygiene education** is still a more fundamental and effective initial approach for this patient.
*Zolpidem*
- This is a **non-benzodiazepine hypnotic** often prescribed for short-term insomnia, but it has potential side effects like **next-day drowsiness** and can be abused, especially in individuals with a history of substance use.
- **Sleep hygiene** should always be optimized first, especially in a young patient whose sleep issues are clearly linked to stress and lifestyle.
Parasomnias US Medical PG Question 8: An 8-year-old girl is brought to the physician by her parents for a 10-month history of disturbing dreams and daytime sleepiness. She has difficulty falling asleep and says she sometimes sees ghosts just before falling asleep at night. She has had a 7-kg (15-lb) weight gain during this period despite no changes in appetite. She is alert and oriented, and neurologic examination is unremarkable. During physical examination, she spontaneously collapses after the physician drops a heavy book, producing a loud noise. She remains conscious after the collapse. Polysomnography with electroencephalogram is most likely to show which of the following?
- A. Slow spike-wave pattern
- B. Periodic sharp waves
- C. Decreased delta wave sleep duration
- D. Diffuse slowing of waves
- E. Rapid onset of REM sleep (Correct Answer)
Parasomnias Explanation: ***Rapid onset of REM sleep***
- The patient's symptoms of **daytime sleepiness**, **hallucinations** (seeing ghosts before sleep, i.e., **hypnagogic hallucinations**), **sleep-onset difficulty**, and the spontaneous collapse (likely **cataplexy** triggered by strong emotion/surprise) are characteristic of **narcolepsy**.
- **Narcolepsy** is often associated with a disinhibition of REM sleep, leading to its occurrence at sleep onset or within 15 minutes of falling asleep, which would be detected by **polysomnography** with **EEG**.
*Slow spike-wave pattern*
- This pattern is characteristic of **absence seizures** (petit mal seizures), which involve brief staring spells and loss of consciousness, not the constellation of sleep disturbances and cataplexy seen here.
- Absence seizures typically do not cause significant **daytime sleepiness** or **hallucinations**.
*Periodic sharp waves*
- **Periodic sharp wave complexes** are pathognomonic for **Creutzfeldt-Jakob disease** (CJD), a rapidly progressive neurodegenerative disorder.
- CJD presents with dementia, myoclonus, and other neurological signs, which are distinct from the patient's symptoms.
*Decreased delta wave sleep duration*
- **Delta wave sleep** (slow-wave sleep or N3 sleep) is a stage of deep non-REM sleep, which is important for restorative sleep.
- While sleep architecture can be disturbed in various sleep disorders, a primary decrease in delta wave sleep duration is not the most specific or hallmark finding for narcolepsy; rather, narcolepsy is defined by its REM sleep abnormalities.
*Diffuse slowing of waves*
- **Diffuse slowing of brain waves** on EEG is a non-specific finding often associated with **encephalopathy**, metabolic disturbances, or diffuse brain dysfunction.
- It does not specifically account for the unique constellation of symptoms seen in this patient, particularly the abrupt onset of sleep-related phenomena and **cataplexy**.
Parasomnias US Medical PG Question 9: A 51-year-old man presents to his physician with decreased libido and inability to achieve an erection. He also reports poor sleep, loss of pleasure to do his job, and depressed mood. His symptoms started a year ago, soon after his wife got into the car accident. She survived and recovered with the minimal deficit, but the patient still feels guilty due to this case. The patient was diagnosed with diabetes 6 months ago, but he does not take any medications for it. He denies any other conditions. His weight is 105 kg (231.5 lb), his height is 172 cm (5 ft 7 in), and his waist circumference is 106 cm. The blood pressure is 150/90 mm Hg, and the heart rate is 73/min. The physical examination only shows increased adiposity. Which of the following tests is specifically intended to distinguish between the organic and psychogenic cause of the patient’s condition?
- A. Angiography
- B. Duplex ultrasound of the penis
- C. Penile tumescence testing (Correct Answer)
- D. Biothesiometry
- E. Injection of prostaglandin E1
Parasomnias Explanation: ***Penile tumescence testing***
- This test, often performed as a **nocturnal penile tumescence (NPT) test**, measures erections during sleep. The presence of normal nocturnal erections indicates a **psychogenic** cause for erectile dysfunction, as physiological mechanisms are intact.
- The absence of nocturnal erections, despite adequate sleep, suggests an **organic** cause, as the body's natural erectile reflex is impaired.
*Angiography*
- **Angiography** is an invasive procedure used to visualize blood vessels and identify arterial blockages or abnormalities. It is typically reserved for cases where vascular disease is strongly suspected as the cause of erectile dysfunction and often considered before revascularization surgery.
- While it can identify **vascular organic causes** of erectile dysfunction, it does not directly differentiate between psychogenic and organic causes universally; it focuses specifically on arterial flow.
*Duplex ultrasound of the penis*
- **Duplex ultrasound** evaluates blood flow within the penile arteries and veins, assessing both arterial inflow and veno-occlusive function. It aids in diagnosing **vascular abnormalities**, such as arterial insufficiency or venous leakage.
- Similar to angiography, duplex ultrasound identifies specific **organic vascular pathologies** but does not definitively distinguish between psychogenic and organic causes of erectile dysfunction if vascular function is normal.
*Biothesiometry*
- **Biothesiometry** measures penile vibratory sensation threshold, which assesses **neurological function** of the penis. It helps detect peripheral neuropathy, a potential organic cause of erectile dysfunction, especially in diabetic patients.
- While useful for uncovering **neurological organic causes**, biothesiometry does not differentiate between psychogenic and organic etiologies in cases where neurological function is normal.
*Injection of prostaglandin E1*
- The **injection of prostaglandin E1** (alprostadil) is a diagnostic and therapeutic tool that induces an erection by relaxing smooth muscle in the penile arteries, increasing blood flow. A strong response indicates intact vascular smooth muscle function.
- A successful response to prostaglandin E1 suggests that vascular smooth muscle and neurological pathways are largely functional, which can indirectly point away from severe organic causes, but it's not a definitive differentiator between **psychogenic and organic** causes as it by-passes some physiological mechanisms.
Parasomnias US Medical PG Question 10: A 21-year-old man presents to the clinic complaining of feeling tired during the day. He is concerned as his grades in school have worsened and he does not want to lose his scholarship. Upon further questioning, the patient describes frequently experiencing a dreamlike state before falling asleep and after waking up. He also has frequent nighttime awakenings where he finds himself unable to move. He denies snoring. The patient does not drink alcohol or abuse any other drugs. The patient's BMI is 21 kg/m2, and his vital signs are all within normal limits. What is this patient's diagnosis?
- A. Obstructive sleep apnea (OSA)
- B. Insomnia
- C. Alcohol withdrawal
- D. Delayed sleep phase syndrome (DSPS)
- E. Narcolepsy (Correct Answer)
Parasomnias Explanation: ***Narcolepsy***
- The patient's symptoms of **excessive daytime sleepiness**, **hypnagogic/hypnopompic hallucinations** (dreamlike state before falling asleep and after waking up), and **sleep paralysis** (unable to move during nighttime awakenings) are the **classic tetrad of narcolepsy** (cataplexy is the 4th feature, not present here).
- The absence of snoring, normal BMI, and lack of alcohol/drug use rule out other common causes of sleep disturbances, supporting the diagnosis of narcolepsy.
- Narcolepsy is a **chronic sleep-wake disorder** caused by hypothalamic hypocretin (orexin) deficiency.
*Obstructive sleep apnea (OSA)*
- While OSA also causes **daytime sleepiness**, a key feature is **snoring**, which this patient denies.
- OSA is often associated with obesity, but this patient has a **normal BMI of 21 kg/m²**.
- OSA would not explain the hypnagogic hallucinations or sleep paralysis.
*Insomnia*
- Insomnia primarily involves difficulty initiating or maintaining sleep, leading to **insufficient sleep quantity or quality**.
- This patient's symptoms are more specific, including episodes of sleep paralysis and vivid dreamlike states, rather than just general difficulty sleeping.
- The hallmark features of narcolepsy distinguish this from simple insomnia.
*Alcohol withdrawal*
- Alcohol withdrawal can cause **sleep disturbances**, but it is typically accompanied by other symptoms like tremors, anxiety, autonomic hyperactivity, and potentially seizures, none of which are present.
- The patient **explicitly denies drinking alcohol**, making this diagnosis highly unlikely.
*Delayed sleep phase syndrome (DSPS)*
- DSPS is a **circadian rhythm disorder** characterized by a delayed sleep-wake cycle, where individuals fall asleep and wake up later than desired.
- While it can cause daytime fatigue if individuals are forced to wake up early, it does **not** involve the specific symptoms of hypnagogic/hypnopompic hallucinations or sleep paralysis seen in this patient.
- DSPS is primarily a timing issue, not a neurological sleep disorder.
More Parasomnias US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.