Normal sleep physiology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Normal sleep physiology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Normal sleep physiology US Medical PG Question 1: An otherwise healthy 43-year-old woman comes to the physician because of several episodes of involuntary movements of her head over the past few months. They are sometimes associated with neck pain and last minutes to hours. Neurologic examination shows no abnormalities. During examination of the neck, the patient's head turns horizontally to the left. She states this movement is involuntary, and that she is unable to unturn her head. After 5 minutes, her head re-straightens. Which of the following best describes this patient's disorder?
- A. Dystonia (Correct Answer)
- B. Athetosis
- C. Akathisia
- D. Hemiballismus
- E. Chorea
Normal sleep physiology Explanation: ***Dystonia***
- This patient presents with **sustained, involuntary muscle contractions** causing repetitive, twisting movements and abnormal postures [1], which are characteristic features of **dystonia**, specifically **cervical dystonia (torticollis)**.
- The description of the head turning involuntarily to the left and inability to unturn it, lasting minutes to hours, fits the pattern of intermittent or spasmodic dystonia.
*Athetosis*
- **Athetosis** involves slow, sinuous, **writhing involuntary movements**, particularly affecting distal limbs [1].
- These movements are often continuous and slow, unlike the more sudden, sustained contractions seen in the patient.
*Akathisia*
- **Akathisia** is characterized by an internal feeling of **restlessness** and a strong urge to move, often described as an inability to sit still.
- It results in fidgeting and pacing, rather than sustained, involuntary posturing of a specific body part.
*Hemiballismus*
- **Hemiballismus** involves **large-amplitude, involuntary, flinging movements** of one side of the body [1].
- This symptom typically arises from lesions in the **subthalamic nucleus** and is distinct from the sustained, twisting movements described [1].
*Chorea*
- **Chorea** presents as **brief, irregular, rapid, and unpredictable involuntary movements** that flow randomly from one body part to another [1].
- Unlike the sustained, fixed posturing seen in dystonia, choreiform movements are often described as "dance-like" and are not maintained.
Normal sleep physiology US Medical PG Question 2: A 20-year-old college student presents to the emergency room complaining of insomnia for the past 48 hours. He explains that although his body feels tired, he is "full of energy and focus" after taking a certain drug an hour ago. He now wants to sleep because he is having hallucinations. His vital signs are T 100.0 F, HR 110 bpm, and BP of 150/120 mmHg. The patient states that he was recently diagnosed with "inattentiveness." Which of the following is the mechanism of action of the most likely drug causing the intoxication?
- A. Blocks NMDA receptors
- B. Activates mu opioid receptors
- C. Displaces norepinephrine from secretory vesicles leading to norepinephrine depletion
- D. Binds to cannabinoid receptors
- E. Increases presynaptic dopamine and norepinephrine release from vesicles (Correct Answer)
Normal sleep physiology Explanation: ***Increases presynaptic dopamine and norepinephrine releases from vesicles***
- The patient's presentation with **insomnia**, feeling "full of energy and focus," **hallucinations**, tachycardia (HR 110 bpm), and hypertension (BP 150/120 mmHg) after taking a drug, especially in the context of a recent diagnosis of "inattentiveness," strongly suggests **amphetamine intoxication**. Amphetamines are commonly prescribed for **ADHD**, and their mechanism involves increasing the release of **dopamine** and **norepinephrine** from presynaptic vesicles.
- This increased release of **catecholamines** leads to the stimulant effects observed, including heightened energy, improved focus, and the adverse effects of agitation, psychosis (hallucinations), and sympathetic overdrive.
*Blocks NMDA receptors*
- Drugs that block **NMDA receptors**, such as **phencyclidine (PCP)** or **ketamine**, can cause dissociative and hallucinatory effects.
- However, the patient's primary complaint of feeling "full of energy and focus" in the context of "inattentiveness" points more towards a classical stimulant rather than a dissociative anesthetic.
*Activates mu opioid receptors*
- Activating **mu opioid receptors** (e.g., by heroin, morphine, fentanyl) typically causes central nervous system **depression**, respiratory depression, miosis, and euphoria, not the stimulant and hyperactive state described.
- The patient's symptoms of increased energy, focus, and elevated vital signs are the opposite of opioid effects.
*Displaces norepinephrine from secretory vesicles leading to norepinephrine depletion*
- This mechanism is characteristic of drugs like **reserpine**, which deplete catecholamines and lead to sedative or antihypertensive effects, not the stimulant and sympathomimetic presentation described.
- Such a mechanism would cause a **decrease** in sympathetic activity, contrary to the patient's elevated heart rate and blood pressure.
*Binds to cannabinoid receptors*
- Binding to **cannabinoid receptors** (e.g., by marijuana)
typically leads to effects such as euphoria, altered perception, impaired memory, and sometimes anxiety or paranoia.
- While hallucinations can occur, the prominent "full of energy and focus" and significant sympathetic activation (tachycardia, hypertension) are not typical of cannabinoid intoxication.
Normal sleep physiology US Medical PG Question 3: A 71-year-old woman comes to her doctor because she is having trouble staying awake in the evening. Over the past year, she has noticed that she gets tired unusually early in the evenings and has trouble staying awake through dinner. She also experiences increased daytime sleepiness, fatigue, and difficulty concentrating. She typically goes to bed around 9 PM and gets out of bed between 2 and 3 AM. She does not have any trouble falling asleep. She takes 30-minute to 1-hour daytime naps approximately 3 times per week. She has no history of severe illness and does not take any medication. Which of the following is the most likely diagnosis?
- A. Non-REM sleep arousal disorder
- B. Depressive disorder
- C. Delayed sleep phase disorder
- D. Advanced sleep phase disorder (Correct Answer)
- E. Insomnia disorder
Normal sleep physiology Explanation: ***Advanced sleep phase disorder***
- The patient's early evening fatigue, difficulty staying awake through dinner, and habitual bedtime of 9 PM with waking between 2-3 AM are classic symptoms of **advanced sleep phase disorder**.
- This condition involves a consistent advance of the **major sleep episode**, occurring significantly earlier than desired and resulting in early morning awakening.
*Non-REM sleep arousal disorder*
- This disorder is characterized by recurrent episodes of **incomplete awakening** from sleep, often accompanied by behaviors like sleepwalking or sleep terrors.
- The patient's symptoms are primarily related to timing of sleep, not **arousals** from sleep.
*Depressive disorder*
- While **sleep disturbance** (insomnia or hypersomnia) is common in depression, the specific pattern of early sleep onset and early morning awakening without difficulty falling asleep points away from a primary depressive disorder here.
- The patient does not describe other critical symptoms of depression such as anhedonia, low mood, or feelings of worthlessness.
*Delayed sleep phase disorder*
- This disorder involves a **delay** in the timing of the major sleep episode, meaning individuals go to bed and wake up much later than conventional times.
- The patient's symptoms are the **opposite** of delayed sleep phase disorder, as she is going to bed and waking up earlier.
*Insomnia disorder*
- Characterized by **difficulty falling asleep**, staying asleep, or early morning awakenings with inability to return to sleep, leading to significant distress or impairment.
- The patient explicitly states she has **no trouble falling asleep**, which rules out primary insomnia as the main issue.
Normal sleep physiology US Medical PG Question 4: A 57-year-old man comes to the physician because of a 3-month history of fatigue, difficulty swallowing, and weight loss. He has smoked 1 pack of cigarettes daily for 30 years. He is 173 cm (5 ft 8 in) tall, and weighs 54 kg (120 lb); BMI is 18 kg/m2. Upper gastrointestinal endoscopy shows an exophytic tumor at the gastroesophageal junction. The patient is diagnosed with advanced esophageal adenocarcinoma. Palliative treatment is begun. Two months later, he complains of difficulty sleeping. His husband says that the patient does not get out of bed most days and has lost interest in seeing his friends. Mental status examination shows a blunted affect, slowed speech, and poor concentration. This patient is at increased risk of developing which of the following findings on polysomnography?
- A. Increased periodic sharp-wave discharge
- B. Decreased REM sleep latency (Correct Answer)
- C. Increased slow-wave sleep-cycle duration
- D. Decreased REM sleep duration
- E. Increased spike-and-wave discharge
Normal sleep physiology Explanation: ***Decreased REM sleep latency***
- This patient's symptoms of **fatigue**, **anhedonia**, **sleep disturbance**, **blunted affect**, **slowed speech**, and **poor concentration** are highly suggestive of **major depressive disorder**.
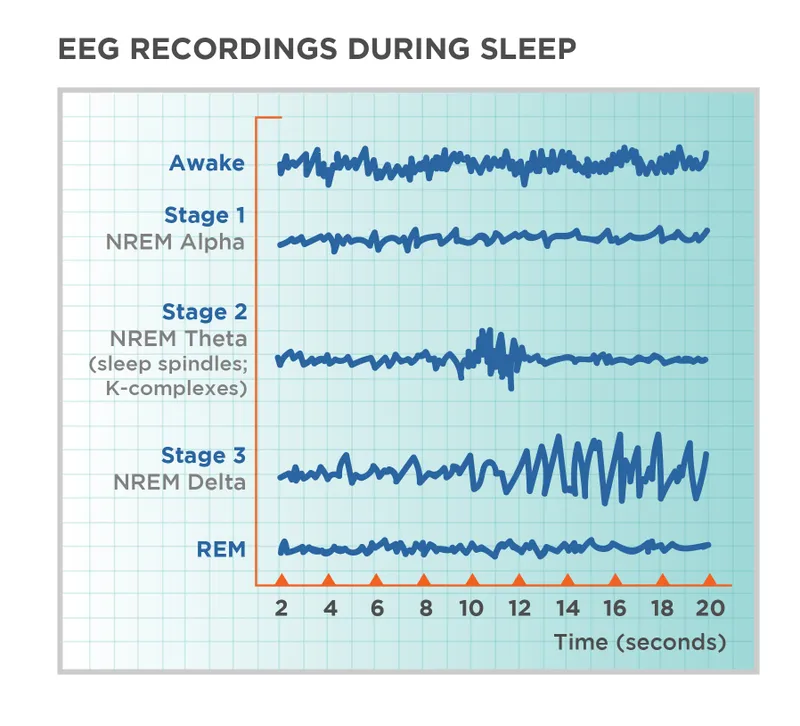
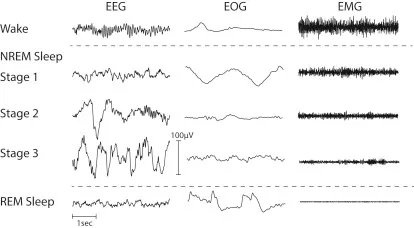
- **Depression** is associated with **decreased REM sleep latency** (shorter time to enter REM sleep) and **increased REM density** (more rapid eye movements during REM).
*Increased periodic sharp-wave discharge*
- **Periodic sharp-wave discharges** on EEG are characteristic of **Creutzfeldt-Jakob disease**, which is a **neurodegenerative prion disease**, not depression.
- The patient's presentation does not align with the neurological signs typical of CJD.
*Increased slow-wave sleep-cycle duration*
- **Slow-wave sleep (SWS)**, or deep sleep, is typically **decreased** in patients with depression.
- An increase in SWS duration would be an unusual finding in the context of major depressive disorder.
*Decreased REM sleep duration*
- While sleep architecture is altered in depression, total **REM sleep duration** is often **increased**, or at least not significantly decreased, in proportion to other sleep stages.
- The more characteristic finding is a shorter time to reach REM sleep, not necessarily a reduction in its total duration.
*Increased spike-and-wave discharge*
- **Spike-and-wave discharges** are characteristic patterns seen on EEG in patients with **epilepsy**, particularly **absence seizures**.
- There is no clinical or historical information to suggest an epileptic disorder in this patient.
Normal sleep physiology US Medical PG Question 5: A 31-year-old man presents to his primary care physician endorsing three months of decreased sleep. He reports an inability to fall asleep; although once asleep, he generally sleeps through the night and wakes up at a desired time. He has instituted sleep hygiene measures, but this has not helped. He has not felt anxious or depressed and is otherwise healthy. You prescribe him a medication that has the potential side effect of priapism. From which of the following locations is the neurotransmitter affected by this medication released?
- A. Locus ceruleus
- B. Substantia nigra
- C. Posterior pituitary
- D. Raphe nucleus (Correct Answer)
- E. Nucleus accumbens
Normal sleep physiology Explanation: ***Raphe nucleus***
- The patient's symptoms of **insomnia** without anxiety or depression, despite good sleep hygiene, suggest a potential for prescribing **trazodone**. Trazodone is an antidepressant with **sedating properties** that acts as a serotonin receptor antagonist and reuptake inhibitor.
- The **raphe nucleus** is the primary source of **serotonin** in the brain, and trazodone primarily affects serotonergic pathways, with priapism being a known but rare side effect associated with alpha-1 adrenergic blockade.
*Locus ceruleus*
- The **locus ceruleus** is the main source of **norepinephrine** in the brain, involved in arousal, attention, and stress responses.
- While norepinephrine plays a role in sleep-wake cycles, it is not the primary neurotransmitter targeted by medications commonly associated with priapism for insomnia management in this context.
*Substantia nigra*
- The **substantia nigra** is a brain structure that produces **dopamine** and is primarily involved in motor control, with its degeneration leading to Parkinson's disease.
- This region and its neurotransmitter are not typically associated with the treatment of insomnia or the specific side effect of priapism.
*Posterior pituitary*
- The **posterior pituitary** gland releases **oxytocin** and **vasopressin** (ADH), which are hormones synthesized in the hypothalamus.
- This structure is part of the endocrine system and is not directly involved in the central nervous system pathways targeted by medications for insomnia with the potential for priapism.
*Nucleus accumbens*
- The **nucleus accumbens** is a key component of the **reward pathway** in the brain, primarily utilizing **dopamine** and involved in motivation, pleasure, and addiction.
- While dopamine has some modulatory roles in sleep, it is not the primary target for effective insomnia treatment or associated with the specific side effects mentioned.
Normal sleep physiology US Medical PG Question 6: A 15-year-old boy is brought to the physician with excessive daytime sleepiness over the past year. His parents are concerned with his below-average school performance over the last 3 months. He goes to bed around midnight and wakes up at 7 am on school days, but sleeps in late on weekends. He exercises regularly after school. He usually has a light snack an hour before bed. He does not snore or have awakenings during sleep. He has no history of a serious illness and takes no medications. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. He does not smoke or drink alcohol. There is no history of a similar problem in the family. His vital signs are within normal limits. His BMI is 22 kg/m2. Physical examination shows no abnormal findings. Which of the following is the most appropriate recommendation at this time?
- A. Take melatonin before bedtime
- B. Avoid snacks before bedtime
- C. Decrease exercise intensity
- D. Increase nighttime sleep hours (Correct Answer)
- E. Take a nap in the afternoon
Normal sleep physiology Explanation: ***Increase nighttime sleep hours***
- The patient's pattern of going to bed at midnight and waking at 7 AM on school days, along with sleeping in late on weekends, suggests a **chronic sleep deficit** accumulated during the week. Adolescents typically require 8-10 hours of sleep per night.
- The excessive daytime sleepiness and declining school performance are strong indicators of insufficient sleep, and **prioritizing more sleep during school nights** is the most direct intervention.
*Take melatonin before bedtime*
- Melatonin supplements are typically used for **sleep-onset insomnia** or **circadian rhythm disorders**, neither of which is clearly indicated here.
- There is no evidence presented of difficulty falling asleep; rather, the issue appears to be insufficient duration of sleep due to **late bedtime schedules**.
*Avoid snacks before bedtime*
- While heavy meals before bedtime can disrupt sleep, this patient reports having only a **light snack**, which is unlikely to be the primary cause of his significant daytime sleepiness.
- There is no mention of indigestion or gastrointestinal discomfort after the snack that would point to this as a problem.
*Decrease exercise intensity*
- Regular exercise generally **improves sleep quality**, and there's no indication that the patient's exercise routine is negatively impacting his sleep.
- While very intense exercise too close to bedtime can be disruptive for some, exercise itself is generally beneficial for sleep and overall health; therefore, reducing it would not be a primary recommendation.
*Take a nap in the afternoon*
- While naps can temporarily alleviate daytime sleepiness, they can also **disrupt nighttime sleep patterns** by reducing sleep drive.
- Napping would be treating the symptom rather than the root cause, which is a **chronic lack of sufficient nighttime sleep**.
Normal sleep physiology US Medical PG Question 7: A 37-year-old male presents to general medical clinic reporting sleeping difficulties. He states that he has daytime sleepiness, having fallen asleep several times while driving his car recently. He sometimes experiences very vivid dreams just before awakening. You ask the patient's wife if she has witnessed any episodes where her husband lost all muscle tone and fell to the ground, and she confirms that he has not had this symptom. The patient notes that this condition runs in his family, and he desperately asks for treatment. You begin him on a first-line medication for this illness, which works by which mechanism of action?
- A. Dopamine reuptake inhibition (Correct Answer)
- B. Serotonin reuptake inhibition
- C. Mu opioid receptor agonism
- D. GABA receptor agonism
- E. Alpha-2 adrenergic receptor antagonism
Normal sleep physiology Explanation: ***Dopamine reuptake inhibition***
- The patient's symptoms of **excessive daytime sleepiness**, falling asleep while driving, and vivid dreams (hypnagogic hallucinations) are classic for **narcolepsy type 2** (without cataplexy).
- **First-line treatment** for excessive daytime sleepiness in narcolepsy is **modafinil** or **armodafinil**, which work primarily through **dopamine reuptake inhibition** (along with other mechanisms including effects on orexin neurons).
- Alternative first-line agents include **methylphenidate** and **amphetamines**, which also work via **dopamine and norepinephrine reuptake inhibition**.
- These medications promote wakefulness and are supported by AASM and AAN clinical practice guidelines.
*Serotonin reuptake inhibition*
- **SSRIs** and **SNRIs** are sometimes used in narcolepsy but primarily for **cataplexy** management, not daytime sleepiness.
- This patient has **no cataplexy**, making this mechanism less relevant for his primary complaint.
- Not considered first-line for the excessive daytime sleepiness that is this patient's main concern.
*Alpha-2 adrenergic receptor antagonism*
- This is the mechanism of **mirtazapine**, an atypical antidepressant.
- **Not a first-line treatment** for narcolepsy or excessive daytime sleepiness.
- Mirtazapine is actually somewhat sedating and would worsen daytime sleepiness, not improve it.
*Mu opioid receptor agonism*
- This describes traditional opioid analgesics, which are **not used** in narcolepsy treatment.
- Opioids cause sedation and would worsen daytime sleepiness.
- **Sodium oxybate** (used in narcolepsy) is sometimes confused with opioids, but it works primarily through GABA-B receptors, not mu opioid receptors.
*GABA receptor agonism*
- **Sodium oxybate** (gamma-hydroxybutyrate/GHB) works primarily through **GABA-B receptor agonism** and is FDA-approved for narcolepsy.
- However, it is used primarily for **cataplexy** and to improve **nighttime sleep quality**, not as first-line for daytime sleepiness alone.
- While effective, it is typically considered after trials of modafinil/stimulants due to its scheduling restrictions (Schedule III) and side effect profile.
Normal sleep physiology US Medical PG Question 8: An 8-year-old girl is brought to the physician by her parents for a 10-month history of disturbing dreams and daytime sleepiness. She has difficulty falling asleep and says she sometimes sees ghosts just before falling asleep at night. She has had a 7-kg (15-lb) weight gain during this period despite no changes in appetite. She is alert and oriented, and neurologic examination is unremarkable. During physical examination, she spontaneously collapses after the physician drops a heavy book, producing a loud noise. She remains conscious after the collapse. Polysomnography with electroencephalogram is most likely to show which of the following?
- A. Slow spike-wave pattern
- B. Periodic sharp waves
- C. Decreased delta wave sleep duration
- D. Diffuse slowing of waves
- E. Rapid onset of REM sleep (Correct Answer)
Normal sleep physiology Explanation: ***Rapid onset of REM sleep***
- The patient's symptoms of **daytime sleepiness**, **hallucinations** (seeing ghosts before sleep, i.e., **hypnagogic hallucinations**), **sleep-onset difficulty**, and the spontaneous collapse (likely **cataplexy** triggered by strong emotion/surprise) are characteristic of **narcolepsy**.
- **Narcolepsy** is often associated with a disinhibition of REM sleep, leading to its occurrence at sleep onset or within 15 minutes of falling asleep, which would be detected by **polysomnography** with **EEG**.
*Slow spike-wave pattern*
- This pattern is characteristic of **absence seizures** (petit mal seizures), which involve brief staring spells and loss of consciousness, not the constellation of sleep disturbances and cataplexy seen here.
- Absence seizures typically do not cause significant **daytime sleepiness** or **hallucinations**.
*Periodic sharp waves*
- **Periodic sharp wave complexes** are pathognomonic for **Creutzfeldt-Jakob disease** (CJD), a rapidly progressive neurodegenerative disorder.
- CJD presents with dementia, myoclonus, and other neurological signs, which are distinct from the patient's symptoms.
*Decreased delta wave sleep duration*
- **Delta wave sleep** (slow-wave sleep or N3 sleep) is a stage of deep non-REM sleep, which is important for restorative sleep.
- While sleep architecture can be disturbed in various sleep disorders, a primary decrease in delta wave sleep duration is not the most specific or hallmark finding for narcolepsy; rather, narcolepsy is defined by its REM sleep abnormalities.
*Diffuse slowing of waves*
- **Diffuse slowing of brain waves** on EEG is a non-specific finding often associated with **encephalopathy**, metabolic disturbances, or diffuse brain dysfunction.
- It does not specifically account for the unique constellation of symptoms seen in this patient, particularly the abrupt onset of sleep-related phenomena and **cataplexy**.
Normal sleep physiology US Medical PG Question 9: A 51-year-old man presents to his physician with decreased libido and inability to achieve an erection. He also reports poor sleep, loss of pleasure to do his job, and depressed mood. His symptoms started a year ago, soon after his wife got into the car accident. She survived and recovered with the minimal deficit, but the patient still feels guilty due to this case. The patient was diagnosed with diabetes 6 months ago, but he does not take any medications for it. He denies any other conditions. His weight is 105 kg (231.5 lb), his height is 172 cm (5 ft 7 in), and his waist circumference is 106 cm. The blood pressure is 150/90 mm Hg, and the heart rate is 73/min. The physical examination only shows increased adiposity. Which of the following tests is specifically intended to distinguish between the organic and psychogenic cause of the patient’s condition?
- A. Angiography
- B. Duplex ultrasound of the penis
- C. Penile tumescence testing (Correct Answer)
- D. Biothesiometry
- E. Injection of prostaglandin E1
Normal sleep physiology Explanation: ***Penile tumescence testing***
- This test, often performed as a **nocturnal penile tumescence (NPT) test**, measures erections during sleep. The presence of normal nocturnal erections indicates a **psychogenic** cause for erectile dysfunction, as physiological mechanisms are intact.
- The absence of nocturnal erections, despite adequate sleep, suggests an **organic** cause, as the body's natural erectile reflex is impaired.
*Angiography*
- **Angiography** is an invasive procedure used to visualize blood vessels and identify arterial blockages or abnormalities. It is typically reserved for cases where vascular disease is strongly suspected as the cause of erectile dysfunction and often considered before revascularization surgery.
- While it can identify **vascular organic causes** of erectile dysfunction, it does not directly differentiate between psychogenic and organic causes universally; it focuses specifically on arterial flow.
*Duplex ultrasound of the penis*
- **Duplex ultrasound** evaluates blood flow within the penile arteries and veins, assessing both arterial inflow and veno-occlusive function. It aids in diagnosing **vascular abnormalities**, such as arterial insufficiency or venous leakage.
- Similar to angiography, duplex ultrasound identifies specific **organic vascular pathologies** but does not definitively distinguish between psychogenic and organic causes of erectile dysfunction if vascular function is normal.
*Biothesiometry*
- **Biothesiometry** measures penile vibratory sensation threshold, which assesses **neurological function** of the penis. It helps detect peripheral neuropathy, a potential organic cause of erectile dysfunction, especially in diabetic patients.
- While useful for uncovering **neurological organic causes**, biothesiometry does not differentiate between psychogenic and organic etiologies in cases where neurological function is normal.
*Injection of prostaglandin E1*
- The **injection of prostaglandin E1** (alprostadil) is a diagnostic and therapeutic tool that induces an erection by relaxing smooth muscle in the penile arteries, increasing blood flow. A strong response indicates intact vascular smooth muscle function.
- A successful response to prostaglandin E1 suggests that vascular smooth muscle and neurological pathways are largely functional, which can indirectly point away from severe organic causes, but it's not a definitive differentiator between **psychogenic and organic** causes as it by-passes some physiological mechanisms.
Normal sleep physiology US Medical PG Question 10: A 21-year-old man presents to the clinic complaining of feeling tired during the day. He is concerned as his grades in school have worsened and he does not want to lose his scholarship. Upon further questioning, the patient describes frequently experiencing a dreamlike state before falling asleep and after waking up. He also has frequent nighttime awakenings where he finds himself unable to move. He denies snoring. The patient does not drink alcohol or abuse any other drugs. The patient's BMI is 21 kg/m2, and his vital signs are all within normal limits. What is this patient's diagnosis?
- A. Obstructive sleep apnea (OSA)
- B. Insomnia
- C. Alcohol withdrawal
- D. Delayed sleep phase syndrome (DSPS)
- E. Narcolepsy (Correct Answer)
Normal sleep physiology Explanation: ***Narcolepsy***
- The patient's symptoms of **excessive daytime sleepiness**, **hypnagogic/hypnopompic hallucinations** (dreamlike state before falling asleep and after waking up), and **sleep paralysis** (unable to move during nighttime awakenings) are the **classic tetrad of narcolepsy** (cataplexy is the 4th feature, not present here).
- The absence of snoring, normal BMI, and lack of alcohol/drug use rule out other common causes of sleep disturbances, supporting the diagnosis of narcolepsy.
- Narcolepsy is a **chronic sleep-wake disorder** caused by hypothalamic hypocretin (orexin) deficiency.
*Obstructive sleep apnea (OSA)*
- While OSA also causes **daytime sleepiness**, a key feature is **snoring**, which this patient denies.
- OSA is often associated with obesity, but this patient has a **normal BMI of 21 kg/m²**.
- OSA would not explain the hypnagogic hallucinations or sleep paralysis.
*Insomnia*
- Insomnia primarily involves difficulty initiating or maintaining sleep, leading to **insufficient sleep quantity or quality**.
- This patient's symptoms are more specific, including episodes of sleep paralysis and vivid dreamlike states, rather than just general difficulty sleeping.
- The hallmark features of narcolepsy distinguish this from simple insomnia.
*Alcohol withdrawal*
- Alcohol withdrawal can cause **sleep disturbances**, but it is typically accompanied by other symptoms like tremors, anxiety, autonomic hyperactivity, and potentially seizures, none of which are present.
- The patient **explicitly denies drinking alcohol**, making this diagnosis highly unlikely.
*Delayed sleep phase syndrome (DSPS)*
- DSPS is a **circadian rhythm disorder** characterized by a delayed sleep-wake cycle, where individuals fall asleep and wake up later than desired.
- While it can cause daytime fatigue if individuals are forced to wake up early, it does **not** involve the specific symptoms of hypnagogic/hypnopompic hallucinations or sleep paralysis seen in this patient.
- DSPS is primarily a timing issue, not a neurological sleep disorder.
More Normal sleep physiology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 Accounts for ~75% of total sleep. Progresses from light to deep sleep, crucial for physical restoration. Characterized by ↓ heart rate, blood pressure, and respiration.
Accounts for ~75% of total sleep. Progresses from light to deep sleep, crucial for physical restoration. Characterized by ↓ heart rate, blood pressure, and respiration.

