Insomnia disorder US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Insomnia disorder. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Insomnia disorder US Medical PG Question 1: An otherwise healthy 55-year-old woman comes to the physician because of a 7-month history of insomnia. She has difficulty initiating sleep, and her sleep onset latency is normally about 1 hour. She takes melatonin most nights. The physician gives the following recommendations: leave the bedroom when unable to fall asleep within 20 minutes to read or listen to music; return only when sleepy; avoid daytime napping. These recommendations are best classified as which of the following?
- A. Cognitive behavioral therapy
- B. Relaxation
- C. Improved sleep hygiene
- D. Stimulus control therapy (Correct Answer)
- E. Sleep restriction
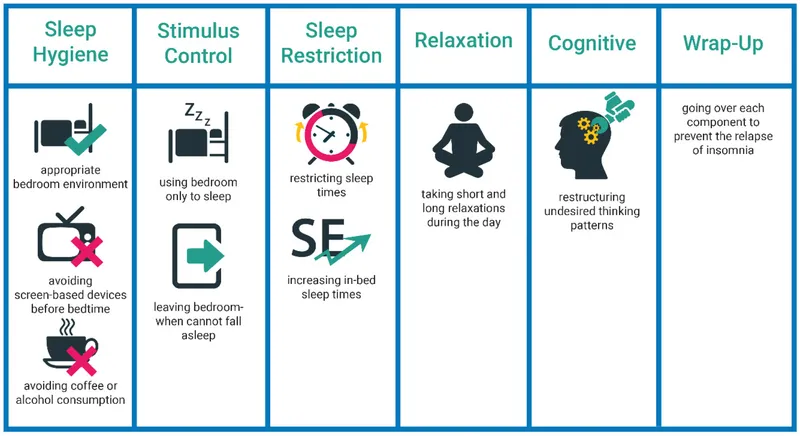
Insomnia disorder Explanation: ***Stimulus control therapy***
- This therapy focuses on **removing cues** that hinder sleep and **establishing a strong association** between the bed/bedroom and sleep.
- The recommendations (leaving the bedroom when awake, returning only when sleepy, avoiding daytime naps) are classic components of **stimulus control therapy** for insomnia.
*Cognitive behavioral therapy*
- **CBT-I** is a comprehensive approach that includes stimulus control, sleep hygiene, relaxation techniques, and cognitive restructuring.
- While stimulus control is a part of CBT-I, the recommendations provided are specifically designed to address conditioning and are thus best classified as stimulus control therapy.
*Relaxation*
- Relaxation techniques involve methods like **progressive muscle relaxation**, **deep breathing exercises**, or **meditation** to reduce physiological arousal.
- The given recommendations do not directly involve these types of activities but rather focus on changing behaviors around sleep.
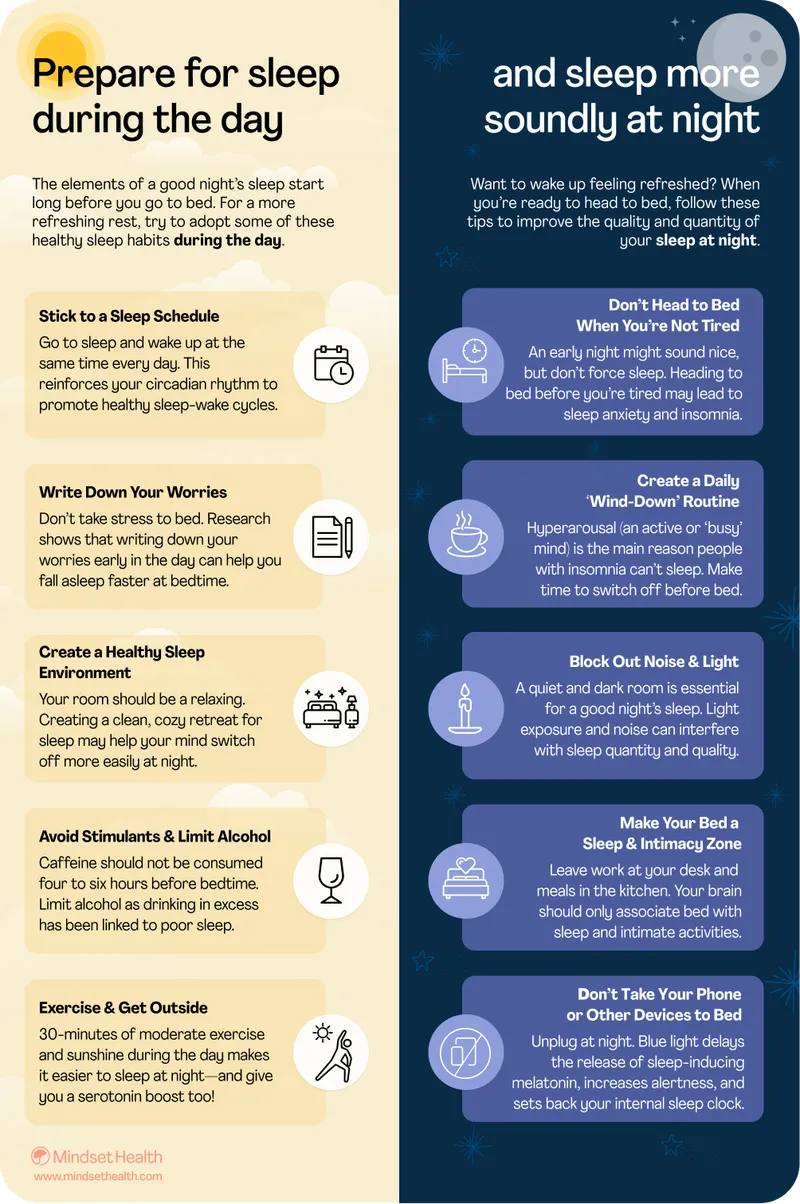
*Improved sleep hygiene*
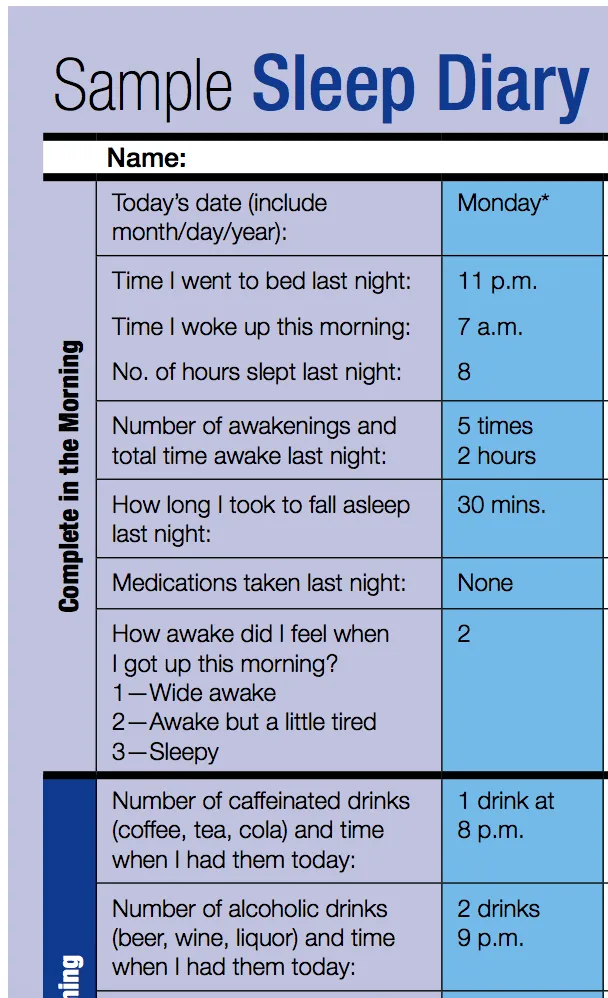
- Sleep hygiene involves practices that promote good sleep, such as maintaining a **regular sleep schedule**, ensuring a **comfortable sleep environment**, and **avoiding caffeine/alcohol** before bed.
- While avoiding daytime naps is related to sleep hygiene, the core recommendations (leaving the bedroom when awake, returning only when sleepy) specifically target conditional associations with the bed, making them more characteristic of stimulus control.
*Sleep restriction*
- Sleep restriction therapy involves **limiting the time spent in bed** to the actual time asleep, with the goal of building up sleep drive and improving sleep efficiency.
- The recommendations given do not specify a fixed reduction in time allowed in bed but rather focus on behavioral responses to wakefulness in bed.
Insomnia disorder US Medical PG Question 2: A 53-year-old woman presented to her PCP with one week of difficulty falling asleep, despite having good sleep hygiene. She denies changes in her mood, weight loss, and anhedonia. She has had difficulty concentrating and feels tired throughout the day. Recently, she was fired from her previous job. What medication would be most helpful for this patient?
- A. Citalopram
- B. Diphenhydramine
- C. Quetiapine
- D. Diazepam
- E. Zolpidem (Correct Answer)
Insomnia disorder Explanation: ***Zolpidem***
- This patient presents with **insomnia** characterized by **difficulty falling asleep**, which is the primary indication for zolpidem.
- Zolpidem is a **non-benzodiazepine GABA-A receptor agonist** that acts quickly to induce sleep, making it effective for sleep onset insomnia.
*Citalopram*
- **Citalopram** is an **SSRI** primarily used for treating depression and anxiety disorders, which are not explicitly indicated as primary issues for this patient.
- While it can sometimes help with sleep in depressed patients, its **onset of action is slow** (weeks), and it is not a first-line agent for acute insomnia.
*Diphenhydramine*
- **Diphenhydramine** is an **antihistamine** with sedative properties, often used for occasional insomnia, but it can lead to significant **daytime sedation, anticholinergic side effects**, and is generally not recommended for chronic use.
- The patient's presentation suggests a need for more targeted and potentially long-term management beyond an over-the-counter antihistamine.
*Quetiapine*
- **Quetiapine** is an **antipsychotic** medication that is sometimes used off-label for insomnia due to its sedative effects, but it carries significant **side effects** like metabolic syndrome, orthostatic hypotension, and tardive dyskinesia.
- It is generally **not recommended as a first-line treatment for insomnia** without co-occurring psychiatric conditions like bipolar disorder or schizophrenia.
*Diazepam*
- **Diazepam** is a **benzodiazepine** that can be used for insomnia, but it has a **long half-life** leading to daytime sedation and a **high potential for dependence and abuse**.
- Its use should be limited to short-term treatment of severe insomnia and is generally avoided in patients who deny mood changes and anhedonia, suggesting a less complex underlying issue.
Insomnia disorder US Medical PG Question 3: A 27-year-old man presents to his primary care physician with concerns about poor sleep quality. The patient states that he often has trouble falling asleep and that it is negatively affecting his studies. He is nervous that he is going to fail out of graduate school. He states that he recently performed poorly at a lab meeting where he had to present his research. This has been a recurrent issue for the patient any time he has had to present in front of groups. Additionally, the patient is concerned that his girlfriend is going to leave him and feels the relationship is failing. The patient has a past medical history of irritable bowel syndrome for which he takes fiber supplements. His temperature is 98.9°F (37.2°C), blood pressure is 117/68 mmHg, pulse is 80/min, respirations are 12/min, and oxygen saturation is 98% on room air. Physical exam is within normal limits. Which of the following is the best initial step in management?
- A. Duloxetine
- B. Alprazolam during presentations
- C. Fluoxetine
- D. Cognitive behavioral therapy (Correct Answer)
- E. Propranolol during presentations
Insomnia disorder Explanation: ***Cognitive behavioral therapy***
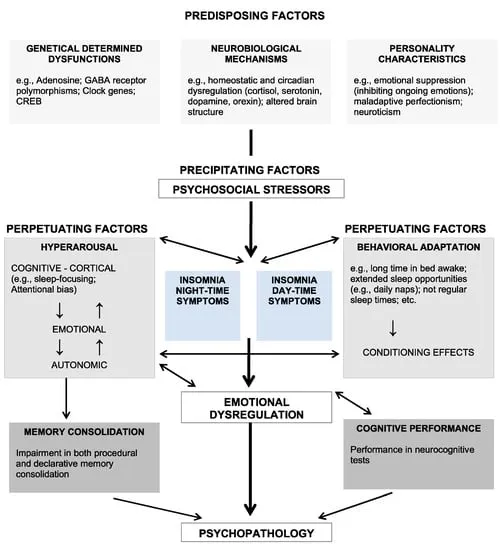
- This patient presents with symptoms highly suggestive of **generalized anxiety disorder (GAD)**, characterized by persistent worry about various life situations (academics, relationships) and difficulty sleeping. **Cognitive behavioral therapy (CBT)** is considered a first-line treatment for GAD, addressing maladaptive thought patterns and behaviors.
- CBT could also address the patient's specific social anxiety related to presentations, by teaching coping mechanisms and restructuring negative thoughts about social situations.
*Duloxetine*
- **Duloxetine** is a **serotonin-norepinephrine reuptake inhibitor (SNRI)**, which is an appropriate pharmacological treatment for GAD. However, initial management for anxiety disorders, especially in a patient expressing concern about medication side effects or preference for non-pharmacological approaches, often prioritizes psychotherapy like CBT.
- While it could be considered, it is typically not the *best initial step* before exploring non-pharmacological options, given the patient's concerns are not immediately life-threatening and psychotherapeutic options have high efficacy.
*Fluoxetine*
- **Fluoxetine** is a **selective serotonin reuptake inhibitor (SSRI)** and is a first-line pharmacological treatment for GAD.
- Similar to duloxetine, while an effective medication, it is not always the *best initial step* as many patients prefer to try psychotherapy first, and it doesn't address the underlying maladaptive thought processes in the same way CBT does.
*Alprazolam during presentations*
- **Alprazolam** is a **benzodiazepine** that provides rapid relief of anxiety symptoms. However, it is primarily used for **acute, short-term anxiety**, not as a long-term solution for generalized anxiety or social anxiety.
- Chronic use of benzodiazepines carries risks of **tolerance, dependence, and withdrawal symptoms**, making it unsuitable as an initial management strategy for persistent anxiety.
*Propranolol during presentations*
- **Propranolol** is a **beta-blocker** that can help manage the **physical symptoms of performance anxiety** (e.g., tremors, palpitations) by blocking adrenergic receptors.
- While helpful for specific situations like presentations for social anxiety, it does not address the underlying cognitive distortions or generalized anxiety disorder, and therefore is not the best initial comprehensive management approach.
Insomnia disorder US Medical PG Question 4: A 35-year-old man comes to the Veterans Affairs hospital because of a 2-month history of anxiety. He recently returned from his third deployment to Iraq, where he served as a combat medic. He has had difficulty readjusting to civilian life. He works as a taxi driver but had to take a leave of absence because of difficulties with driving. Last week, he hit a stop sign because he swerved out of the way of a grocery bag that was in the street. He has difficulty sleeping because of nightmares about the deaths of some of the other soldiers in his unit and states, “it's my fault, I could have saved them. Please help me.” Mental status examination shows a depressed mood and a restricted affect. There is no evidence of suicidal ideation. Which of the following is the most appropriate initial step in treatment?
- A. Dialectical behavioral therapy
- B. Venlafaxine therapy
- C. Cognitive behavioral therapy (Correct Answer)
- D. Motivational interviewing
- E. Prazosin therapy
Insomnia disorder Explanation: ***Cognitive behavioral therapy***
- **Cognitive Behavioral Therapy (CBT)** is considered a first-line psychological treatment for **Post-Traumatic Stress Disorder (PTSD)**, which the patient's symptoms (deployments, intrusive thoughts, nightmares, avoidance, guilt) strongly suggest.
- CBT helps individuals identify and challenge **maladaptive thought patterns** and behaviors related to the trauma, fostering new coping mechanisms.
*Dialectical behavioral therapy*
- **Dialectical Behavioral Therapy (DBT)** is primarily used for individuals with **Borderline Personality Disorder** or severe emotional dysregulation.
- While it can help with emotional regulation, it is not the **first-line therapy** specifically targeting trauma-related cognitive distortions and avoidance behaviors seen in PTSD.
*Venlafaxine therapy*
- **Venlafaxine**, an SNRI, is an antidepressant that can be effective for PTSD symptoms. However, current guidelines recommend **psychotherapy (like CBT)** as the initial step, especially when feasible.
- While pharmacotherapy can be used, it's typically considered **adjunctive** or for cases where psychotherapy alone is insufficient or not preferred.
*Motivational interviewing*
- **Motivational interviewing** is a patient-centered counseling style used to address ambivalence and enhance a person's **intrinsic motivation** for change.
- It is often utilized in substance abuse treatment or when patients are resistant to treatment, but it is not a primary, standalone treatment for the core symptoms of PTSD.
*Prazosin therapy*
- **Prazosin** is an alpha-1 antagonist used off-label to treat **PTSD-related nightmares** and sleep disturbances.
- While it can be helpful for a specific symptom, it does not address the broader spectrum of PTSD symptoms, such as intrusive thoughts, avoidance, or negative cognitions.
Insomnia disorder US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Insomnia disorder Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Insomnia disorder US Medical PG Question 6: A 25-year-old male presents to his primary care physician with a chief complaint of anxiety and fatigue. The patient states that during this past week he has had final exams and has been unable to properly study and prepare because he is so exhausted. He states that he has been going to bed early but has been unable to get a good night’s sleep. The patient admits to occasional cocaine and marijuana use. Otherwise, the patient has no significant past medical history and is not taking any medications. On physical exam you note a tired and anxious appearing young man. His neurological exam is within normal limits. The patient states that he fears he will fail his courses if he does not come up with a solution. Which of the following is the best initial step in management?
- A. Polysomnography
- B. Sleep hygiene education (Correct Answer)
- C. Alprazolam
- D. Melatonin
- E. Zolpidem
Insomnia disorder Explanation: ***Sleep hygiene education***
- This is the **best initial step** because it addresses lifestyle factors that commonly contribute to **insomnia and fatigue**, especially during periods of stress like final exams.
- Helping the patient establish **regular sleep patterns**, avoid stimulants, and create a conducive sleep environment can significantly improve sleep quality without medication.
*Polysomnography*
- This is a diagnostic test typically reserved for when a **primary sleep disorder** like sleep apnea or restless legs syndrome is suspected.
- Given the patient's acute stressor (final exams) and **drug use**, lifestyle interventions should be tried first before pursuing expensive and invasive testing.
*Alprazolam*
- This is a **benzodiazepine** that can be used for acute anxiety or insomnia, but it carries a risk of **dependence, tolerance, and withdrawal**.
- It is not a first-line treatment for a patient experiencing sleep difficulties primarily due to stress and poor sleep habits, and its use should be avoided in those with a history of substance abuse.
*Melatonin*
- Melatonin can be helpful for **circadian rhythm disorders** or jet lag, but its efficacy for primary insomnia is limited and inconsistent.
- While it has fewer side effects than prescription hypnotics, **sleep hygiene education** is still a more fundamental and effective initial approach for this patient.
*Zolpidem*
- This is a **non-benzodiazepine hypnotic** often prescribed for short-term insomnia, but it has potential side effects like **next-day drowsiness** and can be abused, especially in individuals with a history of substance use.
- **Sleep hygiene** should always be optimized first, especially in a young patient whose sleep issues are clearly linked to stress and lifestyle.
Insomnia disorder US Medical PG Question 7: A 17-year-old high school student comes to the physician because of a 6-month history of insomnia. On school nights, he goes to bed around 11 p.m. but has had persistent problems falling asleep and instead studies at his desk until he feels sleepy around 2 a.m. He does not wake up in the middle of the night. He is worried that he does not get enough sleep. He has significant difficulties waking up on weekdays and has repeatedly been late to school. At school, he experiences daytime sleepiness and drinks 1–2 cups of coffee in the mornings. He tries to avoid daytime naps. On the weekends, he goes to bed around 2 a.m. and sleeps in until 10 a.m., after which he feels rested. He has no history of severe illness and does not take medication. Which of the following most likely explains this patient's sleep disorder?
- A. Inadequate sleep hygiene
- B. Irregular sleep-wake disorder
- C. Psychophysiologic insomnia
- D. Delayed sleep-wake disorder (Correct Answer)
- E. Advanced sleep-wake disorder
Insomnia disorder Explanation: ***Delayed sleep-wake disorder***
- This patient exhibits a consistent pattern of **delayed sleep onset** and **delayed wake time**, particularly evident on weekends when he can follow his natural circadian rhythm (going to bed at 2 AM and waking at 10 AM).
- The symptoms, including difficulty falling asleep at conventional times, difficulty waking for school, and daytime sleepiness, are classic for **delayed sleep-wake phase disorder**, where an individual's internal clock is misaligned with societal expectations.
*Inadequate sleep hygiene*
- While aspects like studying in bed are **poor sleep hygiene**, the core issue is not simply bad habits but a fundamental misalignment of his **circadian rhythm** as evidenced by his consistent late sleep onset and wake times when allowed.
- The patient's ability to sleep well and feel rested on weekends when he can follow his natural rhythm suggests that hygiene alone isn't the primary cause.
*Irregular sleep-wake disorder*
- This disorder is characterized by a **lack of a discernible sleep-wake rhythm**, with sleep periods fragmented and scattered throughout the 24-hour day.
- The patient, however, demonstrates a clear, albeit delayed, sleep schedule; he sleeps in one consolidated block and feels rested when allowed to do so.
*Psychophysiologic insomnia*
- This condition involves heightened arousal and **anxiety surrounding sleep**, leading to difficulty falling asleep at night and often improved sleep in novel environments or away from home.
- While he expresses worry about not getting enough sleep, his sleep issues are primarily due to a shifted circadian phase, not just anxiety about sleep itself, and he sleeps restfully when allowed to follow his delayed rhythm.
*Advanced sleep-wake disorder*
- This disorder is characterized by a **habitually early sleep onset** and **early morning awakening**, typically several hours earlier than desired or conventional times.
- The patient, in contrast, consistently struggles to fall asleep until very late hours and desires a later wake time.
Insomnia disorder US Medical PG Question 8: A 77-year-old woman is brought to her primary care provider by her daughter with behavioral changes and an abnormally bad memory for the past few months. The patient’s daughter says she sometimes gets angry and aggressive while at other times she seems lost and stares at her surroundings. Her daughter also reports that she has seen her mother talking to empty chairs. The patient says she sleeps well during the night but still feels sleepy throughout the day. She has no problems getting dressed and maintaining her one bedroom apartment. Past medical history is significant for mild depression and mild osteoporosis. Current medications include escitalopram, alendronic acid, and a multivitamin. The patient is afebrile, and her vital signs are within normal limits. On physical examination, the patient is alert and oriented and sitting comfortably in her chair. A mild left-hand tremor is noted. Muscle strength is 5 out of 5 in the upper and lower extremities bilaterally, but muscle tone is slightly increased. She can perform repetitive alternating movements albeit slowly. She walks with a narrow gait and has mild difficulty turning. Which of the following is the most likely diagnosis in this patient?
- A. Lewy body dementia (Correct Answer)
- B. Alzheimer's disease
- C. Serotonin syndrome
- D. Frontotemporal dementia
- E. Delirium
Insomnia disorder Explanation: ***Lewy body dementia***
- This patient exhibits **fluctuating cognition** (being lost and staring, behavioral changes), **recurrent visual hallucinations** (talking to empty chairs), and spontaneous motor features of **parkinsonism** (mild left-hand tremor, increased muscle tone, slow alternating movements, narrow gait, difficulty turning), all core features of Lewy body dementia.
- The **insidious onset** and progressive decline over months, along with the symptom triad, fit the diagnostic criteria for Lewy body dementia.
*Alzheimer's disease*
- While Alzheimer's involves memory loss and cognitive decline, it is not typically associated with **prominent early visual hallucinations** or **parkinsonian features** at presentation.
- Alzheimer's disease often presents with **memory impairment as the most prominent early symptom**, often preceding other cognitive deficits by years.
*Serotonin syndrome*
- This is an acute drug reaction characterized by a triad of **mental status changes**, **autonomic hyperactivity**, and **neuromuscular abnormalities**, usually developing rapidly after medication changes affecting serotonin levels.
- The patient's symptoms have been present for months, the vital signs are stable, and her medications (escitalopram) have been stable, making an **acute syndrome** like serotonin syndrome unlikely.
*Frontotemporal dementia*
- This type of dementia primarily affects personality, behavior, and language, with **prominent disinhibition or apathy**.
- While behavioral changes are present, the patient's prominent **visual hallucinations** and **parkinsonian features** are not characteristic of frontotemporal dementia.
*Delirium*
- Delirium is characterized by an **acute onset** and fluctuating course of attention and awareness, often triggered by an underlying medical condition, medication, or infection.
- The patient's symptoms have progressed over **several months**, rather than hours or days, and she is afebrile with stable vital signs, making delirium less likely.
Insomnia disorder US Medical PG Question 9: A 50-year-old man with severe obstructive sleep apnea (AHI 65 events/hour) and CPAP intolerance despite multiple mask trials undergoes maxillomandibular advancement surgery. Three months post-operatively, he continues to report excessive daytime sleepiness and his bed partner reports persistent snoring. Post-operative polysomnography shows AHI of 28 events/hour. He has a BMI of 38 kg/m² (unchanged from pre-surgery) and crowded posterior pharynx. Evaluate the next management strategy.
- A. Hypoglossal nerve stimulation therapy evaluation
- B. Repeat maxillomandibular advancement with greater advancement distance
- C. Observe for another 3 months as surgical swelling may still be resolving
- D. Revisit CPAP therapy with auto-adjusting pressure settings (Correct Answer)
- E. Proceed directly to tracheostomy for definitive airway management
Insomnia disorder Explanation: ***Revisit CPAP therapy with auto-adjusting pressure settings***
- **Maxillomandibular advancement (MMA)** significantly reduced the **Apnea-Hypopnea Index (AHI)** from 65 to 28; while not curative, this anatomical change may lower the **positive airway pressure (PAP)** requirements, potentially improving **patient tolerance**.
- **Auto-CPAP** is the most appropriate next step to determine if the post-surgical airway allows for successful treatment at manageable pressures, especially before considering more invasive options.
*Hypoglossal nerve stimulation therapy evaluation*
- This patient's **BMI of 38 kg/m²** currently exceeds the standard FDA-approved threshold of **35 kg/m²** for **hypoglossal nerve stimulation**.
- Evaluation requires a **Drug-Induced Sleep Endoscopy (DISE)** to check for **concentric palatal collapse**, but primary medical optimization remains the priority.
*Repeat maxillomandibular advancement with greater advancement distance*
- **Revision MMA** carries significantly higher surgical risks, including **nerve injury** and **non-union**, and is generally not indicated when initial surgery was technically successful.
- The persistent **AHI of 28** is more likely due to the patient's **persistent obesity** and soft tissue volume rather than inadequate bony advancement.
*Observe for another 3 months as surgical swelling may still be resolving*
- Three months is typically sufficient for the resolution of **post-operative edema** impacting the airway, and active treatment is needed for **moderate OSA** (AHI 28) and **daytime sleepiness**.
- Delaying management puts the patient at continued risk for **cardiovascular complications** and accidents associated with **excessive sleepiness**.
*Proceed directly to tracheostomy for definitive airway management*
- **Tracheostomy** is the most invasive surgical intervention and is reserved for **life-threatening OSA** where all other medical and surgical options have failed.
- It represents a significant **quality-of-life burden** and should not be considered until less invasive modalities like post-surgical **PAP therapy** are re-attempted.
Insomnia disorder US Medical PG Question 10: A 70-year-old man with newly diagnosed Parkinson disease and REM sleep behavior disorder is being considered for treatment. His neurologist is concerned about medication interactions and disease progression. He also has mild cognitive impairment, orthostatic hypotension, and a history of visual hallucinations. Evaluate the optimal therapeutic approach considering his complex medical profile.
- A. Quetiapine for both hallucinations and RBD symptoms
- B. Clonazepam 0.5 mg at bedtime with close monitoring for falls
- C. Rivastigmine to address cognitive impairment and sleep disturbance
- D. Melatonin 3-12 mg at bedtime as first-line therapy (Correct Answer)
- E. Pramipexole dose adjustment to suppress REM sleep
Insomnia disorder Explanation: ***Melatonin 3-12 mg at bedtime as first-line therapy***
- **Melatonin** is the preferred first-line treatment for **REM sleep behavior disorder (RBD)** in elderly patients with neurodegeneration due to its excellent safety profile.
- It effectively reduces **dream enactment** with a lower risk of side effects like **excessive sedation** or motor instability compared to other agents.
*Quetiapine for both hallucinations and RBD symptoms*
- While **Quetiapine** is used to manage **visual hallucinations** in Parkinson's, it is not an established or effective therapy for managing **RBD symptoms**.
- It may worsen **orthostatic hypotension** and daytime somnolence, complicating the patient's existing clinical state.
*Clonazepam 0.5 mg at bedtime with close monitoring for falls*
- **Clonazepam** is highly effective for RBD but is generally avoided in patients with **mild cognitive impairment** and **orthostatic hypotension** due to the high risk of **confusion** and **falls**.
- It can also exacerbate **obstructive sleep apnea** or cause significant **morning-after sedation** in the elderly.
*Rivastigmine to address cognitive impairment and sleep disturbance*
- **Rivastigmine**, a cholinesterase inhibitor, is used for **Parkinson disease dementia** but is not the primary treatment for **REM sleep behavior disorder**.
- Although it may help cognitive symptoms, it does not reliably suppress the physical **dream enactment** characteristic of RBD.
*Pramipexole dose adjustment to suppress REM sleep*
- **Dopamine agonists** like **Pramipexole** are known to potentially **worsen RBD** and can significantly increase the frequency of **visual hallucinations**.
- Increasing the dose in this patient would likely exacerbate his **psychosis** and **orthostatic hypotension**.
More Insomnia disorder US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.