Circadian rhythm sleep-wake disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Circadian rhythm sleep-wake disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Circadian rhythm sleep-wake disorders US Medical PG Question 1: A 57-year-old man comes to the physician because of a 3-month history of fatigue, difficulty swallowing, and weight loss. He has smoked 1 pack of cigarettes daily for 30 years. He is 173 cm (5 ft 8 in) tall, and weighs 54 kg (120 lb); BMI is 18 kg/m2. Upper gastrointestinal endoscopy shows an exophytic tumor at the gastroesophageal junction. The patient is diagnosed with advanced esophageal adenocarcinoma. Palliative treatment is begun. Two months later, he complains of difficulty sleeping. His husband says that the patient does not get out of bed most days and has lost interest in seeing his friends. Mental status examination shows a blunted affect, slowed speech, and poor concentration. This patient is at increased risk of developing which of the following findings on polysomnography?
- A. Increased periodic sharp-wave discharge
- B. Decreased REM sleep latency (Correct Answer)
- C. Increased slow-wave sleep-cycle duration
- D. Decreased REM sleep duration
- E. Increased spike-and-wave discharge
Circadian rhythm sleep-wake disorders Explanation: ***Decreased REM sleep latency***
- This patient's symptoms of **fatigue**, **anhedonia**, **sleep disturbance**, **blunted affect**, **slowed speech**, and **poor concentration** are highly suggestive of **major depressive disorder**.
- **Depression** is associated with **decreased REM sleep latency** (shorter time to enter REM sleep) and **increased REM density** (more rapid eye movements during REM).
*Increased periodic sharp-wave discharge*
- **Periodic sharp-wave discharges** on EEG are characteristic of **Creutzfeldt-Jakob disease**, which is a **neurodegenerative prion disease**, not depression.
- The patient's presentation does not align with the neurological signs typical of CJD.
*Increased slow-wave sleep-cycle duration*
- **Slow-wave sleep (SWS)**, or deep sleep, is typically **decreased** in patients with depression.
- An increase in SWS duration would be an unusual finding in the context of major depressive disorder.
*Decreased REM sleep duration*
- While sleep architecture is altered in depression, total **REM sleep duration** is often **increased**, or at least not significantly decreased, in proportion to other sleep stages.
- The more characteristic finding is a shorter time to reach REM sleep, not necessarily a reduction in its total duration.
*Increased spike-and-wave discharge*
- **Spike-and-wave discharges** are characteristic patterns seen on EEG in patients with **epilepsy**, particularly **absence seizures**.
- There is no clinical or historical information to suggest an epileptic disorder in this patient.
Circadian rhythm sleep-wake disorders US Medical PG Question 2: A 43-year-old man presents to a primary care clinic complaining of several months of fatigue and difficulty concentrating at work. He is tired throughout the day and often falls asleep briefly at work. He sleeps for 9 hours per night, falling asleep easily, waking up several times in the middle of the night, and then having trouble waking up in the morning. Physical exam is notable for obesity and a large neck circumference. His temperature is 98°F (36.7°C), blood pressure is 150/90 mmHg, pulse is 75/min, respirations are 22/min, and BMI is 33 kg/m^2. The rest of the physical exam is normal. Which of the following is the most likely cause of his fatigue?
- A. Obstructive sleep apnea (Correct Answer)
- B. Chronic fatigue syndrome
- C. Narcolepsy
- D. Circadian rhythm sleep wake disorder
- E. Hypothyroidism
Circadian rhythm sleep-wake disorders Explanation: ***Obstructive sleep apnea***
- The patient's **obesity**, **large neck circumference**, chronic fatigue, daytime sleepiness, and **disrupted nocturnal sleep with multiple awakenings** are all classic symptoms and risk factors for **obstructive sleep apnea (OSA)**.
- The nocturnal awakenings occur due to **repeated upper airway obstruction** during sleep, causing brief arousals that fragment sleep architecture despite adequate time in bed.
- The high blood pressure and increased respirations are associated with the physiological stress of repeated airway obstruction and arousal during sleep.
- **OSA is strongly associated with obesity (BMI >30) and increased neck circumference**, both present in this patient.
*Chronic fatigue syndrome*
- While fatigue is a primary symptom, chronic fatigue syndrome typically involves **post-exertional malaise** and is not characterized by the specific pattern of sleep disruption and physical risk factors (obesity, large neck circumference) seen here.
- Diagnosis requires persistent, unexplained fatigue for at least six months, along with other defining symptoms like cognitive difficulties, but the detailed sleep pattern and physical findings point away from this.
*Narcolepsy*
- Narcolepsy is characterized by **uncontrollable daytime sleep attacks** and often involves **cataplexy** (sudden loss of muscle tone triggered by strong emotions).
- While daytime sleepiness is present, the patient's nocturnal sleep pattern (waking multiple times) and physical risk factors are not typical features of narcolepsy.
- Narcolepsy patients typically have **difficulty maintaining nighttime sleep** but do not have the obesity and large neck circumference risk factors.
*Circadian rhythm sleep wake disorder*
- These disorders involve a misalignment between the **internal sleep-wake clock** and the external environment or work schedule, leading to timing difficulties rather than chronic apnea-related sleep disruption.
- The patient's ability to fall asleep easily and the specific physical findings do not align with a primary circadian rhythm disorder.
*Hypothyroidism*
- Hypothyroidism can cause fatigue, weight gain, and sometimes daytime sleepiness, but it does not typically cause the specific pattern of **nocturnal awakenings** and has no direct link to a **large neck circumference** in the context of sleep quality.
- Other classic symptoms like cold intolerance, dry skin, bradycardia, and constipation are not mentioned, and a normal temperature makes severe hypothyroidism less likely.
Circadian rhythm sleep-wake disorders US Medical PG Question 3: A 20-year-old woman reports to student health complaining of 5 days of viral symptoms including sneezing and a runny nose. She started coughing 2 days ago and is seeking cough medication. She additionally mentions that she developed a fever 2 days ago, but this has resolved. On exam, her temperature is 99.0°F (37.2°C), blood pressure is 118/76 mmHg, pulse is 86/min, and respirations are 12/min. Changes in the activity of warm-sensitive neurons in which part of her hypothalamus likely contributed to the development and resolution of her fever?
- A. Anterior hypothalamus (Correct Answer)
- B. Paraventricular nucleus
- C. Suprachiasmatic nucleus
- D. Lateral area
- E. Posterior hypothalamus
Circadian rhythm sleep-wake disorders Explanation: ***Anterior hypothalamus***
- The **anterior hypothalamus** contains warm-sensitive neurons that detect increases in body temperature and activate mechanisms for heat dissipation, such as sweating and vasodilation.
- In fever, **prostaglandins** increase the set point in the anterior hypothalamus, causing the body to retain heat and increase heat production until the new set point is reached; resolution of fever involves resetting this set point back to normal.
*Paraventricular nucleus*
- The **paraventricular nucleus** is primarily involved in neuroendocrine functions, stress response, and the regulation of appetite and autonomic nervous system.
- It plays a significant role in releasing hormones like **corticotropin-releasing hormone (CRH)** and **oxytocin**, not direct temperature regulation.
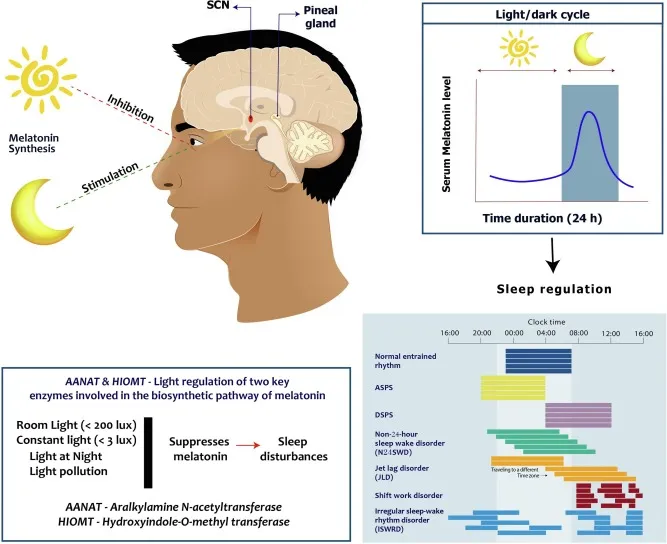
*Suprachiasmatic nucleus*
- The **suprachiasmatic nucleus (SCN)** is the body's main biological clock, regulating **circadian rhythms** including the sleep-wake cycle and daily fluctuations in body temperature.
- While it influences the normal diurnal variation in body temperature, it is not directly responsible for the acute regulation of fever.
*Lateral area*
- The **lateral hypothalamus** primarily functions as the "hunger center," stimulating foraging and feeding behavior.
- Damage to this area can lead to **anorexia** and reduced food intake, not impairments in fever response.
*Posterior hypothalamus*
- The **posterior hypothalamus** is primarily involved in heat conservation and production mechanisms, such as shivering and vasoconstriction, in response to cold.
- It contains cold-sensitive neurons and functions to raise body temperature if it falls below the set point, but it is not where the set point itself is regulated in response to pyrogens.
Circadian rhythm sleep-wake disorders US Medical PG Question 4: A 59-year-old man presents to his primary care provider with the complaint of daytime fatigue. He often has a headache that is worse in the morning and feels tired when he awakes. He perpetually feels fatigued even when he sleeps in. The patient lives alone, drinks 2-3 beers daily, drinks coffee regularly, and has a 10 pack-year smoking history. His temperature is 99.0°F (37.2°C), blood pressure is 180/110 mm Hg, pulse is 80/min, respirations are 13/min, and oxygen saturation is 98% on room air. Physical exam is notable for a BMI of 39 kg/m^2. The rest of the patient's pulmonary and neurological exams are unremarkable. Which of the following is the best next step in management?
- A. Caffeine avoidance
- B. Screening for depression
- C. Alcohol avoidance in the evening
- D. CT head
- E. Weight loss (Correct Answer)
Circadian rhythm sleep-wake disorders Explanation: ***Weight Loss***
- The patient's **BMI of 39 kg/m²** indicates **class III obesity**, which is the strongest modifiable risk factor for **obstructive sleep apnea (OSA)**. The clinical presentation—**daytime fatigue**, morning headaches, unrefreshing sleep despite adequate sleep duration, and hypertension—strongly suggests OSA.
- While **polysomnography** is the gold standard for confirming OSA, the clinical diagnosis is evident in this case. **Weight loss** is the most important initial therapeutic intervention, as even modest weight reduction (10% of body weight) can significantly improve or resolve OSA in obese patients.
- Weight loss reduces upper airway collapse by decreasing fatty tissue deposition around the pharynx and improving lung volumes. This addresses the underlying pathophysiology rather than just treating symptoms.
- This intervention also addresses his **hypertension** (180/110 mm Hg), which is commonly associated with and exacerbated by OSA.
*Caffeine avoidance*
- While excessive caffeine can disrupt sleep architecture, the patient's symptoms—particularly **morning headaches** and **unrefreshing sleep despite sleeping in**—are not characteristic of caffeine-induced insomnia, which typically presents with difficulty initiating sleep.
- These symptoms, combined with obesity and hypertension, point strongly to a sleep-related breathing disorder rather than a stimulant effect.
*Screening for depression*
- Fatigue is indeed a cardinal symptom of major depressive disorder, but the specific pattern here—**morning headaches** (from nocturnal hypercapnia/hypoxemia), **unrefreshing sleep**, and **obesity with hypertension**—is far more consistent with OSA.
- Depression screening could be considered if symptoms persist after addressing the sleep disorder, as untreated OSA can contribute to or worsen mood disorders.
*Alcohol avoidance in the evening*
- **Alcohol consumption** (2-3 beers daily) does worsen OSA by relaxing upper airway dilator muscles and suppressing arousal responses to hypoxemia. Evening alcohol avoidance would be a beneficial **adjunctive measure**.
- However, while helpful, this intervention is less impactful than weight loss. The patient's **severe obesity** (BMI 39 kg/m²) is the predominant and most modifiable risk factor, making weight loss the priority intervention that will have the greatest effect on reducing OSA severity.
*CT head*
- CT head would be indicated if there were focal neurological deficits, papilledema, or features suggesting increased intracranial pressure or structural brain pathology.
- This patient's **neurological exam is unremarkable**, and his headaches are characteristic of OSA (worse in the morning due to nocturnal CO₂ retention, improving throughout the day). Imaging is not warranted.
Circadian rhythm sleep-wake disorders US Medical PG Question 5: A 25-year-old man presents to his primary care physician for trouble with focus and concentration. The patient states that he has lived at home with his parents his entire life but recently was able to get a job at a local factory. Ever since the patient has started working, he has had trouble focusing at his job. He is unable to stay focused on any task. His boss often observes him "daydreaming" with a blank stare off into space. His boss will have to yell at him to startle him back to work. The patient states that he feels fatigued all the time and sometimes will suddenly fall asleep while operating equipment. He has tried going to bed early for the past month but is unable to fall asleep until two hours prior to his alarm. The patient fears that if this continues he will lose his job. Which of the following is the best initial step in management?
- A. Zolpidem
- B. Ethosuximide
- C. Modafinil
- D. Polysomnography (Correct Answer)
- E. Bright light therapy
Circadian rhythm sleep-wake disorders Explanation: ***Polysomnography***
- The patient's symptoms of excessive daytime sleepiness, sudden sleep attacks (possibly **cataplexy**), and difficulty maintaining sleep, along with the "daydreaming" spells, are highly suggestive of **narcolepsy**.
- **Polysomnography** is the gold standard diagnostic test for narcolepsy and other sleep disorders, confirming the diagnosis and ruling out other causes of excessive somnolence.
*Zolpidem*
- **Zolpidem** is a sedative-hypnotic primarily used for treating **insomnia** by helping to initiate and maintain sleep.
- While the patient has difficulty falling asleep, addressing the underlying cause of his **excessive daytime sleepiness** is the priority before symptomatic treatment of insomnia.
*Ethosuximide*
- **Ethosuximide** is an anti-epileptic drug specifically used to treat **absence seizures** (petit mal seizures).
- Although the patient's "daydreaming" spells might resemble absence seizures, the combination with profound daytime sleepiness and sudden sleep attacks points away from epilepsy and towards a primary sleep disorder.
*Modafinil*
- **Modafinil** is a stimulant used to promote wakefulness in patients with excessive daytime sleepiness associated with narcolepsy, obstructive sleep apnea, and shift work sleep disorder.
- While it might be a potential treatment, it is usually initiated *after* a definitive diagnosis is established through **polysomnography** and other sleep studies.
*Bright light therapy*
- **Bright light therapy** is primarily used to treat **seasonal affective disorder** and **circadian rhythm sleep disorders**, such as delayed sleep phase syndrome.
- The patient's symptoms are more severe and complex than typical circadian rhythm issues and include sudden sleep attacks, making this an inappropriate initial intervention without a proper diagnosis.
Circadian rhythm sleep-wake disorders US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Circadian rhythm sleep-wake disorders Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Circadian rhythm sleep-wake disorders US Medical PG Question 7: A 25-year-old male presents to his primary care physician with a chief complaint of anxiety and fatigue. The patient states that during this past week he has had final exams and has been unable to properly study and prepare because he is so exhausted. He states that he has been going to bed early but has been unable to get a good night’s sleep. The patient admits to occasional cocaine and marijuana use. Otherwise, the patient has no significant past medical history and is not taking any medications. On physical exam you note a tired and anxious appearing young man. His neurological exam is within normal limits. The patient states that he fears he will fail his courses if he does not come up with a solution. Which of the following is the best initial step in management?
- A. Polysomnography
- B. Sleep hygiene education (Correct Answer)
- C. Alprazolam
- D. Melatonin
- E. Zolpidem
Circadian rhythm sleep-wake disorders Explanation: ***Sleep hygiene education***
- This is the **best initial step** because it addresses lifestyle factors that commonly contribute to **insomnia and fatigue**, especially during periods of stress like final exams.
- Helping the patient establish **regular sleep patterns**, avoid stimulants, and create a conducive sleep environment can significantly improve sleep quality without medication.
*Polysomnography*
- This is a diagnostic test typically reserved for when a **primary sleep disorder** like sleep apnea or restless legs syndrome is suspected.
- Given the patient's acute stressor (final exams) and **drug use**, lifestyle interventions should be tried first before pursuing expensive and invasive testing.
*Alprazolam*
- This is a **benzodiazepine** that can be used for acute anxiety or insomnia, but it carries a risk of **dependence, tolerance, and withdrawal**.
- It is not a first-line treatment for a patient experiencing sleep difficulties primarily due to stress and poor sleep habits, and its use should be avoided in those with a history of substance abuse.
*Melatonin*
- Melatonin can be helpful for **circadian rhythm disorders** or jet lag, but its efficacy for primary insomnia is limited and inconsistent.
- While it has fewer side effects than prescription hypnotics, **sleep hygiene education** is still a more fundamental and effective initial approach for this patient.
*Zolpidem*
- This is a **non-benzodiazepine hypnotic** often prescribed for short-term insomnia, but it has potential side effects like **next-day drowsiness** and can be abused, especially in individuals with a history of substance use.
- **Sleep hygiene** should always be optimized first, especially in a young patient whose sleep issues are clearly linked to stress and lifestyle.
Circadian rhythm sleep-wake disorders US Medical PG Question 8: A 17-year-old high school student comes to the physician because of a 6-month history of insomnia. On school nights, he goes to bed around 11 p.m. but has had persistent problems falling asleep and instead studies at his desk until he feels sleepy around 2 a.m. He does not wake up in the middle of the night. He is worried that he does not get enough sleep. He has significant difficulties waking up on weekdays and has repeatedly been late to school. At school, he experiences daytime sleepiness and drinks 1–2 cups of coffee in the mornings. He tries to avoid daytime naps. On the weekends, he goes to bed around 2 a.m. and sleeps in until 10 a.m., after which he feels rested. He has no history of severe illness and does not take medication. Which of the following most likely explains this patient's sleep disorder?
- A. Inadequate sleep hygiene
- B. Irregular sleep-wake disorder
- C. Psychophysiologic insomnia
- D. Delayed sleep-wake disorder (Correct Answer)
- E. Advanced sleep-wake disorder
Circadian rhythm sleep-wake disorders Explanation: ***Delayed sleep-wake disorder***
- This patient exhibits a consistent pattern of **delayed sleep onset** and **delayed wake time**, particularly evident on weekends when he can follow his natural circadian rhythm (going to bed at 2 AM and waking at 10 AM).
- The symptoms, including difficulty falling asleep at conventional times, difficulty waking for school, and daytime sleepiness, are classic for **delayed sleep-wake phase disorder**, where an individual's internal clock is misaligned with societal expectations.
*Inadequate sleep hygiene*
- While aspects like studying in bed are **poor sleep hygiene**, the core issue is not simply bad habits but a fundamental misalignment of his **circadian rhythm** as evidenced by his consistent late sleep onset and wake times when allowed.
- The patient's ability to sleep well and feel rested on weekends when he can follow his natural rhythm suggests that hygiene alone isn't the primary cause.
*Irregular sleep-wake disorder*
- This disorder is characterized by a **lack of a discernible sleep-wake rhythm**, with sleep periods fragmented and scattered throughout the 24-hour day.
- The patient, however, demonstrates a clear, albeit delayed, sleep schedule; he sleeps in one consolidated block and feels rested when allowed to do so.
*Psychophysiologic insomnia*
- This condition involves heightened arousal and **anxiety surrounding sleep**, leading to difficulty falling asleep at night and often improved sleep in novel environments or away from home.
- While he expresses worry about not getting enough sleep, his sleep issues are primarily due to a shifted circadian phase, not just anxiety about sleep itself, and he sleeps restfully when allowed to follow his delayed rhythm.
*Advanced sleep-wake disorder*
- This disorder is characterized by a **habitually early sleep onset** and **early morning awakening**, typically several hours earlier than desired or conventional times.
- The patient, in contrast, consistently struggles to fall asleep until very late hours and desires a later wake time.
Circadian rhythm sleep-wake disorders US Medical PG Question 9: A first time mother of a healthy, full term, newborn girl is anxious about sudden infant death syndrome. Which of the following pieces of advice can reduce the risk of SIDS?
- A. Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in a warm blanket
- B. Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in an infant sleeper
- C. Sleep supine in the parent's bed and use a pacifier after 1 month of age
- D. Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and use a home apnea monitor
- E. Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and avoid smoking (Correct Answer)
Circadian rhythm sleep-wake disorders Explanation: ***Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and avoiding smoking***
- **Sleeping supine** (on the back) is the most critical recommendation to reduce SIDS risk, and a **crib without bumpers** and other soft bedding reduces smothering hazards.
- **Pacifier use** after the first month of age has been shown to be protective, and **avoiding smoking** around the infant is crucial as exposure to tobacco smoke significantly increases SIDS risk.
*Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in a warm blanket*
- While **sleeping supine** is correct, **bumpers, pillows, and loose blankets** in the crib are significant risk factors for SIDS, as they can cause accidental suffocation.
- The use of **pillows** is not recommended for infants due to the risk of airway obstruction and suffocation.
*Sleep supine in a crib with bumpers, head propped up on a pillow, and wrapped in an infant sleeper*
- Similar to the previous option, **bumpers and a pillow** are unsafe as they pose a suffocation risk and should be avoided in an infant's sleep environment.
- While an **infant sleeper** (or sleep sack) is generally safer than a loose blanket, the presence of bumpers and a pillow negates this benefit.
*Sleep supine in the parent's bed and use a pacifier after 1 month of age*
- **Co-sleeping (sharing a bed with parents)** significantly increases the risk of SIDS and accidental suffocation, especially if parents smoke, are impaired, or if heavy bedding is present.
- Although **pacifier use** is recommended, sleeping in the parent's bed is a major risk factor that outweighs any potential benefit here.
*Sleep supine in a crib without bumpers, use a pacifier after 1 month of age, and use a home apnea monitor*
- While **sleeping supine** in a **crib without bumpers** and **pacifier use** are correct recommendations, **home apnea monitors** are not recommended for routine SIDS prevention in healthy infants.
- Apnea monitors have not been shown to reduce the incidence of SIDS and can lead to false alarms and unnecessary anxiety without proven benefit.
Circadian rhythm sleep-wake disorders US Medical PG Question 10: A 31-year-old woman presents to your office with one week of recurrent fevers. The highest temperature she recorded was 101°F (38.3°C). She recently returned from a trip to Nigeria to visit family and recalls a painful bite on her right forearm at that time. Her medical history is significant for two malarial infections as a child. She is not taking any medications. On physical examination, her temperature is 102.2°F (39°C), blood pressure is 122/80 mmHg, pulse is 80/min, respirations are 18/min, and pulse oximetry is 99% on room air. She has bilateral cervical lymphadenopathy and a visible, enlarged, mobile posterior cervical node. Cardiopulmonary and abdominal examinations are unremarkable. She has an erythematous induration on her right forearm. The most likely cause of this patient's symptoms can be treated with which of the following medications?
- A. Sulfadiazine and pyrimethamine
- B. Atovaquone and azithromycin
- C. Primaquine
- D. Chloroquine
- E. Fexinidazole (Correct Answer)
Circadian rhythm sleep-wake disorders Explanation: ***Fexinidazole***
- This patient's symptoms (recurrent fevers, cervical lymphadenopathy, erythematous induration after a trip to Nigeria with a painful bite) are highly suggestive of **African trypanosomiasis (sleeping sickness)**.
- **Fexinidazole** is an oral nitroimidazole derivative approved for treating both first and second-stage human African trypanosomiasis (HAT) caused by *Trypanosoma brucei gambiense*.
*Sulfadiazine and pyrimethamine*
- This combination is primarily used to treat **toxoplasmosis**, an infection caused by the parasite *Toxoplasma gondii*.
- While it can cause fever and lymphadenopathy, the travel history to Nigeria and a "painful bite" are not typical for toxoplasmosis transmission.
*Atovaquone and azithromycin*
- This combination is utilized for treating **Babesiosis**, a tick-borne parasitic infection.
- While Babesiosis can cause fever and fatigue, the characteristic erythematous induration and prominent lymphadenopathy point away from this diagnosis.
*Primaquine*
- **Primaquine** is an antimalarial drug specifically used for the **radical cure of *Plasmodium vivax*** and ***Plasmodium ovale*** malaria, targeting the hypnozoite liver stages.
- Although the patient has a history of malaria and a travel history to an endemic area, the current presentation with distinct lymphadenopathy and skin lesion points away from a straightforward malarial relapse or new infection primarily requiring primaquine as the sole treatment.
*Chloroquine*
- **Chloroquine** is an antimalarial drug, but its use is limited primarily to areas where **chloroquine-sensitive *Plasmodium falciparum*** strains are prevalent.
- While the patient traveled to Nigeria, a region where malaria is endemic, the specific constellation of symptoms, including the bite and lymphadenopathy, is less characteristic of typical malaria than of trypanosomiasis.
More Circadian rhythm sleep-wake disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.