Second-generation antipsychotics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Second-generation antipsychotics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Second-generation antipsychotics US Medical PG Question 1: A 22-year-old male with a history of difficult-to-treat bipolar disorder with psychotic features is undergoing a medication adjustment under the guidance of his psychiatrist. The patient was previously treated with lithium and is transitioning to clozapine. Which of the following tests will the patient need routinely?
- A. Thyroid-stimulating hormone, prior to introducing the medication
- B. Basic metabolic panel, weekly
- C. Hemoglobin A1c, weekly
- D. Dexamethasone suppression test, monthly
- E. Complete blood count, weekly (Correct Answer)
Second-generation antipsychotics Explanation: ***Complete blood count, weekly***
- **Clozapine** can cause **agranulocytosis** (a severe drop in white blood cell count), which is a potentially life-threatening side effect.
- Due to this risk, initial treatment with clozapine requires **weekly complete blood count (CBC)** monitoring to detect early signs of agranulocytosis.
*Thyroid-stimulating hormone, prior to introducing the medication*
- While initial thyroid function tests might be considered in the workup for bipolar disorder, routine and specific monitoring of **TSH** is not a primary requirement for **clozapine** initiation.
- **Lithium**, not clozapine, is more directly associated with thyroid dysfunction, so monitoring would be more relevant to the patient's previous medication.
*Basic metabolic panel, weekly*
- A **basic metabolic panel (BMP)** assesses **electrolyte levels**, **kidney function**, and **glucose**, which can be affected by various psychotropic medications.
- While important for overall health monitoring, a **weekly BMP** is not specifically mandated for **clozapine** due to the specific and severe risk of agranulocytosis.
*Hemoglobin A1c, weekly*
- **Clozapine** is associated with a risk of **metabolic side effects**, including **weight gain**, **dyslipidemia**, and **new-onset diabetes**.
- While **HbA1c** is used to monitor long-term glycemic control, it's typically checked less frequently (e.g., quarterly or annually) for metabolic monitoring, not weekly, and is not the primary immediate safety concern for clozapine.
*Dexamethasone suppression test, monthly*
- The **dexamethasone suppression test (DST)** is used to assess **adrenal gland function** and can be relevant in certain psychiatric conditions like **depression with melancholic features** or to rule out **Cushing's syndrome**.
- It is **not a routine monitoring test** for patients starting or on **clozapine** therapy.
Second-generation antipsychotics US Medical PG Question 2: A 35-year-old woman comes to the physician accompanied by her husband after he started noticing strange behavior. He first noticed her talking to herself 8 months ago. For the past 6 months, she has refused to eat any packaged foods out of fear that the government is trying to poison her. She has no significant past medical history. She smoked marijuana in college but has not smoked any since. She appears restless. Mental status examination shows a flat affect. Her speech is clear, but her thought process is disorganized with many loose associations. The patient is diagnosed with schizophrenia and started on olanzapine. This patient is most likely to experience which of the following adverse effects?
- A. Dyslipidemia (Correct Answer)
- B. Diabetes insipidus
- C. Agranulocytosis
- D. Myoglobinuria
- E. Seizures
Second-generation antipsychotics Explanation: ***Dyslipidemia***
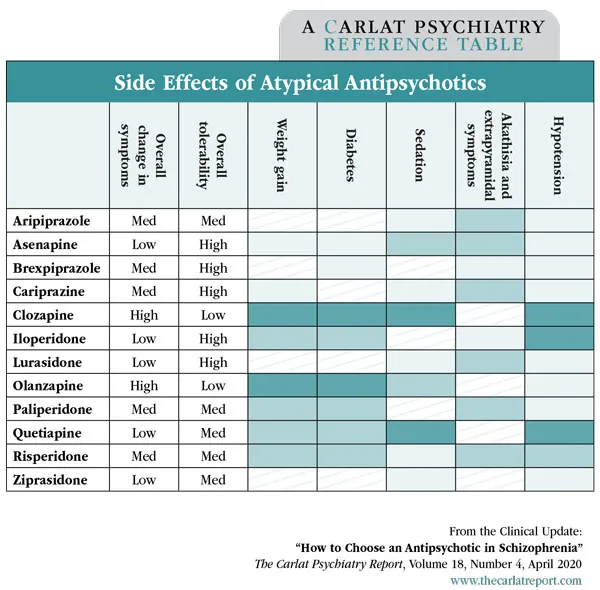
- **Olanzapine** is a **second-generation antipsychotic** commonly associated with significant **metabolic side effects**, including **weight gain**, **dyslipidemia**, and **insulin resistance**.
- These metabolic disturbances increase the risk of cardiovascular disease.
*Diabetes insipidus*
- This is a rare side effect, not typically associated with **olanzapine** or other **second-generation antipsychotics**.
- **Lithium** is an antimanic agent that can cause **nephrogenic diabetes insipidus**, but it is not relevant here.
*Agranulocytosis*
- While a serious side effect of some antipsychotics, **agranulocytosis** is most notably associated with **clozapine**,
- **Olanzapine** has a much lower risk of causing **agranulocytosis** compared to clozapine.
*Myoglobinuria*
- **Myoglobinuria** is associated with conditions like significant muscle damage (e.g., rhabdomyolysis).
- It is not a direct or common adverse effect of **olanzapine** therapy.
*Seizures*
- While some antipsychotics can lower the **seizure threshold**, **olanzapine** generally has a relatively low risk of inducing seizures.
- The risk is higher with certain other antipsychotics, particularly at high doses, or in patients with pre-existing seizure disorders.
Second-generation antipsychotics US Medical PG Question 3: A 31-year-old woman is brought to the physician because of increasing restlessness over the past 2 weeks. She reports that she continuously paces around the house and is unable to sit still for more than 10 minutes at a time. During this period, she has had multiple episodes of anxiety with chest tightness and shortness of breath. She was diagnosed with a psychotic illness 2 months ago. Her current medications include haloperidol and a multivitamin. She appears agitated. Vital signs are within normal limits. Physical examination shows no abnormalities. The examination was interrupted multiple times when she became restless and began to walk around the room. To reduce the likelihood of the patient developing her current symptoms, a drug with which of the following mechanisms of action should have been prescribed instead of her current medication?
- A. H2 receptor antagonism
- B. 5-HT2A receptor antagonism (Correct Answer)
- C. α2 receptor antagonism
- D. NMDA receptor antagonism
- E. GABA receptor antagonism
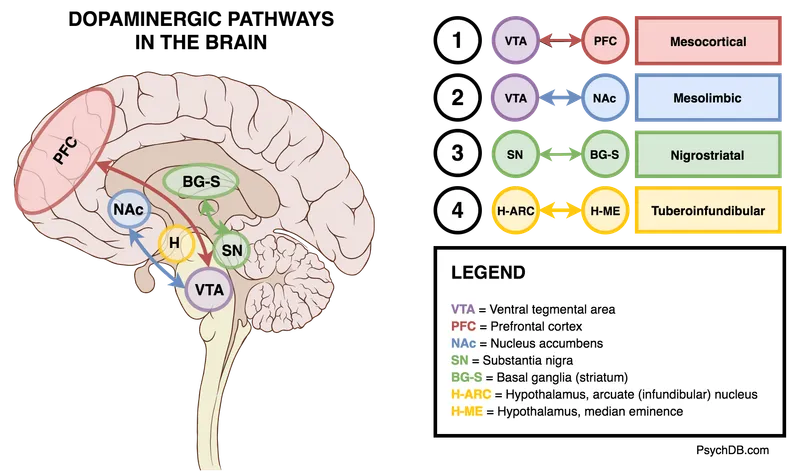
Second-generation antipsychotics Explanation: ***5-HT2A receptor antagonism***
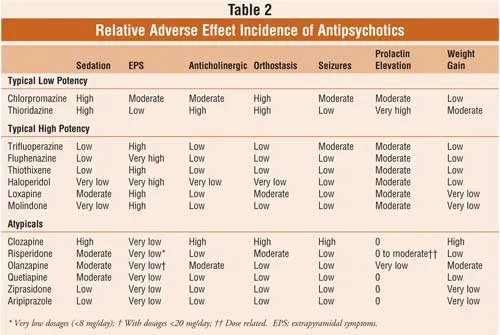
- The patient is experiencing **akathisia**, a common extrapyramidal side effect of **typical antipsychotics** like haloperidol, characterized by subjective or objective motor restlessness.
- Atypical antipsychotics, which exert their antipsychotic effects primarily through **5-HT2A receptor antagonism** along with D2 receptor antagonism, have a lower propensity to cause extrapyramidal symptoms, including akathisia, compared to typical antipsychotics.
*H2 receptor antagonism*
- **H2 receptor antagonists** are primarily used to reduce gastric acid secretion in conditions like peptic ulcer disease and GERD.
- They have no direct role in treating psychosis or preventing extrapyramidal side effects.
*α2 receptor antagonism*
- **Alpha-2 receptor antagonists** (e.g., mirtazapine) are typically used as antidepressants; their mechanism involves increasing norepinephrine and serotonin release.
- This mechanism is not directly therapeutic for psychosis and would not prevent akathisia caused by D2 receptor blockade.
*NMDA receptor antagonism*
- **NMDA receptor antagonists** (e.g., ketamine, memantine) are studied for various neurological and psychiatric conditions, but their primary use is not in typical psychosis treatment, nor do they prevent akathisia from antipsychotics.
- Instead, NMDA receptor hypofunction is hypothesized in schizophrenia, and antagonism could potentially worsen psychotic symptoms.
*GABA receptor antagonism*
- **GABA receptor antagonists** (e.g., flumazenil) block the effects of inhibitory neurotransmitter GABA and can cause seizures and increased anxiety, which would be detrimental in a patient with psychosis and anxiety.
- Medications that *enhance* GABAergic transmission (e.g., benzodiazepines) are sometimes used to treat acute akathisia or anxiety, but long-term antagonism would be contra-indicated.
Second-generation antipsychotics US Medical PG Question 4: A 34-year-old male presents to clinic today complaining that his medication has stopped working. He states despite being able to manage the side effects, a voice has returned again telling him to hurt his Mother. You prescribe him a drug which has shown improved efficacy in treating his disorder but requires frequent followup visits. One week later he returns with the following lab results: WBC : 2500 cells/mcL, Neutrophils : 55% and, Bands : 1%. What drug was this patient prescribed?
- A. Clozapine (Correct Answer)
- B. Lurasidone
- C. Olanzapine
- D. Chlorpromazine
- E. Haloperidol
Second-generation antipsychotics Explanation: ***Clozapine***
- **Clozapine** is an atypical antipsychotic known for its superior efficacy in **treatment-resistant schizophrenia**, which fits the patient's presentation of a recurrence of symptoms despite prior medication.
- The given lab results (WBC 2500 cells/mcL, Neutrophils 55%, Bands 1%) show signs of **neutropenia**, a severe side effect of clozapine that necessitates frequent monitoring of complete blood counts (CBCs).
*Lurasidone*
- **Lurasidone** is an atypical antipsychotic, but it is not typically considered a first-line treatment for treatment-resistant cases and does not carry the same risk of agranulocytosis requiring frequent CBC monitoring as clozapine.
- It would not explain the **observed neutropenia** and the need for frequent follow-up for blood work.
*Olanzapine*
- While **olanzapine** is an effective atypical antipsychotic, it is not uniquely indicated for treatment-resistant cases in the same way clozapine is, nor does it typically require the intensive hematological monitoring.
- Its main severe side effects are metabolic (e.g., weight gain, dyslipidemia), not **neutropenia** that would manifest in these lab results.
*Chlorpromazine*
- **Chlorpromazine** is a first-generation antipsychotic and, while effective, is not known for superior efficacy in treatment-resistant cases compared to clozapine and has a different side effect profile.
- It can cause **agranulocytosis** but is not the drug of choice for treatment-resistant schizophrenia and its side effect profile does not align.
*Haloperidol*
- **Haloperidol** is a potent first-generation antipsychotic, effective for acute psychosis, but less effective for negative symptoms and carries a high risk of extrapyramidal side effects.
- It is not typically chosen for treatment-resistant cases and does not cause the specific hematological issues seen in the lab results that would necessitate weekly follow-up for blood counts.
Second-generation antipsychotics US Medical PG Question 5: A 24-year-old man with a history of schizophrenia presents for follow-up. The patient says that he is still having paranoia and visual hallucinations on his latest atypical antipsychotic medication. Past medical history is significant for schizophrenia diagnosed 1 year ago that failed to be adequately controlled on 2 separate atypical antipsychotic medications. The patient is switched to a typical antipsychotic medication. Which of the following is the mechanism of action of the medication that was most likely prescribed for this patient?
- A. Dopaminergic receptor antagonist (Correct Answer)
- B. Dopaminergic partial agonist
- C. Serotonergic receptor agonist
- D. Serotonergic receptor antagonist
- E. Cholinergic receptor agonist
Second-generation antipsychotics Explanation: ***Dopaminergic receptor antagonist***
- The patient has **treatment-resistant schizophrenia**, indicated by failure to respond to two different atypical antipsychotics.
- Typical antipsychotics like **haloperidol** or **fluphenazine** are primarily **D2 dopamine receptor antagonists**, which may be used when a patient has not responded to atypical agents.
- The **primary mechanism** of typical (first-generation) antipsychotics is **potent D2 receptor blockade** in the mesolimbic pathway, which reduces positive symptoms of schizophrenia.
- Note: Clozapine would be the preferred choice for true treatment-resistant schizophrenia, but typical antipsychotics may still be considered in some clinical scenarios.
*Dopaminergic partial agonist*
- **Dopamine partial agonists**, such as **aripiprazole** or **brexpiprazole**, are **atypical antipsychotics** used for schizophrenia.
- The patient has failed to respond to atypical antipsychotics already, making it unlikely that another atypical agent would be the next choice.
- The question specifically states the patient is switched to a **typical antipsychotic**.
*Serotonergic receptor agonist*
- **Serotonin receptor agonists**, like LSD or psilocybin, are **not used** in the treatment of schizophrenia; they can, in fact, **induce psychotic symptoms**.
- While some antipsychotics modulate serotonin receptors, their therapeutic effect is not through agonism of these receptors.
*Serotonergic receptor antagonist*
- Many **atypical antipsychotics** have significant **serotonin 5-HT2A receptor antagonist** activity, in addition to D2 antagonism.
- However, the question states that the patient is being switched to a **typical antipsychotic**, whose primary and defining mechanism is **D2 antagonism**, not combined serotonin-dopamine antagonism.
*Cholinergic receptor agonist*
- **Cholinergic receptor agonists** are **not used** to treat schizophrenia and would likely worsen symptoms or cause significant side effects.
- These agents would have no therapeutic benefit in psychosis and are not part of the antipsychotic drug class.
Second-generation antipsychotics US Medical PG Question 6: A 44-year-old man presents to his psychiatrist for a follow-up appointment. He is currently being treated for schizophrenia. He states that he is doing well but has experienced some odd movement of his face recently. The patient's sister is with him and states that he has been more reclusive lately and holding what seems to be conversations despite nobody being in his room with him. She has not noticed improvement in his symptoms despite changes in his medications that the psychiatrist has made at the last 3 appointments. His temperature is 99.3°F (37.4°C), blood pressure is 157/88 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for rhythmic movements of the patient's mouth and tongue. Which of the following is a side effect of the next best step in management?
- A. Anxiolysis
- B. Dry mouth and dry eyes
- C. QT prolongation on EKG
- D. Infection (Correct Answer)
- E. Worsening of psychotic symptoms
Second-generation antipsychotics Explanation: ***Infection***
- The patient has **tardive dyskinesia** and **persistent psychotic symptoms** despite changes in medications. The next best step is to switch to **clozapine**.
- **Clozapine** can cause **agranulocytosis**, which increases the risk of serious infections and requires regular monitoring of white blood cell counts.
*Anxiolysis*
- While some antipsychotics can have anxiolytic effects, it is not the primary side effect or the most concerning one for the "next best step" in this context.
- The patient's primary issues are persistent psychosis and tardive dyskinesia, not anxiety that would be specifically targeted as the main side effect.
*Dry mouth and dry eyes*
- These are common **anticholinergic side effects** associated with many antipsychotics, including clozapine, but they are generally less severe and life-threatening compared to the risk of agranulocytosis.
- While unpleasant, they are not the most significant or defining side effect of the "next best step" in managing this patient's complex presentation.
*QT prolongation on EKG*
- **QT prolongation** is a known cardiac side effect of several antipsychotics, including clozapine.
- However, the risk of **agranulocytosis** with **clozapine** is arguably the most critical and distinct side effect requiring stringent monitoring, making it the "next best step" related answer.
*Worsening of psychotic symptoms*
- The "next best step" would be directed at *improving* psychotic symptoms, not worsening them. **Clozapine** is specifically indicated for **treatment-resistant schizophrenia**.
- Worsening psychosis would indicate treatment failure or an adverse reaction, not a typical side effect of the intended beneficial action.
Second-generation antipsychotics US Medical PG Question 7: A 56-year-old man presents with constipation and trouble urinating for the past day. He says that he tried drinking a lot of water but that did not help. He also says that he has been tired all the time recently. Past medical history is significant for schizophrenia, diagnosed 3 months ago, and being managed on chlorpromazine. Current medications also include sildenafil. The vital signs include blood pressure 80/45 mm Hg, respiratory rate 23/min, heart rate 86/min and temperature 38.7°C (101.7°F). On physical examination, the patient appears agitated and confused. Which of the following medications is the most likely cause of this patient's presentation?
- A. Chlorpromazine (Correct Answer)
- B. Ziprasidone
- C. Haloperidol
- D. Aripiprazole
- E. Lithium
Second-generation antipsychotics Explanation: ***Chlorpromazine***
- The patient's presentation with **constipation**, **trouble urinating**, **fever**, **tachycardia**, **hypotension**, **agitation**, and **confusion** is highly suggestive of **anticholinergic toxicity**.
- **Chlorpromazine**, a low-potency first-generation antipsychotic, has significant **anticholinergic side effects** due to its potent blockade of muscarinic receptors, making it the most likely cause.
*Ziprasidone*
- Ziprasidone is a **second-generation antipsychotic** known for a lower propensity for anticholinergic side effects compared to first-generation agents like chlorpromazine.
- While it can cause side effects, severe anticholinergic toxicity is less common and less pronounced with ziprasidone.
*Haloperidol*
- Haloperidol is a **high-potency first-generation antipsychotic** with relatively weak anticholinergic properties compared to chlorpromazine.
- It is more commonly associated with **extrapyramidal symptoms** rather than the severe anticholinergic syndrome described.
*Aripiprazole*
- Aripiprazole is a **second-generation antipsychotic** with **dopamine partial agonist** properties and very low anticholinergic activity.
- It would be an unlikely cause of the profound anticholinergic toxicity observed in this patient.
*Lithium*
- Lithium is a **mood stabilizer** used in bipolar disorder and does not possess significant anticholinergic properties.
- Lithium toxicity typically presents with **tremor**, **nausea**, **vomiting**, **diarrhea**, and **neurological symptoms** like ataxia, rather than the specific constellation of anticholinergic symptoms seen here.
Second-generation antipsychotics US Medical PG Question 8: A 36-year-old woman with schizophrenia comes to the office for a follow-up appointment. She has been hospitalized 4 times in the past year, and she has failed to respond to multiple trials of antipsychotic medications. Six weeks ago, she was brought to the emergency department by her husband because of a bizarre behavior, paranoid delusions, and hearing voices that others did not hear. She was started on a new medication, and her symptoms have improved. Laboratory studies show:
Hemoglobin 13.8 g/dL
Leukocyte count 1,200/mm3
Segmented neutrophils 6%
Eosinophils 0%
Lymphocytes 92%
Monocytes 2%
Platelet count 245,000/mm3
This patient was most likely started on which of the following medications?
- A. Clozapine (Correct Answer)
- B. Promethazine
- C. Fluphenazine
- D. Lithium
- E. Quetiapine
Second-generation antipsychotics Explanation: ***Clozapine***
- The patient's presentation of **treatment-resistant schizophrenia** (failure to respond to multiple antipsychotics and recurrent hospitalizations) strongly points to clozapine as the most likely effective treatment.
- The abnormal lab results, particularly **leukopenia** (total WBC 1,200/mm³) and severe **neutropenia** (segmented neutrophils 6%, absolute neutrophil count ~72/mm³), are a known and serious side effect of clozapine, requiring careful monitoring.
*Promethazine*
- Promethazine is an **antihistamine** with antiemetic and sedative properties, not a primary antipsychotic for schizophrenia.
- It would not be used for chronic management of severe, treatment-resistant schizophrenia and is not associated with the severe hematological side effects seen here.
*Fluphenazine*
- Fluphenazine is a **first-generation antipsychotic** that could be used for schizophrenia, but the patient's history indicates failure of multiple antipsychotic trials.
- While it can cause some side effects, severe leukopenia and neutropenia to the degree seen here are not characteristic of fluphenazine.
*Lithium*
- Lithium is a **mood stabilizer** primarily used for bipolar disorder, not typical first-line or even second-line treatment for schizophrenia as a monotherapy.
- Notably, lithium typically causes **leukocytosis** (increased WBC count), not leukopenia, making it inconsistent with the lab findings showing severe leukopenia and neutropenia.
*Quetiapine*
- Quetiapine is a **second-generation antipsychotic** that is used for schizophrenia, but it is less effective for treatment-resistant cases compared to clozapine.
- While some antipsychotics can cause mild hematologic changes, quetiapine is not known for causing the profound leukopenia and severe neutropenia seen in this patient, which are distinctly associated with clozapine.
Second-generation antipsychotics US Medical PG Question 9: A 30-year-old man comes to the emergency department because of fever and productive cough for the past 4 days. During this period, he has had shortness of breath and chest pain that is worse on inspiration. He also reports fatigue and nausea. He has refractory schizophrenia and recurrent asthma attacks. He used to attend college but was expelled after threatening to harm one of his professors 2 months ago. His temperature is 38.5°C (101.3°F), pulse is 90/min, respirations are 20/min, and blood pressure is 120/80 mm Hg. Crackles and bronchial breath sounds are heard on auscultation of the left lung. Laboratory studies show:
Hemoglobin 13.5 g/dL
Leukocyte count 1,100/mm3
Segmented neutrophils 5%
Eosinophils 0%
Lymphocytes 93%
Monocytes 2%
Platelet count 260,000/mm3
Which of the following medications is this patient most likely taking?
- A. Chlorpromazine
- B. Risperidone
- C. Haloperidol
- D. Olanzapine
- E. Clozapine (Correct Answer)
Second-generation antipsychotics Explanation: ***Clozapine***
- The patient exhibits severe **agranulocytosis** (WBC count 1,100/mm³ with 5% neutrophils, indicating an absolute neutrophil count of 55/mm³), a life-threatening side effect uniquely associated with **clozapine** among antipsychotics.
- Given his history of **refractory schizophrenia** (implying resistance to other antipsychotics), clozapine is the most likely antipsychotic he would be prescribed.
*Chlorpromazine*
- This first-generation antipsychotic can cause adverse effects like **sedation, orthostatic hypotension, and anticholinergic symptoms**, but severe agranulocytosis is rare.
- While it can cause leukopenia, the profound agranulocytosis seen in the patient is not characteristic of chlorpromazine.
*Risperidone*
- Atypical antipsychotic known for side effects such as **hyperprolactinemia, weight gain, and metabolic syndrome**.
- Though it can cause neutropenia or leukopenia, it rarely causes the severe agranulocytosis observed here.
*Haloperidol*
- A high-potency first-generation antipsychotic primarily associated with **extrapyramidal symptoms (EPS)** and **neuroleptic malignant syndrome (NMS)**.
- It does not typically cause the severe bone marrow suppression, specifically agranulocytosis, observed in this patient.
*Olanzapine*
- This atypical antipsychotic is associated with significant **weight gain, sedation, and metabolic syndrome**.
- While it can cause some hematologic abnormalities, it is not known to cause severe agranulocytosis to the same extent as clozapine.
Second-generation antipsychotics US Medical PG Question 10: A 24-year-old man and his mother arrive for a psychiatric evaluation. She is concerned about his health and behavior ever since he dropped out of graduate school and moved back home 8 months ago. He is always very anxious and preoccupied with thoughts of school and getting a job. He also seems to behave very oddly at times such as wearing his winter jacket in summer. He says that he hears voices but he can not understand what they are saying. When prompted he describes a plot to have him killed with poison seeping from the walls. Today, his heart rate is 90/min, respiratory rate is 17/min, blood pressure is 110/65 mm Hg, and temperature is 36.8°C (98.2°F). On physical exam, he appears gaunt and anxious. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. CMP, CBC, and TSH are normal. A urine toxicology test is negative. What is the most likely diagnosis?
- A. Schizophrenia (Correct Answer)
- B. Substance-induced psychosis
- C. Schizophreniform disorder
- D. Schizoaffective disorder
- E. Brief psychotic disorder
Second-generation antipsychotics Explanation: ***Schizophrenia***
- The patient presents with **delusions** ("plot to have him killed"), **hallucinations** ("hears voices"), **disorganized thinking** (preoccupied with school and job but no progress made, wearing winter jacket in summer can be a sign of disorganized behavior), and **negative symptoms** (appears gaunt and anxious, social withdrawal, drop out of school). These symptoms have been present since he dropped out of graduate school 8 months ago, indicating a **duration of at least 6 months**.
- The combination of these symptoms persisting for over 6 months, impacting his functioning, and absence of other medical or substance-related causes, is diagnostic of **schizophrenia**.
*Substance-induced psychosis*
- The **urine toxicology test is negative**, ruling out recent substance use as the cause of his psychotic symptoms.
- The **chronicity** of symptoms (8 months) is less typical for acute substance-induced psychosis, which generally resolves more quickly after the substance is cleared.
*Schizophreniform disorder*
- Schizophreniform disorder involves the same symptoms as schizophrenia but with a **duration of at least 1 month but less than 6 months**.
- The patient's symptoms have been present for **8 months**, exceeding the criteria for schizophreniform disorder.
*Schizoaffective disorder*
- Schizoaffective disorder requires the presence of a **major mood episode** (depressive or manic) concurrent with criteria A of schizophrenia. Additionally, **delusions or hallucinations for at least 2 weeks** must occur in the absence of a major mood episode at some point during the illness.
- While the patient appears anxious, there is **no clear evidence of a persistent major depressive or manic episode** that would qualify for schizoaffective disorder.
*Brief psychotic disorder*
- Brief psychotic disorder is characterized by psychotic symptoms lasting **more than 1 day but less than 1 month**.
- The patient's symptoms have been ongoing for **8 months**, far exceeding the duration for brief psychotic disorder.
More Second-generation antipsychotics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.