Prodromal phase and early intervention US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Prodromal phase and early intervention. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Prodromal phase and early intervention US Medical PG Question 1: A 26-year-old woman is brought to the emergency department by her husband due to her disturbing behavior over the past 24 hours. Her husband says that he has noticed his wife talking to herself and staying in a corner of a room throughout the day without eating or drinking anything. She gave birth to their son 2 weeks ago but has not seen or even acknowledged her baby’s presence ever since he was born. He says that he didn’t think much of it because she seemed overwhelmed during her pregnancy and he considered that she was probably unable to cope with being a new mother; however, last night, he says, his wife told him that their child was the son of the devil and they ought to get rid of him as soon as possible. Which of the following describes this patient’s abnormal reaction to her child?
- A. Brief psychotic disorder
- B. Schizoaffective disorder
- C. Postpartum psychosis (Correct Answer)
- D. Major depressive disorder
- E. Postpartum blues
Prodromal phase and early intervention Explanation: **Postpartum psychosis**
- This patient exhibits **psychotic symptoms** (delusions about the child, hallucinations like talking to herself) and **severe disorganization** (staying in a corner, not eating/drinking, neglecting her baby) within two weeks postpartum.
- This severe and acute onset of psychosis in the **postpartum period** is characteristic of postpartum psychosis, which is a medical emergency requiring immediate intervention.
*Brief psychotic disorder*
- While it involves psychotic symptoms of acute onset and short duration (less than one month), this diagnosis typically applies when symptoms are not directly attributable to a specific precipitating factor like childbirth.
- The clear temporal association with childbirth in this case makes postpartum psychosis a more specific and accurate diagnosis.
*Schizoaffective disorder*
- This disorder typically involves a combination of **mood symptoms** (depressive or manic) and **psychotic symptoms**, where psychotic symptoms are present for at least two weeks in the absence of a major mood episode.
- The sudden onset and direct link to the postpartum period distinguish this case from schizoaffective disorder, which usually has a more chronic or episodic course.
*Major depressive disorder*
- Although the patient shows signs of severe withdrawal and neglect, the presence of **frank psychotic symptoms** (delusions about the child being the "son of the devil") goes beyond the typical presentation of major depressive disorder, even with psychotic features.
- While depression can coexist, the predominant and acute psychotic features point more directly to postpartum psychosis.
*Postpartum blues*
- Postpartum blues are **mild and transient mood disturbances** (tearfulness, irritability, anxiety) occurring in the first few days to two weeks postpartum, typically resolving on their own.
- The patient's symptoms are far more severe, involving **psychotic delusions and severe functional impairment**, making postpartum blues an inadequate diagnosis.
Prodromal phase and early intervention US Medical PG Question 2: An 18-year-old man is brought to the emergency department after his mother found him locked in his room stammering about a government conspiracy to brainwash him in subterranean tunnels. His mother says that he has never done this before, but 6 months ago he stopped going to classes and was subsequently suspended from college. She reports that he has become increasingly taciturn over the course of the past month. He drinks one to two beers daily and has smoked one pack of cigarettes daily for 3 years. He occasionally smokes marijuana. His father was diagnosed with schizophrenia at the age of 25 years. The patient has had no friends or social contacts other than his mother since he was suspended. He appears unkempt and aloof. On mental status examination, he is disorganized and shows poverty of speech. He says his mood is "good." He does not hear voices and has no visual or tactile hallucinations. Toxicology screening is negative. Which of the following is an unfavorable prognostic factor for this patient's condition?
- A. Poor premorbid functioning (Correct Answer)
- B. Late onset of illness
- C. Presence of mood symptoms
- D. Good insight into illness
- E. Strong family support
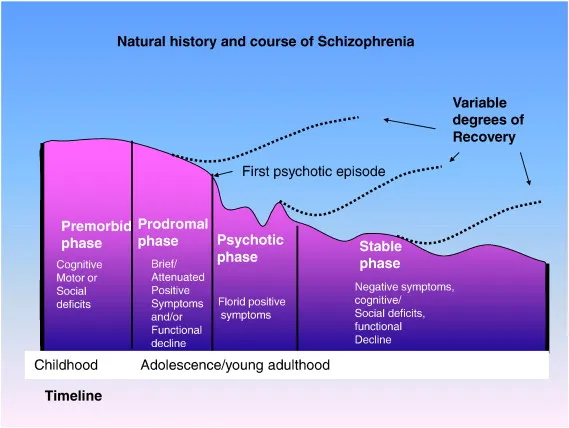
Prodromal phase and early intervention Explanation: ***Poor premorbid functioning***
- **Poor premorbid functioning** is a well-established **unfavorable prognostic factor** in schizophrenia, associated with worse long-term outcomes and functional recovery.
- This patient demonstrates poor premorbid functioning: he declined from being a college student to being suspended, became increasingly isolated with no friends or social contacts, and presents as unkempt and aloof.
- The insidious deterioration over 6 months with prominent negative symptoms (taciturnity, poverty of speech, social withdrawal) further suggests poor premorbid adjustment.
*Late onset of illness*
- **Late onset** (after age 25-30) is associated with a **better prognosis** because brain development is more complete and there is typically better premorbid functioning.
- This is a **favorable**, not unfavorable, prognostic factor.
*Presence of mood symptoms*
- The presence of **prominent mood symptoms** (depression, mania) in psychotic disorders is associated with a **better prognosis** than pure schizophrenia.
- Schizoaffective disorder generally has better outcomes than schizophrenia.
- This is a **favorable** prognostic factor.
*Good insight into illness*
- **Good insight** is a highly **favorable prognostic factor** as it increases treatment adherence and engagement in recovery.
- This patient lacks insight, demonstrating disorganized thought and delusions without awareness of illness.
*Strong family support*
- **Strong family support** is a crucial **favorable prognostic factor**, improving treatment adherence, recovery, and social reintegration.
- While the mother is involved, the patient's complete social isolation (no friends or contacts besides mother) suggests limited overall support network.
Prodromal phase and early intervention US Medical PG Question 3: A mental health volunteer is interviewing locals as part of a community outreach program. A 46-year-old man discloses that he has felt sad for as long as he can remember. He feels as though his life is cursed and if something terrible can happen to him, it usually will. He has difficulty making decisions and feels hopeless. He also feels that he has had worsening suicidal ideations, guilt from past problems, decreased energy, and poor concentration over the past 2 weeks. He is otherwise getting enough sleep and able to hold a job. Which of the following statement best describes this patient's condition?
- A. The patient may have symptoms of mania or psychosis.
- B. The patient is likely to show anhedonia.
- C. The patient likely has paranoid personality disorder.
- D. The patient has double depression. (Correct Answer)
- E. The patient should be started on an SSRI.
Prodromal phase and early intervention Explanation: ***The patient has double depression.***
- The patient describes **chronic low-grade depressive symptoms** ("felt sad for as long as he can remember," "life is cursed," "difficulty making decisions," "hopeless") consistent with **persistent depressive disorder (dysthymia)**, which requires at least 2 years of symptoms.
- The recent worsening of symptoms over the past two weeks, including "worsening suicidal ideations, guilt from past problems, decreased energy, and poor concentration," indicates an additional **major depressive episode (MDE) superimposed on dysthymia**, a condition known as **double depression**.
- This patient currently meets criteria for both conditions simultaneously, not just at risk for developing them.
*The patient may have symptoms of mania or psychosis.*
- There are no symptoms mentioned that suggest **mania**, such as elevated mood, increased energy, decreased need for sleep, grandiosity, or racing thoughts.
- While suicidal ideation is present, there is no evidence of **psychotic features** like hallucinations or delusions.
*The patient is likely to show anhedonia.*
- **Anhedonia** (inability to feel pleasure) is a common symptom of depression and may well be present in this patient.
- However, the patient's presentation specifically highlights the pattern of **chronic dysthymia with a superimposed major depressive episode**, making **double depression** a more precise, comprehensive, and diagnostically specific description of his current condition.
- While anhedonia might be present, it is a symptom rather than a diagnostic formulation.
*The patient likely has paranoid personality disorder.*
- **Paranoid personality disorder** is characterized by pervasive distrust and suspicion of others, interpreting their motives as malevolent, without sufficient basis.
- The patient's feelings of being "cursed" and that "something terrible can happen" reflect **depressive pessimism and negative cognitive distortions**, not paranoid ideation about others' intentions.
- This is consistent with the hopelessness seen in depression.
*The patient should be started on an SSRI.*
- While an **SSRI (selective serotonin reuptake inhibitor)** combined with psychotherapy would likely be appropriate treatment for double depression, making a specific treatment recommendation is premature without comprehensive clinical assessment.
- The question asks for the **best statement describing the patient's condition** (diagnosis), not for treatment recommendations.
Prodromal phase and early intervention US Medical PG Question 4: A 24-year-old man is brought to your emergency department under arrest by the local police. The patient was found naked at a busy intersection jumping up and down on top of a car. Interviewing the patient, you discover that he has not slept in 2 days because he does not feel tired. He reports hearing voices. The patient was previously hospitalized 1 year ago with auditory hallucinations, paranoia, and a normal mood. What is the most likely diagnosis?
- A. Schizophrenia
- B. Bipolar disorder
- C. Brief psychotic disorder
- D. Schizotypal disorder
- E. Schizoaffective disorder (Correct Answer)
Prodromal phase and early intervention Explanation: ***Schizoaffective disorder***
- This patient demonstrates the **hallmark feature** of schizoaffective disorder: **psychotic symptoms occurring both during AND independent of mood episodes**.
- **Current presentation**: Clear **manic episode** (decreased need for sleep, grandiose/disinhibited behavior, psychomotor agitation) with psychotic features (auditory hallucinations).
- **Previous hospitalization**: **Psychotic symptoms (hallucinations, paranoia) in the absence of a mood episode** ("normal mood"), requiring hospitalization for at least 2 weeks - this is the **key diagnostic criterion** for schizoaffective disorder.
- The diagnosis requires an **uninterrupted period of illness** with both psychotic symptoms (meeting Criterion A for schizophrenia) and a major mood episode, PLUS psychotic symptoms for **≥2 weeks without prominent mood symptoms**.
*Bipolar disorder*
- In bipolar disorder with psychotic features, psychotic symptoms occur **exclusively during mood episodes** (manic, hypomanic, or depressive).
- This patient's previous hospitalization with psychosis but **"normal mood"** indicates psychotic symptoms independent of mood episodes, which **rules out** bipolar disorder and points to schizoaffective disorder.
- While the current presentation shows mania with psychosis, the longitudinal course is critical for diagnosis.
*Schizophrenia*
- Schizophrenia involves **continuous psychotic symptoms** without prominent mood episodes dominating the clinical picture.
- This patient has **prominent manic symptoms** (decreased sleep, grandiose behavior, agitation) that are central to the current presentation, making schizophrenia less likely.
- The presence of full mood episodes that occupy a **substantial portion** of the illness duration favors schizoaffective disorder over schizophrenia.
*Brief psychotic disorder*
- Brief psychotic disorder involves psychotic symptoms lasting **<1 month** with full return to baseline functioning.
- This patient has a **recurrent course** with hospitalization 1 year ago, indicating a chronic/recurring condition rather than a brief, self-limited episode.
*Schizotypal disorder*
- This is a **personality disorder** characterized by social deficits, cognitive/perceptual distortions, and eccentric behavior, but **NOT overt psychotic episodes**.
- Does not involve acute psychotic breaks with severe symptoms like hallucinations requiring hospitalization or manic episodes.
Prodromal phase and early intervention US Medical PG Question 5: A 20-year-old student is referred to his college's student health department because his roommates are concerned about his recent behavior. He rarely leaves his room, has not showered in several days, appears to be praying constantly even though he is not religious, and has not been studying despite previously being an extremely good student. After evaluating this patient, a physician decides to recommend initiation of pharmacological treatment. The patient's family is concerned because they heard that the drug being recommended may be associated with heart problems. Which of the following characteristics is a property of the most likely drug that was prescribed in this case?
- A. May cause weight gain and metabolic changes
- B. Lower risk of extrapyramidal symptoms
- C. High affinity for serotonin 5-HT2A receptors
- D. Prolongs the QT interval (Correct Answer)
- E. Generally less sedating than older antipsychotics
Prodromal phase and early intervention Explanation: ***Prolongs the QT interval***
- The patient presents with **first-episode psychosis** (social withdrawal, poor hygiene, bizarre behavior, academic decline in a previously high-functioning young adult)
- The family's specific concern about **"heart problems"** is the key clue pointing to **QT interval prolongation**
- Among antipsychotics used for first-episode psychosis, **ziprasidone** is most notably associated with QT prolongation and carries an FDA warning about this cardiac effect
- While other antipsychotics may also prolong QT to varying degrees, ziprasidone's association with this adverse effect is well-established and would prompt specific family counseling about cardiac risks
- QT prolongation increases risk of **torsades de pointes**, a potentially fatal arrhythmia
*May cause weight gain and metabolic changes*
- **Weight gain and metabolic syndrome** (hyperglycemia, dyslipidemia) are common adverse effects of many **atypical antipsychotics**, particularly olanzapine and clozapine
- While these are serious long-term concerns, they would typically be described as "weight" or "diabetes" problems rather than acute "heart problems"
- This is not the distinguishing feature being emphasized by the family's concern
*Lower risk of extrapyramidal symptoms*
- **Lower EPS risk** is a characteristic feature of **atypical (second-generation) antipsychotics** compared to typical (first-generation) agents
- This is actually a therapeutic advantage and would not be a concern for the family
- This property applies to most atypical antipsychotics, not specifically to the one causing family concern about cardiac effects
*High affinity for serotonin 5-HT2A receptors*
- **5-HT2A receptor antagonism** is a defining pharmacological property of **atypical antipsychotics** that contributes to their lower EPS risk and efficacy for negative symptoms
- This mechanism applies broadly to the atypical antipsychotic class
- It does not explain the specific family concern about "heart problems"
*Generally less sedating than older antipsychotics*
- Sedation profiles vary widely among antipsychotics; some atypicals (quetiapine) are quite sedating while others (aripiprazole, ziprasidone) are less so
- Sedation is not typically characterized as a "heart problem"
- This does not address the cardiac safety concern highlighted in the question
Prodromal phase and early intervention US Medical PG Question 6: A 21-year-old man presents to the emergency room requesting surgery to remove "microchips," which he believes were implanted in his brain by "Russian spies" 6 months ago to control his thoughts. He also reports hearing the "spies" talk to each other through embedded "microspeakers." You notice that his hair appears unwashed and some of his clothes are on backward. Urine toxicology is negative for illicit drugs. Which of the following additional findings are you most likely to see in this patient during the course of his illness?
- A. Anhedonia, guilty rumination, and insomnia
- B. Grandiose delusions, racing thoughts, and pressured speech
- C. Asociality, flat affect, and alogia (Correct Answer)
- D. Amnesia, multiple personality states, and de-realization
- E. Intrusive thoughts, ritualized behaviors, and anxious mood
Prodromal phase and early intervention Explanation: ***Asociality, flat affect, and alogia***
- This patient exhibits **delusions (persecutory, control)** and **auditory hallucinations**, classic positive symptoms of **schizophrenia**. The question asks about findings "during the course of his illness," which points to the **typical progression of schizophrenia**: patients initially present with **positive symptoms** (as seen in this case) and **over time develop negative symptoms** such as **asociality** (lack of motivation to engage in social interaction), **flat affect** (reduced emotional expression), and **alogia** (poverty of speech).
- The disorganized appearance (unwashed hair, clothes on backward) already demonstrates **disorganized behavior**, part of the schizophrenia spectrum. Negative symptoms typically emerge or worsen as the illness progresses, representing the most likely additional findings.
*Anhedonia, guilty rumination, and insomnia*
- While **anhedonia** and **insomnia** can be seen in schizophrenia, their presence alongside prominent **guilty rumination** would more strongly suggest a **depressive disorder with psychotic features**, rather than primary schizophrenia, especially with the patient's specific, classic psychotic symptoms.
- The primary symptoms described (delusions of control, auditory hallucinations) are more characteristic of primary psychotic disorders, and guilty rumination is not a typical feature of schizophrenia progression.
*Grandiose delusions, racing thoughts, and pressured speech*
- These symptoms are hallmark features of **mania** or a **manic episode with psychotic features**. While psychotic features can occur in bipolar disorder with mania, the patient's specific delusions of being controlled by spies and hearing voices discussing him are more typical of schizophrenia.
- The absence of information about elevated mood, increased energy, or decreased need for sleep also makes mania less likely compared to schizophrenia.
*Amnesia, multiple personality states, and de-realization*
- These symptoms are characteristic of **dissociative disorders**. **Amnesia** and **multiple personality states** (now known as identity alteration in dissociative identity disorder) involve disturbances in memory and identity.
- **De-realization** involves feelings of unreality regarding one's surroundings. None of these align with the patient's primary presentation of well-formed delusions and hallucinations characteristic of a psychotic disorder.
*Intrusive thoughts, ritualized behaviors, and anxious mood*
- These are core features of **obsessive-compulsive disorder (OCD)**. The patient's symptoms are clearly defined as delusions (fixed false beliefs) and hallucinations (perceptions without external stimuli), which are distinct from the ego-dystonic intrusive thoughts and ritualistic compulsions of OCD.
- While anxiety may be present in psychotic disorders, the primary presentation here is not dominated by OCD-like symptoms, and these would not be expected to develop as part of schizophrenia's natural course.
Prodromal phase and early intervention US Medical PG Question 7: A 35-year-old man comes to the Veterans Affairs hospital because of a 2-month history of anxiety. He recently returned from his third deployment to Iraq, where he served as a combat medic. He has had difficulty readjusting to civilian life. He works as a taxi driver but had to take a leave of absence because of difficulties with driving. Last week, he hit a stop sign because he swerved out of the way of a grocery bag that was in the street. He has difficulty sleeping because of nightmares about the deaths of some of the other soldiers in his unit and states, “it's my fault, I could have saved them. Please help me.” Mental status examination shows a depressed mood and a restricted affect. There is no evidence of suicidal ideation. Which of the following is the most appropriate initial step in treatment?
- A. Dialectical behavioral therapy
- B. Venlafaxine therapy
- C. Cognitive behavioral therapy (Correct Answer)
- D. Motivational interviewing
- E. Prazosin therapy
Prodromal phase and early intervention Explanation: ***Cognitive behavioral therapy***
- **Cognitive Behavioral Therapy (CBT)** is considered a first-line psychological treatment for **Post-Traumatic Stress Disorder (PTSD)**, which the patient's symptoms (deployments, intrusive thoughts, nightmares, avoidance, guilt) strongly suggest.
- CBT helps individuals identify and challenge **maladaptive thought patterns** and behaviors related to the trauma, fostering new coping mechanisms.
*Dialectical behavioral therapy*
- **Dialectical Behavioral Therapy (DBT)** is primarily used for individuals with **Borderline Personality Disorder** or severe emotional dysregulation.
- While it can help with emotional regulation, it is not the **first-line therapy** specifically targeting trauma-related cognitive distortions and avoidance behaviors seen in PTSD.
*Venlafaxine therapy*
- **Venlafaxine**, an SNRI, is an antidepressant that can be effective for PTSD symptoms. However, current guidelines recommend **psychotherapy (like CBT)** as the initial step, especially when feasible.
- While pharmacotherapy can be used, it's typically considered **adjunctive** or for cases where psychotherapy alone is insufficient or not preferred.
*Motivational interviewing*
- **Motivational interviewing** is a patient-centered counseling style used to address ambivalence and enhance a person's **intrinsic motivation** for change.
- It is often utilized in substance abuse treatment or when patients are resistant to treatment, but it is not a primary, standalone treatment for the core symptoms of PTSD.
*Prazosin therapy*
- **Prazosin** is an alpha-1 antagonist used off-label to treat **PTSD-related nightmares** and sleep disturbances.
- While it can be helpful for a specific symptom, it does not address the broader spectrum of PTSD symptoms, such as intrusive thoughts, avoidance, or negative cognitions.
Prodromal phase and early intervention US Medical PG Question 8: A 23-year-old male presents to the emergency department. He was brought in by police for shouting on a subway. The patient claims that little people were trying to kill him, and he was acting within his rights to defend himself. The patient has a past medical history of marijuana and IV drug use as well as multiple suicide attempts. He is currently homeless. While in the ED, the patient is combative and refuses a physical exam. He is given IM haloperidol and diphenhydramine. The patient is transferred to the inpatient psychiatric unit and is continued on haloperidol throughout the next week. Though he is no longer aggressive, he is seen making "armor" out of paper plates and plastic silverware to defend himself. The patient is switched onto risperidone. The following week the patient is still seen gathering utensils, and muttering about people trying to harm him. The patient's risperidone is discontinued. Which of the following is the best next step in management?
- A. Olanzapine
- B. Thioridazine
- C. Clozapine (Correct Answer)
- D. Chlorpromazine
- E. Fluphenazine
Prodromal phase and early intervention Explanation: ***Clozapine***
- This patient has demonstrated **treatment-resistant schizophrenia**, evidenced by persistent positive symptoms despite trials of haloperidol and risperidone, necessitating a trial of clozapine.
- **Clozapine** is an atypical antipsychotic that is uniquely effective for treatment-resistant schizophrenia, especially in patients with a history of **suicidality**.
*Olanzapine*
- While **olanzapine** is an effective atypical antipsychotic, it is generally considered a first-line or second-line agent, and this patient has already failed two antipsychotics (haloperidol and risperidone).
- Its efficacy in **treatment-resistant cases** is not superior to clozapine.
*Thioridazine*
- **Thioridazine** is a first-generation antipsychotic with a high risk of **QT prolongation** and other cardiac side effects, making it a less safe option.
- It is not typically reserved for **treatment-resistant schizophrenia** due to its side effect profile and lack of superior efficacy compared to newer agents.
*Chlorpromazine*
- **Chlorpromazine** is another first-generation antipsychotic that is not indicated for **treatment-resistant schizophrenia** at this stage.
- It carries significant anticholinergic and sedative side effects, similar to thioridazine, and is not significantly more effective than haloperidol for this indication.
*Fluphenazine*
- **Fluphenazine** is a potent first-generation antipsychotic, often available as a **depot injection** for adherence issues.
- However, it is not considered the best next step for **treatment-resistant schizophrenia** after failure of two different classes of antipsychotics.
Prodromal phase and early intervention US Medical PG Question 9: A 22-year-old man presents to the emergency department with anxiety. The patient states that he is very anxious and has not been able to take his home anxiety medications. He is requesting to have his home medications administered. The patient has a past medical history of anxiety and depression. His current medications include clonazepam, amitriptyline, and lorazepam. Notably, the patient has multiple psychiatric providers who currently care for him. His temperature is 99.2°F (37.3°C), blood pressure is 130/85 mmHg, pulse is 112/min, respirations are 22/min, and oxygen saturation is 100% on room air. Physical exam is notable for an anxious, sweating, and tremulous young man who becomes more confused during his stay in the emergency department. Which of the following should be given to this patient?
- A. Diazepam (Correct Answer)
- B. Sodium bicarbonate
- C. Flumazenil
- D. Supportive therapy and monitoring
- E. Midazolam
Prodromal phase and early intervention Explanation: ***Diazepam***
- This patient presents with classic **benzodiazepine withdrawal syndrome**: anxiety, tremors, sweating, tachycardia, tachypnea, and progressive confusion after being unable to take his home benzodiazepines (clonazepam and lorazepam).
- Benzodiazepine withdrawal is a **medical emergency** that can progress to seizures, delirium, and death if untreated.
- **Diazepam** is the preferred treatment due to its **long half-life**, which provides smooth, sustained benzodiazepine receptor activity and prevents withdrawal progression.
- The autonomic instability (elevated pulse and respiratory rate) and neurological symptoms (tremors, confusion) require immediate benzodiazepine administration, not just supportive care.
*Supportive therapy and monitoring*
- While monitoring is important, **supportive care alone is inadequate** for benzodiazepine withdrawal with autonomic instability and confusion.
- Untreated benzodiazepine withdrawal can rapidly progress to **seizures, severe delirium, and cardiovascular collapse**.
- The objective signs (tachycardia, tremors, sweating, confusion) indicate physiological withdrawal, not simply anxiety or drug-seeking behavior.
- Active treatment with benzodiazepines is the **standard of care** to prevent life-threatening complications.
*Sodium bicarbonate*
- Sodium bicarbonate treats **metabolic acidosis** or specific overdoses (e.g., tricyclic antidepressants, aspirin).
- There is no indication of acidosis or TCA toxicity in this presentation; the patient has withdrawal symptoms, not overdose.
*Flumazenil*
- Flumazenil is a benzodiazepine antagonist that **reverses benzodiazepine effects** in acute overdose.
- It is **absolutely contraindicated** in patients with chronic benzodiazepine use or dependence, as it can precipitate **severe withdrawal, seizures, and status epilepticus**.
- This patient needs benzodiazepine administration, not reversal.
*Midazolam*
- While midazolam is a benzodiazepine that could treat withdrawal acutely, its **short half-life** makes it less ideal for managing withdrawal syndrome.
- **Diazepam or chlordiazepoxide** (long-acting agents) are preferred for withdrawal management as they provide sustained coverage and smoother tapering.
- Midazolam would require frequent redosing and carries higher risk of rebound withdrawal.
Prodromal phase and early intervention US Medical PG Question 10: Two days after undergoing hemicolectomy for colon cancer, a 78-year-old man is found agitated and confused in his room. He says that a burglar broke in. The patient points at one corner of the room and says “There he is, doctor!” Closer inspection reveals that the patient is pointing to his bathrobe, which is hanging on the wall. The patient has type 2 diabetes mellitus and arterial hypertension. Current medications include insulin and hydrochlorothiazide. His temperature is 36.9°C (98.4°F), pulse is 89/min, respirations are 15/min, and blood pressure is 145/98 mm Hg. Physical examination shows a nontender, nonerythematous midline abdominal wound. On mental status examination, the patient is agitated and oriented only to person. Which of the following best describes this patient's perception?
- A. Hallucination
- B. Illusion (Correct Answer)
- C. Loose association
- D. Delusion
- E. External attribution
Prodromal phase and early intervention Explanation: ***Illusion***
- An **illusion** is a **misinterpretation of an actual external stimulus**, as seen when the patient perceives his bathrobe as a burglar.
- This symptom, combined with **agitation**, **confusion**, and **recent surgery**, is highly suggestive of **delirium**.
*Hallucination*
- A **hallucination** is a **perception in the absence of an external stimulus**, meaning the patient would see or hear something that is not there at all.
- The patient here is clearly reacting to an existing object (the bathrobe), albeit misinterpreting it.
*Loose association*
- **Loose association** refers to a **thought disorder** where ideas shift from one subject to another in a way that is unrelated or minimally related, making the speech difficult to follow.
- This describes a pattern of thought, not a perceptual disturbance involving an external object.
*Delusion*
- A **delusion** is a **fixed, false belief** that is not amenable to change in light of conflicting evidence and is not in keeping with the individual's cultural background.
- While the patient believes a burglar is present, this belief arises from a direct misinterpretation of an object rather than a fixed, unfounded belief.
*External attribution*
- **External attribution** is a psychological concept where individuals ascribe responsibility for events or outcomes to **external factors** rather than internal ones.
- This term describes a cognitive bias in explaining causality, not a perceptual disturbance.
More Prodromal phase and early intervention US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.