Neurobiological theories of schizophrenia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neurobiological theories of schizophrenia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neurobiological theories of schizophrenia US Medical PG Question 1: A 72-year-old man is brought to your office by his daughter due to concern over recent behavioral changes. Over the last several months he has had increasing difficulty with remembering recent events. She mentions that he is embarrassed due to a new inability to control urination. His medical history is significant for hypertension and insomnia. His medications include alprazolam and hydrochlorothiazide. On physical exam, he is oriented to time and place and thinks his daughter is exaggerating; however, when asked to recall 3 items, the patient refuses to continue the mental status exam. He has 5/5 strength bilaterally. He walks in short strides by sliding his feet across the floor. Which of the following would you expect to see in this patient?
- A. Depigmentation of the substantia nigra pars compacta
- B. Convex hemorrhage that does not cross suture lines
- C. Atrophy of the caudate and putamen
- D. Distortion of corona radiata fibers (Correct Answer)
- E. Atrophy of the subthalamic nucleus
Neurobiological theories of schizophrenia Explanation: ***Distortion of corona radiata fibers***
- The patient's symptoms of **memory decline**, **urinary incontinence**, and **gait disturbance** (magnetic gait) form the classic triad of **normal pressure hydrocephalus (NPH)**.
- In NPH, the enlarged ventricles cause **stretching and distortion of the periventricular white matter tracts**, including the ascending and descending fibers of the **corona radiata**, which leads to the characteristic neurological symptoms.
*Depigmentation of the substantia nigra pars compacta*
- This is a hallmark pathological finding in **Parkinson's disease**, characterized by the loss of **dopaminergic neurons** in the substantia nigra.
- While gait disturbance (shuffling gait) can occur in Parkinson's, the presenting symptoms of **urinary incontinence** and prominent memory decline are not typical primary features, and the gait description is more suggestive of NPH.
*Convex hemorrhage that does not cross suture lines*
- This describes an **epidural hematoma**, typically resulting from **head trauma** and often associated with rupture of the **middle meningeal artery**.
- The clinical presentation is usually acute with signs of increased intracranial pressure, rather than the chronic, progressive symptoms described in the patient.
*Atrophy of the caudate and putamen*
- This is a characteristic finding in **Huntington's disease**, a neurodegenerative disorder.
- Huntington's typically presents with **chorea** (involuntary movements), psychiatric disturbances, and cognitive decline, which do not align with the patient's primary symptoms of gait disturbance and incontinence.
*Atrophy of the subthalamic nucleus*
- Atrophy of the subthalamic nucleus is not a distinct primary disorder associated with the patient's constellation of symptoms.
- The subthalamic nucleus plays a role in motor control, and damage to it can cause **hemiballismus**, which is not described here.
Neurobiological theories of schizophrenia US Medical PG Question 2: A 37-year-old woman presents to the general medical clinic with a chief complaint of anxiety. She has been having severe anxiety and fatigue for the past seven months. She has difficulty concentrating and her work has suffered, and she has also developed diarrhea from the stress. She doesn't understand why she feels so anxious and is unable to attribute it to any specific aspect of her life right now. You decide to begin pharmacotherapy. All of the following are suitable mechanisms of drugs that can treat this illness EXCEPT:
- A. A drug that stimulates 5-HT1A receptors
- B. A drug that blocks dopamine 2 receptors (Correct Answer)
- C. A drug that acts as a GABA agonist
- D. A drug that blocks 5-HT reuptake
- E. A drug that blocks both serotonin and norepinephrine reuptake
Neurobiological theories of schizophrenia Explanation: ***A drug that blocks dopamine 2 receptors***
- This option describes **first-generation antipsychotics**, which primarily block **dopamine D2 receptors**. These are generally used for psychotic disorders (e.g., schizophrenia) and severe agitation, not typically for generalized anxiety disorder as a first-line treatment.
- Blocking D2 receptors can lead to **extrapyramidal symptoms** and is not a common therapeutic target for anxiety, which is more reliably treated by targeting serotonin, norepinephrine, and GABA systems.
*A drug that stimulates 5-HT1A receptors*
- This describes **buspirone**, an anxiolytic that is effective for **generalized anxiety disorder (GAD)**.
- **Stimulation of 5-HT1A receptors** helps to modulate serotonin activity and reduce anxiety without significant sedative effects or risk of dependence associated with benzodiazepines.
*A drug that acts as a GABA agonist*
- This describes **benzodiazepines**, which enhance the inhibitory effects of **GABA** in the central nervous system.
- They are effective for acute anxiety relief but carry risks of **sedation**, **tolerance**, and **dependence**, making them suitable mainly for short-term or intermittent use.
*A drug that blocks 5-HT reuptake*
- This describes **selective serotonin reuptake inhibitors (SSRIs)**, which are considered first-line treatment for various anxiety disorders, including GAD.
- By increasing **serotonin levels** in the synaptic cleft, SSRIs help to regulate mood and reduce anxiety symptoms over time.
*A drug that blocks both serotonin and norepinephrine reuptake*
- This describes **serotonin-norepinephrine reuptake inhibitors (SNRIs)**, such as venlafaxine or duloxetine.
- SNRIs are also first-line treatments for GAD, working by increasing both **serotonin** and **norepinephrine** in the brain, offering broad-spectrum anxiolytic and antidepressant effects.
Neurobiological theories of schizophrenia US Medical PG Question 3: A patient with a pituitary tumor demonstrates elevated prolactin levels. Which of the following changes in dopamine signaling best explains the hyperprolactinemia?
- A. Increased D1 receptor activation
- B. Enhanced dopamine reuptake
- C. Increased dopamine synthesis
- D. Decreased tuberoinfundibular dopamine release (Correct Answer)
- E. Increased D2 receptor activation
Neurobiological theories of schizophrenia Explanation: ***Decreased tuberoinfundibular dopamine release***
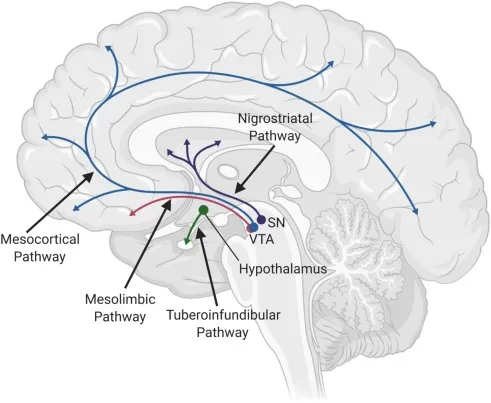
- **Dopamine** acts as a **prolactin-inhibiting hormone (PIH)**, primarily through the **tuberoinfundibular pathway** from the hypothalamus to the pituitary [1].
- A **pituitary tumor** can compress or damage the pituitary stalk or the hypothalamus, leading to decreased dopamine delivery to the pituitary and thus **hyperprolactinemia** [1].
*Increased D1 receptor activation*
- **D1 receptors** are generally associated with **excitatory effects** and are not the primary receptors mediating dopamine's inhibitory effect on prolactin.
- **Dopamine's inhibitory action** on prolactin secretion is predominantly mediated by **D2 receptors**.
*Enhanced dopamine reuptake*
- Enhanced reuptake would lead to **less dopamine availability** at the receptor site, which would indeed cause hyperprolactinemia.
- However, this is not the most direct or specific consequence of a **pituitary tumor's mechanical effects** on dopamine signaling [1].
*Increased dopamine synthesis*
- **Increased dopamine synthesis** would lead to higher dopamine levels and thus **inhibit prolactin secretion**, which is contrary to the hyperprolactinemia observed in the patient.
- This option would result in **hypoprolactinemia**.
*Increased D2 receptor activation*
- **D2 receptor activation** by dopamine **inhibits prolactin release** from lactotrophs in the pituitary [1].
- Therefore, increased D2 receptor activation would lead to **decreased prolactin levels**, not hyperprolactinemia.
Neurobiological theories of schizophrenia US Medical PG Question 4: A 26-year-old man is brought to the hospital by his wife who complains that her husband has been behaving oddly for the past few hours. The patient’s wife says that she has known him for only 4 months. The wife is unable to give any past medical history. The patient’s speech is difficult to follow, and he seems very distracted. After 15 minutes, he becomes agitated and starts to bang his head on a nearby pillar. He is admitted to the psychiatric ward and is given an emergency medication, after which he calms down. In the next 2 days, he continues to become agitated at times and required 2 more doses of the same drug. On the 4th day of admission, he appears very weak, confused, and does not respond to questions appropriately. His vital signs include: temperature 40.0°C (104.0°F), blood pressure 160/95 mm Hg, and pulse 114/min. On physical examination, he is profusely diaphoretic. He is unable to stand upright or even get up from his bed. Which of the following is the mechanism of action of the drug which most likely caused this patient’s current condition?
- A. Skeletal muscle relaxation
- B. Agonistic effect on dopamine receptors
- C. Serotonin reuptake inhibition
- D. Histamine H2 receptor blocking
- E. Dopamine receptor blocking (Correct Answer)
Neurobiological theories of schizophrenia Explanation: ***Dopamine receptor blocking***
- The patient's presentation with **fever, altered mental status, muscle rigidity**, and **autonomic instability** (tachycardia, hypertension, diaphoresis) after receiving antipsychotic medication strongly suggests **neuroleptic malignant syndrome (NMS)**.
- NMS is caused by a severe decrease in **dopaminergic activity**, primarily due to the blockade of **D2 dopamine receptors** in the basal ganglia and hypothalamus by antipsychotics.
- The classic tetrad of NMS includes: **hyperthermia, muscle rigidity, altered mental status**, and **autonomic instability**.
*Skeletal muscle relaxation*
- While agitation might be treated with benzodiazepines, which cause muscle relaxation, this mechanism does not explain the **severe rigidity, hyperthermia**, and **autonomic dysfunction** seen in the patient.
- **Muscle rigidity** (lead-pipe rigidity) is a hallmark of the patient's current condition, contradicting the idea of muscle relaxation.
*Agonistic effect on dopamine receptors*
- An agonistic effect on dopamine receptors would typically lead to symptoms similar to **psychosis** or **mania**, not the severe rigidity and hypodopaminergic state observed in NMS.
- This mechanism would counteract the effects of antipsychotics and would not cause NMS.
*Serotonin reuptake inhibition*
- This is the mechanism of action for **SSRIs**, and an excess of serotonin can lead to **serotonin syndrome**, which shares some features with NMS but typically includes **hyperreflexia** and **myoclonus**, rather than lead-pipe rigidity.
- The context of treating acute psychosis with an emergency medication points more towards an antipsychotic, not an antidepressant.
*Histamine H2 receptor blocking*
- **Histamine H2 receptor blockers** are used to treat conditions like **acid reflux** and **peptic ulcers**; they have no direct neurological effects that would cause NMS.
- This mechanism is entirely irrelevant to the patient's psychiatric symptoms and subsequent severe adverse reaction.
Neurobiological theories of schizophrenia US Medical PG Question 5: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Neurobiological theories of schizophrenia Explanation: ***Mesolimbic pathway***
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Neurobiological theories of schizophrenia US Medical PG Question 6: A 28-year-old woman presents with weight gain and a milky-white discharge from her breasts. Patient says she noticed herself gaining weight and a milky white discharge from her breasts. Past medical history is significant for schizophrenia, recently diagnosed and treated with risperidone. No history of headache, nausea, and vomiting. No other current medications. Her last menstrual period was 2 months ago. Review of systems is significant for decreased libido. Patient is afebrile and vital signs are within normal limits. On physical examination, patient had a weight gain of 3 kg (6.6 lb) over the past month. There is bilateral breast tenderness present. A urine pregnancy test is negative. Which of the following is the most likely etiology of this patient’s symptoms?
- A. Increase in dopamine activity in mesolimbic pathway
- B. Decrease in dopamine activity in mesolimbic pathway
- C. Decrease in dopamine activity in tuberoinfundibular pathway (Correct Answer)
- D. Decrease in dopamine activity in nigrostriatal pathway
- E. Increase in dopamine activity in tuberoinfundibular pathway
Neurobiological theories of schizophrenia Explanation: ***Decrease in dopamine activity in tuberoinfundibular pathway***
- The patient is taking **risperidone**, an antipsychotic that blocks **dopamine D2 receptors**. This blockade in the **tuberoinfundibular pathway** leads to increased prolactin secretion.
- Elevated **prolactin** levels cause **galactorrhea** (milky discharge), **amenorrhea** (missed periods), **weight gain**, and **decreased libido**.
*Increase in dopamine activity in mesolimbic pathway*
- An **increase in dopamine activity** in the **mesolimbic pathway** is associated with the positive symptoms of **schizophrenia** (e.g., hallucinations, delusions).
- Antipsychotics like risperidone aim to decrease this activity, not increase it, and this pathway is not directly involved in prolactin regulation.
*Decrease in dopamine activity in mesolimbic pathway*
- A **decrease in dopamine activity** in the **mesolimbic pathway** is the desired therapeutic effect of antipsychotics like risperidone, reducing psychotic symptoms.
- While it explains the treatment of schizophrenia, it does not explain the specific side effects of hyperprolactinemia.
*Decrease in dopamine activity in nigrostriatal pathway*
- A **decrease in dopamine activity** in the **nigrostriatal pathway** is responsible for **extrapyramidal symptoms** (EPS) such as parkinsonism (tremor, rigidity), akathisia, and dystonia.
- While antipsychotics can cause EPS, these are not the predominant symptoms (galactorrhea, weight gain, amenorrhea) described in the patient.
*Increase in dopamine activity in tuberoinfundibular pathway*
- An **increase in dopamine activity** in the **tuberoinfundibular pathway** would lead to a decrease in prolactin secretion, as dopamine is a **prolactin-inhibiting hormone**.
- This would result in symptoms opposite to what the patient is experiencing, such as no galactorrhea or even hypoprolactinemia.
Neurobiological theories of schizophrenia US Medical PG Question 7: A 20-year-old male is brought to a psychiatrist by his parents for bizarre behavior. His parents report that over the past two semesters in school, his personality and behavior have changed noticeably. He refuses to leave his room because he believes people are spying on him. He hears voices that are persecutory and is convinced that people at school have chips implanted in their brains to spy on him. Screenings for depression and mania are negative. His past medical history is unremarkable. His family history is notable for a maternal uncle with bipolar disorder. He does not drink alcohol or smoke. His temperature is 98.8°F (37.1°C), blood pressure is 115/70 mmHg, pulse is 85/min, and respirations are 18/min. On examination, he appears to be responding to internal stimuli. Which of the following pathways is primarily responsible for these symptoms?
- A. Papez circuit
- B. Mesocortical pathway
- C. Nigrostriatal pathway
- D. Tuberoinfundibular pathway
- E. Mesolimbic pathway (Correct Answer)
Neurobiological theories of schizophrenia Explanation: ***Mesolimbic pathway***
- The **mesolimbic pathway** is primarily associated with the **positive symptoms of psychosis**, such as **hallucinations and delusions**, due to **dopamine hyperactivity**.
- The patient's **persecutory delusions, auditory hallucinations, and paranoia** are hallmark positive symptoms seen in conditions like schizophrenia, which are mediated by this pathway.
*Papez circuit*
- The **Papez circuit** is involved in **emotion and memory**, connecting structures like the hippocampus and cingulate gyrus.
- Dysregulation of this circuit would more likely manifest as deficits in memory or emotional regulation rather than the prominent psychotic features described.
*Mesocortical pathway*
- The **mesocortical pathway** projects to the **prefrontal cortex** and is implicated in **negative symptoms** (e.g., apathy, flat affect) and **cognitive deficits** (e.g., executive dysfunction) of psychosis, often due to **dopamine hypoactivity**.
- While cognitive and negative symptoms can co-occur in psychotic disorders, they are not the primary, most striking symptoms described here.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** is crucial for **motor control**, connecting the substantia nigra to the striatum.
- Dysfunction in this pathway leads to **extrapyramidal symptoms** (e.g., tremors, rigidity, dyskinesia), which are not present in this patient's presentation.
*Tuberoinfundibular pathway*
- The **tuberoinfundibular pathway** connects the hypothalamus to the pituitary gland and regulates **prolactin secretion**.
- Its primary role is in neuroendocrine function, and its dysfunction would lead to **hyperprolactinemia** and related symptoms, not the psychotic features described.
Neurobiological theories of schizophrenia US Medical PG Question 8: A 28-year-old man is brought to the emergency department after he was found half dressed and incoherent in the middle of the road. In the emergency department he states that he has not slept for 36 hours and that he has incredible ideas that will make him a billionaire within a few months. He also states that secret agents from Russia are pursuing him and that he heard one of them speaking through the hospital intercom. His past medical history is significant only for a broken arm at age 13. On presentation, his temperature is 102.2°F (39°C), blood pressure is 139/88 mmHg, pulse is 112/min, and respirations are 17/min. Physical exam reveals pupillary dilation and psychomotor agitation. Which of the following mechanisms is most likely responsible for this patient's symptoms?
- A. N-methyl-D-aspartate receptor antagonist
- B. Gamma-aminobutyric acid receptor agonist
- C. Increased biogenic amine release (Correct Answer)
- D. 5-HT receptor agonist
- E. Opioid receptor agonist
Neurobiological theories of schizophrenia Explanation: ***Increased biogenic amine release***
- The patient exhibits a classic constellation of symptoms consistent with **stimulant intoxication**, including **psychomotor agitation**, **pupillary dilation**, **tachycardia**, **hyperthermia**, **insomnia**, **grandiosity**, and **paranoia**.
- Stimulants like **amphetamines** and **cocaine** primarily exert their effects by increasing the release and inhibiting the reuptake of **biogenic amines** (dopamine, norepinephrine, serotonin) in the brain, leading to an exaggerated sympathetic response and altered mental status.
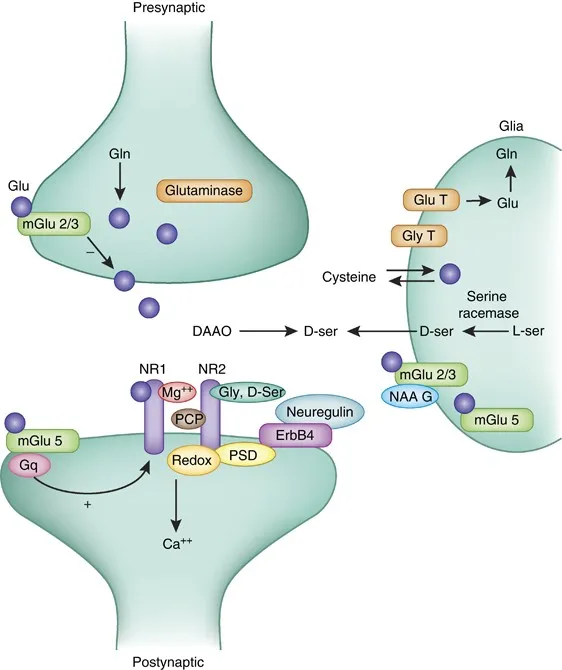
*N-methyl-D-aspartate receptor antagonist*
- **NMDA receptor antagonists** (e.g., phencyclidine - PCP, ketamine) are associated with dissociative symptoms, nystagmus, and sometimes aggression, but generally do not present with the prominent **hyperthermia** and grandiosity seen here.
- While they can cause psychotic symptoms, the specific combination of signs points more strongly to **stimulant intoxication**.
*Gamma-aminobutyric acid receptor agonist*
- **GABA receptor agonists** (e.g., benzodiazepines, barbiturates) cause **CNS depression**, sedation, respiratory depression, and ataxia.
- These effects are contrary to the patient's presentation of **agitation**, **increased heart rate**, and **hyperthermia**.
*5-HT receptor agonist*
- While drugs like **LSD** and **MDMA** (ecstasy) act as 5-HT receptor agonists and can cause hallucinations and altered perception, the prominent **paranoia**, **grandiosity**, and **significant hyperthermia** in this scenario are more characteristic of stimulant toxicity, which involves a broader increase in biogenic amine release beyond just serotonin.
- MDMA, in particular, can cause hyperthermia, but the full clinical picture is more suggestive of traditional stimulants.
*Opioid receptor agonist*
- **Opioid receptor agonists** (e.g., heroin, morphine) typically cause **CNS depression**, **miosis** (pinpoint pupils), respiratory depression, and sedation.
- These effects are the **opposite** of the patient's symptoms of pupillary dilation, agitation, and hyperthermia.
Neurobiological theories of schizophrenia US Medical PG Question 9: A 27-year-old woman is brought to the office at the insistence of her fiancé to be evaluated for auditory hallucinations for the past 8 months. The patient’s fiancé tells the physician that the patient often mentions that she can hear her own thoughts speaking aloud to her. The hallucinations have occurred intermittently for at least 1-month periods. Past medical history is significant for hypertension. Her medications include lisinopril and a daily multivitamin both of which she frequently neglects. She lost her security job 7 months ago after failing to report to work on time. The patient’s vital signs include: blood pressure 132/82 mm Hg; pulse 72/min; respiratory rate 18/min, and temperature 36.7°C (98.1°F). On physical examination, the patient has a flat affect and her focus fluctuates from the window to the door. She is disheveled with a foul smell. She has difficulty focusing on the discussion and does not quite understand what is happening around her. A urine toxicology screen is negative. Which of the following is the correct diagnosis for this patient?
- A. Schizoaffective disorder
- B. Schizophrenia (Correct Answer)
- C. Schizoid personality disorder
- D. Schizophreniform disorder
- E. Schizotypal personality disorder
Neurobiological theories of schizophrenia Explanation: ***Schizophrenia***
- The patient exhibits core symptoms of schizophrenia, including **auditory hallucinations** (hearing thoughts speaking aloud), **disorganized thinking** (difficulty focusing, fluctuating focus), and **negative symptoms** (flat affect, disheveled, foul smell, loss of job due to poor function). These symptoms have been present for **at least 6 months** (8 months of hallucinations, 7 months of job loss), which meets the diagnostic criteria.
- The duration of symptoms (over 6 months) differentiates it from schizophreniform disorder, and the absence of prominent mood episodes rules out schizoaffective disorder.
*Schizoaffective disorder*
- This diagnosis requires a **major mood episode** (depressive or manic) concurrent with Criterion A of schizophrenia, along with a period of **at least 2 weeks of delusions or hallucinations in the absence of prominent mood symptoms**.
- While the patient has some signs of distress (lost job, disorganized), a full major mood episode is not described, and the primary symptoms are clearly psychotic.
*Schizoid personality disorder*
- This is characterized by a pervasive pattern of **detachment from social relationships** and a restricted range of emotional expression, often appearing indifferent to praise or criticism.
- The patient's symptoms are primarily psychotic (hallucinations, disorganized thought), not just social withdrawal or emotional flatness. She doesn't necessarily avoid social contact, but her psychosis interferes with it.
*Schizophreniform disorder*
- This disorder presents with symptoms identical to schizophrenia but with a **duration of at least 1 month but less than 6 months**.
- The patient's symptoms, particularly the auditory hallucinations, have been present for 8 months and are therefore outside the timeframe for schizophreniform disorder.
*Schizotypal personality disorder*
- This disorder involves a pervasive pattern of **social and interpersonal deficits** marked by acute discomfort with, and reduced capacity for, close relationships, as well as **cognitive or perceptual distortions** and eccentric behaviors.
- While there may be some odd beliefs or magical thinking, **full-blown psychotic symptoms like prominent auditory hallucinations** (hearing thoughts speaking aloud) are generally not present as consistently or severely as seen in this patient, who meets criteria for a major psychotic disorder.
Neurobiological theories of schizophrenia US Medical PG Question 10: A 21-year-old man presents to an outpatient psychiatrist with chief complaints of fatigue and “hearing voices.” He describes multiple voices which sometimes call his name or say nonsensical things to him before he falls asleep at night. He occasionally awakes to see “strange people” in his room, which frighten him but then disappear. The patient is particularly worried by this because his uncle developed schizophrenia when he was in his 20s. The patient also thinks he had a seizure a few days ago, saying he suddenly fell to the ground without warning, though he remembers the episode and denied any abnormal movements during it. He is in his 3rd year of college and used to be a top student, but has been getting C and D grades over the last year, as he has had trouble concentrating and fallen asleep during exams numerous times. He denies changes in mood and has continued to sleep 8 hours per night and eat 3 meals per day recently. Which of the following medications will be most beneficial for this patient?
- A. Haloperidol
- B. Valproic acid
- C. Risperidone
- D. Modafinil (Correct Answer)
- E. Levetiracetam
Neurobiological theories of schizophrenia Explanation: ***Modafinil***
- This patient presents with **narcolepsy**, characterized by the **classic tetrad**: excessive daytime sleepiness (falling asleep during exams), **cataplexy** (sudden fall without loss of consciousness or abnormal movements), **hypnagogic hallucinations** (hearing voices before sleep), and **hypnopompic hallucinations** (seeing people upon awakening).
- The hallucinations are **not true psychotic symptoms** but rather dream-like phenomena occurring at sleep-wake transitions, which are common in narcolepsy.
- **Modafinil** is a first-line **wakefulness-promoting agent** that treats the excessive daytime sleepiness and improves alertness, addressing the primary pathology.
- The patient's family history of schizophrenia is a red herring; his symptoms are explained by narcolepsy, not a primary psychotic disorder.
*Risperidone*
- Risperidone is an **atypical antipsychotic** used for schizophrenia and other psychotic disorders.
- This patient does **not have a primary psychotic disorder**—the hallucinations are hypnagogic/hypnopompic phenomena associated with narcolepsy, not true psychotic hallucinations.
- Using an antipsychotic would be inappropriate and could **worsen daytime sleepiness** due to sedating effects, exacerbating the patient's core problem.
*Haloperidol*
- Haloperidol is a **first-generation antipsychotic** with significant risk of **extrapyramidal side effects**.
- Like risperidone, it would be inappropriate here as the patient does not have a psychotic disorder, and it would worsen sedation and daytime sleepiness.
*Valproic acid*
- Valproic acid is a **mood stabilizer and anticonvulsant** used for bipolar disorder and seizure disorders.
- The described "seizure" event is actually **cataplexy** (preserved consciousness, no abnormal movements), not a true seizure, so an anticonvulsant is not indicated.
- It would not address the narcolepsy symptoms and can cause sedation.
*Levetiracetam*
- Levetiracetam is an **anticonvulsant** medication.
- The patient's description (remembering the episode, no abnormal movements) is inconsistent with a seizure and consistent with **cataplexy**, which is treated by addressing the underlying narcolepsy, not with anticonvulsants.
More Neurobiological theories of schizophrenia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.