Negative symptoms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Negative symptoms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Negative symptoms US Medical PG Question 1: A 24-year-old man is brought to your emergency department under arrest by the local police. The patient was found naked at a busy intersection jumping up and down on top of a car. Interviewing the patient, you discover that he has not slept in 2 days because he does not feel tired. He reports hearing voices. The patient was previously hospitalized 1 year ago with auditory hallucinations, paranoia, and a normal mood. What is the most likely diagnosis?
- A. Schizophrenia
- B. Bipolar disorder
- C. Brief psychotic disorder
- D. Schizotypal disorder
- E. Schizoaffective disorder (Correct Answer)
Negative symptoms Explanation: ***Schizoaffective disorder***
- This patient demonstrates the **hallmark feature** of schizoaffective disorder: **psychotic symptoms occurring both during AND independent of mood episodes**.
- **Current presentation**: Clear **manic episode** (decreased need for sleep, grandiose/disinhibited behavior, psychomotor agitation) with psychotic features (auditory hallucinations).
- **Previous hospitalization**: **Psychotic symptoms (hallucinations, paranoia) in the absence of a mood episode** ("normal mood"), requiring hospitalization for at least 2 weeks - this is the **key diagnostic criterion** for schizoaffective disorder.
- The diagnosis requires an **uninterrupted period of illness** with both psychotic symptoms (meeting Criterion A for schizophrenia) and a major mood episode, PLUS psychotic symptoms for **≥2 weeks without prominent mood symptoms**.
*Bipolar disorder*
- In bipolar disorder with psychotic features, psychotic symptoms occur **exclusively during mood episodes** (manic, hypomanic, or depressive).
- This patient's previous hospitalization with psychosis but **"normal mood"** indicates psychotic symptoms independent of mood episodes, which **rules out** bipolar disorder and points to schizoaffective disorder.
- While the current presentation shows mania with psychosis, the longitudinal course is critical for diagnosis.
*Schizophrenia*
- Schizophrenia involves **continuous psychotic symptoms** without prominent mood episodes dominating the clinical picture.
- This patient has **prominent manic symptoms** (decreased sleep, grandiose behavior, agitation) that are central to the current presentation, making schizophrenia less likely.
- The presence of full mood episodes that occupy a **substantial portion** of the illness duration favors schizoaffective disorder over schizophrenia.
*Brief psychotic disorder*
- Brief psychotic disorder involves psychotic symptoms lasting **<1 month** with full return to baseline functioning.
- This patient has a **recurrent course** with hospitalization 1 year ago, indicating a chronic/recurring condition rather than a brief, self-limited episode.
*Schizotypal disorder*
- This is a **personality disorder** characterized by social deficits, cognitive/perceptual distortions, and eccentric behavior, but **NOT overt psychotic episodes**.
- Does not involve acute psychotic breaks with severe symptoms like hallucinations requiring hospitalization or manic episodes.
Negative symptoms US Medical PG Question 2: A 35-year-old woman comes to the physician accompanied by her husband after he started noticing strange behavior. He first noticed her talking to herself 8 months ago. For the past 6 months, she has refused to eat any packaged foods out of fear that the government is trying to poison her. She has no significant past medical history. She smoked marijuana in college but has not smoked any since. She appears restless. Mental status examination shows a flat affect. Her speech is clear, but her thought process is disorganized with many loose associations. The patient is diagnosed with schizophrenia and started on olanzapine. This patient is most likely to experience which of the following adverse effects?
- A. Dyslipidemia (Correct Answer)
- B. Diabetes insipidus
- C. Agranulocytosis
- D. Myoglobinuria
- E. Seizures
Negative symptoms Explanation: ***Dyslipidemia***
- **Olanzapine** is a **second-generation antipsychotic** commonly associated with significant **metabolic side effects**, including **weight gain**, **dyslipidemia**, and **insulin resistance**.
- These metabolic disturbances increase the risk of cardiovascular disease.
*Diabetes insipidus*
- This is a rare side effect, not typically associated with **olanzapine** or other **second-generation antipsychotics**.
- **Lithium** is an antimanic agent that can cause **nephrogenic diabetes insipidus**, but it is not relevant here.
*Agranulocytosis*
- While a serious side effect of some antipsychotics, **agranulocytosis** is most notably associated with **clozapine**,
- **Olanzapine** has a much lower risk of causing **agranulocytosis** compared to clozapine.
*Myoglobinuria*
- **Myoglobinuria** is associated with conditions like significant muscle damage (e.g., rhabdomyolysis).
- It is not a direct or common adverse effect of **olanzapine** therapy.
*Seizures*
- While some antipsychotics can lower the **seizure threshold**, **olanzapine** generally has a relatively low risk of inducing seizures.
- The risk is higher with certain other antipsychotics, particularly at high doses, or in patients with pre-existing seizure disorders.
Negative symptoms US Medical PG Question 3: A 28-year-old woman is brought into the clinic by her husband with concerns that she might be depressed. She delivered a healthy newborn a week and a half ago without any complications. Since then, she has been having trouble sleeping, eating poorly, and has stopped playing with the baby. The patient says she feels like she is drained all the time and feels guilty for not doing more for the baby. Which of the following is the best course of treatment for this patient?
- A. Reassurance
- B. Fluoxetine (Correct Answer)
- C. Risperidone
- D. Amitriptyline
- E. No treatment
Negative symptoms Explanation: ***Fluoxetine***
- This patient's symptoms (trouble sleeping, poor appetite, guilt, and anhedonia towards the baby) occurring 10 days postpartum are highly suggestive of **postpartum depression**. **SSRIs** like fluoxetine are first-line pharmacological treatments for this condition.
- Fluoxetine is a **selective serotonin reuptake inhibitor (SSRI)** that helps regulate mood by increasing serotonin levels in the brain. It is generally considered safe during breastfeeding, with a relatively low infant exposure compared to other antidepressants.
*Reassurance*
- Reassurance alone may be appropriate for **postpartum blues**, which are milder and self-limiting, typically resolving within two weeks.
- This patient's symptoms are more severe and persistent, lasting beyond typical postpartum blues and significantly impacting her functioning, indicating a need for more substantial intervention.
*Risperidone*
- Risperidone is an **atypical antipsychotic** primarily used to treat conditions like schizophrenia or bipolar disorder, or as an adjunct for severe refractory depression with psychotic features.
- There is no indication of psychosis in this patient's presentation, and the use of an antipsychotic would be disproportionate and carry unnecessary side effects.
*Amitriptyline*
- Amitriptyline is a **tricyclic antidepressant (TCA)**. While effective for depression, TCAs are generally not first-line due to a less favorable side effect profile (e.g., anticholinergic effects, cardiac conductivity issues) compared to SSRIs.
- SSRIs like fluoxetine are preferred for initial treatment of postpartum depression due to their better tolerability and safety profile.
*No treatment*
- This patient exhibits clear symptoms of **postpartum depression**, which is a serious condition that can worsen without intervention and impact both the mother's and infant's well-being.
- Untreated depression can lead to significant functional impairment, chronic suffering, and in severe cases, harm to oneself or the baby.
Negative symptoms US Medical PG Question 4: A 21-year-old man presents to the emergency room requesting surgery to remove "microchips," which he believes were implanted in his brain by "Russian spies" 6 months ago to control his thoughts. He also reports hearing the "spies" talk to each other through embedded "microspeakers." You notice that his hair appears unwashed and some of his clothes are on backward. Urine toxicology is negative for illicit drugs. Which of the following additional findings are you most likely to see in this patient during the course of his illness?
- A. Anhedonia, guilty rumination, and insomnia
- B. Grandiose delusions, racing thoughts, and pressured speech
- C. Asociality, flat affect, and alogia (Correct Answer)
- D. Amnesia, multiple personality states, and de-realization
- E. Intrusive thoughts, ritualized behaviors, and anxious mood
Negative symptoms Explanation: ***Asociality, flat affect, and alogia***
- This patient exhibits **delusions (persecutory, control)** and **auditory hallucinations**, classic positive symptoms of **schizophrenia**. The question asks about findings "during the course of his illness," which points to the **typical progression of schizophrenia**: patients initially present with **positive symptoms** (as seen in this case) and **over time develop negative symptoms** such as **asociality** (lack of motivation to engage in social interaction), **flat affect** (reduced emotional expression), and **alogia** (poverty of speech).
- The disorganized appearance (unwashed hair, clothes on backward) already demonstrates **disorganized behavior**, part of the schizophrenia spectrum. Negative symptoms typically emerge or worsen as the illness progresses, representing the most likely additional findings.
*Anhedonia, guilty rumination, and insomnia*
- While **anhedonia** and **insomnia** can be seen in schizophrenia, their presence alongside prominent **guilty rumination** would more strongly suggest a **depressive disorder with psychotic features**, rather than primary schizophrenia, especially with the patient's specific, classic psychotic symptoms.
- The primary symptoms described (delusions of control, auditory hallucinations) are more characteristic of primary psychotic disorders, and guilty rumination is not a typical feature of schizophrenia progression.
*Grandiose delusions, racing thoughts, and pressured speech*
- These symptoms are hallmark features of **mania** or a **manic episode with psychotic features**. While psychotic features can occur in bipolar disorder with mania, the patient's specific delusions of being controlled by spies and hearing voices discussing him are more typical of schizophrenia.
- The absence of information about elevated mood, increased energy, or decreased need for sleep also makes mania less likely compared to schizophrenia.
*Amnesia, multiple personality states, and de-realization*
- These symptoms are characteristic of **dissociative disorders**. **Amnesia** and **multiple personality states** (now known as identity alteration in dissociative identity disorder) involve disturbances in memory and identity.
- **De-realization** involves feelings of unreality regarding one's surroundings. None of these align with the patient's primary presentation of well-formed delusions and hallucinations characteristic of a psychotic disorder.
*Intrusive thoughts, ritualized behaviors, and anxious mood*
- These are core features of **obsessive-compulsive disorder (OCD)**. The patient's symptoms are clearly defined as delusions (fixed false beliefs) and hallucinations (perceptions without external stimuli), which are distinct from the ego-dystonic intrusive thoughts and ritualistic compulsions of OCD.
- While anxiety may be present in psychotic disorders, the primary presentation here is not dominated by OCD-like symptoms, and these would not be expected to develop as part of schizophrenia's natural course.
Negative symptoms US Medical PG Question 5: A 24-year-old man with a history of schizophrenia presents for follow-up. The patient says that he is still having paranoia and visual hallucinations on his latest atypical antipsychotic medication. Past medical history is significant for schizophrenia diagnosed 1 year ago that failed to be adequately controlled on 2 separate atypical antipsychotic medications. The patient is switched to a typical antipsychotic medication. Which of the following is the mechanism of action of the medication that was most likely prescribed for this patient?
- A. Dopaminergic receptor antagonist (Correct Answer)
- B. Dopaminergic partial agonist
- C. Serotonergic receptor agonist
- D. Serotonergic receptor antagonist
- E. Cholinergic receptor agonist
Negative symptoms Explanation: ***Dopaminergic receptor antagonist***
- The patient has **treatment-resistant schizophrenia**, indicated by failure to respond to two different atypical antipsychotics.
- Typical antipsychotics like **haloperidol** or **fluphenazine** are primarily **D2 dopamine receptor antagonists**, which may be used when a patient has not responded to atypical agents.
- The **primary mechanism** of typical (first-generation) antipsychotics is **potent D2 receptor blockade** in the mesolimbic pathway, which reduces positive symptoms of schizophrenia.
- Note: Clozapine would be the preferred choice for true treatment-resistant schizophrenia, but typical antipsychotics may still be considered in some clinical scenarios.
*Dopaminergic partial agonist*
- **Dopamine partial agonists**, such as **aripiprazole** or **brexpiprazole**, are **atypical antipsychotics** used for schizophrenia.
- The patient has failed to respond to atypical antipsychotics already, making it unlikely that another atypical agent would be the next choice.
- The question specifically states the patient is switched to a **typical antipsychotic**.
*Serotonergic receptor agonist*
- **Serotonin receptor agonists**, like LSD or psilocybin, are **not used** in the treatment of schizophrenia; they can, in fact, **induce psychotic symptoms**.
- While some antipsychotics modulate serotonin receptors, their therapeutic effect is not through agonism of these receptors.
*Serotonergic receptor antagonist*
- Many **atypical antipsychotics** have significant **serotonin 5-HT2A receptor antagonist** activity, in addition to D2 antagonism.
- However, the question states that the patient is being switched to a **typical antipsychotic**, whose primary and defining mechanism is **D2 antagonism**, not combined serotonin-dopamine antagonism.
*Cholinergic receptor agonist*
- **Cholinergic receptor agonists** are **not used** to treat schizophrenia and would likely worsen symptoms or cause significant side effects.
- These agents would have no therapeutic benefit in psychosis and are not part of the antipsychotic drug class.
Negative symptoms US Medical PG Question 6: A 23-year-old college student presents with his parents for a follow-up appointment. He was recently diagnosed with schizophrenia and was started on risperidone approx. 2 months ago. He reports a significant improvement since the start of treatment. His parents report that their son’s symptoms of delusions, hallucinations, and paranoid behavior have been ameliorated. On physical examination, the patient seems uncomfortable. He frequently fidgets and repeatedly crosses and uncrosses his legs. When asked if something is troubling him, he gets up and starts pacing. He says, “It’s always like this. I cannot sit still. It is frustrating.” What is the most likely diagnosis?
- A. Generalized anxiety disorder
- B. Tardive dyskinesia
- C. Ataxia
- D. Akathisia (Correct Answer)
- E. Restless legs syndrome
Negative symptoms Explanation: ***Akathisia***
- This patient presents with **motor restlessness** (fidgeting, pacing, inability to sit still) that emerged after starting an antipsychotic medication, risperidone. These are classic symptoms of **akathisia**, a medication side effect.
- The patient's verbalization, "I cannot sit still. It is frustrating," further supports the internal experience of restlessness characteristic of akathisia.
*Generalized anxiety disorder*
- While anxiety can cause restlessness, the specific description of physical agitation and the strong temporal relationship with starting a new antipsychotic make **akathisia** a more likely diagnosis.
- Generalized anxiety disorder typically involves chronic, excessive worry and is not primarily characterized by an irresistible urge to move.
*Tardive dyskinesia*
- Tardive dyskinesia involves **involuntary, repetitive body movements**, often in the face (e.g., grimacing, tongue protrusion) or limbs.
- It usually develops after **long-term use** of antipsychotics (months to years), whereas akathisia can occur shortly after initiation or dose changes.
*Ataxia*
- Ataxia refers to a lack of **voluntary coordination** of muscle movements, leading to an unsteady gait or impaired balance.
- The patient's symptoms are of restlessness and an uncontrollable urge to move, not a lack of coordination.
*Restless legs syndrome*
- Restless legs syndrome is characterized by an **uncomfortable sensation in the legs** with an urge to move them, typically worse at rest and relieved by movement.
- This patient's restlessness is more pervasive, involving whole-body agitation and an inability to simply sit still, not just an uncomfortable sensation primarily in the legs.
Negative symptoms US Medical PG Question 7: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Negative symptoms Explanation: ***Mesolimbic pathway***
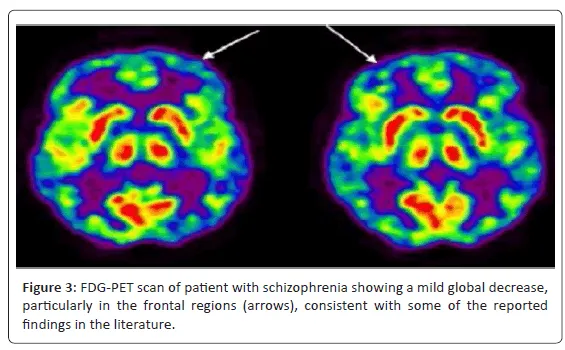
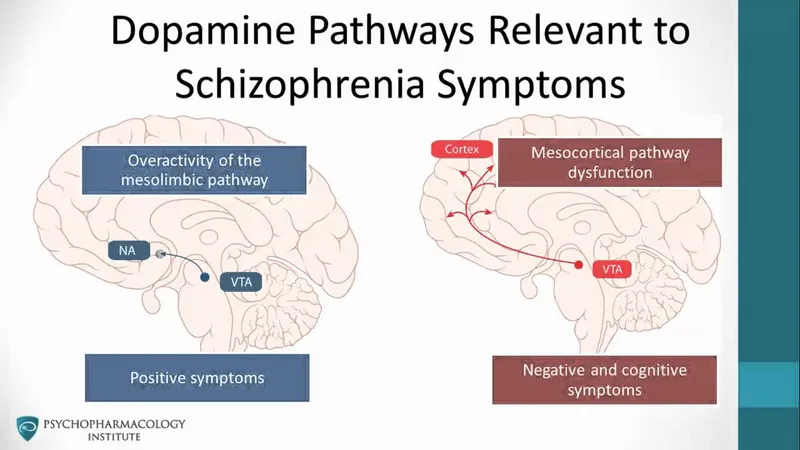
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Negative symptoms US Medical PG Question 8: A 23-year-old male presents to the emergency department. He was brought in by police for shouting on a subway. The patient claims that little people were trying to kill him, and he was acting within his rights to defend himself. The patient has a past medical history of marijuana and IV drug use as well as multiple suicide attempts. He is currently homeless. While in the ED, the patient is combative and refuses a physical exam. He is given IM haloperidol and diphenhydramine. The patient is transferred to the inpatient psychiatric unit and is continued on haloperidol throughout the next week. Though he is no longer aggressive, he is seen making "armor" out of paper plates and plastic silverware to defend himself. The patient is switched onto risperidone. The following week the patient is still seen gathering utensils, and muttering about people trying to harm him. The patient's risperidone is discontinued. Which of the following is the best next step in management?
- A. Olanzapine
- B. Thioridazine
- C. Clozapine (Correct Answer)
- D. Chlorpromazine
- E. Fluphenazine
Negative symptoms Explanation: ***Clozapine***
- This patient has demonstrated **treatment-resistant schizophrenia**, evidenced by persistent positive symptoms despite trials of haloperidol and risperidone, necessitating a trial of clozapine.
- **Clozapine** is an atypical antipsychotic that is uniquely effective for treatment-resistant schizophrenia, especially in patients with a history of **suicidality**.
*Olanzapine*
- While **olanzapine** is an effective atypical antipsychotic, it is generally considered a first-line or second-line agent, and this patient has already failed two antipsychotics (haloperidol and risperidone).
- Its efficacy in **treatment-resistant cases** is not superior to clozapine.
*Thioridazine*
- **Thioridazine** is a first-generation antipsychotic with a high risk of **QT prolongation** and other cardiac side effects, making it a less safe option.
- It is not typically reserved for **treatment-resistant schizophrenia** due to its side effect profile and lack of superior efficacy compared to newer agents.
*Chlorpromazine*
- **Chlorpromazine** is another first-generation antipsychotic that is not indicated for **treatment-resistant schizophrenia** at this stage.
- It carries significant anticholinergic and sedative side effects, similar to thioridazine, and is not significantly more effective than haloperidol for this indication.
*Fluphenazine*
- **Fluphenazine** is a potent first-generation antipsychotic, often available as a **depot injection** for adherence issues.
- However, it is not considered the best next step for **treatment-resistant schizophrenia** after failure of two different classes of antipsychotics.
Negative symptoms US Medical PG Question 9: A 23-year-old woman is brought to the physician by her father because of irritability, mood swings, and difficulty sleeping over the past 10 days. A few days ago, she quit her job and spent all of her savings on supplies for a “genius business plan.” She has been energetic despite sleeping only 1–2 hours each night. She was diagnosed with major depressive disorder 2 years ago. Mental status examination shows pressured speech, a labile affect, and flight of ideas. Throughout the examination, she repeatedly states “I feel great, I don't need to be here.” Urine toxicology screening is negative. Which of the following is the most likely diagnosis?
- A. Schizoaffective disorder
- B. Bipolar disorder type II
- C. Bipolar disorder type I (Correct Answer)
- D. Delusional disorder
- E. Attention-deficit hyperactivity disorder
Negative symptoms Explanation: ***Bipolar disorder type I***
- The patient's presentation of lasting **elevated mood**, decreased need for sleep, increased energy, pressured speech, flight of ideas, and impulsive behavior (quitting job, spending savings) are hallmark symptoms of a **manic episode**.
- A diagnosis of **Bipolar I Disorder** requires the occurrence of at least one manic episode, which is clearly evident here and distinguishes it from other mood disorders, especially given her prior history of major depressive disorder.
*Schizoaffective disorder*
- This disorder involves a period of illness during which there is an uninterrupted period of major mood episode (depressive or manic) concurrent with symptoms of **schizophrenia**, such as delusions or hallucinations, for at least 2 weeks in the absence of a major mood episode.
- The patient's symptoms are primarily mood-driven and do not include the characteristic psychotic features that persist independently of mood disturbances.
*Bipolar disorder type II*
- Bipolar II Disorder is characterized by at least one major depressive episode and at least one **hypomanic episode**.
- The patient's current symptoms, including significant impairment in social/occupational functioning, are indicative of a **manic episode**, not a hypomanic episode, which by definition does not cause marked impairment or require hospitalization.
*Delusional disorder*
- This disorder is characterized by the presence of **non-bizarre delusions** that last for at least one month, without other prominent psychotic symptoms or significant impairment in functioning.
- While the patient's "genius business plan" might seem delusional, her pervasive mood disturbance, flight of ideas, and significant functional impairment are not consistent with the primary features of delusional disorder.
*Attention-deficit hyperactivity disorder*
- ADHD is characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development, often presenting in childhood.
- While there is some overlap in symptoms like impulsivity and difficulty sleeping, the episodic nature, the extent of **mood disturbance**, grandiosity, and **pressured speech** are more characteristic of a manic episode than ADHD.
Negative symptoms US Medical PG Question 10: Choose the correctly matched pairs regarding the drugs used in schizophrenia:
1. D2 antagonism: Reduces positive symptoms
2. 5HT2A antagonism: Reduces negative symptoms
3. 5HT1A agonism: Weight loss
4. Muscarinic antagonism: Reduces extrapyramidal symptoms
- A. 1,4
- B. 1,2,4
- C. 1,2,3,4
- D. 1,2 (Correct Answer)
Negative symptoms Explanation: ***1,2***
- **D2 antagonism** is the primary mechanism by which antipsychotics reduce **positive symptoms** of schizophrenia, such as hallucinations and delusions.
- **5HT2A antagonism** is a key mechanism of atypical antipsychotics contributing to the reduction of **negative symptoms** (e.g., apathy, anhedonia, flat affect) and cognitive deficits, while also reducing the risk of extrapyramidal symptoms.
*1,2,3,4*
- This option is incorrect because **5HT1A agonism** is not associated with **weight loss**. While 5HT1A partial agonism (as seen with aripiprazole and brexpiprazole) may improve negative symptoms, anxiety, and cognitive function, it does not directly cause weight loss.
- Additionally, **muscarinic antagonism** does not reduce extrapyramidal symptoms as a primary mechanism. Rather, anticholinergic (muscarinic antagonist) drugs like benztropine are used to **treat** EPS after it occurs. The reduction of EPS in atypical antipsychotics primarily comes from 5HT2A antagonism and lower D2 binding affinity.
*1,2,4*
- This option is incorrect because **muscarinic antagonism** is not a mechanism that reduces EPS. Anticholinergic agents are used therapeutically to counteract EPS caused by dopamine blockade, but anticholinergic effects themselves do not prevent or reduce EPS.
- The reduction of EPS with atypical antipsychotics is mainly due to **5HT2A antagonism** balancing dopaminergic blockade, selective limbic over striatal binding, and fast D2 dissociation kinetics.
*1,4*
- This option is incorrect because it omits **5HT2A antagonism**, which is crucial for reducing **negative symptoms** in schizophrenia.
- It also incorrectly includes muscarinic antagonism as a mechanism that reduces EPS, when in reality anticholinergics are used to treat EPS rather than prevent it.
More Negative symptoms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.