Genetics of schizophrenia US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Genetics of schizophrenia. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Genetics of schizophrenia US Medical PG Question 1: A mother from rural Louisiana brings her 4-year-old son to a pediatrician. Her son is intellectually disabled, and she hopes that genetic testing will help determine the cause of her son's condition. She had previously been opposed to allowing physicians to treat her son, but his impulsive behavior and learning disabilities are making it difficult to manage his care on her own. On exam, the child has a long, thin face with a large jaw, protruding ears, and macroorchidism. The physician also hears a high-pitched holosystolic murmur at the apex of the heart that radiates to the axilla. Which of the following trinucleotide repeats is most likely affected in this individual?
- A. GAA on chromosome 9
- B. CGG on the sex chromosome X (Correct Answer)
- C. CTG on chromosome 19
- D. CTG on chromosome 8
- E. CAG on chromosome 4
Genetics of schizophrenia Explanation: ***CGG on the sex chromosome X***
- The constellation of **intellectual disability**, a **long, thin face with a large jaw**, **protruding ears**, and **macroorchidism** are classic features of **Fragile X syndrome**.
- Fragile X syndrome is caused by an expansion of the **CGG trinucleotide repeat** in the **FMR1 gene** on the **X chromosome**. The **high-pitched holosystolic murmur at the apex radiating to the axilla** suggests **mitral valve prolapse**, which is also frequently associated with Fragile X.
*GAA on chromosome 9*
- This describes the **GAA trinucleotide repeat expansion** associated with **Friedreich's ataxia**, affecting the **FXN gene** on **chromosome 9**.
- Friedreich's ataxia is characterized by **progressive ataxia**, **dysarthria**, and **loss of vibratory/proprioceptive sensation**, not macroorchidism or the specific facial features seen here.
*CTG on chromosome 19*
- This describes the **CTG trinucleotide repeat expansion** associated with **myotonic dystrophy type 1**, affecting the **DMPK gene** on **chromosome 19**.
- Myotonic dystrophy is characterized by **myotonia** (delayed muscle relaxation), **muscle weakness**, and **cataracts**, which are not consistently present in this case.
*CTG on chromosome 8*
- While **CTG repeats** are involved in some genetic conditions, the specific association with **chromosome 8** as a cause for the described symptoms (intellectual disability, specific facial features, macroorchidism, and mitral valve prolapse) is not a common trinucleotide repeat disorder.
- This option does not correspond to a recognized trinucleotide repeat disorder that presents with the given clinical picture.
*CAG on chromosome 4*
- This describes the **CAG trinucleotide repeat expansion** associated with **Huntington's disease**, affecting the **HTT gene** on **chromosome 4**.
- Huntington's disease typically presents with **chorea**, **psychiatric symptoms**, and **dementia** later in life, not with the childhood onset intellectual disability and physical features described.
Genetics of schizophrenia US Medical PG Question 2: A 5-year-old boy is brought to the clinic by his mother for an annual check-up. The family recently moved from Nebraska and is hoping to establish care. The patient is home schooled and mom is concerned about her son’s development. He is only able to say 2 to 3 word sentences and has been “behind on his alphabet." He always seems to be disinterested and "just seems to be behind.” The patient is observed to be focused on playing with his cars during the interview. Physical examination demonstrate a well-nourished child with poor eye contact, a prominent jaw, a single palmar crease, and bilaterally enlarged testicles. What is the most likely mechanism of this patient’s findings?
- A. CGG trinucleotide repeat expansion (Correct Answer)
- B. Microdeletion of the long arm of chromosome 7
- C. Meiotic nondisjunction of chromosome 21
- D. CTG trinucleotide repeat expansion
- E. Microdeletion of the short arm of chromosome 5
Genetics of schizophrenia Explanation: ***CGG trinucleotide repeat expansion***
- The patient presents with key features of **Fragile X Syndrome**: developmental delay ("behind on his alphabet," 2-3 word sentences), poor eye contact, prominent jaw, and **bilaterally enlarged testicles (macroorchidism)**.
- Fragile X Syndrome is caused by an expansion of a **CGG trinucleotide repeat** in the *FMR1* gene on the X chromosome.
*Microdeletion of the long arm of chromosome 7*
- This mechanism is associated with **Williams Syndrome**, characterized by elfin facies, an outgoing personality, and cardiovascular anomalies (especially supravalvular aortic stenosis).
- These features differ significantly from the patient's presentation; specifically, macroorchidism and poor eye contact are not typical of Williams Syndrome.
*Meiotic nondisjunction of chromosome 21*
- This leads to **Down Syndrome**, which presents with intellectual disability, distinctive facial features such as epicanthal folds and a flat nasal bridge, a single palmar crease, and hypotonia.
- While a single palmar crease is present in this patient, the prominent jaw, poor eye contact, and macroorchidism are not characteristic of Down Syndrome.
*CTG trinucleotide repeat expansion*
- A **CTG trinucleotide repeat expansion** is associated with **Myotonic Dystrophy**, a multisystem disorder characterized by myotonia, muscle wasting, cataracts, and frontal baldness.
- This condition typically presents with muscle weakness and myotonia, which are not described in the patient's symptoms, and does not cause macroorchidism or prominent jaw.
*Microdeletion of the short arm of chromosome 5*
- This microdeletion causes **Cri-du-chat syndrome**, characterized by a distinctive high-pitched cry resembling a cat's meow, microcephaly, intellectual disability, and widely spaced eyes.
- The patient's symptoms (e.g., prominent jaw, macroorchidism, no mention of a characteristic cry) do not align with the typical presentation of Cri-du-chat syndrome.
Genetics of schizophrenia US Medical PG Question 3: Two dizygotic twins present to the university clinic because they believe they are being poisoned through the school's cafeteria food. They have brought these concerns up in the past, but no other students or cafeteria staff support this belief. Both of them are average students with strong and weak subject areas as demonstrated by their course grade-books. They have no known medical conditions and are not known to abuse illicit substances. Which statement best describes the condition these patients have?
- A. A trial separation is likely to worsen symptoms.
- B. The disorder is its own disease entity in DSM-5.
- C. Antipsychotic medications are rarely beneficial.
- D. Can affect two or more closely related individuals. (Correct Answer)
- E. Cognitive behavioral therapy is a good first-line.
Genetics of schizophrenia Explanation: ***Can affect two or more closely related individuals.***
- The shared delusional belief in **folie à deux**, also known as **shared psychotic disorder**, typically occurs in two or more people who are closely associated.
- In this case, the **dizygotic twins** sharing the same delusional belief about being poisoned from cafeteria food fits this pattern.
*A trial separation is likely to worsen symptoms.*
- **Separating the individuals** involved in **folie à deux** is often a crucial step in treatment, as it can help break the cycle of shared delusion and allow for individual therapy.
- Separation typically IMPROVES rather than worsens symptoms by removing the reinforcement of the shared delusion.
*The disorder is its own disease entity in DSM-5.*
- In the **DSM-5**, **folie à deux** is no longer considered a separate diagnostic category.
- Instead, it is classified under **Other Specified Schizophrenia Spectrum and Other Psychotic Disorder** or **Unspecified Schizophrenia Spectrum and Other Psychotic Disorder**, with the specific context of shared delusion noted.
*Antipsychotic medications are rarely beneficial.*
- **Antipsychotics** are actually commonly used in treating folie à deux, particularly for the **primary individual** who initially developed the delusion.
- They can be an important component of treatment, often combined with separation and psychotherapy.
*Cognitive behavioral therapy is a good first-line.*
- **Cognitive Behavioral Therapy (CBT)** can be beneficial, particularly after separation, to help individuals challenge and reframe their delusional beliefs.
- However, the **first-line intervention** for shared psychotic disorder is **separation of the involved individuals**, followed by individual therapy (which may include CBT) and medication as needed.
Genetics of schizophrenia US Medical PG Question 4: A 23-year-old woman and her husband come to a genetic counselor because she is concerned about the chance of having an inherited defect if they had a child. Family history reveals no significant family history in her husband; however, her sister had a son who has seizures, failure to thrive, and neurodegeneration. She does not remember the name of the disease but remembers that her nephew had sparse, brittle hair that kinked in odd directions. She does not think that any other members of her family including her sister's husband have had this disorder. If this couple had a son, what is the most likely chance that he would have the same disorder that affected the patient's nephew?
- A. 100%
- B. 12.5%
- C. 25% (Correct Answer)
- D. 50%
- E. Close to 0%
Genetics of schizophrenia Explanation: ***25%***
- The nephew's symptoms of **seizures, failure to thrive, neurodegeneration**, and **sparse, brittle, kinky hair** are highly indicative of **Menkes disease**, an **X-linked recessive** disorder.
- Since the patient's sister had an affected son, the sister is an **obligate carrier** of the mutation.
- The patient and her sister share the same parents, so their mother must be a carrier (or have the mutation).
- The patient herself has a **50% chance of being a carrier**.
- **If the patient is a carrier**, each son has a **50% chance** of being affected.
- **Overall probability**: 0.5 (chance patient is carrier) × 0.5 (chance son inherits mutation) = **0.25 = 25%**.
*Close to 0%*
- This would only be correct if the patient had no chance of being a carrier, which is not the case given her family history.
- Her sister's affected son confirms the mutation is present in the maternal lineage.
*100%*
- This would only occur if the patient were definitely a carrier AND all male offspring inherited the mutation, or if the disorder were autosomal dominant with complete penetrance.
- For **X-linked recessive** disorders, even carrier mothers only pass the mutation to 50% of sons on average.
*12.5%*
- This percentage might represent additional generational steps or compound probabilities not relevant to this direct parent-child scenario.
- The correct calculation for this scenario is 50% × 50% = 25%.
*50%*
- This would be correct if we knew with certainty that the patient is a carrier.
- However, since we only know her sister is a carrier, the patient has a 50% chance of being a carrier herself, making the overall risk 25%.
- This is a common error in genetic counseling calculations—forgetting to account for the uncertain carrier status of the at-risk individual.
Genetics of schizophrenia US Medical PG Question 5: A 5-year-old boy is brought to the physician because of behavioral problems. His mother says that he has frequent angry outbursts and gets into fights with his classmates. He constantly complains of feeling hungry, even after eating a full meal. He has no siblings, and both of his parents are healthy. He is at the 25th percentile for height and is above the 95th percentile for weight. Physical examination shows central obesity, undescended testes, almond-shaped eyes, and a thin upper lip. Which of the following genetic changes is most likely associated with this patient's condition?
- A. Mitotic nondisjunction of chromosome 21
- B. Mutation of FBN-1 gene on chromosome 15
- C. Microdeletion of long arm of chromosome 7
- D. Loss of paternal gene expression on chromosome 15 (Correct Answer)
- E. Deletion of Phe508 on chromosome 7
Genetics of schizophrenia Explanation: ***Loss of paternal gene expression on chromosome 15***
- The patient's symptoms, including **hyperphagia**, **obesity**, behavioral issues, short stature, and **hypogonadism** (undescended testes), are characteristic of **Prader-Willi syndrome**.
- Prader-Willi syndrome is most commonly caused by the **loss of paternal gene expression** from the **q11-q13 region of chromosome 15**, either due to a paternal deletion, maternal uniparental disomy, or a defect in the imprinting center.
*Microdeletion of long arm of chromosome 7*
- A microdeletion on the long arm of chromosome 7 (7q11.23) is associated with **Williams syndrome**, characterized by an **elfin facial appearance**, supravalvular aortic stenosis, and intellectual disability.
- This does not match the patient's symptoms of obesity, hyperphagia, or hypogonadism.
*Deletion of Phe508 on chromosome 7*
- A deletion of phenylalanine at position 508 (**ΔF508**) on chromosome 7 is the most common mutation in the **cystic fibrosis transmembrane conductance regulator (CFTR)** gene, causing **cystic fibrosis**.
- Cystic fibrosis is an **autosomal recessive disorder** requiring mutations in both alleles (inherited from both parents), and primarily affects the exocrine glands, leading to lung disease, pancreatic insufficiency, and infertility, which are unrelated to the patient's presentation.
*Mutation of FBN-1 gene on chromosome 15*
- A mutation in the **FBN1 gene** on chromosome 15 (15q21.1) causes **Marfan syndrome**, which is a connective tissue disorder.
- Marfan syndrome presents with tall stature, long limbs (**arachnodactyly**), lens dislocation, and aortic root dilation, none of which are described in this patient.
*Mitotic nondisjunction of chromosome 21*
- Mitotic nondisjunction of chromosome 21 can lead to **mosaic Down syndrome**, but **trisomy 21** (due to meiotic nondisjunction) is the most common cause of Down syndrome.
- Down syndrome is associated with characteristic facial features, intellectual disability, and congenital heart defects, which are distinct from the symptoms presented.
Genetics of schizophrenia US Medical PG Question 6: A 29-year-old man comes to the physician with his wife because she has noticed a change in his behavior over the past 2 weeks. His wife reports that he is very distracted and irritable. His colleagues have voiced concerns that he has not been turning up for work regularly and behaves erratically when he does. Previously, her husband had been a reliable and reasonable person. The patient says that he feels “fantastic”; he only needs 4 hours of sleep each night and wakes up cheerful and full of energy each morning. He thinks that his wife is overreacting. The patient has been healthy except for a major depressive episode 5 years ago that was treated with paroxetine. He currently takes no medications. His pulse is 98/min, respirations are 12/min, and blood pressure is 128/62 mm Hg. Mental status examination shows frenzied speech and a flight of ideas. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Advanced paternal age
- B. Genetic predisposition (Correct Answer)
- C. Higher socioeconomic class
- D. Maternal obstetric complications
- E. Being married
Genetics of schizophrenia Explanation: ***Genetic predisposition***
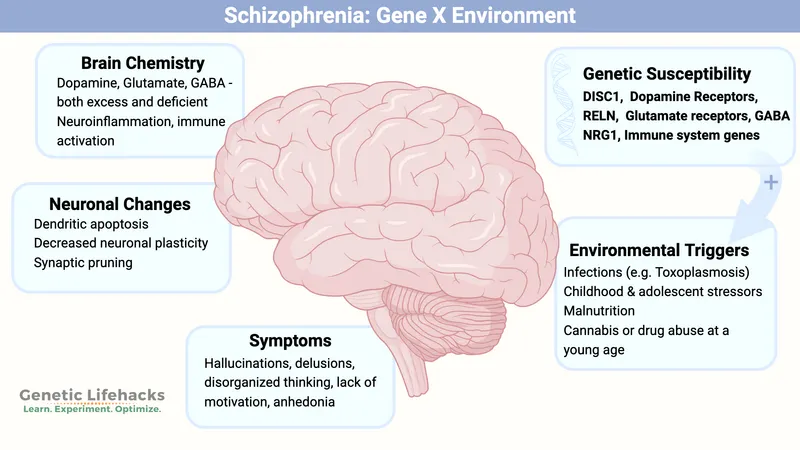
- A strong **genetic predisposition** is a primary predisposing factor for bipolar disorder, as evidenced by a significantly higher concordance rate in monozygotic twins compared to dizygotic twins or the general population.
- The patient's presentation with **manic symptoms** (decreased need for sleep, euphoria, irritability, frenzied speech, flight of ideas, erratic behavior) following a history of a **major depressive episode** is highly suggestive of **bipolar I disorder**.
*Advanced paternal age*
- While advanced paternal age has been associated with an increased risk of some neurodevelopmental disorders like **schizophrenia** and **autism spectrum disorder**, its link to bipolar disorder is less robust and not considered the strongest predisposing factor.
- The primary risk factor for bipolar disorder involves heritability rather than specific parental age.
*Higher socioeconomic class*
- There is **no consistent evidence** to suggest that higher socioeconomic class is a predisposing factor for bipolar disorder.
- Bipolar disorder affects individuals across all socioeconomic levels.
*Maternal obstetric complications*
- Maternal obstetric complications, such as **prenatal infections** or **hypoxia**, have been implicated in the development of certain psychiatric disorders, particularly **schizophrenia**.
- However, for bipolar disorder, genetic factors play a far more significant and direct role than obstetric complications.
*Being married*
- **Marital status** does not serve as a predisposing factor for the development of bipolar disorder.
- While relationship challenges can be a consequence or stressor for individuals with bipolar disorder, marriage itself is not a cause.
Genetics of schizophrenia US Medical PG Question 7: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Genetics of schizophrenia Explanation: ***Mesolimbic pathway***
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Genetics of schizophrenia US Medical PG Question 8: A 35-year-old nulligravid woman and her 33-year-old husband come to the physician for genetic counseling prior to conception. The husband has had severe psoriasis since adolescence that is now well-controlled under combination treatment with UV light therapy and etanercept. His father and two brothers also have this condition, and the couple wants to know how likely it is that their child will have psoriasis. The inheritance pattern of this patient's illness is most similar to which of the following conditions?
- A. Alport syndrome
- B. Schizophrenia (Correct Answer)
- C. Familial hypercholesterolemia
- D. Alpha thalassemia minor
- E. Oculocutaneous albinism
Genetics of schizophrenia Explanation: ***Schizophrenia***
- Psoriasis exhibits a **complex, multifactorial inheritance pattern**, influenced by multiple genes and environmental factors, similar to **schizophrenia**.
- No single gene dictates its expression, leading to variable penetrance and a risk that is higher in first-degree relatives but not Mendelian.
*Alport syndrome*
- This is an **X-linked dominant genetic disorder** primarily affecting the kidneys, ears, and eyes, characterized by a clear Mendelian inheritance pattern.
- The inheritance pattern in **Alport syndrome** is distinct and follows predictable ratios based on sex and parental genotypes.
*Familial hypercholesterolemia*
- This condition is inherited in an **autosomal dominant** manner, meaning a single copy of the mutated gene is sufficient to cause the disease, resulting in high penetrance.
- Its inheritance pattern is **monogenic** and follows a clear Mendelian 50% risk for offspring of an affected individual.
*Alpha thalassemia minor*
- This is an **autosomal recessive** condition, where affected individuals inherit two copies of the mutated gene (one from each parent).
- While it has a genetic basis, it is a **monogenic disorder** with a well-defined recessive inheritance, unlike the complex inheritance of psoriasis.
*Oculocutaneous albinism*
- This is typically an **autosomal recessive disorder** characterized by a significant reduction or absence of melanin production in the skin, hair, and eyes.
- Like alpha thalassemia minor, it is a **monogenic disorder** with a clear Mendelian recessive inheritance.
Genetics of schizophrenia US Medical PG Question 9: A 16-year-old boy is brought in to a psychiatrist's office by his mother for increasingly concerning erratic behavior. Her son has recently entered a new relationship, and he constantly voices beliefs that his girlfriend is cheating on him. He ended his last relationship after voicing the same beliefs about his last partner. During the visit, the patient reports that these beliefs are justified, since everyone at school is “out to get him.” He says that even his teachers are against him, based on their criticism of his schoolwork. His mother adds that her son has always held grudges against people and has always taken comments very personally. The patient has no psychiatric history and is in otherwise good health. What condition is this patient genetically predisposed for?
- A. Antisocial personality disorder
- B. Major depressive disorder
- C. Narcolepsy
- D. Substance use disorder
- E. Schizophrenia (Correct Answer)
Genetics of schizophrenia Explanation: ***Schizophrenia***
- The patient's symptoms of **pervasive distrust**, **suspiciousness**, beliefs that others are "out to get him," and taking comments personally are characteristic of **paranoid personality disorder**.
- **Paranoid personality disorder (PPD)** is considered part of the **schizotypal spectrum** or **cluster A personality disorders**, and individuals with PPD have a higher genetic predisposition to develop **schizophrenia** and other psychotic disorders.
*Antisocial personality disorder*
- This disorder is characterized by **disregard for and violation of the rights of others**, impulsivity, and lack of remorse, which are not the primary features described here.
- While individuals with this disorder may exhibit manipulative behavior, their core issue is not paranoid ideation but rather a pattern of social irresponsibility and law-breaking.
*Major depressive disorder*
- This condition is characterized by **persistent sadness**, loss of interest or pleasure, and other vegetative symptoms, which are not present in this patient's presentation.
- The patient's primary symptoms revolve around **paranoia and suspiciousness**, not mood disturbances.
*Narcolepsy*
- Narcolepsy is a **neurological condition** characterized by overwhelming daytime sleepiness and sudden attacks of sleep.
- This diagnosis is entirely unrelated to the patient's psychological symptoms of paranoia and distrust.
*Substance use disorder*
- While substance use can sometimes induce paranoid thinking, the patient's long-standing history of **grudges** and taking comments personally, even prior to potential substance exposure (implied by no psychiatric history mentioned for substance abuse), suggests a more ingrained personality trait rather than solely substance-induced paranoia.
- There is **no information provided about substance use**, making this a less likely primary condition or genetic predisposition.
Genetics of schizophrenia US Medical PG Question 10: A 25-year-old woman is brought to a psychiatrist's office by her husband who states that he is worried about her recent behavior, as it has become more violent. The patient's husband states that his family drove across the country to visit them and that his wife 'threatened his parents with a knife' at dinner last night. Police had to be called to calm her down. He states that she has been acting 'really crazy' for the last 9 months, and the initial behavior that caused him alarm was her admission that his deceased sister was talking to her through a decorative piece of ceramic art in the living room. Initially, he thought she was joking, but soon realized her complaints of 'hearing ghosts' talking to her throughout the house were persisting and 'getting worse'. Over the past 9 months, she has experienced multiple periods of profound sadness, with persistent insomnia and an unintentional weight loss of 12 pounds over several months. She has been complaining of feeling 'worthless' and has had markedly diminished interest in activities for much of this time period. Her general hygiene has also suffered from her recent lack of motivation and she insists that the 'ghosts' are asking her to kill as many people as she can so they won't be alone in the house. Her husband is extremely concerned that she may harm herself or someone else. He states that she currently does not take any medications or illicit drugs as far as he knows. She does not smoke or drink alcohol. The patient herself does not make eye contact or want to speak to the psychiatrist, allowing her husband to speak on her behalf. Which of the following is the most likely diagnosis in this patient?
- A. Schizophreniform disorder
- B. Schizophrenia
- C. Delusional disorder
- D. Schizoaffective disorder (Correct Answer)
- E. Brief psychotic disorder
Genetics of schizophrenia Explanation: ***Schizoaffective disorder***
- This patient exhibits symptoms of both a **major depressive disorder** (multiple periods of profound **sadness**, persistent **insomnia**, **weight loss** over several months, feelings of **worthlessness**, and markedly **diminished interest in activities**) and a **psychotic disorder** (auditory **hallucinations**, command hallucinations, **delusions**, violent behavior).
- The total symptom duration is **9 months**, with **mood symptoms present for the majority of this period**, meeting the key DSM-5 criterion for schizoaffective disorder.
- The patient also demonstrates **psychotic symptoms (hallucinations) that persist throughout**, including periods when mood symptoms may fluctuate, satisfying the requirement for delusions or hallucinations for ≥2 weeks in the absence of a major mood episode.
- The combination of prominent mood episodes concurrent with schizophrenia-spectrum symptoms, with mood symptoms present for the majority of the illness duration, confirms schizoaffective disorder.
*Schizophreniform disorder*
- This disorder involves symptoms characteristic of **schizophrenia** lasting **between 1 and 6 months**.
- The patient's symptoms have been present for **9 months**, exceeding the maximum duration for schizophreniform disorder.
*Schizophrenia*
- Schizophrenia requires persistent psychotic symptoms lasting **at least 6 months**, with at least one month of active-phase symptoms.
- While this patient has psychotic symptoms for 9 months, the **prominent and prolonged depressive symptoms** that are present for the **majority of the illness duration** distinguish this from schizophrenia.
- In schizophrenia, mood symptoms, if present, are **brief relative to the total duration** of the psychotic illness, which is not the case here.
*Delusional disorder*
- Delusional disorder is characterized by **non-bizarre delusions** for at least 1 month, without other prominent psychotic symptoms.
- This patient experiences prominent **auditory hallucinations** ("hearing ghosts," "deceased sister talking to her") and **command hallucinations**, which are not features of delusional disorder.
- The presence of hallucinations rules out this diagnosis.
*Brief psychotic disorder*
- This diagnosis involves sudden onset of psychotic symptoms lasting **more than 1 day but less than 1 month**, with eventual full recovery.
- The patient's symptoms have persisted for **9 months**, far exceeding the duration criterion for brief psychotic disorder.
More Genetics of schizophrenia US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.