Cognitive symptoms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cognitive symptoms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cognitive symptoms US Medical PG Question 1: A 23-year-old man presents to an outpatient psychiatrist complaining of anxiety and a persistent feeling that “something terrible will happen to my family.” He describes 1 year of vague, disturbing thoughts about his family members contracting a “horrible disease” or dying in an accident. He believes that he can prevent these outcomes by washing his hands of “the contaminants” any time that he touches something and by performing praying and counting rituals each time that he has unwanted, disturbing thoughts. The thoughts and rituals have become more frequent recently, making it impossible for him to work, and he expresses feeling deeply embarrassed by them. Which of the following is the most effective treatment for this patient's disorder?
- A. Psychodynamic psychotherapy and citalopram
- B. Cognitive behavioral therapy and haloperidol
- C. Cognitive behavioral therapy and clonazepam
- D. Cognitive behavioral therapy and fluoxetine (Correct Answer)
- E. Psychodynamic psychotherapy and aripiprazole
Cognitive symptoms Explanation: ***Cognitive behavioral therapy and fluoxetine***
- This patient presents with symptoms highly suggestive of **obsessive-compulsive disorder (OCD)**, characterized by intrusive, distressing thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed to neutralize the anxiety.
- **Cognitive Behavioral Therapy (CBT)**, specifically Exposure and Response Prevention (ERP), is the most effective psychotherapy for OCD, and **SSRIs** like fluoxetine are the first-line pharmacotherapy.
*Psychodynamic psychotherapy and citalopram*
- While citalopram (an SSRI) is an appropriate pharmacological treatment for OCD, **psychodynamic psychotherapy** is generally not considered first-line or most effective for OCD due to its focus on unconscious conflicts rather than direct symptom reduction.
- This approach may not provide the structured, symptom-focused interventions needed to manage obsessions and compulsions effectively.
*Cognitive behavioral therapy and haloperidol*
- **CBT** is an excellent choice, but **haloperidol**, an antipsychotic, is not a first-line treatment for OCD; it is primarily used for psychotic disorders or as an augmentation strategy in severe, treatment-resistant OCD, which is not indicated here.
- Using an antipsychotic as a primary treatment for OCD without a clear indication of psychosis or severe non-response to SSRIs is inappropriate and can lead to unnecessary side effects.
*Cognitive behavioral therapy and clonazepam*
- **CBT** is appropriate, but **clonazepam**, a benzodiazepine, is generally not recommended as a monotherapy or primary adjunctive treatment for OCD due to its *sedative side effects*, *potential for dependence*, and *lack of efficacy* in addressing the core symptoms of OCD.
- Benzodiazepines may be used for short-term anxiety relief but do not treat the underlying obsessive-compulsive processes.
*Psychodynamic psychotherapy and aripiprazole*
- **Psychodynamic psychotherapy** is not the most effective approach for OCD.
- **Aripiprazole**, an atypical antipsychotic, is typically used as an augmentation strategy for *treatment-resistant OCD* when initial SSRI trials have failed, not as a first-line medication, and this patient's case does not describe treatment resistance.
Cognitive symptoms US Medical PG Question 2: A 24-year-old man presents to the emergency department after a motor vehicle collision. He was in the front seat and unrestrained driver in a head on collision. His temperature is 99.2°F (37.3°C), blood pressure is 90/65 mmHg, pulse is 152/min, respirations are 16/min, and oxygen saturation is 100% on room air. Physical exam is notable for a young man who opens his eyes spontaneously and is looking around. He answers questions with inappropriate responses but discernible words. He withdraws from pain but does not have purposeful movement. Which of the following is this patient's Glasgow coma scale?
- A. 9
- B. 15
- C. 7
- D. 11 (Correct Answer)
- E. 13
Cognitive symptoms Explanation: ***11***
- **Eye-opening (E)**: The patient opens his eyes spontaneously, scoring **E4**.
- **Verbal response (V)**: He gives inappropriate responses but discernible words, scoring **V3**.
- **Motor response (M)**: He withdraws from pain but does not have purposeful movement, scoring **M4**.
- Therefore, the total Glasgow Coma Scale (GCS) score is **E4 + V3 + M4 = 11**.
*9*
- This score would imply a lower verbal or motor response, such as **incomprehensible sounds (V2)** or **abnormal flexion (M3)**, which is not consistent with the patient's presentation.
- For example, E4 + V2 + M3 would equal 9.
*15*
- A GCS of 15 indicates **normal neurological function**, meaning the patient would be fully oriented, obey commands, and open eyes spontaneously, which is not the case here.
- This score is for a patient who is fully conscious and responsive.
*7*
- A GCS of 7 suggests a **severe brain injury**, which would typically present with a much poorer response, such as **no verbal response (V1)** or **abnormal extension (M2)**.
- For example, E4 + V1 + M2 would equal 7.
*13*
- This score would mean a higher level of consciousness, such as **confused conversation (V4)** or **localizing pain (M5)**, which is better than the patient's described responses.
- For example, E4 + V4 + M5 would equal 13.
Cognitive symptoms US Medical PG Question 3: A 23-year-old woman is brought to the emergency department by her friend because of strange behavior. Two hours ago, she was at a night club where she got involved in a fight with the bartender. Her friend says that she was smoking a cigarette before she became irritable and combative. She repeatedly asked “Why are you pouring blood in my drink?” before hitting the bartender. She has no history of psychiatric illness. Her temperature is 38°C (100.4°F), pulse is 100/min, respirations are 19/min, and blood pressure is 158/95 mm Hg. Examination shows muscle rigidity. She has a reduced degree of facial expression. She has no recollection of her confrontation with the bartender. Which of the following is the most likely primary mechanism responsible for this patient's symptoms?
- A. Stimulation of cannabinoid receptors
- B. Inhibition of NMDA receptors (Correct Answer)
- C. Inhibition of norepinephrine, serotonin, and dopamine reuptake
- D. Stimulation of 5HT2A and dopamine D2 receptors
- E. Inhibition of dopamine D2 receptors
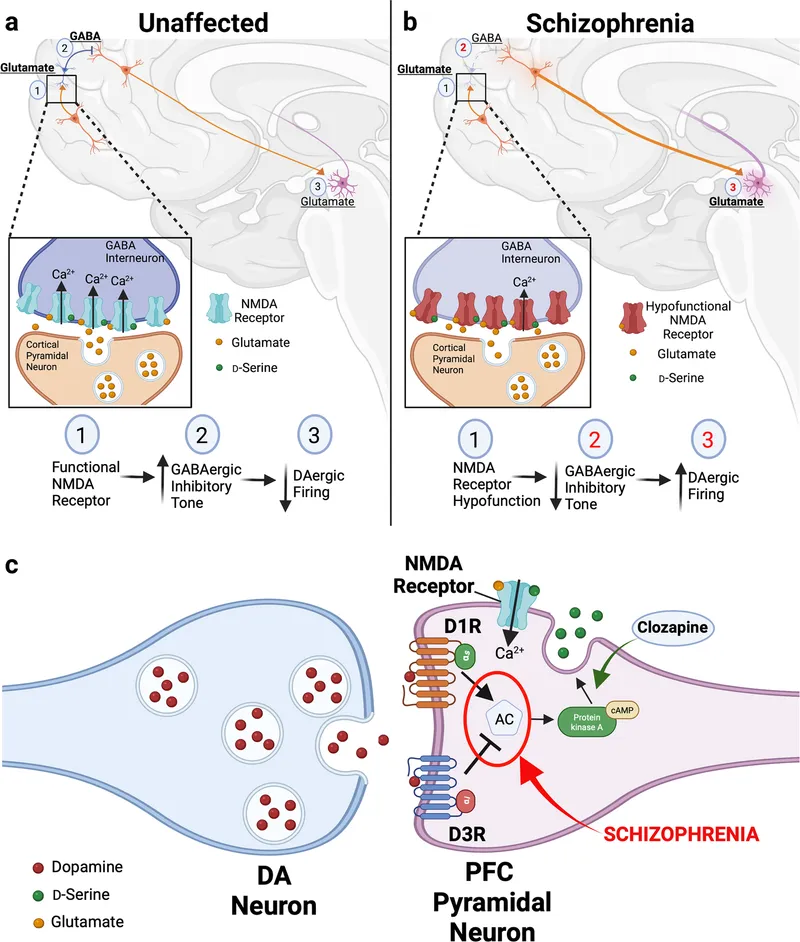
Cognitive symptoms Explanation: ***Inhibition of NMDA receptors***
- The patient's symptoms, including **combativeness**, **erratic behavior**, **delusions** ("Why are you pouring blood in my drink?"), **hypertension**, **tachycardia**, and **muscle rigidity**, are characteristic of **PCP intoxication**.
- **Phencyclidine (PCP)** acts primarily as an **NMDA receptor antagonist**, blocking calcium channels and leading to these neurotoxic effects.
*Stimulation of cannabinoid receptors*
- **Cannabis intoxication** typically involves **euphoria**, distorted perception, impaired memory, and increased appetite, which are not the primary features described here.
- While agitation can occur, the severe combativeness, delusions, and specific vital sign changes point away from cannabinoid receptor stimulation as the primary mechanism for this presentation.
*Inhibition of norepinephrine, serotonin, and dopamine reuptake*
- This mechanism is characteristic of stimulants like **cocaine** or **amphetamines**. While these drugs can cause agitation, paranoia, hypertension, and tachycardia, they typically do not cause the prominent **muscle rigidity** and **delusional thought** content as described.
- The "smoking a cigarette" context might suggest stimulants, but the overall clinical picture is more consistent with PCP.
*Stimulation of 5HT2A and dopamine D2 receptors*
- Stimulation of **5HT2A receptors** is associated with **hallucinogens** like LSD, causing perceptual distortions and altered consciousness, but typically not the intense combativeness, muscle rigidity, and specific delusions seen here.
- While **dopamine D2 receptor stimulation** can contribute to psychosis, it's not the primary mechanism that brings together all the described symptoms in this acute, severe presentation.
*Inhibition of dopamine D2 receptors*
- **Dopamine D2 receptor inhibition** is the mechanism of action for antipsychotic medications and generally leads to a reduction in psychotic symptoms, not the intense agitation, combativeness, and psychotic features observed in this patient.
- Such inhibition can lead to extrapyramidal symptoms, but not the acute, substance-induced presentation described.
Cognitive symptoms US Medical PG Question 4: A 60-year-old man is brought to the emergency department by police officers because he was acting strangely in public. The patient was found talking nonsensically to characters on cereal boxes in the store. Past medical history is significant for multiple hospitalizations for alcohol-related injuries and seizures. The patient’s vital signs are within normal limits. Physical examination shows a disheveled male who is oriented to person, but not time or place. Neurologic examination shows nystagmus and severe gait ataxia. A T1/T2 MRI is performed and demonstrates evidence of damage to the mammillary bodies. The patient is given the appropriate treatment for recovering most of his cognitive functions. However, significant short-term memory deficits persist. The patient remembers events from his past such as the school and college he attended, his current job, and the names of family members quite well. Which of the following is the most likely diagnosis in this patient?
- A. Schizophrenia
- B. Korsakoff's syndrome (Correct Answer)
- C. Wernicke encephalopathy
- D. Delirium
- E. Delirium tremens
Cognitive symptoms Explanation: ***Korsakoff's syndrome***
- The patient's history of **chronic alcohol abuse**, along with **gait ataxia**, **nystagmus**, and most notably, significant **anterograde amnesia** (inability to form new long-term memories) despite preserved remote memory, points to Korsakoff's syndrome.
- **Damage to the mammillary bodies** on MRI is a classic finding in Korsakoff's syndrome, a direct result of **thiamine deficiency**.
- The patient demonstrates the characteristic pattern: **impaired new memory formation** while retaining memories from his past (school, college, job, family names).
*Schizophrenia*
- Schizophrenia typically presents with **hallucinations and delusions** (e.g., talking to cereal box characters), but it is not commonly associated with physical signs like **nystagmus** or **gait ataxia**, nor with MRI findings of mammillary body damage.
- While the initial presentation of talking to cereal box characters might suggest psychosis, the complete clinical picture, especially the neurological deficits and persistent memory impairment, points away from schizophrenia as the primary diagnosis.
*Wernicke encephalopathy*
- Wernicke encephalopathy shares symptoms like **nystagmus** and **ataxia** with this patient and is also due to **thiamine deficiency** in alcoholics.
- However, Wernicke encephalopathy typically presents with more acute and severe symptoms, including **global confusion** and **ophthalmoplegia**, and represents the acute phase. The dominant chronic **anterograde amnesia** described here is characteristic of Korsakoff's syndrome, which represents the chronic sequela.
*Delirium*
- Delirium is characterized by an **acute disturbance in attention and cognition**, often with a fluctuating course, and can be seen in alcohol withdrawal.
- While the patient shows some disorientation, the chronic nature of the symptoms, the specific neurological deficits (nystagmus, ataxia), and particularly the persistent, isolated **anterograde amnesia** are not typical features of delirium.
*Delirium tremens*
- Delirium tremens is a severe form of **alcohol withdrawal** characterized by **autonomic hyperactivity**, severe delirium, hallucinations, and seizures.
- While the patient has a history of alcohol-related seizures, his current vital signs are normal, and the persistent, chronic memory deficits and specific MRI findings are not hallmarks of acute delirium tremens but rather a chronic neurological complication.
Cognitive symptoms US Medical PG Question 5: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Cognitive symptoms Explanation: ***Mesolimbic pathway***
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Cognitive symptoms US Medical PG Question 6: A 24-year-old woman is brought to the hospital by her mother because she has "not been herself" for the past 3 months. The patient says she hears voices in her head. The mother said that when she is talking to her daughter she can’t seem to make out what she is saying; it is as if her thoughts are disorganized. When talking with the patient, you notice a lack of energy and an apathetic affect. Which of the following is the most likely diagnosis for this patient?
- A. Major depressive disorder
- B. Schizophrenia
- C. Brief psychotic disorder
- D. Schizotypal disorder
- E. Schizophreniform disorder (Correct Answer)
Cognitive symptoms Explanation: ***Schizophreniform disorder***
- The patient exhibits core **psychotic symptoms** (hearing voices, disorganized thoughts) for a duration of **3 months**, which is characteristic of schizophreniform disorder (symptoms lasting **1 to 6 months**).
- Her **lack of energy** and **apathetic affect** align with the negative symptoms commonly seen in psychotic disorders.
*Major depressive disorder*
- While **lack of energy** and **apathetic affect** can be present, the prominent **hallucinations** (hearing voices) and **disorganized thoughts** are not primary features of major depressive disorder.
- A diagnosis of depression alone would not fully account for her psychotic symptoms.
*Schizophrenia*
- Schizophrenia requires symptoms to be present for **at least 6 months**, including at least one month of **active phase symptoms**. This patient's symptoms have only been present for 3 months.
- While the symptoms are consistent with schizophrenia, the **duration criterion** has not yet been met.
*Brief psychotic disorder*
- Brief psychotic disorder is characterized by psychotic symptoms lasting **less than 1 month**. This patient's symptoms have been ongoing for 3 months.
- The chronicity of symptoms makes this diagnosis unlikely.
*Schizotypal disorder*
- Schizotypal disorder is a **personality disorder** characterized by peculiar thoughts and behaviors, but typically **without overt psychotic episodes** or pronounced disorganized speech/hallucinations as described.
- While there may be odd beliefs or ideas of reference, the clear **auditory hallucinations** and **thought disorder** in this case point to a more severe psychotic condition.
Cognitive symptoms US Medical PG Question 7: A 75-year-old woman presents to her primary care physician with her son because she is convinced that people are stealing from her. Her son claims she has been misplacing her medications and money throughout the house. She recently lost her husband to old age and has become reclusive and no longer wants people to visit. Physical examination is unremarkable and the patient is oriented to person, time, and place. A mini-mental status examination (MMSE) is performed and she has difficulty recalling words after 5 minutes and also has problems with serial subtraction. Which of the following is the most likely diagnosis in this patient?
- A. Histrionic personality disorder
- B. Schizophrenia
- C. Delirium
- D. Schizoid personality disorder
- E. Dementia (Correct Answer)
Cognitive symptoms Explanation: ***Dementia***
- The patient has **primary cognitive impairment** evidenced by MMSE deficits (poor delayed recall, impaired serial subtraction) and functional decline (misplacing items).
- Her **delusions of theft are secondary to dementia**, a common behavioral and psychological symptom of dementia (BPSD), particularly in Alzheimer's disease.
- The **insidious onset** in a 75-year-old with progressive memory decline points to a neurodegenerative process.
- Orientation remains intact in early-to-moderate dementia, which doesn't rule out the diagnosis.
- The stressor (husband's death) may have unmasked or accelerated symptom recognition but doesn't explain the cognitive deficits.
*Histrionic personality disorder*
- Characterized by **excessive emotionality** and **attention-seeking behavior**, which are not evident in this presentation.
- Personality disorders are lifelong patterns, not new-onset conditions in elderly patients with cognitive decline.
- Does not explain the objective cognitive deficits on MMSE.
*Schizophrenia*
- Schizophrenia typically has onset in **late adolescence to early adulthood**, not at age 75.
- While late-onset schizophrenia exists, the **prominent cognitive impairment** (memory, executive function) as the PRIMARY feature points toward dementia rather than a primary psychotic disorder.
- Schizophrenia would show more pervasive psychotic symptoms without the specific pattern of memory and executive dysfunction seen here.
*Delirium*
- Delirium has **acute onset** (hours to days) with **fluctuating consciousness** and altered attention.
- This patient is **oriented to person, time, and place** and has a gradual, progressive course (misplacing items over time).
- No mention of acute medical illness, medication changes, or rapid cognitive fluctuation.
*Schizoid personality disorder*
- A lifelong pattern of **social detachment** and restricted emotional expression, not a new condition in late life.
- Does not explain the cognitive impairment, memory deficits, or delusional beliefs.
- The patient's reclusiveness is reactive to recent loss and concerns about theft, not a longstanding personality trait.
Cognitive symptoms US Medical PG Question 8: A 30-year-old computer scientist receives negative feedback on a recent project from his senior associate. He is told sternly that he must improve his performance on the next project. Later that day, he yells at his intern, a college student, for not showing enough initiative, though he had voiced only satisfaction with his performance up until this point. Which of the following psychological defense mechanisms is he demonstrating?
- A. Acting out
- B. Countertransference
- C. Projection
- D. Displacement (Correct Answer)
- E. Transference
Cognitive symptoms Explanation: ***Displacement***
- **Displacement** is a defense mechanism where a person redirects strong emotions, especially negative ones like anger, from the original source to a substitute target that is perceived as less threatening.
- The computer scientist's anger, initially generated by criticism from his senior associate, is redirected to his intern, who is a safer target.
*Acting out*
- **Acting out** involves expressing unconscious emotional conflicts or impulses through behavior, often inappropriate or destructive, rather than through words or feelings.
- While yelling at the intern is a behavior, the primary motive here is redirecting an emotion, not expressing a hidden conflict or impulse without awareness.
*Countertransference*
- **Countertransference** refers to the therapist's emotional reactions to a patient, rooted in their own unresolved conflicts, and is specific to the therapeutic relationship.
- This scenario involves an individual's reaction to workplace stress, not a dynamic within a therapeutic setting.
*Projection*
- **Projection** is attributing one's own unacceptable thoughts, feelings, or impulses to another person.
- In this case, the computer scientist isn't attributing his own poor performance or anger to the intern; rather, he is _redirecting_ his anger.
*Transference*
- **Transference** is the unconscious redirection of feelings and attitudes from a person in the past (e.g., a parent) to a person in the present (e.g., a therapist or boss).
- This scenario involves a direct reaction to a current stressor and redirection of emotion, not the reliving of past relationship dynamics with a new figure.
Cognitive symptoms US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Cognitive symptoms Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Cognitive symptoms US Medical PG Question 10: A 78-year-old man is brought to the physician by his daughter for a follow-up examination. The daughter noticed that he has gradually become more forgetful and withdrawn over the last year. He frequently misplaces his car keys and forgets the names of his neighbors, whom he has known for 30 years. He has difficulty recalling his address and telephone number. He recently had an episode of urinary and fecal incontinence. Last week, his neighbor found him wandering the parking lot of the grocery store. He has hypertension and hyperlipidemia. He had smoked one pack of cigarettes daily for 40 years but quit 18 years ago. His current medications include hydrochlorothiazide and atorvastatin. He appears healthy; BMI is 23 kg/m2. His temperature is 37.2°C (99.0°F), pulse is 86/min, respirations are 14/min, and blood pressure is 136/84 mm Hg. Mini-mental state examination score is 19/30. He is not bothered by his forgetfulness. Cranial nerves II–XII are intact. He has 5/5 strength and full sensation to light touch in all extremities. His patellar, Achilles, and biceps reflexes are 2+ bilaterally. His gait is steady. MRI scan of the brain shows ventriculomegaly and prominent cerebral sulci. Which of the following is the most appropriate pharmacotherapy?
- A. Acetazolamide
- B. Sertraline
- C. Memantine
- D. Thiamine
- E. Donepezil (Correct Answer)
Cognitive symptoms Explanation: ***Donepezil***
- The patient exhibits features consistent with **Alzheimer's disease**, including gradual memory loss, difficulty with daily tasks, episodes of incontinence, and a Mini-Mental State Examination (MMSE) score of 19/30. Donepezil, a **cholinesterase inhibitor**, is a first-line treatment for mild to moderate Alzheimer's to slow cognitive decline.
- The MRI findings of **ventriculomegaly and prominent cerebral sulci** are consistent with general cerebral atrophy often seen in Alzheimer's disease, not hydrocephalus requiring shunting or other specific brain pathologies (normal pressure hydrocephalus would have gait disturbance as a prominent feature, which is absent here).
*Acetazolamide*
- **Acetazolamide** is a **carbonic anhydrase inhibitor** used to treat conditions like glaucoma, altitude sickness, and idiopathic intracranial hypertension.
- There is no indication of elevated intracranial pressure or hydrocephalus that would warrant the use of acetazolamide in this patient.
*Sertraline*
- **Sertraline** is a **selective serotonin reuptake inhibitor (SSRI)** primarily used to treat depression, anxiety disorders, and obsessive-compulsive disorder.
- While depression can coexist with dementia, the primary cognitive symptoms described here are not primarily depressive; therefore, an antidepressant is not the most appropriate initial pharmacotherapy for cognitive decline.
*Memantine*
- **Memantine** is an **NMDA receptor antagonist** used in moderate to severe Alzheimer's disease, often in combination with cholinesterase inhibitors or when cholinesterase inhibitors are not tolerated.
- While appropriate for moderate to severe Alzheimer's, **cholinesterase inhibitors** are typically the initial treatment for mild to moderate stages, and the patient's MMSE score of 19/30 often falls into the mild-moderate category where donepezil is usually favored first.
*Thiamine*
- **Thiamine** (vitamin B1) supplementation is primarily used to treat **Wernicke-Korsakoff syndrome**, which is associated with chronic alcohol abuse and presents with ataxia, ophthalmoplegia, and confusion, none of which are the primary presenting symptoms here.
- There is no evidence of **nutritional deficiency** or alcohol abuse in this patient to suggest thiamine deficiency as the cause of his cognitive decline.
More Cognitive symptoms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.