Schizophrenia

On this page
🧠 The Schizophrenia Spectrum: Decoding Reality's Glitch
Schizophrenia disrupts the brain's ability to distinguish internal experience from external reality, affecting roughly 1% of the population yet remaining one of psychiatry's most misunderstood conditions. You'll explore how dopamine and glutamate dysregulation creates hallucinations and delusions, why motivation and emotion seem to vanish, and how cognitive deficits often prove more disabling than psychosis itself. By mastering the neurobiological underpinnings and evidence-based treatment algorithms, you'll gain the clinical framework to restore function and build recovery pathways for patients navigating this complex disorder.
📌 Remember: SCHIZOPHRENIA - Symptoms for 6+ months, Cognitive decline, Hallucinations, Impaired function, Zero medical cause, Organized delusions, Positive symptoms, Hearing voices, Reality testing lost, Emotional blunting, Negative symptoms, Insight absent, Affect flat
The disorder's complexity extends beyond symptom presentation to encompass genetic vulnerability (80% heritability), environmental triggers, and neurodevelopmental abnormalities. Early recognition becomes crucial, as 75% of individuals experience prodromal symptoms 2-5 years before full syndrome emergence.
| Symptom Domain | Prevalence | Onset Pattern | Treatment Response | Functional Impact | Neurobiological Basis |
|---|---|---|---|---|---|
| Positive Symptoms | 95% | Acute episodes | 70-80% respond | Moderate-severe | Dopamine hyperactivity |
| Negative Symptoms | 85% | Insidious onset | 30-40% respond | Severe disability | Prefrontal hypofunction |
| Cognitive Symptoms | 90% | Pre-illness decline | 20-30% respond | Greatest predictor | NMDA hypofunction |
| Disorganization | 60% | Variable pattern | 60-70% respond | Social impairment | Frontotemporal dysfunction |
- Epidemiological Patterns
- Global prevalence: 1.1% (range 0.7-1.4%)
- Lifetime risk: 0.7-0.8% across cultures
- Male-to-female ratio: 1.4:1 for early onset
- Males: Peak onset 18-25 years
- Females: Bimodal distribution 25-35 and 45-49 years
- Urban birth risk: 2.4x higher than rural
- Migration status: 2.9x increased risk in first-generation immigrants
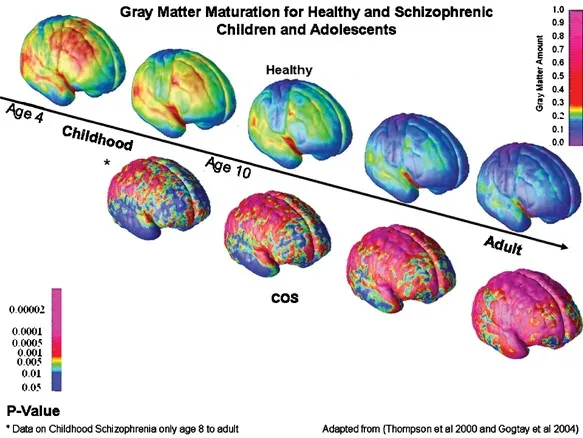
💡 Master This: Schizophrenia's neurodevelopmental hypothesis explains why cognitive deficits precede psychotic symptoms by years. Synaptic pruning abnormalities during adolescence unmask underlying vulnerabilities, with 40% gray matter reduction in prefrontal regions by first episode.
The diagnostic framework requires two or more positive, negative, or disorganization symptoms for ≥6 months, with significant functional decline. However, understanding the underlying neurobiological mechanisms transforms clinical recognition from symptom checklist to sophisticated pattern recognition of disrupted neural circuits.
Connect this foundational understanding through neurobiological mechanisms to understand how specific neurotransmitter disruptions create the complex symptom constellation that defines schizophrenia's clinical presentation.
🧠 The Schizophrenia Spectrum: Decoding Reality's Glitch
⚡ Neurochemical Command Center: The Dopamine-Glutamate Orchestra
📌 Remember: DOPAMINE PATHS - Dorsal striatum (motor), Orbital frontal (executive), Prefrontal cortex (cognitive), Anterior cingulate (emotional), Mesolimbic (reward), Insula (awareness), Nucleus accumbens (motivation), Emotional processing
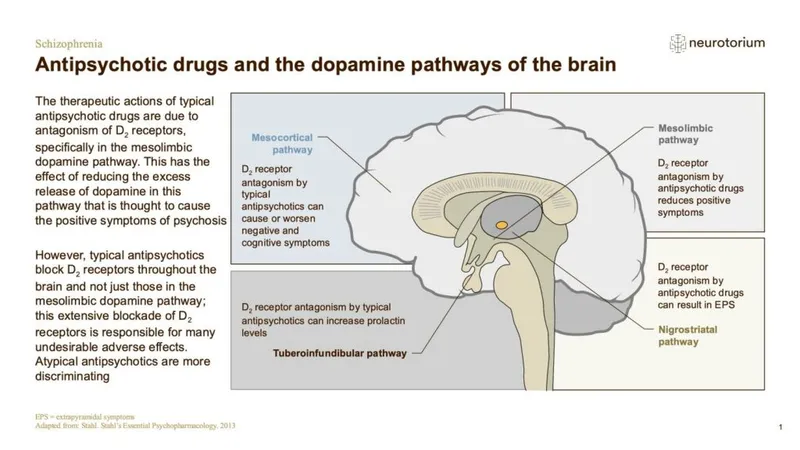
The revised dopamine hypothesis explains schizophrenia's paradoxical presentation: hyperactivity in mesolimbic pathways creates positive symptoms, while hypoactivity in mesocortical pathways produces negative and cognitive symptoms. This dual dysfunction occurs simultaneously, explaining why traditional antipsychotics targeting all dopamine receptors often worsen negative symptoms.
| Neurotransmitter System | Primary Dysfunction | Symptom Domain | Receptor Subtype | Treatment Target | Clinical Evidence |
|---|---|---|---|---|---|
| Dopamine | Mesolimbic hyperactivity | Positive symptoms | D2/D3 receptors | Antipsychotic blockade | 70-80% response rate |
| Dopamine | Mesocortical hypoactivity | Negative/cognitive | D1 receptors | Partial agonism | 30-40% improvement |
| Glutamate | NMDA hypofunction | All domains | NMDA receptors | Glycine transport inhibition | 20-30% cognitive benefit |
| GABA | Interneuron dysfunction | Gamma oscillations | GABA-A receptors | Positive allosteric modulators | Research phase |
| Acetylcholine | α7 nicotinic deficiency | Cognitive symptoms | α7 nAChR | Receptor agonists | 15-25% cognitive improvement |
- Dopamine Circuit Dysfunction
- Mesolimbic pathway (ventral tegmental area → nucleus accumbens)
- Hyperactivity: Creates positive symptoms
- D2 receptor density: ↑15-20% in psychosis
- Dopamine release: ↑300-400% during acute episodes
- Mesocortical pathway (VTA → prefrontal cortex)
- Hypoactivity: Produces negative/cognitive symptoms
- D1 receptor function: ↓30-40% in chronic illness
- Working memory correlation: r = 0.6-0.7 with D1 function
- Mesolimbic pathway (ventral tegmental area → nucleus accumbens)
💡 Master This: The glutamate-GABA-dopamine cascade explains schizophrenia's complexity. NMDA hypofunction → reduced GABA interneuron activity → glutamate disinhibition → downstream dopamine dysregulation. This cascade explains why NMDA enhancers show promise across all symptom domains.
Serotonin system involvement adds another layer of complexity, particularly the 5-HT2A receptor interaction with dopamine. Atypical antipsychotics leverage this interaction, with 5-HT2A antagonism modulating dopamine release and reducing extrapyramidal side effects by 60-70% compared to typical agents.
The cholinergic system contributes significantly to cognitive symptoms, with α7 nicotinic receptor dysfunction explaining the 90% smoking rate in schizophrenia patients. These receptors modulate gamma oscillations (30-80 Hz) essential for cognitive binding and working memory.
Connect these neurochemical disruptions through symptom manifestation to understand how specific neurotransmitter imbalances create the recognizable clinical patterns that guide diagnostic recognition and treatment selection.
⚡ Neurochemical Command Center: The Dopamine-Glutamate Orchestra
🎭 The Positive Symptom Theater: When Reality Becomes Fiction
📌 Remember: POSITIVE SYMPTOMS - Paranoid delusions, Organized hallucinations, Speech disorganized, Ideas of reference, Thought broadcasting, Insight impaired, Voices commanding, Eccentricity marked
Delusions affect 90% of schizophrenia patients and represent fixed false beliefs maintained despite contradictory evidence. Paranoid delusions occur in 65% of cases, followed by grandiose (25%), somatic (15%), and religious (20%) themes. The conviction strength typically reaches 8-10/10 on clinical scales, distinguishing true delusions from overvalued ideas.
- Delusion Classification and Prevalence
- Paranoid/Persecutory: 65% of patients
- Ideas of reference: 45% (neutral events have personal meaning)
- Surveillance beliefs: 40% (being watched/followed)
- Conspiracy theories: 35% (elaborate persecution plots)
- Grandiose delusions: 25% prevalence
- Special identity: Believing one is famous/important person
- Special powers: Supernatural or extraordinary abilities
- Special mission: Chosen for important task/purpose
- Somatic delusions: 15% prevalence
- Body dysmorphia: Grotesque physical changes
- Infestation: Parasites or foreign objects in body
- Medical conditions: Believing one has serious illness
- Paranoid/Persecutory: 65% of patients
⭐ Clinical Pearl: Auditory hallucinations occur in 75% of schizophrenia patients, with third-person commentary and command voices being most diagnostically specific. Visual hallucinations occur in only 15% and should prompt investigation for substance use or medical causes.
| Positive Symptom | Prevalence | Diagnostic Specificity | Treatment Response | Functional Impact | Neurobiological Correlate |
|---|---|---|---|---|---|
| Auditory Hallucinations | 75% | High for 3rd person | 80-85% improve | Moderate-severe | Superior temporal gyrus |
| Paranoid Delusions | 65% | Moderate specificity | 70-75% improve | Severe social impact | Amygdala hyperactivity |
| Thought Disorder | 50% | High specificity | 60-70% improve | Communication barrier | Left hemisphere language |
| Bizarre Behavior | 40% | Moderate specificity | 75-80% improve | Functional disability | Frontal-subcortical circuits |
| Visual Hallucinations | 15% | Low specificity | 85-90% improve | Variable impact | Occipital-temporal regions |
💡 Master This: Thought disorder severity correlates with functional outcome more strongly than hallucinations or delusions. Formal thought disorder affects 50% of patients and includes derailment, tangentiality, circumstantiality, and word salad in severe cases.
Disorganized speech represents the external manifestation of formal thought disorder, ranging from mild circumstantiality to complete incoherence. Poverty of content occurs when speech is adequate in amount but conveys little information, while pressure of speech may accompany grandiose delusions.
Insight impairment affects 85% of patients during acute episodes, with anosognosia (lack of illness awareness) being neurobiologically based rather than psychological denial. This impairment correlates with right hemisphere dysfunction and significantly impacts treatment adherence.
Connect these positive symptom patterns through negative symptom recognition to understand how schizophrenia's deficit syndrome creates equally important but more subtle clinical presentations that determine long-term functional outcomes.
🎭 The Positive Symptom Theater: When Reality Becomes Fiction
🌫️ The Great Absence: Negative Symptoms and the Vanishing Self
📌 Remember: THE 5 A's - Alogia (poverty of speech), Anhedonia (loss of pleasure), Avolition (lack of motivation), Affective flattening (emotional blunting), Asociality (social withdrawal)
Avolition represents the core negative symptom, affecting 70% of patients with moderate-to-severe intensity. This profound lack of motivation extends beyond simple laziness to encompass goal-directed behavior deficits, initiative loss, and persistent apathy that devastates occupational and social functioning.
- Negative Symptom Domains and Assessment
- Affective Flattening (75% prevalence)
- Facial expression: Reduced emotional responsiveness
- Vocal inflection: Monotonous, flat speech patterns
- Gesture reduction: Minimal spontaneous movement
- Eye contact: Poor social engagement patterns
- Alogia (60% prevalence)
- Poverty of speech: Reduced verbal output
- Poverty of content: Empty, uninformative speech
- Increased latency: Delayed responses to questions
- Blocking: Sudden speech interruptions
- Anhedonia (80% prevalence)
- Social anhedonia: Loss of interpersonal pleasure
- Physical anhedonia: Reduced sensory enjoyment
- Anticipatory deficits: Cannot imagine future pleasure
- Consummatory preservation: May enjoy activities when engaged
- Affective Flattening (75% prevalence)
⭐ Clinical Pearl: Primary negative symptoms must be distinguished from secondary causes including depression (40% comorbidity), medication side effects (extrapyramidal symptoms), and environmental deprivation. Primary negative symptoms persist despite optimal antipsychotic dosing and depression treatment.
| Negative Symptom | Prevalence | Functional Impact | Treatment Response | Assessment Scale | Neurobiological Basis |
|---|---|---|---|---|---|
| Anhedonia | 80% | Severe social disability | 20-30% improve | SANS, PANSS-N | Reward circuit dysfunction |
| Affective Flattening | 75% | Communication barrier | 25-35% improve | SANS, CAINS | Emotional processing deficits |
| Avolition | 70% | Occupational failure | 15-25% improve | CAINS, BNSS | Motivational circuit damage |
| Asociality | 65% | Social isolation | 30-40% improve | SANS, SDS | Social cognition impairment |
| Alogia | 60% | Interpersonal dysfunction | 35-45% improve | SANS, PANSS-N | Language network disruption |
💡 Master This: Negative symptoms emerge 2-5 years before positive symptoms during the prodromal phase and predict functional outcome more accurately than positive symptoms. Social functioning at 5-year follow-up correlates r = 0.7-0.8 with negative symptom severity at first episode.
Assessment challenges complicate negative symptom evaluation, as these symptoms overlap with depression (40% comorbidity), medication side effects, and social deprivation. The Clinical Assessment Interview for Negative Symptoms (CAINS) and Brief Negative Symptom Scale (BNSS) provide more precise measurement than older instruments.
Treatment resistance characterizes negative symptoms, with conventional antipsychotics often worsening these deficits through dopamine blockade in already hypoactive mesocortical pathways. Atypical antipsychotics show modest superiority (effect size 0.2-0.3), while adjunctive treatments targeting glutamate, GABA, and cholinergic systems show emerging promise.
The social cognition component of negative symptoms involves theory of mind deficits, emotion recognition impairment, and social perception abnormalities that compound the direct motivational and emotional deficits, creating cascading social disability.
Connect these negative symptom patterns through cognitive dysfunction recognition to understand how schizophrenia's neurocognitive deficits create the hidden disability that most powerfully predicts real-world functional outcomes.
🌫️ The Great Absence: Negative Symptoms and the Vanishing Self
🧩 The Cognitive Maze: Unraveling the Hidden Disability
📌 Remember: COGNITIVE DOMAINS - Working memory, Attention/vigilance, Verbal learning, Visual learning, Reasoning/problem solving, Speed of processing, Social cognition
Working memory deficits affect 85% of patients and represent the most severe cognitive impairment in schizophrenia. N-back task performance shows 40-50% reduction compared to healthy controls, with dorsolateral prefrontal cortex showing decreased activation during working memory challenges.
- Cognitive Domain Impairment Patterns
- Working Memory (85% affected)
- Spatial working memory: d = -1.2 effect size
- Verbal working memory: d = -1.0 effect size
- N-back performance: 40-50% below normal
- Digit span backward: 2-3 digits vs 5-6 normal
- Attention/Vigilance (80% affected)
- Sustained attention: d = -1.1 effect size
- Continuous performance: 25-30% more errors
- Vigilance decrement: Rapid deterioration over time
- Distractibility: Increased interference susceptibility
- Processing Speed (75% affected)
- Symbol coding: d = -1.3 effect size
- Trail making A: 50-60% slower completion
- Simple reaction time: 100-150ms delays
- Complex processing: Exponential slowing
- Working Memory (85% affected)
⭐ Clinical Pearl: Cognitive deficits precede psychotic symptoms by 2-5 years and remain stable throughout illness course, suggesting neurodevelopmental rather than neurodegenerative pathology. Premorbid IQ drops 8-10 points before first episode.
| Cognitive Domain | Effect Size | Prevalence | Functional Correlation | Treatment Response | Neural Substrate |
|---|---|---|---|---|---|
| Working Memory | d = -1.2 | 85% | r = 0.6-0.7 | Minimal | Dorsolateral PFC |
| Processing Speed | d = -1.3 | 75% | r = 0.5-0.6 | None | Frontoparietal networks |
| Attention/Vigilance | d = -1.1 | 80% | r = 0.4-0.5 | Minimal | Anterior cingulate |
| Verbal Learning | d = -1.0 | 70% | r = 0.5-0.6 | Minimal | Left temporal lobe |
| Executive Function | d = -0.9 | 75% | r = 0.6-0.7 | Minimal | Prefrontal cortex |
| Social Cognition | d = -1.1 | 80% | r = 0.7-0.8 | Moderate | Temporal-parietal junction |
💡 Master This: Gamma oscillations (30-80 Hz) generated by parvalbumin-positive interneurons are crucial for cognitive binding and working memory. NMDA receptor hypofunction disrupts these interneurons, explaining the cognitive-gamma-NMDA connection in schizophrenia pathophysiology.
Cognitive remediation therapy shows modest benefits (effect size 0.3-0.4) when combined with vocational rehabilitation, but pharmacological approaches remain largely ineffective. Cholinesterase inhibitors, AMPA receptor agonists, and glycine transport inhibitors show preliminary promise but lack definitive efficacy.
Metacognition deficits compound primary cognitive impairments, with patients showing poor insight into their cognitive limitations and overestimating their abilities. This metacognitive bias interferes with rehabilitation engagement and compensatory strategy development.
The cognitive reserve hypothesis suggests that higher premorbid IQ and educational attainment provide protective effects against functional decline, with each year of education associated with 10-15% better functional outcomes despite similar cognitive deficit severity.
Connect these cognitive dysfunction patterns through treatment algorithm development to understand how evidence-based interventions target specific symptom domains while managing the complex risk-benefit profiles of antipsychotic medications.
🧩 The Cognitive Maze: Unraveling the Hidden Disability
⚖️ Treatment Command Center: Evidence-Based Intervention Algorithms
First-episode psychosis represents a critical intervention window where early treatment within 3-6 months of symptom onset correlates with better long-term outcomes. Duration of untreated psychosis (DUP) exceeding 6 months predicts worse functional recovery and increased treatment resistance.
📌 Remember: TREATMENT PHASES - Acute stabilization (4-6 weeks), Stabilization phase (6 months), Maintenance therapy (indefinite), Recovery focus (psychosocial)
Antipsychotic selection follows evidence-based algorithms prioritizing efficacy, tolerability, and individual risk factors. Second-generation antipsychotics show equivalent efficacy to first-generation agents for positive symptoms but offer superior tolerability and modest advantages for negative symptoms and cognitive function.
- First-Line Antipsychotic Selection
- Aripiprazole (15-30mg daily)
- Mechanism: Partial D2/5-HT1A agonist
- Advantages: Low metabolic risk, minimal sedation
- Disadvantages: Akathisia (25%), activation
- Target population: Young adults, metabolic concerns
- Olanzapine (10-20mg daily)
- Mechanism: D2/5-HT2A/H1 antagonist
- Advantages: Rapid efficacy, mood stabilization
- Disadvantages: Weight gain (7-10kg), diabetes risk
- Target population: Severe symptoms, agitation
- Risperidone (4-8mg daily)
- Mechanism: D2/5-HT2A antagonist
- Advantages: Proven efficacy, available generically
- Disadvantages: Hyperprolactinemia, EPS at higher doses
- Target population: Cost considerations, compliance issues
- Aripiprazole (15-30mg daily)
⭐ Clinical Pearl: Clozapine remains the gold standard for treatment-resistant schizophrenia, defined as failure of 2+ adequate antipsychotic trials. Response rates reach 60-70% in treatment-resistant cases, but weekly monitoring for agranulocytosis (0.8% incidence) is mandatory.
| Antipsychotic | Efficacy Rating | Weight Gain Risk | Metabolic Risk | EPS Risk | Sedation Level | Prolactin Elevation |
|---|---|---|---|---|---|---|
| Aripiprazole | High | Low (+2kg) | Very Low | Low | Minimal | None |
| Olanzapine | Very High | Very High (+7kg) | High | Low | High | Moderate |
| Risperidone | High | Moderate (+4kg) | Moderate | Moderate | Moderate | High |
| Quetiapine | Moderate | Moderate (+3kg) | Moderate | Very Low | High | None |
| Clozapine | Highest | High (+6kg) | High | None | Very High | Low |
| Haloperidol | High | Low (+1kg) | Low | Very High | Low | High |
💡 Master This: Metabolic monitoring requires baseline and regular assessment of weight, glucose, lipids, and blood pressure. Olanzapine and clozapine carry highest metabolic risk, with diabetes incidence of 15-20% vs 5-7% with aripiprazole or ziprasidone.
Adjunctive treatments target specific symptom domains and side effect management. Antidepressants benefit comorbid depression (40% prevalence), while mood stabilizers may enhance negative symptom response. Cognitive enhancers remain investigational despite significant unmet need.
Treatment-resistant schizophrenia (TRS) affects 20-30% of patients and requires systematic approach including clozapine trial, combination strategies, and psychosocial interventions. Electroconvulsive therapy shows efficacy for catatonic features and treatment-resistant cases.
Connect these evidence-based treatment algorithms through comprehensive care integration to understand how psychosocial interventions, family support, and community resources create the recovery-oriented framework essential for optimal long-term outcomes.
⚖️ Treatment Command Center: Evidence-Based Intervention Algorithms
🌐 Recovery Architecture: Building Comprehensive Care Networks
Recovery-oriented care shifts focus from symptom management to functional restoration, quality of life enhancement, and personal goal achievement. This paradigm recognizes that clinical remission (symptom reduction) differs fundamentally from functional recovery (meaningful life participation), with only 20-30% achieving both simultaneously.

📌 Remember: RECOVERY PILLARS - Rehabilitation services, Education/vocational training, Cognitive behavioral therapy, Occupational therapy, Vocational rehabilitation, Exercise programs, Relapse prevention, Yearning for independence
Assertive Community Treatment (ACT) represents the gold standard for high-risk patients with frequent hospitalizations or poor treatment adherence. ACT teams provide 24/7 availability, in-vivo services, and low caseloads (10:1 patient-to-staff ratio), reducing hospitalization rates by 40-50% and improving housing stability by 60-70%.
- Evidence-Based Psychosocial Interventions
- Cognitive Behavioral Therapy (CBT) for psychosis
- Efficacy: Medium effect size (d = 0.4-0.5)
- Target symptoms: Delusions, hallucinations, negative symptoms
- Duration: 16-20 sessions over 6 months
- Mechanisms: Reality testing, coping strategies, relapse prevention
- Family Therapy/Education
- Relapse reduction: 50-60% decrease in 2-year relapse rates
- Family burden: Significant reduction in caregiver stress
- Components: Psychoeducation, communication training, problem-solving
- Duration: 9-12 months with booster sessions
- Social Skills Training
- Functional improvement: Moderate effect sizes (d = 0.5-0.6)
- Skill domains: Conversation, assertiveness, problem-solving
- Generalization: Enhanced with in-vivo practice
- Maintenance: Requires ongoing reinforcement
- Cognitive Behavioral Therapy (CBT) for psychosis
⭐ Clinical Pearl: Supported employment using Individual Placement and Support (IPS) model achieves competitive employment in 60-70% of participants vs 20-30% with traditional vocational rehabilitation. Rapid job search and ongoing support are key principles.
| Intervention Type | Target Population | Effect Size | Duration | Cost-Effectiveness | Evidence Level |
|---|---|---|---|---|---|
| ACT Teams | High-risk, frequent users | d = 0.7-0.8 | Ongoing | High (reduced hospitalizations) | Level 1 |
| CBT for Psychosis | Persistent symptoms | d = 0.4-0.5 | 6 months | Moderate | Level 1 |
| Family Therapy | High expressed emotion | d = 0.6-0.7 | 12 months | High (relapse prevention) | Level 1 |
| Supported Employment | Vocational goals | d = 0.8-1.0 | Ongoing | Very High | Level 1 |
| Cognitive Remediation | Cognitive deficits | d = 0.3-0.4 | 3-6 months | Moderate | Level 2 |
| Peer Support | All phases | d = 0.3-0.5 | Variable | High | Level 2 |
💡 Master This: Expressed emotion in families predicts relapse risk, with high criticism or emotional over-involvement increasing 9-month relapse rates from 25% to 65%. Family interventions targeting communication patterns and problem-solving skills significantly reduce this risk.
Peer support services leverage lived experience to provide hope, practical guidance, and role modeling for recovery. Peer specialists with personal recovery experience show unique effectiveness in engagement, treatment adherence, and community integration.
Technology-enhanced interventions include smartphone apps for medication reminders, symptom monitoring, and crisis intervention. Virtual reality shows promise for social skills training and cognitive rehabilitation, while telepsychiatry improves access in underserved areas.
Integrated dual diagnosis treatment addresses substance use disorders affecting 50% of schizophrenia patients. Motivational interviewing, contingency management, and dual diagnosis groups show superior outcomes compared to parallel treatment approaches.
The recovery journey typically spans 5-10 years with multiple phases including crisis stabilization, acute treatment, stabilization, rehabilitation, and recovery maintenance. Realistic expectations and long-term perspective are essential for sustained engagement and meaningful progress.
🌐 Recovery Architecture: Building Comprehensive Care Networks
Practice Questions: Schizophrenia
Test your understanding with these related questions
A 29-year-old woman is brought to the physician by her father because of a change in her behavior over the past 8 months. The father says that his daughter has become increasingly withdrawn; she has not answered any phone calls or visited her family and friends. The patient says that she has to stay at home because a foreign intelligence service is monitoring her. She thinks that they are using a magnetic field to read her mind. Mental status exam shows disjointed and perseverative thinking. She is anxious and has a flat affect. Which of the following is the most likely diagnosis?












