Schizoaffective disorder US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Schizoaffective disorder. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Schizoaffective disorder US Medical PG Question 1: A 23-year-old woman is brought to the emergency department by her boyfriend because of a 4-month history of feeling sad. Her boyfriend says that, during this period, she has slept and eaten very little and has been unable to focus at work. She says that she feels “empty inside” and has been hearing voices telling her that she is worthless. She first heard these voices 7 months ago when they started to make fun of her. She does not drink alcohol or use illicit drugs. Physical and neurological examinations show no abnormalities. On mental status examination, her speech is slow and monotonous; she abruptly stops talking in the middle of sentences and does not finish them. She occasionally directs her attention to the ceiling as if she were listening to someone. Which of the following is the most likely diagnosis?
- A. Schizophreniform disorder
- B. Schizoaffective disorder (Correct Answer)
- C. Schizotypal personality disorder
- D. Mood disorder with psychotic features
- E. Schizophrenia
Schizoaffective disorder Explanation: ***Schizoaffective disorder***
- The patient presents with a **major depressive episode** (sadness, anhedonia, sleep and appetite disturbance, poor concentration, feelings of worthlessness) concurrent with **psychotic symptoms** (auditory hallucinations) for 4 months.
- A key diagnostic criterion for schizoaffective disorder is the presence of **psychotic symptoms for at least 2 weeks in the absence of a major mood episode**, which is met by the prolonged duration of voices starting 7 months ago, while the depressive symptoms have been present for 4 months.
*Schizophreniform disorder*
- This disorder involves a constellation of **psychotic symptoms** lasting at least 1 month but **less than 6 months**.
- While she has psychotic symptoms, the prominent and prolonged mood symptoms (sadness, anhedonia, changes in sleep/appetite) suggest a mood component beyond what is typically seen in schizophreniform disorder.
*Schizotypal personality disorder*
- Characterized by pervasive patterns of social and interpersonal deficits marked by **acute discomfort** with, and **reduced capacity for, close relationships**, as well as **cognitive or perceptual distortions** and eccentric behaviors.
- This diagnosis does not account for the prominent mood symptoms (major depressive episode) and the clear psychotic symptoms (persistent auditory hallucinations independent of mood state) described in the patient.
*Mood disorder with psychotic features*
- In a mood disorder with psychotic features, the **psychotic symptoms occur exclusively during the mood episodes**.
- The patient reported hearing voices "7 months ago," while her depressive symptoms started "4 months ago," indicating that the **psychotic features preceded and occurred independently of the major depressive episode** for at least a 3-month period.
*Schizophrenia*
- Schizophrenia requires at least **6 months of continuous signs of disturbance**, including at least 1 month of **active-phase symptoms** (delusions, hallucinations, disorganized speech, disorganized or catatonic behavior, negative symptoms).
- While the patient has psychotic symptoms for 7 months, the prominent and lengthy mood symptoms that occurred concurrently and independently of the psychosis point away from a primary diagnosis of schizophrenia.
Schizoaffective disorder US Medical PG Question 2: A 24-year-old man presents to the emergency department after a suicide attempt. He is admitted to the hospital and diagnosed with schizoaffective disorder. A review of medical records reveals a history of illicit drug use, particularly cocaine and amphetamines. He is started on aripiprazole, paroxetine, and trazodone. At the time of discharge, he appeared more coherent and with a marked improvement in positive symptoms of hallucinations and delusions but still with a flat effect. During the patient’s first follow-up visit, his mother reports he has become increasingly agitated and restless despite compliance with his medications. She reports that her son’s hallucinations and delusions have stopped and he does not have suicidal ideations, but he cannot sit still and continuously taps his feet, wiggles his fingers, and paces in his room. When asked if anything is troubling him, he stands up and paces around the room. He says, “I cannot sit still. Something is happening to me.” A urine drug screen is negative. What is the next best step in the management of this patient?
- A. Add propranolol (Correct Answer)
- B. Increase the aripiprazole dose
- C. Stop aripiprazole and switch to clozapine
- D. Add lithium
- E. Stop paroxetine
Schizoaffective disorder Explanation: ***Add propranolol***
- The patient's symptoms of **agitation**, **restlessness**, inability to sit still, **foot tapping**, and **finger wiggling** are highly suggestive of **akathisia**, a common extrapyramidal side effect of antipsychotic medications, particularly **aripiprazole**.
- **Beta-blockers**, such as **propranolol**, are the **first-line treatment** for akathisia due to their ability to provide symptomatic relief by reducing the adrenergic hyperactivity associated with this condition.
*Increase the aripiprazole dose*
- Increasing the dose of **aripiprazole** would likely **worsen** the akathisia, as it is a dose-dependent side effect of **antipsychotic medications**.
- The patient's positive symptoms are already controlled, so increasing the dose is not indicated and could cause more harm.
*Stop aripiprazole and switch to clozapine*
- While switching antipsychotics is an option for persistent side effects, abruptly stopping an effective medication like **aripiprazole** could lead to a **relapse of psychotic symptoms**.
- **Clozapine** is typically reserved for **treatment-resistant schizophrenia** and carries risks of severe side effects like **agranulocytosis**, making it an inappropriate first step for akathisia.
*Add lithium*
- **Lithium** is primarily used as a **mood stabilizer** for bipolar disorder and in augmenting antidepressants; it is not indicated for treating **akathisia**.
- While some cases of akathisia might be mistaken for mood episodes, the classic motor restlessness points to an **extrapyramidal side effect**.
*Stop paroxetine*
- **Paroxetine**, an **SSRI**, is less likely to cause severe akathisia compared to antipsychotics, and discontinuing it would not address the most probable cause of the patient's symptoms, which is the **aripiprazole**.
- Stopping the antidepressant could also exacerbate the patient's **mood symptoms**, given his history of **schizoaffective disorder** and prior suicide attempt.
Schizoaffective disorder US Medical PG Question 3: A 24-year-old man is brought to your emergency department under arrest by the local police. The patient was found naked at a busy intersection jumping up and down on top of a car. Interviewing the patient, you discover that he has not slept in 2 days because he does not feel tired. He reports hearing voices. The patient was previously hospitalized 1 year ago with auditory hallucinations, paranoia, and a normal mood. What is the most likely diagnosis?
- A. Schizophrenia
- B. Bipolar disorder
- C. Brief psychotic disorder
- D. Schizotypal disorder
- E. Schizoaffective disorder (Correct Answer)
Schizoaffective disorder Explanation: ***Schizoaffective disorder***
- This patient demonstrates the **hallmark feature** of schizoaffective disorder: **psychotic symptoms occurring both during AND independent of mood episodes**.
- **Current presentation**: Clear **manic episode** (decreased need for sleep, grandiose/disinhibited behavior, psychomotor agitation) with psychotic features (auditory hallucinations).
- **Previous hospitalization**: **Psychotic symptoms (hallucinations, paranoia) in the absence of a mood episode** ("normal mood"), requiring hospitalization for at least 2 weeks - this is the **key diagnostic criterion** for schizoaffective disorder.
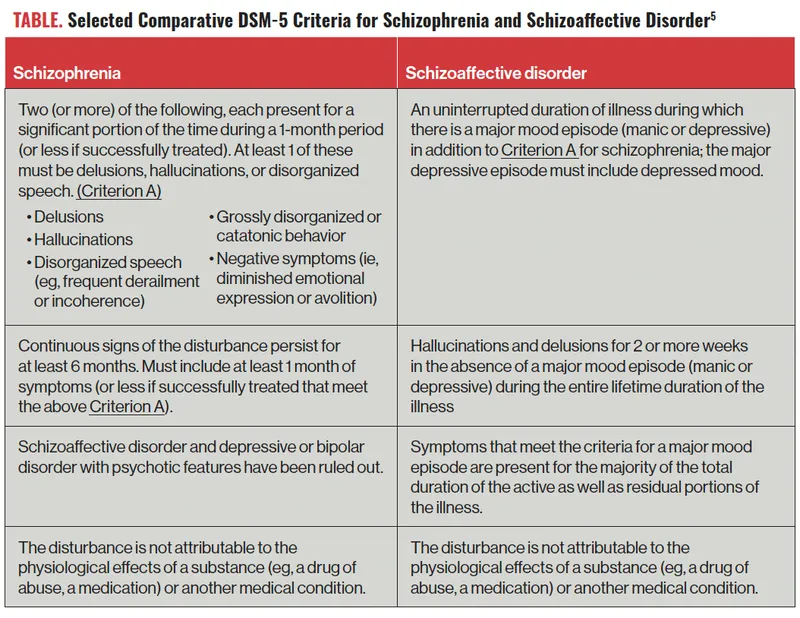
- The diagnosis requires an **uninterrupted period of illness** with both psychotic symptoms (meeting Criterion A for schizophrenia) and a major mood episode, PLUS psychotic symptoms for **≥2 weeks without prominent mood symptoms**.
*Bipolar disorder*
- In bipolar disorder with psychotic features, psychotic symptoms occur **exclusively during mood episodes** (manic, hypomanic, or depressive).
- This patient's previous hospitalization with psychosis but **"normal mood"** indicates psychotic symptoms independent of mood episodes, which **rules out** bipolar disorder and points to schizoaffective disorder.
- While the current presentation shows mania with psychosis, the longitudinal course is critical for diagnosis.
*Schizophrenia*
- Schizophrenia involves **continuous psychotic symptoms** without prominent mood episodes dominating the clinical picture.
- This patient has **prominent manic symptoms** (decreased sleep, grandiose behavior, agitation) that are central to the current presentation, making schizophrenia less likely.
- The presence of full mood episodes that occupy a **substantial portion** of the illness duration favors schizoaffective disorder over schizophrenia.
*Brief psychotic disorder*
- Brief psychotic disorder involves psychotic symptoms lasting **<1 month** with full return to baseline functioning.
- This patient has a **recurrent course** with hospitalization 1 year ago, indicating a chronic/recurring condition rather than a brief, self-limited episode.
*Schizotypal disorder*
- This is a **personality disorder** characterized by social deficits, cognitive/perceptual distortions, and eccentric behavior, but **NOT overt psychotic episodes**.
- Does not involve acute psychotic breaks with severe symptoms like hallucinations requiring hospitalization or manic episodes.
Schizoaffective disorder US Medical PG Question 4: A 57-year-old man is brought to the emergency department by the police after he was found running around a local park naked and screaming late at night. During intake, the patient talks non-stop about the government spying on him and his family, but provides little useful information besides his name and date of birth. Occasionally he refers to himself in the third person. He refuses to eat anything and will only drink clear fluids because he is afraid of being poisoned. A medical records search reveals that the patient has been treated for psychotic behavior and occasional bouts of severe depression for several years. Today, his heart rate is 90/min, respiratory rate is 19/min, blood pressure is 135/85 mm Hg, and temperature is 37.0°C (98.6°F). On physical exam, he appears gaunt and anxious. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. CMP, CBC, and TSH are normal. A urine toxicology test is negative. What is the most likely diagnosis?
- A. Schizophrenia
- B. Major depressive disorder
- C. Schizoaffective disorder (Correct Answer)
- D. Brief psychotic disorder
- E. Bipolar 1 disorder
Schizoaffective disorder Explanation: ***Schizoaffective disorder***
- The patient exhibits features of both a **mood disorder** (severe depression) and a **psychotic disorder** (delusions, disorganized behavior, referring to himself in the third person), which are key characteristics of schizoaffective disorder.
- The history of **psychotic behavior** and **severe depression** over several years, with current presentation involving both prominent mood symptoms (agitation, gaunt appearance suggesting poor self-care due to mood) and psychotic features (paranoia, disorganized speech), supports this diagnosis over other psychotic or mood disorders.
*Schizophrenia*
- While the patient exhibits **psychotic symptoms** (delusions, disorganization), the history of "occasional bouts of severe depression" suggests a more prominent and recurring mood component than typically seen in schizophrenia.
- In schizophrenia, mood symptoms are often confined to brief periods relative to the duration of the psychotic illness or are not a prominent and defining feature.
*Major depressive disorder*
- This diagnosis is incorrect because the patient displays clear and pervasive **psychotic symptoms** such as paranoia, disorganized speech, and bizarre behavior (running naked, screaming), which are beyond what is typically seen in major depressive disorder with psychotic features (where psychosis is congruent with the depressive theme).
- The historical pattern of **psychotic behavior** occurring separately from or alongside depressive episodes points away from a primary diagnosis of major depressive disorder.
*Brief psychotic disorder*
- This diagnosis is characterized by psychotic symptoms lasting **less than one month**, with an eventual full return to premorbid functioning.
- The patient's history of **several years** of psychotic behavior and severe depression rules out this acute and time-limited condition.
*Bipolar 1 disorder*
- While bipolar 1 disorder can feature **psychotic symptoms** during manic or depressive episodes, the presentation here emphasizes persistent psychotic features (delusions of being spied on, fear of poisoning) that are not always directly tied to mood episodes or are more enduring than typical for bipolar disorder.
- The long-standing history of both **psychotic and depressive episodes** suggests a more integrated condition of mood and psychosis rather than distinct episodes as seen in bipolar 1 disorder.
Schizoaffective disorder US Medical PG Question 5: A 28-year-old woman presents with continuous feelings of sadness and rejection. She says that over the past couple of weeks, she has been unable to concentrate on her job and has missed several days of work. She also has no interest in any activity and typically rejects invitations to go out with friends. She has no interest in food or playing with her dog. Her husband is concerned about this change in behavior. A few months ago, she was very outgoing and made many plans with her friends. She remembers being easily distracted and also had several ‘brilliant ideas’ on what she should be doing with her life. She did not sleep much during that week, but now all she wants to do is lie in bed all day. She denies any suicidal or homicidal ideations. She has no past medical history and has never been hospitalized. Laboratory tests were normal. Which of the following is the most likely diagnosis in this patient?
- A. Major depressive disorder
- B. Dysthymia
- C. Bipolar disorder, type II (Correct Answer)
- D. Schizoaffective disorder
- E. Bipolar disorder, type I
Schizoaffective disorder Explanation: ***Bipolar disorder, type II***
− This patient's current symptoms of profound **sadness, anhedonia, low energy, and social withdrawal** are indicative of a major depressive episode.
− The history of prior periods of **decreased need for sleep, brilliant ideas, and being easily distracted** suggests a hypomanic episode, a hallmark of bipolar disorder type II.
*Major depressive disorder*
− While the patient is currently experiencing a **major depressive episode**, the history of previous hypomanic symptoms rules out a diagnosis of unipolar major depressive disorder.
− **Major depressive disorder** does not include a history of manic or hypomanic episodes.
*Dysthymia*
− **Dysthymia** (persistent depressive disorder) is characterized by chronic, milder depressive symptoms lasting at least two years.
− The current episode is severe and marked by a clear change from a previous elevated mood state, which is inconsistent with dysthymia.
*Schizoaffective disorder*
− **Schizoaffective disorder** involves episodes of mood disturbance alongside symptoms of schizophrenia (e.g., hallucinations, delusions) that occur at least two weeks without prominent mood symptoms.
− This patient's symptoms are primarily mood-related and do not include psychotic features characteristic of schizophrenia.
*Bipolar disorder, type I*
− **Bipolar disorder type I** is characterized by the occurrence of at least one manic episode, which involves more severe symptoms, significant impairment, and often psychosis.
− The patient's previous "brilliant ideas" and decreased need for sleep describe a **hypomanic episode** rather than a full manic episode and are not associated with marked functional impairment or psychotic features.
Schizoaffective disorder US Medical PG Question 6: A 23-year-old woman is brought to the physician by her father because of irritability, mood swings, and difficulty sleeping over the past 10 days. A few days ago, she quit her job and spent all of her savings on supplies for a “genius business plan.” She has been energetic despite sleeping only 1–2 hours each night. She was diagnosed with major depressive disorder 2 years ago. Mental status examination shows pressured speech, a labile affect, and flight of ideas. Throughout the examination, she repeatedly states “I feel great, I don't need to be here.” Urine toxicology screening is negative. Which of the following is the most likely diagnosis?
- A. Schizoaffective disorder
- B. Bipolar disorder type II
- C. Bipolar disorder type I (Correct Answer)
- D. Delusional disorder
- E. Attention-deficit hyperactivity disorder
Schizoaffective disorder Explanation: ***Bipolar disorder type I***
- The patient's presentation of lasting **elevated mood**, decreased need for sleep, increased energy, pressured speech, flight of ideas, and impulsive behavior (quitting job, spending savings) are hallmark symptoms of a **manic episode**.
- A diagnosis of **Bipolar I Disorder** requires the occurrence of at least one manic episode, which is clearly evident here and distinguishes it from other mood disorders, especially given her prior history of major depressive disorder.
*Schizoaffective disorder*
- This disorder involves a period of illness during which there is an uninterrupted period of major mood episode (depressive or manic) concurrent with symptoms of **schizophrenia**, such as delusions or hallucinations, for at least 2 weeks in the absence of a major mood episode.
- The patient's symptoms are primarily mood-driven and do not include the characteristic psychotic features that persist independently of mood disturbances.
*Bipolar disorder type II*
- Bipolar II Disorder is characterized by at least one major depressive episode and at least one **hypomanic episode**.
- The patient's current symptoms, including significant impairment in social/occupational functioning, are indicative of a **manic episode**, not a hypomanic episode, which by definition does not cause marked impairment or require hospitalization.
*Delusional disorder*
- This disorder is characterized by the presence of **non-bizarre delusions** that last for at least one month, without other prominent psychotic symptoms or significant impairment in functioning.
- While the patient's "genius business plan" might seem delusional, her pervasive mood disturbance, flight of ideas, and significant functional impairment are not consistent with the primary features of delusional disorder.
*Attention-deficit hyperactivity disorder*
- ADHD is characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development, often presenting in childhood.
- While there is some overlap in symptoms like impulsivity and difficulty sleeping, the episodic nature, the extent of **mood disturbance**, grandiosity, and **pressured speech** are more characteristic of a manic episode than ADHD.
Schizoaffective disorder US Medical PG Question 7: A 27-year-old man is brought to the emergency department from a homeless shelter because of bizarre behavior. He avoids contact with others and has complained to the supervising staff that he thinks people are reading his mind. Three days ago, he unplugged every electrical appliance on his floor of the shelter because he believed they were being used to transmit messages about him to others. The patient has schizophrenia and has been prescribed risperidone but has been unable to comply with his medications because of his unstable living situation. He is disheveled and malodorous. His thought process is disorganized and he does not make eye contact. Which of the following is the most appropriate long-term pharmacotherapy?
- A. Intravenous propranolol
- B. Intramuscular benztropine
- C. Oral haloperidol
- D. Intramuscular risperidone (Correct Answer)
- E. Oral diazepam
Schizoaffective disorder Explanation: ***Intramuscular risperidone***
- Given the patient's **non-compliance** due to an unstable living situation, a **long-acting injectable antipsychotic** like intramuscular risperidone is the most appropriate choice for long-term management. This ensures consistent medication delivery regardless of daily adherence.
- This medication directly addresses the **positive symptoms of schizophrenia** (paranoia, disorganized thought) that are evident in the patient's bizarre behavior and delusional beliefs.
*Intravenous propranolol*
- Propranolol is a **beta-blocker** used to treat anxiety, hypertension, and tremors, but it is **not an antipsychotic** and does not address the core symptoms of schizophrenia.
- It could potentially be used for symptom control like akathisia if present, but not as primary long-term pharmacotherapy for psychosis.
*Intramuscular benztropine*
- Benztropine is an **anticholinergic medication** primarily used to treat **extrapyramidal symptoms (EPS)** induced by antipsychotics (e.g., dystonia, parkinsonism).
- It does not have antipsychotic effects and would not treat the patient's psychotic symptoms.
*Oral haloperidol*
- While haloperidol is an **effective antipsychotic**, it is an **oral formulation**. Given the patient's history of **non-compliance** with oral medication (risperidone), switching to another oral antipsychotic, even one as potent as haloperidol, is unlikely to solve the adherence issue, especially in an unstable living situation.
- Long-term management requires a strategy that overcomes the compliance barrier.
*Oral diazepam*
- Diazepam is a **benzodiazepine** primarily used for anxiety, sedation, and seizure control.
- It has **no antipsychotic properties** and would not treat the underlying psychotic symptoms of schizophrenia. It would only provide temporary sedation.
Schizoaffective disorder US Medical PG Question 8: A 27-year-old woman is brought to the office at the insistence of her fiancé to be evaluated for auditory hallucinations for the past 8 months. The patient’s fiancé tells the physician that the patient often mentions that she can hear her own thoughts speaking aloud to her. The hallucinations have occurred intermittently for at least 1-month periods. Past medical history is significant for hypertension. Her medications include lisinopril and a daily multivitamin both of which she frequently neglects. She lost her security job 7 months ago after failing to report to work on time. The patient’s vital signs include: blood pressure 132/82 mm Hg; pulse 72/min; respiratory rate 18/min, and temperature 36.7°C (98.1°F). On physical examination, the patient has a flat affect and her focus fluctuates from the window to the door. She is disheveled with a foul smell. She has difficulty focusing on the discussion and does not quite understand what is happening around her. A urine toxicology screen is negative. Which of the following is the correct diagnosis for this patient?
- A. Schizoaffective disorder
- B. Schizophrenia (Correct Answer)
- C. Schizoid personality disorder
- D. Schizophreniform disorder
- E. Schizotypal personality disorder
Schizoaffective disorder Explanation: ***Schizophrenia***
- The patient exhibits core symptoms of schizophrenia, including **auditory hallucinations** (hearing thoughts speaking aloud), **disorganized thinking** (difficulty focusing, fluctuating focus), and **negative symptoms** (flat affect, disheveled, foul smell, loss of job due to poor function). These symptoms have been present for **at least 6 months** (8 months of hallucinations, 7 months of job loss), which meets the diagnostic criteria.
- The duration of symptoms (over 6 months) differentiates it from schizophreniform disorder, and the absence of prominent mood episodes rules out schizoaffective disorder.
*Schizoaffective disorder*
- This diagnosis requires a **major mood episode** (depressive or manic) concurrent with Criterion A of schizophrenia, along with a period of **at least 2 weeks of delusions or hallucinations in the absence of prominent mood symptoms**.
- While the patient has some signs of distress (lost job, disorganized), a full major mood episode is not described, and the primary symptoms are clearly psychotic.
*Schizoid personality disorder*
- This is characterized by a pervasive pattern of **detachment from social relationships** and a restricted range of emotional expression, often appearing indifferent to praise or criticism.
- The patient's symptoms are primarily psychotic (hallucinations, disorganized thought), not just social withdrawal or emotional flatness. She doesn't necessarily avoid social contact, but her psychosis interferes with it.
*Schizophreniform disorder*
- This disorder presents with symptoms identical to schizophrenia but with a **duration of at least 1 month but less than 6 months**.
- The patient's symptoms, particularly the auditory hallucinations, have been present for 8 months and are therefore outside the timeframe for schizophreniform disorder.
*Schizotypal personality disorder*
- This disorder involves a pervasive pattern of **social and interpersonal deficits** marked by acute discomfort with, and reduced capacity for, close relationships, as well as **cognitive or perceptual distortions** and eccentric behaviors.
- While there may be some odd beliefs or magical thinking, **full-blown psychotic symptoms like prominent auditory hallucinations** (hearing thoughts speaking aloud) are generally not present as consistently or severely as seen in this patient, who meets criteria for a major psychotic disorder.
Schizoaffective disorder US Medical PG Question 9: A 25-year-old woman is brought to a psychiatrist's office by her husband who states that he is worried about her recent behavior, as it has become more violent. The patient's husband states that his family drove across the country to visit them and that his wife 'threatened his parents with a knife' at dinner last night. Police had to be called to calm her down. He states that she has been acting 'really crazy' for the last 9 months, and the initial behavior that caused him alarm was her admission that his deceased sister was talking to her through a decorative piece of ceramic art in the living room. Initially, he thought she was joking, but soon realized her complaints of 'hearing ghosts' talking to her throughout the house were persisting and 'getting worse'. Over the past 9 months, she has experienced multiple periods of profound sadness, with persistent insomnia and an unintentional weight loss of 12 pounds over several months. She has been complaining of feeling 'worthless' and has had markedly diminished interest in activities for much of this time period. Her general hygiene has also suffered from her recent lack of motivation and she insists that the 'ghosts' are asking her to kill as many people as she can so they won't be alone in the house. Her husband is extremely concerned that she may harm herself or someone else. He states that she currently does not take any medications or illicit drugs as far as he knows. She does not smoke or drink alcohol. The patient herself does not make eye contact or want to speak to the psychiatrist, allowing her husband to speak on her behalf. Which of the following is the most likely diagnosis in this patient?
- A. Schizophreniform disorder
- B. Schizophrenia
- C. Delusional disorder
- D. Schizoaffective disorder (Correct Answer)
- E. Brief psychotic disorder
Schizoaffective disorder Explanation: ***Schizoaffective disorder***
- This patient exhibits symptoms of both a **major depressive disorder** (multiple periods of profound **sadness**, persistent **insomnia**, **weight loss** over several months, feelings of **worthlessness**, and markedly **diminished interest in activities**) and a **psychotic disorder** (auditory **hallucinations**, command hallucinations, **delusions**, violent behavior).
- The total symptom duration is **9 months**, with **mood symptoms present for the majority of this period**, meeting the key DSM-5 criterion for schizoaffective disorder.
- The patient also demonstrates **psychotic symptoms (hallucinations) that persist throughout**, including periods when mood symptoms may fluctuate, satisfying the requirement for delusions or hallucinations for ≥2 weeks in the absence of a major mood episode.
- The combination of prominent mood episodes concurrent with schizophrenia-spectrum symptoms, with mood symptoms present for the majority of the illness duration, confirms schizoaffective disorder.
*Schizophreniform disorder*
- This disorder involves symptoms characteristic of **schizophrenia** lasting **between 1 and 6 months**.
- The patient's symptoms have been present for **9 months**, exceeding the maximum duration for schizophreniform disorder.
*Schizophrenia*
- Schizophrenia requires persistent psychotic symptoms lasting **at least 6 months**, with at least one month of active-phase symptoms.
- While this patient has psychotic symptoms for 9 months, the **prominent and prolonged depressive symptoms** that are present for the **majority of the illness duration** distinguish this from schizophrenia.
- In schizophrenia, mood symptoms, if present, are **brief relative to the total duration** of the psychotic illness, which is not the case here.
*Delusional disorder*
- Delusional disorder is characterized by **non-bizarre delusions** for at least 1 month, without other prominent psychotic symptoms.
- This patient experiences prominent **auditory hallucinations** ("hearing ghosts," "deceased sister talking to her") and **command hallucinations**, which are not features of delusional disorder.
- The presence of hallucinations rules out this diagnosis.
*Brief psychotic disorder*
- This diagnosis involves sudden onset of psychotic symptoms lasting **more than 1 day but less than 1 month**, with eventual full recovery.
- The patient's symptoms have persisted for **9 months**, far exceeding the duration criterion for brief psychotic disorder.
Schizoaffective disorder US Medical PG Question 10: A 21-year-old man presents to an outpatient psychiatrist with chief complaints of fatigue and “hearing voices.” He describes multiple voices which sometimes call his name or say nonsensical things to him before he falls asleep at night. He occasionally awakes to see “strange people” in his room, which frighten him but then disappear. The patient is particularly worried by this because his uncle developed schizophrenia when he was in his 20s. The patient also thinks he had a seizure a few days ago, saying he suddenly fell to the ground without warning, though he remembers the episode and denied any abnormal movements during it. He is in his 3rd year of college and used to be a top student, but has been getting C and D grades over the last year, as he has had trouble concentrating and fallen asleep during exams numerous times. He denies changes in mood and has continued to sleep 8 hours per night and eat 3 meals per day recently. Which of the following medications will be most beneficial for this patient?
- A. Haloperidol
- B. Valproic acid
- C. Risperidone
- D. Modafinil (Correct Answer)
- E. Levetiracetam
Schizoaffective disorder Explanation: ***Modafinil***
- This patient presents with **narcolepsy**, characterized by the **classic tetrad**: excessive daytime sleepiness (falling asleep during exams), **cataplexy** (sudden fall without loss of consciousness or abnormal movements), **hypnagogic hallucinations** (hearing voices before sleep), and **hypnopompic hallucinations** (seeing people upon awakening).
- The hallucinations are **not true psychotic symptoms** but rather dream-like phenomena occurring at sleep-wake transitions, which are common in narcolepsy.
- **Modafinil** is a first-line **wakefulness-promoting agent** that treats the excessive daytime sleepiness and improves alertness, addressing the primary pathology.
- The patient's family history of schizophrenia is a red herring; his symptoms are explained by narcolepsy, not a primary psychotic disorder.
*Risperidone*
- Risperidone is an **atypical antipsychotic** used for schizophrenia and other psychotic disorders.
- This patient does **not have a primary psychotic disorder**—the hallucinations are hypnagogic/hypnopompic phenomena associated with narcolepsy, not true psychotic hallucinations.
- Using an antipsychotic would be inappropriate and could **worsen daytime sleepiness** due to sedating effects, exacerbating the patient's core problem.
*Haloperidol*
- Haloperidol is a **first-generation antipsychotic** with significant risk of **extrapyramidal side effects**.
- Like risperidone, it would be inappropriate here as the patient does not have a psychotic disorder, and it would worsen sedation and daytime sleepiness.
*Valproic acid*
- Valproic acid is a **mood stabilizer and anticonvulsant** used for bipolar disorder and seizure disorders.
- The described "seizure" event is actually **cataplexy** (preserved consciousness, no abnormal movements), not a true seizure, so an anticonvulsant is not indicated.
- It would not address the narcolepsy symptoms and can cause sedation.
*Levetiracetam*
- Levetiracetam is an **anticonvulsant** medication.
- The patient's description (remembering the episode, no abnormal movements) is inconsistent with a seizure and consistent with **cataplexy**, which is treated by addressing the underlying narcolepsy, not with anticonvulsants.
More Schizoaffective disorder US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.