Antipsychotic side effect management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antipsychotic side effect management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antipsychotic side effect management US Medical PG Question 1: A 19-year-old woman, accompanied by her parents, presents after a one-week history of abnormal behavior, delusions, and unusual aggression. She denies fever, seizures or illicit drug use. Family history is negative for psychiatric illnesses. She was started on risperidone and sent home with her parents. Three days later, she is brought to the emergency department with fever and confusion. She is not verbally responsive. At the hospital, her temperature is 39.8°C (103.6°F), the blood pressure is 100/60 mm Hg, the pulse rate is 102/min, and the respiratory rate is 16/min. She is extremely diaphoretic and appears stiff. She has spontaneous eye-opening but she is not verbally responsive and she is not following commands. Laboratory studies show:
Sodium 142 mmol/L
Potassium 5.0 mmol/L
Creatinine 1.8 mg/dl
Calcium 10.4 mg/dl
Creatine kinase 9800 U/L
White blood cells 14,500/mm3
Hemoglobin 12.9 g/dl
Platelets 175,000/mm3
Urinalysis shows protein 1+, hemoglobin 3+ with occasional leukocytes and no red blood casts. What is the best first step in the management of this condition?
- A. Paracetamol
- B. Dantrolene
- C. Intravenous hydration
- D. Switch risperidone to clozapine
- E. Stop risperidone (Correct Answer)
Antipsychotic side effect management Explanation: ***Stop risperidone***
- The patient's presentation with **fever, altered mental status, muscle rigidity**, and elevated **creatine kinase** after starting risperidone is highly suggestive of **neuroleptic malignant syndrome (NMS)**.
- The **first and most critical step** in managing NMS is to **immediately discontinue the offending antipsychotic medication**, as continuation can worsen the severe symptoms and increase mortality.
*Paracetamol*
- While the patient has a high fever (39.8°C), **paracetamol** (acetaminophen) alone is **insufficient** to address the underlying severe hyperthermia and other systemic effects of NMS.
- The fever in NMS is due to **muscle rigidity** and **dysregulation of the hypothalamic thermoregulatory center**, which requires more comprehensive management than antipyretics.
*Dantrolene*
- **Dantrolene** is a **muscle relaxant** often used in NMS to reduce muscle rigidity and hyperthermia by inhibiting calcium release from the sarcoplasmic reticulum.
- However, the **withdrawal of the causative agent** (risperidone) is always the **initial and most crucial management step** before or in conjunction with supportive medications like dantrolene or bromocriptine.
*Intravenous hydration*
- **Intravenous hydration** is an important **supportive measure** in NMS to manage dehydration, support renal function (due to potential **rhabdomyolysis** from elevated CK), and help with temperature regulation.
- While critical, it is **not the *first* step**; discontinuing the causative drug is paramount.
*Switch risperidone to clozapine*
- Switching to another antipsychotic, even clozapine, is **inappropriate** at this stage because the patient is experiencing a severe adverse reaction to an antipsychotic.
- Reintroducing another antipsychotic could **exacerbate NMS** or trigger a similar reaction, and the immediate priority is to stabilize the patient by removing the trigger.
Antipsychotic side effect management US Medical PG Question 2: A 45-year-old obese man is evaluated in a locked psychiatric facility. He was admitted to the unit after he was caught running through traffic naked while tearing out his hair. His urine toxicology screening was negative for illicit substances and after careful evaluation and additional history, provided by his parents, he was diagnosed with schizophrenia and was treated with aripiprazole. His symptoms did not improve after several dosage adjustments and he was placed on haloperidol, but this left him too lethargic and slow and he was placed on loxapine. After several dosage adjustments today, he is still quite confused. He describes giant spiders and robots that torture him in his room. He describes an incessant voice screaming at him to run away. He also strongly dislikes his current medication and would like to try something else. Which of the following is indicated in this patient?
- A. Haloperidol
- B. Olanzapine
- C. Chlorpromazine
- D. Fluphenazine
- E. Clozapine (Correct Answer)
Antipsychotic side effect management Explanation: ***Clozapine***
- This patient has **treatment-resistant schizophrenia**, indicated by a lack of response to multiple trials of antipsychotics, including aripiprazole (atypical), haloperidol (typical), and loxapine (atypical).
- **Clozapine** is the only antipsychotic proven effective for treatment-resistant schizophrenia, significantly reducing psychotic symptoms and suicidality.
*Haloperidol*
- Haloperidol is a **first-generation antipsychotic** that the patient has already tried and found to be too sedating and slow.
- Continuing with haloperidol would likely result in persistent side effects and inadequate symptom control given his prior negative experience.
*Olanzapine*
- Olanzapine is a **second-generation atypical antipsychotic**; however, it is not typically indicated as a first-line treatment for treatment-resistant schizophrenia after failure of multiple agents.
- While effective for schizophrenia, it would be less effective than clozapine in a patient who has failed several previous antipsychotic trials.
*Chlorpromazine*
- Chlorpromazine is a **first-generation antipsychotic** that carries a higher risk of sedation, extrapyramidal symptoms, and anticholinergic side effects.
- It is unlikely to be more effective than haloperidol, which the patient already found too sedating and slow, and would not be the preferred choice for treatment-resistant schizophrenia.
*Fluphenazine*
- Fluphenazine is a **first-generation antipsychotic** with potent dopamine D2 receptor blockade, often leading to significant extrapyramidal side effects.
- Like other first-generation antipsychotics, it is not indicated as the next step for treatment-resistant schizophrenia after failure of multiple trials.
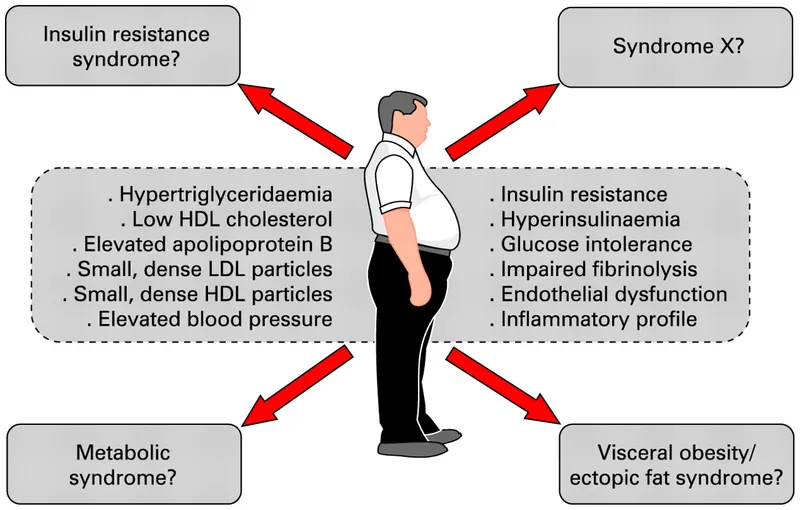
Antipsychotic side effect management US Medical PG Question 3: A study is conducted to investigate the relationship between the development of type 2 diabetes mellitus and the use of atypical antipsychotic medications in patients with schizophrenia. 300 patients who received the atypical antipsychotic clozapine and 300 patients who received the typical antipsychotic haloperidol in long-acting injectable form were followed for 2 years. At the end of the observation period, the incidence of type 2 diabetes mellitus was compared between the two groups. Receipt of clozapine was found to be associated with an increased risk of diabetes mellitus relative to haloperidol (RR = 1.43, 95% p<0.01).
Developed type 2 diabetes mellitus Did not develop type 2 diabetes mellitus
Clozapine 30 270
Haloperidol 21 279
Based on these results, what proportion of patients receiving clozapine would not have been diagnosed with type 2 diabetes mellitus if they had been taking a typical antipsychotic?
- A. 1.48
- B. 0.3 (Correct Answer)
- C. 0.43
- D. 0.03
- E. 33.3
Antipsychotic side effect management Explanation: ***0.3***
- The question asks for the **proportion of patients** receiving clozapine who *would not have been diagnosed* with type 2 diabetes if they had been taking a **typical antipsychotic (haloperidol)**. This is essentially asking for the **attributable risk proportion** among the exposed.
- First, calculate the **incidence of diabetes in the clozapine group**: 30/300 = 0.10. Then, calculate the **incidence of diabetes in the haloperidol group**: 21/300 = 0.07. The difference in incidence (attributable risk) is 0.10 - 0.07 = 0.03. To find the proportion among those exposed, divide this difference by the incidence in the clozapine group: 0.03 / 0.10 = **0.3**.
*1.48*
- This value is close to the **Relative Risk (RR)** of 1.43, which indicates how many times more likely the clozapine group is to develop diabetes compared to the haloperidol group. It does not represent the proportion of patients who would benefit from switching medications.
- The question asks for a proportion that reflects the prevention of diabetes, not a measure of relative risk.
*0.43*
- This value is close to the **attributable risk fraction** (attributable risk percent / 100), which is calculated as (RR - 1) / RR = (1.43 - 1) / 1.43 = 0.43 / 1.43 ≈ 0.30. It's not a direct proportion of patients.
- While related to the increased risk, 0.43 does not directly answer the question about the proportion of patients who would *not* have developed diabetes if they had taken haloperidol.
*0.03*
- This value represents the **absolute difference in risk (attributable risk)**: 0.10 (clozapine incidence) - 0.07 (haloperidol incidence) = 0.03.
- This is the difference in incidence, not the proportion of clozapine users who would avoid diabetes if they were on haloperidol. The question asks for a proportion *among* those receiving clozapine.
*33.3*
- This value is likely derived from incorrect calculations or misinterpretation of the question as an alternative percentage.
- It does not align with any standard epidemiological measure for comparing the impact of switching medications in the context of attributable risk or risk reduction.
Antipsychotic side effect management US Medical PG Question 4: A 44-year-old man presents to his psychiatrist for a follow-up appointment. He is currently being treated for schizophrenia. He states that he is doing well but has experienced some odd movement of his face recently. The patient's sister is with him and states that he has been more reclusive lately and holding what seems to be conversations despite nobody being in his room with him. She has not noticed improvement in his symptoms despite changes in his medications that the psychiatrist has made at the last 3 appointments. His temperature is 99.3°F (37.4°C), blood pressure is 157/88 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for rhythmic movements of the patient's mouth and tongue. Which of the following is a side effect of the next best step in management?
- A. Anxiolysis
- B. Dry mouth and dry eyes
- C. QT prolongation on EKG
- D. Infection (Correct Answer)
- E. Worsening of psychotic symptoms
Antipsychotic side effect management Explanation: ***Infection***
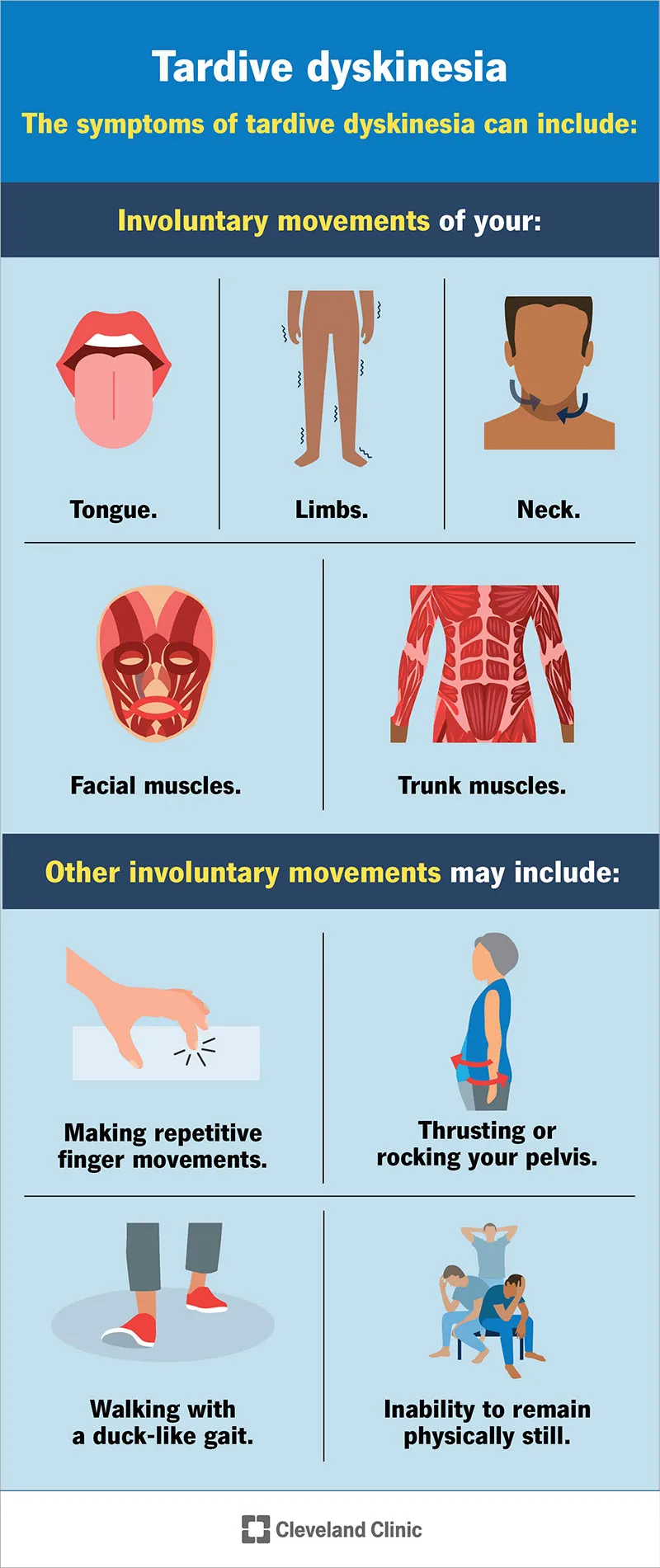
- The patient has **tardive dyskinesia** and **persistent psychotic symptoms** despite changes in medications. The next best step is to switch to **clozapine**.
- **Clozapine** can cause **agranulocytosis**, which increases the risk of serious infections and requires regular monitoring of white blood cell counts.
*Anxiolysis*
- While some antipsychotics can have anxiolytic effects, it is not the primary side effect or the most concerning one for the "next best step" in this context.
- The patient's primary issues are persistent psychosis and tardive dyskinesia, not anxiety that would be specifically targeted as the main side effect.
*Dry mouth and dry eyes*
- These are common **anticholinergic side effects** associated with many antipsychotics, including clozapine, but they are generally less severe and life-threatening compared to the risk of agranulocytosis.
- While unpleasant, they are not the most significant or defining side effect of the "next best step" in managing this patient's complex presentation.
*QT prolongation on EKG*
- **QT prolongation** is a known cardiac side effect of several antipsychotics, including clozapine.
- However, the risk of **agranulocytosis** with **clozapine** is arguably the most critical and distinct side effect requiring stringent monitoring, making it the "next best step" related answer.
*Worsening of psychotic symptoms*
- The "next best step" would be directed at *improving* psychotic symptoms, not worsening them. **Clozapine** is specifically indicated for **treatment-resistant schizophrenia**.
- Worsening psychosis would indicate treatment failure or an adverse reaction, not a typical side effect of the intended beneficial action.
Antipsychotic side effect management US Medical PG Question 5: A 60-year-old woman and her son are visited at her home by a health aid. He is her caregiver but has difficulty getting her out of the house. Her son is concerned about continuous and repetitive mouth and tongue movements that started about 2 weeks ago and have become more evident ever since. She is non-verbal at baseline and can complete most activities of daily living. She suffers from an unspecified psychiatric disorder. Her medications include fluphenazine. Today, her heart rate is 90/min, respiratory rate is 17/min, blood pressure is 125/87 mm Hg, and temperature is 37.0°C (98.6°F). On physical exam, she appears gaunt and anxious. She is drooling and her mouth is making a chewing motion that is occasionally disrupted by wagging her tongue back and forth. She seems to be performing these motions absentmindedly. Her heart has a regular rate and rhythm and her lungs are clear to auscultation bilaterally. CMP, CBC, and TSH are normal. A urine toxicology test is negative. What is the next best step in her management?
- A. Reduce the dosage
- B. Stop the medication (Correct Answer)
- C. Start clozapine
- D. Switch to chlorpromazine
- E. Expectant management
Antipsychotic side effect management Explanation: ***Stop the medication***
- The patient is presenting with symptoms of **tardive dyskinesia**, characterized by **involuntary, repetitive movements**, often involving the face (e.g., lip smacking, tongue protrusion, chewing motions), which are a known side effect of long-term use of **first-generation antipsychotics** like fluphenazine.
- The recommended management for drug-induced tardive dyskinesia is to discontinue the offending medication if possible, especially given the severity and recent onset of symptoms.
*Reduce the dosage*
- While dosage reduction might be considered in some side effects, for established **tardive dyskinesia**, simply reducing the dose of the causative agent often does not halt the progression or alleviate symptoms effectively and may even worsen them in some cases.
- The goal is to remove the underlying cause to prevent further neurological damage and potentially reverse the symptoms.
*Start clozapine*
- **Clozapine** is an atypical (second-generation) antipsychotic that is sometimes used in the management of severe tardive dyskinesia because it has a **lower risk of causing extrapyramidal symptoms** and can sometimes ameliorate existing ones.
- However, the initial step should be to remove the offending agent (fluphenazine) before introducing a new medication, especially one with its own significant side effect profile like agranulocytosis.
*Switch to chlorpromazine*
- **Chlorpromazine** is also a **first-generation antipsychotic** and carries a significant risk of causing **extrapyramidal symptoms and tardive dyskinesia**, similar to fluphenazine.
- Switching to another first-generation antipsychotic would not address the root cause of the tardive dyskinesia and would likely continue or worsen the symptoms.
*Expectant management*
- **Expectant management** (watching and waiting) is inappropriate for tardive dyskinesia because the condition can be **permanent** and worsen over time if the causative medication is continued.
- Prompt intervention by discontinuing the culprit drug is crucial to prevent irreversible symptoms and improve the patient's quality of life.
Antipsychotic side effect management US Medical PG Question 6: A 23-year old man is brought to the emergency department by his brother after trying to jump out of a moving car. He says that the Federal Bureau of Investigation has been following him for the last 7 months. He recently quit his job at a local consulting firm to work on his mission to rid the world from evil. He does not smoke, drink alcoholic beverages, or use illicit drugs. He takes no medications. His temperature is 36.7°C (98.1°F), pulse is 90/min, respirations are 20/min, and blood pressure is 120/86 mm Hg. On mental status examination, his response to the first question lasted 5 minutes without interruption. He switched topics a number of times and his speech was pressured. He spoke excessively about his plan to “bring absolute justice to the world”. He has a labile affect. There is no evidence of suicidal ideation. A toxicology screen is negative. He is admitted to the hospital for his symptoms and starts therapy. One week later, he develops difficulty walking and a tremor that improves with activity. Which of the following is the most likely cause of this patient's latest symptoms?
- A. Selective serotonin reuptake inhibitor
- B. Serotonin–norepinephrine reuptake inhibitor
- C. Dopamine antagonist (Correct Answer)
- D. Histamine antagonist
- E. Acetylcholine antagonist
Antipsychotic side effect management Explanation: ***Dopamine antagonist***
- The patient's initial symptoms (delusions, pressured speech, grandiosity, labile affect) are consistent with **mania or psychosis**. Starting therapy for such conditions frequently involves **dopamine antagonists (antipsychotics)**.
- The later development of difficulty walking and a tremor that improves with activity suggests **extrapyramidal symptoms (EPS)**, such as **drug-induced parkinsonism**, which is a common side effect of dopamine antagonists due to their blockade of D2 receptors in the nigrostriatal pathway.
*Selective serotonin reuptake inhibitor*
- While SSRIs can cause side effects like **akathisia** or **serotonin syndrome**, they are not typically associated with the tremor and gait difficulties described as improving with activity (parkinsonism-like symptoms).
- SSRIs are primarily used for **depression and anxiety disorders**, and while sometimes used as adjunctive therapy in bipolar disorder, they are not first-line for acute mania/psychosis and are unlikely to cause these specific motor symptoms a week into treatment.
*Serotonin–norepinephrine reuptake inhibitor*
- SNRIs, similar to SSRIs, are used for **depression and anxiety**, and their side effect profile does not typically include **drug-induced parkinsonism** or gait disturbances that improve with activity.
- The primary mechanism of action and common side effects of SNRIs do not align with the neurological symptoms of **tremor and difficulty walking** as described.
*Histamine antagonist*
- Histamine antagonists (like H1 blockers) are often used for **allergies or insomnia** and are not primary treatments for psychosis or mania.
- While some may cause **sedation or anticholinergic effects**, they do not typically cause the specific motor symptoms of **tremor and gait abnormalities** that improve with activity, consistent with drug-induced parkinsonism.
*Acetylcholine antagonist*
- Acetylcholine antagonists (anticholinergics) are sometimes used to **treat EPS** caused by dopamine antagonists, rather than being the direct cause of these symptoms themselves.
- While they can cause side effects like **dry mouth, blurred vision, or cognitive impairment**, they do not induce the characteristic tremor and gait issues that improve with activity as described.
Antipsychotic side effect management US Medical PG Question 7: A 30-year-old male presents to a local clinic with a complaint of a stiff neck. The patient is known to be sporadic with follow-up appointments but was last seen recently for a regular depot injection. He initially presented with complaints of paranoid delusions and auditory hallucinations that lasted for 7 months and caused significant social and financial deterioration. He was brought into the clinic by his older brother, who provides social support. Because of the patient's tendency to be non-compliant with medications, the patient was placed on a specific drug to mitigate this pattern. Which of the following medications is responsible for the patient's movement disorder?
- A. Thioridazine
- B. Clozapine
- C. Haloperidol (Correct Answer)
- D. Olanzapine
- E. Benztropine
Antipsychotic side effect management Explanation: ***Haloperidol***
- The patient's history of **paranoid delusions** and **auditory hallucinations** lasting 7 months, along with significant social and financial deterioration, is consistent with **schizophrenia**.
- Given the patient's **non-compliance** and lack of social support, he was likely prescribed a **long-acting injectable antipsychotic**. **Haloperidol decanoate** is a first-generation antipsychotic often used in this scenario, known for its higher risk of **extrapyramidal symptoms (EPS)** like a **stiff neck (dystonia)** compared to second-generation agents.
*Thioridazine*
- **Thioridazine** is a **first-generation antipsychotic** but is associated with a **lower incidence of EPS** compared to other high-potency typical antipsychotics like haloperidol.
- It also carries significant risks of **cardiac arrhythmias (QT prolongation)** and **retinal toxicity**, making it a less common choice for long-term management, especially with compliance issues.
*Clozapine*
- **Clozapine** is an atypical (second-generation) antipsychotic known for its efficacy in **treatment-resistant schizophrenia** and a very **low risk of EPS**.
- However, it requires **weekly blood monitoring** due to the risk of **agranulocytosis**, which makes it unsuitable for a patient with compliance issues and lack of social support.
*Olanzapine*
- **Olanzapine** is a **second-generation antipsychotic** that is available as a **long-acting injection**. While it can cause some EPS, the risk is generally **lower than with haloperidol**.
- It is more commonly associated with **metabolic side effects** such as weight gain, hyperglycemia, and dyslipidemia, rather than severe acute dystonia as the primary concern.
*Benztropine*
- **Benztropine** is an **anticholinergic medication** used to **treat the EPS induced by antipsychotics**, such as dystonia and parkinsonism.
- If a patient is experiencing a stiff neck due to an antipsychotic, benztropine would be a treatment for the side effect, not the cause of it.
Antipsychotic side effect management US Medical PG Question 8: A 28-year-old female patient with a history of schizophrenia, type 2 diabetes mellitus, and hypothyroidism comes to clinic stating she would like to be put back on a medication. She recently stopped taking her haloperidol as it made it hard for her to "sit still." She requests to be put on olanzapine as a friend from a support group said it was helpful. Why should this medication be avoided in this patient?
- A. The patient has type 2 diabetes (Correct Answer)
- B. The patient may develop galactorrhea
- C. Tardive dyskinesia will likely result from the prolonged use of olanzapine
- D. There is a high risk for retinopathy
- E. The patient is at a high risk for torsades de pointes
Antipsychotic side effect management Explanation: **The patient has type 2 diabetes**
- Olanzapine is associated with a high risk of **metabolic side effects**, including **weight gain**, **hyperglycemia**, and **dyslipidemia**, which would exacerbate her pre-existing type 2 diabetes.
- Given her history of diabetes, choosing a different antipsychotic with a lower metabolic risk profile would be more appropriate to prevent further metabolic complications.
*The patient may develop galactorrhea*
- **First-generation antipsychotics** and some **second-generation antipsychotics** like **risperidone** or **paliperidone** are more commonly associated with hyperprolactinemia, which can lead to galactorrhea.
- Olanzapine has a relatively **lower propensity** to cause significant elevations in prolactin compared to other antipsychotics.
*Tardive dyskinesia will likely result from the prolonged use of olanzapine*
- While all antipsychotics carry some risk of **tardive dyskinesia**, **second-generation antipsychotics** like olanzapine have a **lower risk** compared to first-generation antipsychotics such as haloperidol.
- The patient stopped haloperidol due to **akathisia**, an acute extrapyramidal symptom, not tardive dyskinesia, and olanzapine is generally associated with a lower incidence of extrapyramidal symptoms.
*There is a high risk for retinopathy*
- **Retinopathy** is not a common or significant adverse effect associated with olanzapine.
- **Thioridazine**, a first-generation antipsychotic, is uniquely associated with **pigmentary retinopathy** at high doses.
*The patient is at a high risk for torsades de pointes*
- Olanzapine carries a **low risk** for QTc prolongation and **torsades de pointes** compared to some other antipsychotics like **ziprasidone** or **thioridazine**.
- There is no indication from the patient's history that she is at an increased risk for QT prolongation, such as pre-existing cardiac conditions or electrolyte imbalances.
Antipsychotic side effect management US Medical PG Question 9: A 59-year-old woman comes to the clinic complaining of an intermittent, gnawing epigastric pain for the past 2 months. The pain is exacerbated with food and has been getting progressively worse. The patient denies any weight changes, nausea, vomiting, cough, or dyspepsia. Medical history is significant for chronic back pain for which she takes ibuprofen. Her father passed at the age of 55 due to pancreatic cancer. Labs were unremarkable except for a mild decrease in hemoglobin. What medication is most appropriate to be switched to from the current medication at this time?
- A. Naproxen
- B. Ranitidine
- C. Aspirin
- D. Acetaminophen
- E. Omeprazole (Correct Answer)
Antipsychotic side effect management Explanation: ***Omeprazole***
- The patient's symptoms of **gnawing epigastric pain** exacerbated by food, along with a history of chronic ibuprofen use and mild anemia, strongly suggest a **peptic ulcer**.
- **Omeprazole**, a proton pump inhibitor (PPI), is the most effective medication for healing ulcers and preventing their recurrence by reducing gastric acid production.
*Naproxen*
- **Naproxen** is a non-steroidal anti-inflammatory drug (NSAID), similar to ibuprofen, and would likely worsen the patient's symptoms by further inhibiting prostaglandin synthesis necessary for gastric mucosal protection.
- Continuing an NSAID without gastroprotection would increase the risk of ulcer complications, such as bleeding.
*Ranitidine*
- **Ranitidine** is an H2-receptor antagonist, which reduces stomach acid, but it is generally less potent than PPIs like omeprazole for treating and healing ulcers, especially in cases of NSAID-induced gastropathy.
- Its efficacy for advanced or severe peptic ulcer disease is inferior to that of PPIs.
- Note: Ranitidine was withdrawn from the US market in 2020 due to NDMA contamination; alternative H2 blockers include famotidine.
*Aspirin*
- **Aspirin** is an NSAID with significant antiplatelet effects and is well-known to cause and exacerbate peptic ulcers and gastrointestinal bleeding.
- Switching to aspirin would be contraindicated in the presence of strong evidence suggesting active peptic ulcer disease.
*Acetaminophen*
- **Acetaminophen** (paracetamol) is an analgesic that does not have significant anti-inflammatory properties and is not associated with gastric irritation or ulcer formation.
- While it could be used for pain relief, it does not address the underlying issue of peptic ulcer disease or provide gastroprotection, making it an inadequate switch for effective management.
Antipsychotic side effect management US Medical PG Question 10: A 25-year-old woman presented to an urgent care center with a complaint of a cough for more than 3 weeks that was accompanied by night sweats, weight loss, and malaise. On physical examination, the patient had slightly pale palpebral conjunctivae, bilateral posterior cervical lymphadenopathy, but with no adventitious breath sounds in the lung fields bilaterally. The remainder of the physical examination was routine. The patient was started on a drug regimen that was to be taken for 6 months. On follow-up after 2 months, the ALT and AST levels were elevated. Which of the following anti-tubercular drugs could have contributed to this laboratory result?
- A. Streptomycin
- B. Rifampicin
- C. Ethambutol
- D. Isoniazid (Correct Answer)
- E. Pyrazinamide
Antipsychotic side effect management Explanation: ***Isoniazid***
- **Isoniazid** is the **most commonly implicated** anti-tubercular drug in hepatotoxicity, particularly in the first 2 months of therapy, which matches this patient's timeline.
- While **Pyrazinamide** and **Rifampicin** can also cause hepatotoxicity, **Isoniazid** causes hepatotoxicity in **10-20% of patients** with elevated transaminases and is the **most frequent single agent** responsible for drug-induced liver injury in TB treatment.
- The hepatotoxicity manifests as elevated **ALT and AST levels** and can range from mild, asymptomatic enzyme elevations to severe, fatal hepatitis.
- Risk factors include **fast acetylator status**, alcohol use, and concurrent use of other hepatotoxic drugs.
*Rifampicin*
- **Rifampicin** can cause **hepatotoxicity**, but when it occurs alone (without Isoniazid), it typically presents as a **cholestatic pattern** with elevated alkaline phosphatase and bilirubin rather than predominantly elevated transaminases.
- Its primary adverse effects include **red-orange discoloration** of bodily fluids and significant drug interactions due to potent **cytochrome P450 enzyme induction**.
- Hepatotoxicity from Rifampicin is **less common** than from Isoniazid when used as monotherapy.
*Pyrazinamide*
- **Pyrazinamide** can cause **hepatotoxicity** and is associated with elevated liver enzymes, making it a possible contributor.
- However, **hepatotoxicity from Pyrazinamide** is **dose-dependent** and typically seen more with higher doses (>30 mg/kg/day) or in patients with pre-existing liver disease.
- It is also associated with **hyperuricemia** and can precipitate gouty arthritis, which is not indicated in this clinical scenario.
- In standard first-line therapy, **Isoniazid remains statistically more likely** to cause isolated transaminase elevation.
*Streptomycin*
- **Streptomycin** is an aminoglycoside antibiotic primarily known for its **ototoxicity** (vestibular and cochlear damage) and **nephrotoxicity**, rather than hepatotoxicity.
- Liver enzyme elevation is **not a characteristic adverse effect** of streptomycin and is rarely reported.
*Ethambutol*
- **Ethambutol** is primarily associated with **optic neuritis**, leading to decreased visual acuity and red-green color blindness, which requires monitoring with regular visual acuity and color vision testing.
- While mild liver enzyme elevations can rarely occur, significant **hepatotoxicity is uncommon** and not a characteristic primary adverse effect of ethambutol.
More Antipsychotic side effect management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.