Psychotic Disorders

On this page
🧠 The Psychotic Mind: Decoding Reality's Disruption
Psychotic disorders shatter the boundary between inner experience and external reality, creating profound disruptions in thought, perception, and behavior that challenge both patients and clinicians. You'll master the symptom architecture that defines these conditions, sharpen your diagnostic precision through pattern recognition, and learn evidence-based treatment algorithms that restore function. By integrating neurobiological mechanisms with rapid clinical assessment tools, you'll build the expertise to navigate complex presentations, distinguish mimics from true psychosis, and intervene decisively when reality itself becomes the patient's adversary.
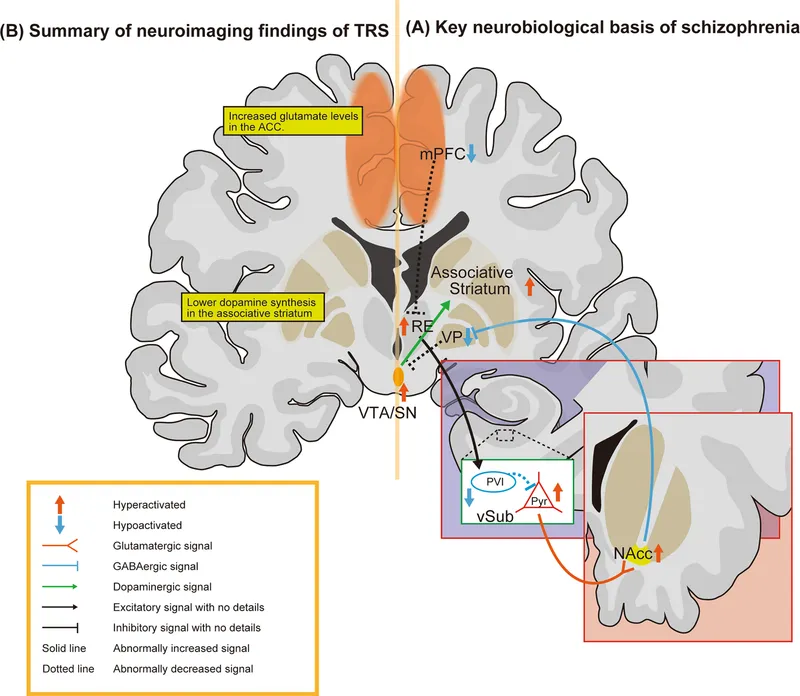
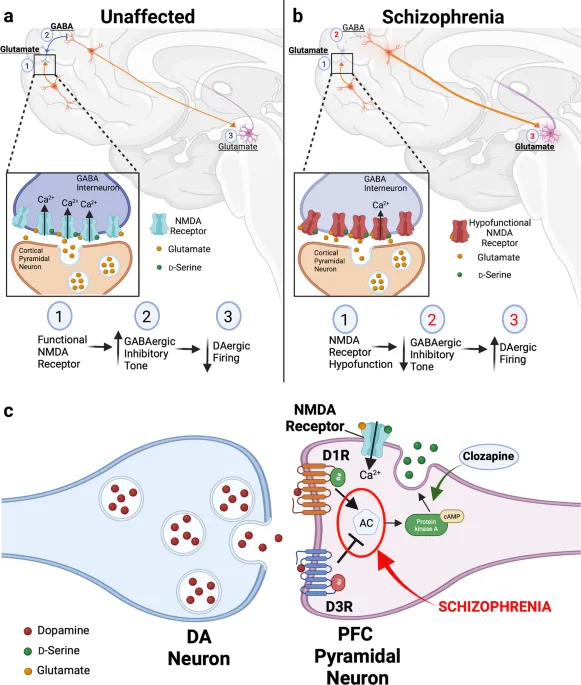
The dopaminergic hypothesis remains central to psychosis understanding, with D2 receptor blockade achieving therapeutic efficacy in 70-80% of patients. However, modern conceptualization extends beyond simple dopamine excess to include glutamate hypofunction, GABAergic dysfunction, and complex neurodevelopmental abnormalities.
📌 Remember: PSYCHOSIS - Perceptual disturbances (hallucinations), Suspiciousness (paranoia), Yearning for isolation, Cognitive disorganization, Hostility, Odd behavior, Speech abnormalities, Insight impairment, Social withdrawal
-
Primary Psychotic Disorders
- Schizophrenia: >6 months duration, significant functional decline
- Brief Psychotic Disorder: 1 day to 1 month, sudden onset with stressor
- With marked stressor: 80% recovery rate
- Without stressor: 60% recovery rate
- Schizophreniform Disorder: 1-6 months duration, intermediate prognosis
- Delusional Disorder: >1 month of delusions, preserved functioning
- Schizoaffective Disorder: mood episodes concurrent with psychotic symptoms
-
Secondary Psychotic Conditions
- Substance-Induced: Cannabis increases risk 2-3x, methamphetamine 5-7x
- Medical Conditions: Autoimmune encephalitis, temporal lobe epilepsy, Huntington's disease
- Anti-NMDA receptor encephalitis: 90% present with psychiatric symptoms first
- Systemic lupus erythematosus: 5-15% develop psychosis
⭐ Clinical Pearl: First-episode psychosis patients show 15-25% brain volume reduction in frontal and temporal regions, with progressive decline in untreated cases. Early intervention within 3 months improves 5-year outcomes by 40-60%.
The neurodevelopmental model explains psychosis emergence through two-hit hypothesis: genetic vulnerability combined with environmental stressors during critical developmental periods. Prenatal infections, obstetric complications, and adolescent cannabis use represent major environmental risk factors.
💡 Master This: Psychotic disorders result from complex gene-environment interactions affecting multiple neurotransmitter systems. The dopamine hypothesis explains positive symptoms, while glutamate hypofunction and GABAergic dysfunction account for negative symptoms and cognitive impairment.
Understanding psychotic disorders requires recognizing their heterogeneous presentations, variable courses, and differential treatment responses - knowledge that transforms clinical assessment from symptom cataloging into sophisticated neurobiological pattern recognition.
🧠 The Psychotic Mind: Decoding Reality's Disruption
🎭 Symptom Architecture: The Psychotic Spectrum
Positive Symptoms: Reality Distortion Syndrome
-
Hallucinations: Auditory most common (60-80% of patients)
- Command hallucinations: 10-15% prevalence, high violence risk
- Running commentary: 20-30% prevalence, poor prognosis indicator
- Visual hallucinations: 15-25% prevalence, consider medical causes
- Substance-induced: methamphetamine 40-70%, alcohol withdrawal 25%
- Medical conditions: Lewy body dementia 80%, delirium 30-40%
-
Delusions: Fixed false beliefs resistant to contradictory evidence
- Persecutory: 65-80% of psychotic patients
- Grandiose: 20-30% prevalence, manic episodes 60-70%
- Somatic: 15-25% prevalence, medical workup essential
- Bizarre delusions: Schizophrenia likelihood >90%
- Non-bizarre delusions: Delusional disorder vs mood disorders
📌 Remember: DELUSIONS types - Delusions of control, Erotomanic, Litigious, Unfaithfulness (jealousy), Somatic, Identity, Occupational, Nihilistic, Sins/guilt
Negative Symptoms: The Deficit Syndrome
-
Primary Negative Symptoms: Core disease manifestations
- Avolition: 60-70% prevalence, strongest functional predictor
- Alogia: 40-50% prevalence, poverty of speech content
- Anhedonia: 70-80% prevalence, social and physical subtypes
- Affective flattening: 50-60% prevalence, reduced emotional expression
- Asociality: 60-70% prevalence, social withdrawal and isolation
-
Secondary Negative Symptoms: Result from other factors
- Medication-induced: Extrapyramidal symptoms 30-40% with typicals
- Depression: 25-30% comorbidity rate in schizophrenia
- Environmental deprivation: Institutionalization effects
⭐ Clinical Pearl: Negative symptoms predict functional outcomes better than positive symptoms. Persistent negative symptoms for >6 months indicate deficit syndrome with poor prognosis and limited treatment response.
| Symptom Domain | Prevalence | Functional Impact | Treatment Response | Prognostic Value |
|---|---|---|---|---|
| Positive Symptoms | 80-90% | Moderate | Good (70-80%) | Limited |
| Negative Symptoms | 60-80% | Severe | Poor (20-30%) | Strong |
| Cognitive Symptoms | 85-95% | Severe | Minimal (10-15%) | Strongest |
| Disorganization | 40-60% | Variable | Moderate (50-60%) | Moderate |
| Mood Symptoms | 50-70% | Moderate | Good (60-70%) | Moderate |
-
Working Memory Deficits: 1-2 standard deviations below normal
- Digit span backward: Reduced in 90% of patients
- N-back tasks: Severe impairment correlates with functional disability
-
Executive Function Impairment: Planning, problem-solving, cognitive flexibility
- Wisconsin Card Sort: Perseverative errors increased 3-4x
- Trail Making B: Processing speed reduced 40-50%
-
Attention Deficits: Sustained attention and selective attention
- Continuous Performance Test: False alarms increased 2-3x
- Vigilance tasks: Signal detection impaired 50-60%
💡 Master This: Cognitive symptoms emerge years before psychotic onset, persist despite antipsychotic treatment, and predict real-world functioning better than positive symptoms. They represent core illness features requiring targeted interventions.
The symptom architecture reveals psychotic disorders as complex neurocognitive syndromes affecting multiple brain networks - understanding this complexity guides targeted assessment and individualized treatment approaches that address specific symptom domains rather than treating psychosis as a monolithic entity.
🎭 Symptom Architecture: The Psychotic Spectrum
🔍 Diagnostic Precision: Pattern Recognition Mastery
Primary Diagnostic Framework: The Psychosis Hierarchy
-
Medical Conditions (Rule out first)
- Autoimmune: Anti-NMDA receptor encephalitis (90% psychiatric presentation)
- Neurological: Temporal lobe epilepsy (10-15% psychosis rate)
- Endocrine: Hyperthyroidism (5-10%), Cushing's syndrome (15-20%)
- Infectious: Neurosyphilis (5%), HIV encephalopathy (10-15%)
- Red flags: Acute onset, altered consciousness, neurological signs
- Workup positive rate: 5-10% in first-episode psychosis
-
Substance-Induced Psychosis (Second priority)
- Cannabis: 2-3x increased risk, dose-dependent relationship
- Stimulants: Methamphetamine (40-70% psychosis rate), cocaine (25-30%)
- Alcohol: Withdrawal (25%), chronic use (5-10%)
- Hallucinogens: PCP (60-80%), LSD (20-30%)
- Temporal criterion: Symptoms within 1 month of intoxication/withdrawal
- Duration: Usually resolves within 1 month of abstinence
📌 Remember: SUBSTANCE psychosis clues - Sudden onset, Urine toxicology positive, Brief duration, Specific substance history, Temporal relationship, Abstinence improves symptoms, No premorbid dysfunction, Clear consciousness, Early age onset
Primary Psychotic Disorders: Temporal Patterns
-
Brief Psychotic Disorder: 1 day to 1 month
- With stressor: 80% recovery rate, good prognosis
- Without stressor: 60% recovery rate, higher recurrence risk
- Postpartum onset: 50% recurrence with subsequent pregnancies
-
Schizophreniform Disorder: 1-6 months duration
- Provisional diagnosis if <6 months elapsed
- Good prognostic features: Acute onset, confusion, good premorbid function
- Conversion rate: 60-70% progress to schizophrenia
-
Schizophrenia: >6 months with significant functional decline
- Continuous signs for ≥6 months
- Active phase: ≥1 month of positive symptoms
- Functional decline: Work, relationships, self-care
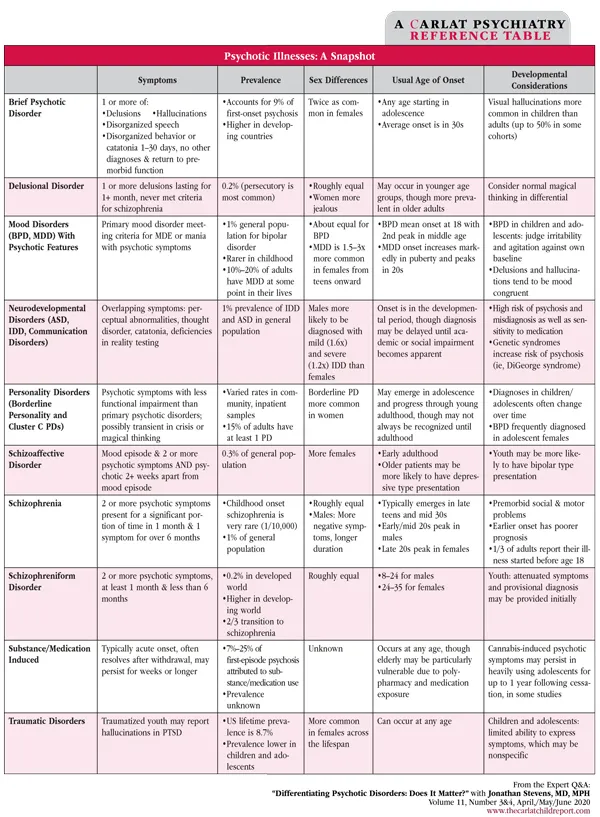
| Disorder | Duration | Functional Decline | Mood Episodes | Key Features |
|---|---|---|---|---|
| Brief Psychotic | 1 day-1 month | Minimal | Not prominent | Sudden onset/recovery |
| Schizophreniform | 1-6 months | Variable | Not prominent | Intermediate course |
| Schizophrenia | >6 months | Significant | Brief relative to psychosis | Chronic deterioration |
| Schizoaffective | >6 months | Significant | Prominent throughout | Mood + psychosis |
| Delusional | >1 month | Minimal | Not prominent | Isolated delusions |
-
Major Depression with Psychotic Features
- Mood-congruent: Guilt, worthlessness, somatic delusions
- Mood-incongruent: Persecutory, grandiose delusions (worse prognosis)
- Prevalence: 15-20% of severe depression episodes
-
Bipolar Disorder with Psychosis
- Manic episodes: Grandiose delusions (60-70%), mood-congruent
- Depressive episodes: Guilt, persecution themes
- Mixed episodes: Complex presentations, high suicide risk
-
Schizoaffective Disorder: Psychosis without mood symptoms for ≥2 weeks
- Depressive type: Major depression + psychosis
- Bipolar type: Manic/mixed episodes + psychosis
- Diagnostic challenge: Temporal relationships crucial
⭐ Clinical Pearl: Schizoaffective disorder requires psychotic symptoms for ≥2 weeks in the absence of prominent mood symptoms. If psychosis occurs only during mood episodes, diagnose mood disorder with psychotic features.
💡 Master This: Diagnostic precision requires systematic exclusion of medical and substance causes, careful temporal analysis of mood and psychotic symptoms, and functional assessment. The hierarchy prioritizes treatable medical conditions over primary psychiatric diagnoses.
Pattern recognition mastery transforms complex presentations into systematic diagnostic approaches - enabling accurate diagnosis, appropriate treatment selection, and prognostic counseling that guides long-term management strategies.
🔍 Diagnostic Precision: Pattern Recognition Mastery
⚖️ Differential Diagnosis: The Clinical Detective
Primary vs Secondary Psychosis: Discriminating Features
-
Age of Onset Patterns
- Schizophrenia: Peak 18-25 years (males), 25-35 years (females)
- Late-onset psychosis (>40 years): Medical causes 60-70% probability
- Very late-onset (>60 years): Dementia 40-50%, medical 30-40%
- Childhood onset (<13 years): Rare (<1%), severe course
-
Premorbid Functioning Indicators
- Schizophrenia: Gradual decline over months to years
- Brief psychotic disorder: Normal functioning until acute onset
- Medical psychosis: Acute change from baseline functioning
- Substance-induced: Functioning related to substance use pattern
-
Cognitive Profile Distinctions
- Schizophrenia: Generalized deficits, 1-2 SD below normal
- Bipolar psychosis: Selective deficits, 0.5-1 SD below normal
- Medical psychosis: Fluctuating or domain-specific deficits
- Substance-induced: Reversible deficits with abstinence
📌 Remember: MEDICAL psychosis red flags - Memory impairment, Elevated vital signs, Disorientation, Incontinence, Catatonic features, Acute onset, Level of consciousness changes
| Discriminating Feature | Schizophrenia | Bipolar Psychosis | Medical Psychosis | Substance-Induced |
|---|---|---|---|---|
| Onset Pattern | Gradual (months) | Episodic | Acute (days) | Temporal to use |
| Consciousness | Clear | Clear | Often impaired | Variable |
| Cognitive Pattern | Persistent deficits | Episodic deficits | Fluctuating | Reversible |
| Physical Signs | Minimal | Minimal | Often present | Substance-specific |
| Course | Chronic | Episodic | Variable | Self-limited |
-
Schizoaffective vs Schizophrenia
- Mood episode duration: ≥50% of total illness duration (schizoaffective)
- Psychosis without mood: ≥2 weeks required (schizoaffective)
- Functional decline: Similar in both conditions
- Treatment response: Better mood response in schizoaffective
-
Schizoaffective vs Mood Disorder with Psychosis
- Psychosis timing: Only during mood episodes (mood disorder)
- Residual symptoms: Persistent psychosis (schizoaffective)
- Severity: More severe mood symptoms (mood disorder)
- Prognosis: Better in mood disorders
-
Delusional Disorder vs Schizophrenia
- Delusion type: Non-bizarre (delusional disorder) vs bizarre (schizophrenia)
- Functioning: Preserved except delusion-related areas
- Other symptoms: Minimal hallucinations or disorganization
- Insight: Better in non-delusional areas
Substance-Induced Psychosis: Specific Patterns
-
Cannabis-Induced Psychosis
- Risk factors: High THC content (>10%), daily use, adolescent onset
- Symptoms: Paranoid delusions (80%), auditory hallucinations (60%)
- Duration: Days to weeks after cessation
- Conversion risk: 25-30% develop schizophrenia within 3 years
-
Stimulant-Induced Psychosis
- Methamphetamine: Paranoid delusions (90%), tactile hallucinations (40%)
- Cocaine: Paranoid ideation (70%), formication (30%)
- Duration: Hours to days after last use
- Chronic use: Persistent symptoms in 10-15%
-
Alcohol-Related Psychosis
- Withdrawal: Visual hallucinations (60%), delirium tremens (5%)
- Chronic use: Alcoholic hallucinosis (2-3% prevalence)
- Duration: 3-7 days typical course
- Treatment: Benzodiazepines first-line
⭐ Clinical Pearl: Cannabis-induced psychosis in adolescents carries highest conversion risk to schizophrenia (40-50% within 5 years). Early intervention and sustained abstinence reduce conversion rates by 30-40%.
Medical Conditions: High-Yield Associations
-
Autoimmune Encephalitis
- Anti-NMDA receptor: Psychiatric symptoms in 90%, young females
- Anti-LGI1: Temporal lobe seizures + psychosis
- Diagnosis: CSF antibodies, brain MRI, EEG abnormalities
- Treatment: Immunotherapy within 4 weeks optimal
-
Neurological Conditions
- Huntington's disease: Psychosis in 25%, movement disorders
- Wilson's disease: Psychiatric symptoms in 50%, copper studies
- Temporal lobe epilepsy: Interictal psychosis in 10-15%
- Brain tumors: Frontal and temporal locations highest risk
💡 Master This: Systematic differential diagnosis requires temporal analysis, substance history, medical screening, and cognitive assessment. Red flags for secondary causes include acute onset, altered consciousness, neurological signs, and atypical age of presentation.
The clinical detective approach transforms complex presentations into systematic diagnostic algorithms - enabling accurate identification of treatable conditions and appropriate therapeutic interventions based on specific disorder characteristics.
⚖️ Differential Diagnosis: The Clinical Detective
🎯 Treatment Algorithms: Evidence-Based Intervention
First-Episode Psychosis: Rapid Intervention Protocol
-
Initial Assessment Phase (0-72 hours)
- Medical clearance: CBC, CMP, TSH, B12, folate, RPR
- Substance screening: Urine toxicology, alcohol level
- Neuroimaging: Brain MRI if focal signs or atypical presentation
- Risk assessment: Suicide (40% attempt rate), violence (10-15%)
-
Antipsychotic Selection Algorithm
- First-line: Atypical antipsychotics (aripiprazole, olanzapine, risperidone)
- Dosing: Start low (25-50% target dose), titrate weekly
- Target symptoms: Positive symptoms improve 1-2 weeks, negative symptoms 4-6 weeks
- Treatment duration: Minimum 1-2 years for first episode
Antipsychotic Selection: Evidence-Based Matching
-
Efficacy Considerations
- Positive symptoms: All antipsychotics equally effective (70-80% response)
- Negative symptoms: Aripiprazole, cariprazine superior
- Cognitive symptoms: Minimal differences, adjunctive strategies needed
- Treatment-resistant: Clozapine 30-40% response rate
-
Side Effect Profiles: Risk-Benefit Analysis
- Metabolic risk: Olanzapine > quetiapine > risperidone > aripiprazole
- EPS risk: Haloperidol > risperidone > olanzapine > quetiapine
- Prolactin elevation: Risperidone > paliperidone > olanzapine
- QTc prolongation: Ziprasidone > quetiapine > olanzapine
| Antipsychotic | Metabolic Risk | EPS Risk | Sedation | Prolactin | Special Considerations |
|---|---|---|---|---|---|
| Aripiprazole | Low | Low | Low | Minimal | Partial agonist, activating |
| Olanzapine | High | Low | High | Moderate | Weight gain 7-10 kg |
| Risperidone | Moderate | Moderate | Moderate | High | Dose-dependent EPS |
| Quetiapine | Moderate | Low | High | Low | Requires BID dosing |
| Haloperidol | Low | High | Low | High | High potency typical |
Treatment-Resistant Schizophrenia: Clozapine Protocol
- Definition: Failure of ≥2 antipsychotic trials at adequate doses for ≥6 weeks
- Prevalence: 20-30% of schizophrenia patients
- Clozapine Efficacy: 30-40% response rate in treatment-resistant cases
- Monitoring Requirements:
- ANC monitoring: Weekly for 6 months, then biweekly for 6 months
- Metabolic monitoring: Baseline and every 3 months
- Cardiac monitoring: Baseline ECG, troponin if chest pain
- Seizure risk: Dose-dependent, 1-4% incidence
📌 Remember: CLOZAPINE monitoring - CBC weekly initially, Lipids every 3 months, Obesity monitoring, Zero tolerance for missed labs, ANC <1000 discontinue, Pneumonia risk, Infection surveillance, Neutropenia monitoring, ECG baseline
Psychosocial Interventions: Evidence-Based Adjuncts
-
Cognitive Behavioral Therapy for Psychosis (CBTp)
- Efficacy: Small to moderate effect sizes (0.3-0.5)
- Target symptoms: Delusions, hallucinations, negative symptoms
- Duration: 16-20 sessions over 4-6 months
- Combination: Antipsychotics + CBTp superior to monotherapy
-
Family Interventions
- Expressed emotion reduction: 50% relapse reduction
- Psychoeducation: Illness understanding, medication adherence
- Communication training: Problem-solving skills
- Duration: 9-12 months minimum for sustained benefits
-
Cognitive Remediation
- Target: Working memory, attention, executive function
- Efficacy: Small effect sizes (0.2-0.4) on cognition
- Functional transfer: Limited without vocational rehabilitation
- Duration: 40-50 hours over 3-6 months
⭐ Clinical Pearl: Combination treatment with antipsychotics + psychosocial interventions reduces relapse rates by 40-50% compared to medication alone. Early intervention within 3 months of first episode improves 10-year outcomes significantly.
Maintenance Treatment: Long-Term Strategies
-
Relapse Prevention
- Medication adherence: 40-60% non-adherence rate
- Long-acting injectables: 25-30% relapse reduction
- Monitoring frequency: Monthly first year, quarterly thereafter
- Duration: Minimum 2 years first episode, lifelong multiple episodes
-
Functional Recovery Goals
- Symptom remission: PANSS total <70 or 30% reduction
- Functional improvement: Return to work/school in 40-60%
- Quality of life: Subjective wellbeing measures
- Social functioning: Relationship maintenance, independent living
💡 Master This: Treatment algorithms prioritize rapid symptom control, side effect minimization, and functional recovery. Measurement-based care using standardized scales guides dose optimization and treatment switching decisions for optimal outcomes.
Evidence-based intervention transforms complex treatment decisions into systematic protocols - enabling personalized care that maximizes efficacy while minimizing adverse effects through careful monitoring and algorithmic adjustments.
🎯 Treatment Algorithms: Evidence-Based Intervention
🔗 Neurobiology Integration: The Psychotic Brain Network
The Dopamine Hypothesis: Refined Understanding
-
Mesolimbic Pathway Hyperactivity
- Ventral tegmental area to nucleus accumbens
- Positive symptoms: Hallucinations, delusions from excessive dopamine
- D2 receptor density: Increased 10-15% in antipsychotic-naive patients
- Treatment target: D2 blockade 60-80% for therapeutic effect
-
Mesocortical Pathway Hypoactivity
- VTA to prefrontal cortex reduced dopamine
- Negative symptoms: Avolition, alogia, anhedonia
- Cognitive symptoms: Working memory, executive function deficits
- Treatment challenge: D2 blockade may worsen cortical hypofunction
-
Nigrostriatal Pathway Implications
- Substantia nigra to striatum
- Motor control: EPS risk with D2 blockade
- Individual variation: CYP2D6 polymorphisms affect metabolism
- Monitoring: AIMS scale every 6 months for tardive dyskinesia
📌 Remember: DOPAMINE pathways - Default (mesolimbic hyperactivity), Organization (mesocortical hypoactivity), Positive symptoms (excess), Anhedonia (deficit), Motor (nigrostriatal), Inhibition (tuberoinfundibular), Negative symptoms (cortical), Extrapyramidal (striatal)
Glutamate Hypofunction: The NMDA Hypothesis
-
NMDA Receptor Hypofunction
- Primary deficit: Reduced glutamate signaling
- Secondary effects: GABAergic interneuron dysfunction
- Disinhibition: Excessive glutamate release in some regions
- Developmental timing: Adolescent onset matches NMDA maturation
-
Circuit-Level Consequences
- Gamma oscillations: Reduced 40Hz activity in cognitive tasks
- Parvalbumin interneurons: 30-40% reduction in schizophrenia
- Excitatory/inhibitory balance: Disrupted across multiple regions
- Plasticity deficits: Impaired long-term potentiation
-
Therapeutic Implications
- Glycine transport inhibitors: Modest efficacy for negative symptoms
- mGluR agonists: Potential targets for cognitive enhancement
- AMPA modulators: Cognitive improvement in early trials
- Combination approaches: NMDA enhancement + antipsychotics
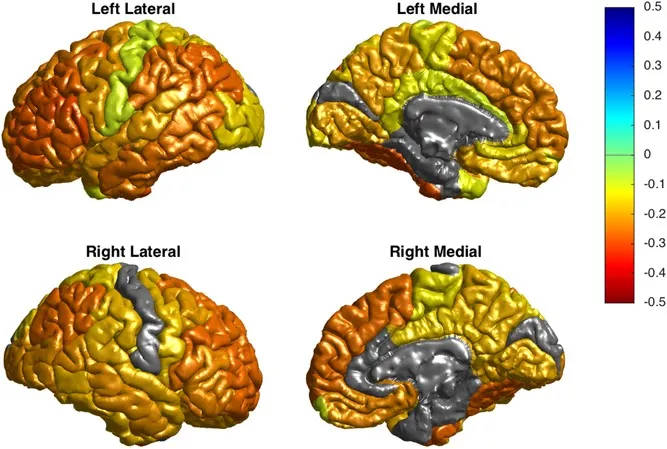
Structural Brain Changes: Progressive Alterations
-
Gray Matter Reductions
- Frontal cortex: 10-15% volume loss, progressive over 5 years
- Temporal cortex: Superior temporal gyrus 20-25% reduction
- Hippocampus: 4-8% volume loss, memory deficits correlation
- Thalamus: 8-12% reduction, connectivity hub disruption
-
White Matter Abnormalities
- Corpus callosum: Reduced interhemispheric connectivity
- Uncinate fasciculus: Temporal-frontal disconnection
- Cingulum bundle: Default network disruption
- Fractional anisotropy: Decreased in multiple tracts
-
Ventricular Enlargement
- Lateral ventricles: 20-30% larger than controls
- Third ventricle: Enlarged in 70-80% of patients
- Progressive changes: 2-3% annual increase
- Treatment effects: Antipsychotics may slow progression
| Brain Region | Volume Change | Functional Impact | Treatment Response | Progressive Change |
|---|---|---|---|---|
| Prefrontal Cortex | -10 to -15% | Executive function | Partial | Yes |
| Superior Temporal | -20 to -25% | Auditory processing | Limited | Yes |
| Hippocampus | -4 to -8% | Memory formation | Minimal | Moderate |
| Thalamus | -8 to -12% | Connectivity hub | Variable | Yes |
| Striatum | Variable | Motor control | Good | Medication-related |
-
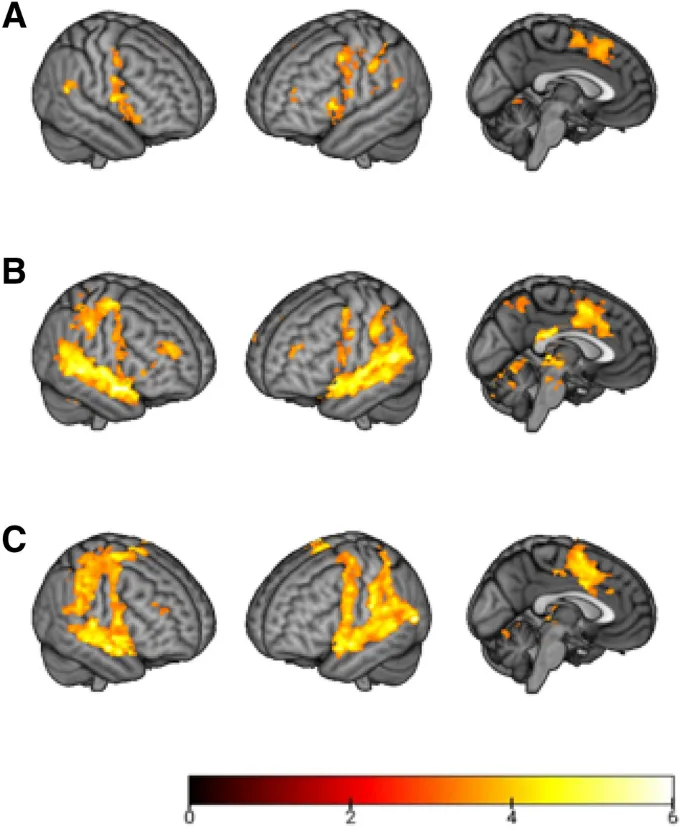
Default Mode Network (DMN)
- Hyperactivity: Increased self-referential processing
- Delusion formation: Aberrant salience attribution
- Meditation/mindfulness: Potential therapeutic target
- Antipsychotic effects: Normalize DMN activity partially
-
Salience Network
- Anterior insula: Reduced salience detection
- Anterior cingulate: Impaired conflict monitoring
- Hallucination correlation: Network switching deficits
- Cognitive training: May improve network function
-
Central Executive Network
- Dorsolateral PFC: Working memory deficits
- Posterior parietal: Attention control impairment
- Cognitive remediation: Target for intervention
- Stimulant augmentation: Potential cognitive enhancement
⭐ Clinical Pearl: Network-based understanding explains symptom heterogeneity and treatment resistance. Combination approaches targeting multiple neurotransmitter systems show superior efficacy compared to dopamine-only interventions.
Emerging Therapeutic Targets
-
Cholinergic Enhancement
- Alpha-7 nicotinic receptors: Cognitive improvement target
- Cholinesterase inhibitors: Modest benefits for negative symptoms
- Nicotine patches: Cognitive enhancement in smokers
- Allosteric modulators: Selective receptor enhancement
-
Inflammatory Modulation
- Microglial activation: Increased in schizophrenia
- Cytokine elevation: IL-6, TNF-alpha elevated
- Anti-inflammatory: Aspirin, minocycline adjunctive benefits
- Omega-3 fatty acids: Neuroprotective effects
💡 Master This: Psychotic disorders result from complex network disruptions involving multiple neurotransmitter systems. Future treatments will target specific circuit dysfunctions rather than broad dopamine blockade, enabling personalized interventions based on individual network profiles.
The neurobiology integration reveals psychosis as sophisticated network disorders requiring multi-target interventions - transforming treatment from symptom suppression to circuit restoration through precision medicine approaches.
🔗 Neurobiology Integration: The Psychotic Brain Network
🎯 Clinical Mastery Arsenal: Rapid Assessment Tools
Essential Rating Scales: Quantified Assessment
-
Positive and Negative Syndrome Scale (PANSS)
- 30 items: 7 positive, 7 negative, 16 general psychopathology
- Severity range: 30-210 total score
- Clinical significance: ≥30% reduction indicates treatment response
- Remission criteria: All items ≤3 (mild) for ≥6 months
- Positive subscale: P1, P3, P6 (delusions, hallucinations, suspiciousness)
- Negative subscale: N1, N4, N6 (blunted affect, social withdrawal, lack of spontaneity)
-
Brief Psychiatric Rating Scale (BPRS)
- 18-24 items: Rapid assessment in 10-15 minutes
- Severity range: 18-126 (18-item version)
- Clinical utility: Emergency settings, frequent monitoring
- Factor structure: Positive, negative, depression, mania
-
Clinical Global Impression (CGI)
- CGI-S: Severity rating 1-7 scale
- CGI-I: Improvement rating 1-7 scale
- Clinical significance: CGI-I ≤2 indicates much improved
- Regulatory standard: Primary endpoint in clinical trials
📌 Remember: PANSS remission criteria - Positive symptoms ≤3, Affect blunted ≤3, Negative symptoms ≤3, Social withdrawal ≤3, Suspiciousness ≤3 for ≥6 months
Risk Assessment Framework: Safety Prioritization
-
Suicide Risk Stratification
- High-risk factors: Command hallucinations (15-20% attempt rate)
- Acute phase: 40% lifetime attempt rate in schizophrenia
- Protective factors: Treatment engagement, family support
- Assessment tools: Columbia Suicide Severity Rating Scale
-
Violence Risk Assessment
- Static factors: History of violence (strongest predictor)
- Dynamic factors: Active symptoms, substance use, medication adherence
- Base rates: 10-15% violence rate in first-episode psychosis
- Assessment tools: HCR-20, STAMP (Short-Term Assessment of Risk and Treatability)
-
Substance Use Screening
- Prevalence: 50-60% lifetime substance use in schizophrenia
- Cannabis: 25-30% current use rate
- Alcohol: 20-25% abuse/dependence rate
- Screening tools: AUDIT, DAST-10, urine toxicology
| Risk Domain | Assessment Tool | Time Required | Clinical Utility | Sensitivity/Specificity |
|---|---|---|---|---|
| Suicide | C-SSRS | 5-10 minutes | High | Sens 95%/Spec 85% |
| Violence | HCR-20 | 20-30 minutes | Moderate | Sens 80%/Spec 70% |
| Substance Use | AUDIT/DAST | 5 minutes | High | Sens 90%/Spec 80% |
| Medication Adherence | MARS | 5 minutes | Moderate | Sens 85%/Spec 75% |
| Cognitive Function | MoCA | 10 minutes | Moderate | Sens 85%/Spec 70% |
-
First-Episode Psychosis Checklist
- Age: 15-35 years (typical range)
- Onset: Gradual (weeks to months) vs acute (days)
- Substance use: Recent or chronic use history
- Medical history: Autoimmune, neurological, endocrine conditions
- Family history: Psychotic disorders, mood disorders
-
Medical Clearance Protocol
- Laboratory: CBC, CMP, TSH, B12, folate, RPR, HIV
- Toxicology: Urine drug screen, alcohol level
- Neuroimaging: Brain MRI if focal signs or age >40
- Additional: EEG if seizure history, LP if encephalitis suspected
Treatment Monitoring Dashboard: Objective Metrics
-
Symptom Tracking
- PANSS: Monthly for first 6 months, then quarterly
- CGI-S/I: Every visit for rapid assessment
- Target: ≥30% PANSS reduction by 12 weeks
- Remission: PANSS items ≤3 for ≥6 months
-
Side Effect Monitoring
- Metabolic: Weight, BMI, waist circumference monthly
- Laboratory: Glucose, lipids at baseline, 3 months, annually
- Movement: AIMS every 6 months, SAS if EPS suspected
- Cardiac: ECG if QTc-prolonging medications
-
Functional Assessment
- Global Assessment of Functioning (GAF): 0-100 scale
- Personal and Social Performance (PSP): Four domains assessment
- Quality of Life Scale (QLS): 21 items, functional outcomes
- Work/school: Return to function in 40-60% with treatment
⭐ Clinical Pearl: Measurement-based care using standardized scales improves treatment outcomes by 25-30% compared to clinical judgment alone. Monthly PANSS assessments guide dose optimization and medication switching decisions.
Emergency Assessment Protocol: Crisis Management
-
Immediate Safety Assessment (0-15 minutes)
- Suicidal ideation: Direct questioning, plan assessment
- Homicidal ideation: Target identification, means assessment
- Agitation level: ACES (Agitation-Calmness Evaluation Scale)
- Capacity assessment: Decision-making ability
-
Rapid Stabilization (15-60 minutes)
- Verbal de-escalation: Calm environment, active listening
- Medication: Haloperidol 5mg IM or olanzapine 10mg IM
- Restraints: Last resort, 15-minute checks
- Family contact: Collateral information, support system
-
Disposition Planning (60-120 minutes)
- Hospitalization criteria: Imminent danger, grave disability
- Outpatient safety: Support system, follow-up arranged
- Medication initiation: Antipsychotic if not contraindicated
- Crisis plan: Warning signs, emergency contacts
💡 Master This: Clinical mastery requires systematic assessment, objective monitoring, and evidence-based decision-making. Standardized tools transform subjective impressions into quantifiable metrics that guide treatment optimization and outcome prediction.
The clinical mastery arsenal enables rapid, accurate assessment and systematic monitoring - transforming complex presentations into manageable clinical data that supports evidence-based treatment decisions and optimal patient outcomes.
🎯 Clinical Mastery Arsenal: Rapid Assessment Tools
Practice Questions: Psychotic Disorders
Test your understanding with these related questions
A 26-year-old man is brought to the emergency department by his wife because of bizarre and agitated behavior for the last 6 weeks. He thinks that the NSA is spying on him and controlling his mind. His wife reports that the patient has become withdrawn and at times depressed for the past 3 months. He lost his job because he stopped going to work 4 weeks ago. Since then, he has been working on an invention that will block people from being able to control his mind. Physical and neurologic examinations show no abnormalities. On mental status examination, he is confused and suspicious with marked psychomotor agitation. His speech is disorganized and his affect is labile. Which of the following is the most likely diagnosis?













