Psychotherapeutic approaches (DBT, MBT) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Psychotherapeutic approaches (DBT, MBT). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 1: A 29-year-old woman is hospitalized due to depression and suicidal ideation. She has a 5-year history of chaotic relationships that last only a few short weeks or months. Each relationship has left her feeling abandoned, empty, and extremely upset. During these periods, the patient confesses to shopping and making big purchases on impulse. She says she gets bored easily and moves on to the next adventure. The patient denies any changes in appetite, energy level, or concentration. On examination, multiple linear lacerations of varying phases of healing were noted on her forearms and trunk. Following consultation, she praises physicians to be ‘the best people on the planet’, but when the nurse came in to take her blood, she furiously stated that ‘all nurses are incompetent and cruel’. Which of the following is the most likely diagnosis?
- A. Borderline personality disorder (Correct Answer)
- B. Histrionic personality disorder
- C. Major depressive disorder (MDD)
- D. Bipolar I disorder
- E. Factitious disorder
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Borderline personality disorder***
- This condition is characterized by a pervasive pattern of **instability in interpersonal relationships**, **self-image**, and **affects**, along with marked impulsivity, as evidenced by chaotic relationships, feelings of abandonment, and impulsive shopping.
- The patient's rapid shift from idealizing physicians to devaluing nurses (the "best people" to "incompetent and cruel") is characteristic of **splitting**, a common defense mechanism in borderline personality disorder, and the self-inflicted lacerations indicate **self-harm**, another hallmark feature.
*Histrionic personality disorder*
- Characterized by **excessive emotionality** and **attention-seeking behavior**, often through dramatic and sexually provocative means.
- While there may be some superficial overlap in relationship instability, the primary symptoms of splitting, impulsivity (shopping), and self-harm are less prominent here than in borderline personality disorder.
*Major depressive disorder (MDD)*
- While the patient exhibits **depression and suicidal ideation**, MDD typically involves core symptoms like persistent sadness, anhedonia, and changes in appetite, sleep, and energy, which the patient denies ("denies any changes in appetite, energy level, or concentration").
- The long-standing pattern of chaotic relationships, impulsivity, and splitting points away from MDD as the primary diagnosis, suggesting a more pervasive personality difficulty.
*Bipolar I disorder*
- This disorder is characterized by distinct periods of **mania or hypomania** alternating with depressive episodes.
- While impulsivity can be seen in hypomanic/manic states, the patient's symptoms are described as persistent emotional instability and chaotic relationships present for five years, rather than episodic changes in mood and energy, and she denies changes in appetite or energy.
*Factitious disorder*
- Involves **falsification of physical or psychological signs or symptoms**, or induction of injury or disease, associated with identified deception, to assume the sick role.
- Although the patient has self-inflicted lacerations, this behavior is more consistent with **self-harm** seen in borderline personality disorder as a coping mechanism for emotional distress, rather than a deliberate attempt to deceive medical professionals for secondary gain.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 2: A 23-year-old woman is brought to the emergency room by her mother after she is found to have cut both of her wrists with razor blades. The patient admits to a history of self-mutilation and attributed this incident to a recent breakup with a man she had been seeing for the previous 2 weeks. On morning rounds, the patient reports that the nurses are incompetent but the doctors are some of the best in the world. The patient's vitals are stable and her wrist lacerations are very superficial requiring only simple dressings without sutures. The patient is discharged a few days later and she feels well. Which of the following is the most appropriate initial treatment for this patient?
- A. Amitriptyline
- B. Fluoxetine
- C. Dialectical behavior therapy (Correct Answer)
- D. Cognitive behavioral therapy
- E. Lithium
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Dialectical behavior therapy***
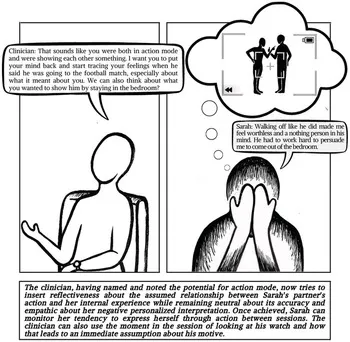
- The patient's presentation with **recurrent self-harm**, **mood instability** following a brief relationship, and **splitting** ("nurses are incompetent but doctors are the best") are classic features of **borderline personality disorder (BPD)**.
- **Dialectical behavior therapy (DBT)** is the gold-standard and most effective initial treatment for BPD, specifically targeting **emotional dysregulation**, self-harm, and suicidal behaviors.
*Amitriptyline*
- **Amitriptyline** is a **tricyclic antidepressant (TCA)**, primarily used for depression and chronic pain.
- While antidepressants might be used *adjunctively* for comorbid mood symptoms in BPD, they are not the primary or most appropriate *initial* treatment for the core features of BPD itself, and TCAs have a high overdose risk.
*Fluoxetine*
- **Fluoxetine** is a **selective serotonin reuptake inhibitor (SSRI)**, commonly used for depression, anxiety disorders, and some eating disorders.
- Similar to other antidepressants, SSRIs may treat comorbid depressive or anxiety symptoms in BPD but do not address the fundamental **personality organization issues** or behavioral patterns like self-harm and splitting characteristic of BPD.
*Cognitive behavioral therapy*
- **Cognitive behavioral therapy (CBT)** is effective for a wide range of mental health conditions, including depression and anxiety, by focusing on changing negative thought patterns and behaviors.
- While elements of CBT are incorporated into DBT, **DBT is specifically adapted and more effective for BPD** due to its emphasis on **emotion regulation**, distress tolerance, and interpersonal effectiveness skills, which are crucial for this patient's presentation.
*Lithium*
- **Lithium** is a mood stabilizer primarily used to treat **bipolar disorder**.
- Although there can be some overlap in symptoms (e.g., mood swings), the patient's presentation is more indicative of BPD due to the **recurrent self-harm, interpersonal instability**, and **splitting**, rather than the distinct mood episodes seen in bipolar disorder.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 3: A 25-year-old woman is brought to the emergency department by her boyfriend after she cut her forearms with a knife. She has had multiple visits to the emergency department in the past few months for self-inflicted wounds. She claims that her boyfriend is the worst person in the world. She and her boyfriend have broken up 20 times in the past 6 months. She says she cut herself not because she wants to kill herself; she feels alone and empty and wants her boyfriend to take care of her. Her boyfriend claims that she is prone to outbursts of physical aggression as well as mood swings. He says that these mood swings last a few hours and vary from states of exuberance and self-confidence to states of self-doubt and melancholy. On examination, the patient appears well-dressed and calm. She has normal speech, thought processes, and thought content. Which of the following is the most likely diagnosis?
- A. Dependent personality disorder
- B. Borderline personality disorder (Correct Answer)
- C. Bipolar II disorder
- D. Cyclothymic disorder
- E. Histrionic personality disorder
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Borderline personality disorder***
- This patient exhibits characteristic features of **borderline personality disorder**, including **impulsivity** (self-harm), **unstable relationships** (frequent breakups, idealization/devaluation of boyfriend), **affective instability** (rapid mood swings lasting hours), and feelings of **emptiness** and **abandonment**.
- **Self-harm** in BPD is often a coping mechanism for intense emotional pain or a way to elicit care, rather than a genuine suicide attempt, as stated by the patient.
*Dependent personality disorder*
- Characterized by an **excessive need to be cared for**, leading to submissive and clinging behavior and fears of separation, which is not the primary presentation here.
- While there is a desire for care, the prominent features of **impulsivity**, **affective instability**, and **unstable relationships** are not typical of dependent personality disorder.
*Bipolar II disorder*
- Involves episodes of **hypomania** and **major depression**, with mood swings typically lasting for at least **four days** (hypomania) or **two weeks** (major depression), much longer than the hours described here.
- The patient's presentation emphasizes **interpersonal instability** and **self-harm** more than episodic mood disturbances.
*Cyclothymic disorder*
- Involves **numerous periods of hypomanic symptoms** and numerous periods of **depressive symptoms** for at least two years, but these symptoms are less severe than full-blown hypomanic or major depressive episodes.
- The rapid mood shifts within hours and the intensity of **interpersonal dysfunction** and **self-harm** are more indicative of borderline personality disorder.
*Histrionic personality disorder*
- Characterized by **excessive emotionality** and **attention-seeking behavior**, often sexually provocative, and using physical appearance to draw attention.
- While emotionality is present, the **self-harm**, **emptiness**, and **rapid mood shifts** are not core features of histrionic personality disorder.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 4: A 35-year-old man comes to the Veterans Affairs hospital because of a 2-month history of anxiety. He recently returned from his third deployment to Iraq, where he served as a combat medic. He has had difficulty readjusting to civilian life. He works as a taxi driver but had to take a leave of absence because of difficulties with driving. Last week, he hit a stop sign because he swerved out of the way of a grocery bag that was in the street. He has difficulty sleeping because of nightmares about the deaths of some of the other soldiers in his unit and states, “it's my fault, I could have saved them. Please help me.” Mental status examination shows a depressed mood and a restricted affect. There is no evidence of suicidal ideation. Which of the following is the most appropriate initial step in treatment?
- A. Dialectical behavioral therapy
- B. Venlafaxine therapy
- C. Cognitive behavioral therapy (Correct Answer)
- D. Motivational interviewing
- E. Prazosin therapy
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Cognitive behavioral therapy***
- **Cognitive Behavioral Therapy (CBT)** is considered a first-line psychological treatment for **Post-Traumatic Stress Disorder (PTSD)**, which the patient's symptoms (deployments, intrusive thoughts, nightmares, avoidance, guilt) strongly suggest.
- CBT helps individuals identify and challenge **maladaptive thought patterns** and behaviors related to the trauma, fostering new coping mechanisms.
*Dialectical behavioral therapy*
- **Dialectical Behavioral Therapy (DBT)** is primarily used for individuals with **Borderline Personality Disorder** or severe emotional dysregulation.
- While it can help with emotional regulation, it is not the **first-line therapy** specifically targeting trauma-related cognitive distortions and avoidance behaviors seen in PTSD.
*Venlafaxine therapy*
- **Venlafaxine**, an SNRI, is an antidepressant that can be effective for PTSD symptoms. However, current guidelines recommend **psychotherapy (like CBT)** as the initial step, especially when feasible.
- While pharmacotherapy can be used, it's typically considered **adjunctive** or for cases where psychotherapy alone is insufficient or not preferred.
*Motivational interviewing*
- **Motivational interviewing** is a patient-centered counseling style used to address ambivalence and enhance a person's **intrinsic motivation** for change.
- It is often utilized in substance abuse treatment or when patients are resistant to treatment, but it is not a primary, standalone treatment for the core symptoms of PTSD.
*Prazosin therapy*
- **Prazosin** is an alpha-1 antagonist used off-label to treat **PTSD-related nightmares** and sleep disturbances.
- While it can be helpful for a specific symptom, it does not address the broader spectrum of PTSD symptoms, such as intrusive thoughts, avoidance, or negative cognitions.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 5: A 19-year-old man presents to the emergency room after a suicidal gesture following a fight with his new girlfriend. He tearfully tells you that she is “definitely the one," unlike his numerous previous girlfriends, who were "all mean and selfish” and with whom he frequently fought. During this fight, his current girlfriend suggested that they spend time apart, so he opened a window and threatened to jump unless she promised to never leave him. You gather that his other relationships have ended in similar ways. He endorses impulsive behaviors and describes his moods as “intense” and rapidly changing in response to people around him. He often feels “depressed” for one day and then elated the next. You notice several superficial cuts and scars on the patient’s arms and wrists, and he admits to cutting his wrists in order to “feel something other than my emptiness.” Which of the following is the most likely diagnosis for this patient?
- A. Bipolar I disorder
- B. Major depressive disorder
- C. Borderline personality disorder (Correct Answer)
- D. Bipolar II disorder
- E. Histrionic personality disorder
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Borderline personality disorder***
- This patient exhibits characteristic features of **borderline personality disorder (BPD)**, including a pattern of **unstable relationships** marked by idealization ("definitely the one") and devaluation ("all mean and selfish").
- Other key features are **impulsivity** (suicidal gesture, cutting), **affective instability** ("intense" and rapidly changing moods), chronic feelings of **emptiness**, and a history of **self-harm** (superficial cuts and scars).
*Bipolar I disorder*
- While the patient describes rapidly changing and "intense" moods, the rapid shifts over days and reactivity to others are more characteristic of **mood lability** in BPD than distinct **manic or hypomanic episodes** lasting several days or longer, which define bipolar disorder.
- The suicidal gesture stemming from interpersonal conflict and fear of abandonment, combined with chronic self-harm, points strongly away from a primary mood disorder.
*Major depressive disorder*
- Although the patient reports feeling "depressed," the predominant features are not a persistent depressed mood or anhedonia but rather **unstable relationships**, **impulsivity**, and **affective dysregulation** beyond typical depressive symptoms.
- The "elated" periods described are also inconsistent with unipolar depression.
*Bipolar II disorder*
- This diagnosis requires a history of at least one **major depressive episode** and at least one **hypomanic episode**. While the patient describes mood shifts, they are described as "rapidly changing in response to people around him" and lasting for a day, which is more consistent with **affective instability** seen in BPD rather than sustained hypomanic episodes.
- The prominent features of self-harm and unstable relationships are not central to Bipolar II disorder.
*Histrionic personality disorder*
- Patients with **histrionic personality disorder** typically display excessive emotionality and attention-seeking behavior, often with a theatrical presentation.
- While there may be some overlap in attention-seeking aspects (suicidal gesture), the profound **instability of mood**, chronic **emptiness**, self-harm, and intense **fear of abandonment** are core to BPD and less characteristic of histrionic traits.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 6: A 33-year-old man with documented antisocial personality disorder and substance use disorder is convicted of assault. The defense attorney requests psychiatric testimony that the defendant's personality disorder diminished his capacity to conform his conduct to the law. His history includes multiple prior convictions, repeated lying, failure to sustain employment, lack of remorse, and disregard for others' safety. However, he understood the wrongfulness of his actions and planned the assault in advance. Evaluate the relationship between antisocial personality disorder and criminal responsibility.
- A. Chronic pattern of behavior demonstrates inability to conform conduct to law
- B. Combination of personality disorder and substance use negates criminal responsibility
- C. Comorbid substance use disorder supports insanity defense
- D. Antisocial personality disorder does not meet criteria for insanity defense as patients retain capacity to understand wrongfulness (Correct Answer)
- E. Personality disorders qualify for diminished capacity due to impaired impulse control
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Antisocial personality disorder does not meet criteria for insanity defense as patients retain capacity to understand wrongfulness***
- In forensic psychiatry, individuals with **antisocial personality disorder** are generally considered criminally responsible because they retain the **cognitive capacity** to distinguish right from wrong.
- The legal system distinguishes between a "cannot conform" (e.g., severe psychosis) and a "will not conform" (personality disorder); since the defendant **planned the assault**, he demonstrated **volitional control**.
*Chronic pattern of behavior demonstrates inability to conform conduct to law*
- A history of repeated legal infractions reflects a **choice to disregard social norms** rather than an organic or psychotic inability to process reality.
- Under most legal standards, inclusive of the **M'Naghten Rule**, a repetitive criminal history does not constitute the "mental disease or defect" required for an **insanity defense**.
*Combination of personality disorder and substance use negates criminal responsibility*
- Combined pathology does not equate to a loss of **mens rea** (guilty mind); substance use is often viewed as **voluntary intoxication**, which rarely excuses criminal acts.
- The presence of these disorders does not inherently impair the defendant's **rational understanding** of the wrongfulness of the specific criminal act.
*Comorbid substance use disorder supports insanity defense*
- **Substance use disorders** are specifically excluded from the definition of "mental disease or defect" in the context of the **insanity defense** in many jurisdictions.
- To qualify for insanity, a condition must typically involve a disconnection from reality, whereas substance use is considered a **behavioral choice** with known legal risks.
*Personality disorders qualify for diminished capacity due to impaired impulse control*
- **Diminished capacity** is a specific legal defense that usually requires a severe mental impairment that prevents the formation of **specific intent**, which is not seen here as the defendant **planned the assault**.
- While patients with personality disorders exhibit **impulsivity**, they still possess the foundational **legal sanity** required to be held responsible for premeditated actions.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 7: A 26-year-old woman presents requesting cosmetic surgery consultation. She is preoccupied with achieving the 'perfect' appearance, has undergone multiple procedures, and expresses disappointment with each result. She describes herself as special and destined for greatness, becomes enraged when her primary care physician suggested psychiatric evaluation, and states she will report him for 'not understanding her needs.' She expects special treatment in the clinic and becomes irritated when kept waiting. On mental status exam, she shows intact reality testing. Analyze the most likely underlying personality structure.
- A. Histrionic personality disorder with attention-seeking behavior
- B. Obsessive-compulsive personality disorder with perfectionism
- C. Borderline personality disorder with identity disturbance
- D. Narcissistic personality disorder with difficulty tolerating narcissistic injury (Correct Answer)
- E. Body dysmorphic disorder with poor insight
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Narcissistic personality disorder with difficulty tolerating narcissistic injury***
- The patient exhibits core features of **Narcissistic Personality Disorder (NPD)**, including a **grandiose sense of self-importance**, beliefs of being "special," and an extreme **sense of entitlement** regarding special treatment in the clinic.
- Her enraged reaction to the suggestion of a psychiatric evaluation is a classic example of **narcissistic rage**, which occurs after a **narcissistic injury** (a threat to one's inflated self-image or perceived perfection).
*Histrionic personality disorder with attention-seeking behavior*
- While both can involve vanity, histrionic patients are typically **emotionally labile** and seek any kind of attention, rather than specifically requiring **admiration and status**.
- This patient's **grandiosity** and entitlement differ from the **theatricality** and shallow emotional expression characteristic of histrionic behavior.
*Obsessive-compulsive personality disorder with perfectionism*
- Perfectionism in OCPD is driven by **rigidity**, a need for **control**, and preoccupation with rules rather than a desire for a "perfect" grandiose physical appearance.
- Unlike this patient, individuals with OCPD are typically **ego-syntonic regarding their work ethic** but lack the **arrogance** and self-aggrandizement seen here.
*Borderline personality disorder with identity disturbance*
- Borderline patients primarily experience **affective instability**, **fear of abandonment**, and chronic feelings of emptiness, which are not described in this scenario.
- While both can involve rage, borderline rage is usually triggered by **rejection or loss**, whereas this patient's rage stems from a blow to her **ego and superiority**.
*Body dysmorphic disorder with poor insight*
- Although she is preoccupied with her appearance, the pervasive pattern of **grandiosity**, **lack of empathy**, and **entitlement** suggests a personality structure rather than an isolated body image disorder.
- Patients with **Body Dysmorphic Disorder (BDD)** usually present with shame or distress over specific "defects" rather than a belief that they are **"destined for greatness."**
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 8: A 50-year-old man is brought for evaluation by his wife who reports 25 years of strange behavior. He has no close friends, prefers solitary activities, shows little emotion even at family events, and appears indifferent to praise or criticism. He works as a night security guard and has never desired a romantic relationship beyond the marriage his family arranged. He denies hallucinations or paranoia. On exam, he shows restricted affect but is cooperative and logical. What distinguishes this presentation from schizoid personality disorder with comorbid depression?
- A. Preserved occupational functioning despite social isolation
- B. Family history negative for mood disorders
- C. Lack of response to antidepressant medication
- D. Lifelong pattern present before any mood symptoms with no anhedonia complaints (Correct Answer)
- E. Absence of neurovegetative symptoms of depression
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Lifelong pattern present before any mood symptoms with no anhedonia complaints***
- **Schizoid personality disorder** is characterized by a pervasive, **lifelong pattern** of social detachment and emotional restrictedness that is **ego-syntonic**, meaning the patient does not perceive it as a problem.
- Unlike depression, which typically involves a discrete change from baseline and subjective **anhedonia** (distress over the loss of interest), this patient has never desired social connection and remains **content** in his isolation.
*Preserved occupational functioning despite social isolation*
- While common in schizoid personality disorder, occupational functioning does not reliably rule out **comorbid depression**, as many high-functioning individuals maintain work duties while depressed.
- Functional status is less diagnostically definitive than the **longitudinal history** and the presence or absence of subjective distress.
*Family history negative for mood disorders*
- A negative family history does not exclude a diagnosis of **Major Depressive Disorder**, nor does it confirm a **personality disorder**.
- While mood disorders have a genetic component, diagnosis is based on the patient's **clinical presentation** and symptom timeline rather than heritage.
*Lack of response to antidepressant medication*
- Medication response is not a diagnostic criterion; many patients with **treatment-resistant depression** may fail to respond to antidepressants.
- **Personality disorders** are primarily managed with therapy, but the lack of response to a pill does not distinguish the underlying etiology of the social withdrawal.
*Absence of neurovegetative symptoms of depression*
- While the absence of sleep or appetite changes argues against depression, certain types like **atypical depression** may exhibit different patterns.
- The most defining feature for this diagnosis remains the **pervasive, lifelong lack of desire** for relationships, rather than just the absence of physical signs of a mood episode.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 9: A 29-year-old woman with borderline personality disorder presents to the emergency department after superficial self-cutting following an argument with her boyfriend. She demands admission, stating 'I'll kill myself if you send me home.' She has had 15 psychiatric hospitalizations in the past 3 years, typically lasting 2-3 days. Her outpatient therapist reports she is engaged in DBT and makes these threats regularly to avoid distress. She denies intent or plan for suicide, vital signs are stable, cuts are superficial. What is the most therapeutic management approach?
- A. Admit to observation unit for 24-hour monitoring
- B. Involuntary commitment for repeated self-harm behavior
- C. Admit to inpatient psychiatric unit to ensure safety
- D. Discharge with crisis resources and DBT therapist follow-up (Correct Answer)
- E. Prescribe anxiolytics and discharge with next-day psychiatry appointment
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Discharge with crisis resources and DBT therapist follow-up***
- In **Borderline Personality Disorder (BPD)**, repetitive brief hospitalizations often reinforce **maladaptive coping** and regression rather than providing therapeutic benefit.
- Since the patient has no **suicidal intent or plan** and is active in **Dialectical Behavior Therapy (DBT)**, the most therapeutic approach is to encourage distress tolerance in the outpatient setting.
*Admit to observation unit for 24-hour monitoring*
- Short-term monitoring can inadvertently validate the use of **self-harm as a communication tool**, undermining the goals of outpatient therapy.
- This approach fails to address the underlying pattern of **instrumental suicide threats** used to avoid immediate emotional distress.
*Involuntary commitment for repeated self-harm behavior*
- The Patient does not meet legal criteria for **involuntary commitment** as she explicitly denies a specific suicide plan or intent.
- Commitment is often counter-therapeutic in stable BPD patients, as it can worsen **splitting** and create dependency on the inpatient system.
*Admit to inpatient psychiatric unit to ensure safety*
- Frequent inpatient admissions for patients with BPD are associated with **iatrogenic harm** and a decrease in the patient's long-term ability to self-soothe.
- Safety is better managed through a **crisis plan** and coordination with her existing **DBT therapist** rather than environmental containment.
*Prescribe anxiolytics and discharge with next-day psychiatry appointment*
- **Benzodiazepines** and other anxiolytics should be avoided in BPD due to the high risk of **disinhibition**, substance misuse, and overdose potential.
- Providing immediate medication reinforcements for self-harm behaviors can interfere with the patient's **behavioral modification** and skill acquisition in therapy.
Psychotherapeutic approaches (DBT, MBT) US Medical PG Question 10: A 38-year-old man with antisocial personality disorder is admitted to the medical service for endocarditis from IV drug use. He is charming with nurses but becomes hostile when confronted about treatment non-adherence. He was found attempting to obtain opioids by feigning pain severity. The team is divided: some staff want to discharge him for manipulative behavior, while others advocate for continued treatment. He has violated unit rules multiple times. As the consulting psychiatrist, what is the most appropriate recommendation?
- A. Transfer to psychiatric facility for personality disorder treatment
- B. Implement one-to-one observation to prevent manipulation
- C. Continue medical treatment with firm behavioral contingencies and consistent limit-setting (Correct Answer)
- D. Discharge patient immediately due to manipulative behavior endangering staff
- E. Increase opioid medication to improve therapeutic alliance
Psychotherapeutic approaches (DBT, MBT) Explanation: ***Continue medical treatment with firm behavioral contingencies and consistent limit-setting***
- Patients with **antisocial personality disorder** require necessary medical care for life-threatening conditions like **endocarditis**, despite challenging social behaviors.
- Management hinges on **consistent limit-setting** and clear communication among all staff to minimize **splitting behaviors** and manipulative rule-breaking.
*Transfer to psychiatric facility for personality disorder treatment*
- A psychiatric facility is generally unequipped to manage acute **intravenous antibiotic therapy** and medical complications of **endocarditis**.
- Movement to a different facility does not address the primary behavioral issues and only delays necessary **medical stabilization**.
*Implement one-to-one observation to prevent manipulation*
- **One-to-one observation** is a resource-intensive intervention typically reserved for acute **suicidality** or **self-harm**, not for managing personality traits.
- This approach may inadvertently reinforce **maladaptive attention-seeking** behaviors rather than encouraging patient accountability.
*Discharge patient immediately due to manipulative behavior endangering staff*
- **Immediate discharge** for non-violent manipulation constitutes **patient abandonment** when treating a high-mortality condition like endocarditis.
- While the behavior is disruptive, it does not currently pose a direct **physical safety threat** that would justify the ethical breach of denying life-saving care.
*Increase opioid medication to improve therapeutic alliance*
- Increasing opioids in a patient with **IV drug use** and **malingering** symptoms reinforces drug-seeking behavior and worsens the addiction cycle.
- **Therapeutic alliance** with antisocial patients is built through clear, predictable boundaries, not by conceding to manipulative demands.
More Psychotherapeutic approaches (DBT, MBT) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.