Personality disorders

On this page
🧠 The Personality Architecture: Understanding Enduring Patterns
Personality disorders represent some of medicine's most challenging diagnoses-not because they're rare, but because they shape every clinical encounter in ways that can confound even experienced practitioners. You'll learn to recognize the enduring patterns that distinguish personality pathology from transient symptoms, master the frameworks that separate overlapping presentations, and build therapeutic strategies that actually work when standard approaches fail. This isn't about memorizing criteria; it's about developing the clinical intuition to see how deeply ingrained patterns of thinking, feeling, and relating create both suffering and resistance to change. By integrating diagnostic precision with practical intervention tools, you'll transform these complex patients from frustrating puzzles into opportunities for meaningful clinical impact.
📌 Remember: STABLE - Significant distress, Traits inflexible, Across situations, By early adulthood, Lasting patterns, Ego-syntonic (feels normal to patient)
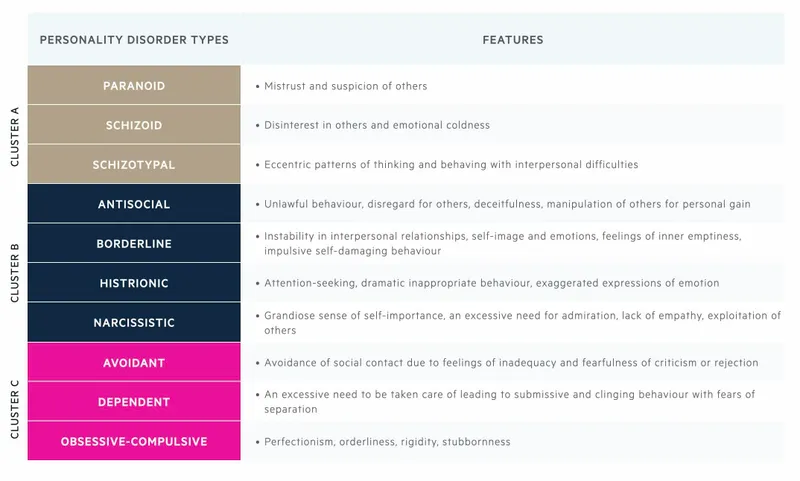
The DSM-5 organizes personality disorders into three distinct clusters based on descriptive similarities:
- Cluster A (Odd/Eccentric): 3 disorders affecting 0.7-2.4% of population
- Paranoid PD: 0.8-2.4% prevalence
- Schizoid PD: 0.8% prevalence
- Schizotypal PD: 0.6% prevalence
- Cluster B (Dramatic/Emotional): 4 disorders with highest clinical impact
- Antisocial PD: 0.5-1.9% prevalence, 3:1 male predominance
- Borderline PD: 0.7-2.7% prevalence, 75% female
- Histrionic PD: 1.84% prevalence
- Narcissistic PD: 1-6% prevalence, 7.7% male vs 4.8% female
- Cluster C (Anxious/Fearful): 3 disorders with high comorbidity rates
- Avoidant PD: 1.2% prevalence
- Dependent PD: 0.49-0.6% prevalence
- Obsessive-Compulsive PD: 2.1-7.9% prevalence
⭐ Clinical Pearl: Personality disorders show 85% diagnostic stability over 6-year follow-up periods, making early recognition crucial for long-term management planning.
| Cluster | Core Features | Prevalence | Gender Ratio | Comorbidity Risk |
|---|---|---|---|---|
| A (Odd) | Social withdrawal, cognitive distortions | 0.6-2.4% | Equal | High psychotic risk |
| B (Dramatic) | Emotional dysregulation, impulsivity | 0.5-6% | Variable | High Axis I disorders |
| C (Anxious) | Anxiety, fear-based behaviors | 0.49-7.9% | Slight female | High anxiety/mood |
💡 Master This: Personality disorders are ego-syntonic (feel normal to the patient) versus Axis I disorders which are ego-dystonic (feel abnormal). This fundamental difference explains why <40% of personality disorder patients seek treatment voluntarily.
The neurobiological foundation involves dysregulation in key brain circuits:
- Prefrontal cortex: Executive function and impulse control (20-30% volume reduction in Cluster B)
- Amygdala: Emotional processing (hyperactivity in 60% of borderline patients)
- Anterior cingulate: Social cognition and empathy (reduced connectivity in antisocial PD)
Understanding these architectural patterns provides the foundation for recognizing how specific personality configurations create predictable clinical presentations and treatment challenges.
🧠 The Personality Architecture: Understanding Enduring Patterns
🎭 The Dramatic Cluster: Emotional Storms and Interpersonal Chaos
📌 Remember: WILD Cluster B - Wild emotions, Impulsive behaviors, Labile relationships, Dramatic presentations
Borderline Personality Disorder represents the prototype of emotional instability:
- Prevalence: 0.7-2.7% general population, 75% female predominance
- Suicide risk: 8-10% completion rate, 75% attempt at least once
- Hospitalization: 5.9 days average length of stay vs 4.1 days for other psychiatric conditions
- Healthcare costs: $18,000 annually per patient (3x higher than depression)
Antisocial Personality Disorder shows the most concerning behavioral patterns:
- Criminal involvement: 47% of male prisoners meet criteria
- Substance abuse: 90% lifetime prevalence of substance use disorders
- Violence risk: 4-8x higher than general population
- Treatment dropout: >70% discontinue therapy within 6 months
⭐ Clinical Pearl: Cluster B disorders show 50-70% comorbidity with substance use disorders, compared to 15-20% in general population. Screen aggressively for dual diagnosis.
Narcissistic Personality Disorder demonstrates the grandiosity-vulnerability paradox:
- Prevalence: 1-6% general population, 7.7% males vs 4.8% females
- Comorbidity: 40% develop major depression, 24% bipolar disorder
- Relationship stability: <30% maintain long-term partnerships
- Occupational impact: 2.5x higher job turnover rates
Histrionic Personality Disorder features attention-seeking behaviors:
- Prevalence: 1.84% general population, slight female predominance
- Emotional expression: Rapidly shifting and shallow emotions
- Suggestibility: High vulnerability to influence and manipulation
- Somatic complaints: 3x higher medical utilization without organic cause
💡 Master This: Cluster B splitting behaviors create staff conflicts in 85% of inpatient admissions. Consistent treatment team communication and clear boundaries prevent therapeutic sabotage.
| Disorder | Core Drive | Relationship Pattern | Crisis Trigger | Treatment Response |
|---|---|---|---|---|
| Borderline | Abandonment fear | Intense, unstable | Perceived rejection | DBT most effective |
| Antisocial | Power/control | Exploitative | Legal consequences | Poor prognosis |
| Narcissistic | Admiration need | Entitled, superior | Criticism/failure | Fragile engagement |
| Histrionic | Attention seeking | Dramatic, shallow | Being ignored | Moderate response |
🎭 The Dramatic Cluster: Emotional Storms and Interpersonal Chaos
🔍 Pattern Recognition Mastery: The Clinical Detective Framework
📌 Remember: CONTEXT - Consistency across situations, Onset by early adulthood, Not better explained by other disorders, Time duration (pervasive pattern), Ego-syntonic presentation, X-ray the interpersonal style, Threshold for functional impairment
Consistency Markers distinguish personality traits from episodic symptoms:
- Temporal stability: Patterns present for >2 years minimum
- Situational pervasiveness: Evident across ≥3 life domains (work, relationships, social)
- Stress independence: Behaviors persist during stable periods
- Cultural deviation: Patterns markedly different from cultural norms
"See This, Think That" Clinical Correlations:
- Chronic emptiness + self-harm → Borderline PD (90% sensitivity)
- Grandiosity + exploitation → Narcissistic PD (85% specificity)
- Social withdrawal + odd beliefs → Schizotypal PD (80% positive predictive value)
- Rule violations + lack remorse → Antisocial PD (95% specificity when both present)
- Perfectionism + rigidity → OCPD (75% sensitivity)
High-Yield Assessment Questions:
- Relationship patterns: "Describe your three most important relationships"
- Conflict resolution: "How do you handle disagreements with others?"
- Self-perception: "What would others say are your strengths and weaknesses?"
- Stress responses: "How do you cope when things don't go your way?"
⭐ Clinical Pearl: Collateral information increases diagnostic accuracy by 40-60%. Personality disorders create blind spots in self-reporting due to ego-syntonic nature.
Differential Diagnosis Red Flags:
- Mood episodes: Temporal relationship distinguishes personality vs. mood disorders
- Substance use: Clean periods reveal underlying personality patterns
- Medical conditions: Neurological screening rules out organic causes
- Cultural factors: Immigration/acculturation stress can mimic personality pathology
Assessment Timeline Optimization:
- Initial screening: 15-20 minutes using structured questions
- Comprehensive evaluation: 2-3 sessions over 4-6 weeks
- Collateral interviews: 30 minutes with family/friends when possible
- Psychological testing: MMPI-2 or PAI for complex cases
💡 Master This: Axis I symptoms are ego-dystonic (patient wants relief), while personality features are ego-syntonic (patient sees as normal). This distinction guides treatment engagement strategies.
| Assessment Domain | Key Questions | Red Flag Responses | Diagnostic Weight |
|---|---|---|---|
| Interpersonal | Relationship stability | "People always disappoint me" | High |
| Emotional | Mood regulation | "I go from 0-100 instantly" | High |
| Behavioral | Impulse control | "I act first, think later" | Moderate |
| Cognitive | Self-perception | "Rules don't apply to me" | High |
| Occupational | Work history | Multiple job losses | Moderate |
🔍 Pattern Recognition Mastery: The Clinical Detective Framework
⚖️ The Differential Diagnosis Matrix: Separating Signal from Noise
📌 Remember: TEMPORAL - Timing of onset, Episodic vs. persistent, Mood congruence, Pervasiveness across contexts, Organic rule-outs, Relationship to stressors, Age-appropriate development, Level of functioning
Personality Disorders vs. Major Mental Illness:
Borderline PD vs. Bipolar Disorder represents the most challenging differential:
- Episode duration: Bipolar episodes last weeks-months, BPD mood swings occur hours-days
- Trigger dependence: BPD reactivity to interpersonal stressors (90% of episodes), bipolar episodes often spontaneous
- Interepisode functioning: Bipolar patients show normal functioning between episodes, BPD shows persistent instability
- Treatment response: Bipolar responds to mood stabilizers (70-80% response), BPD requires psychotherapy as primary intervention
Antisocial PD vs. Substance-Induced Behavior:
- Onset timing: ASPD behaviors present before age 15, substance use typically begins later
- Clean periods: ASPD patterns persist during sustained sobriety (>6 months)
- Motivation: ASPD shows primary antisocial drive, substance users may show secondary antisocial behavior
- Treatment response: Substance users show behavioral improvement with addiction treatment
⭐ Clinical Pearl: Comorbidity rates between personality disorders and Axis I conditions reach 60-80%. Don't assume either/or - systematic assessment often reveals dual diagnosis requiring integrated treatment.
Cluster-Specific Differentials:
Cluster A vs. Psychotic Spectrum:
- Schizotypal PD: Odd beliefs without frank delusions, social anxiety predominates
- Schizophrenia: Fixed delusions, hallucinations, marked functional decline
- Delusional Disorder: Circumscribed delusions with preserved functioning in other areas
Cluster B vs. Impulse Control Disorders:
- Borderline PD: Broad emotional dysregulation affecting multiple life domains
- Intermittent Explosive Disorder: Isolated aggressive episodes with normal interepisode functioning
Cluster C vs. Anxiety Disorders:
- Avoidant PD: Pervasive social inhibition since early adulthood
- Social Anxiety Disorder: Specific social fears with desire for social connection
💡 Master This: Longitudinal assessment over 6-12 months provides the most reliable differentiation. Personality patterns show remarkable consistency, while Axis I disorders show episodic variation.
| Differential | Key Distinguisher | Timeline | Functional Pattern | Treatment Response |
|---|---|---|---|---|
| PD vs Mood | Episodic vs persistent | Mood: weeks-months | Mood: episodic decline | Mood: medication responsive |
| PD vs Psychotic | Reality testing | Psychotic: acute onset | Psychotic: marked decline | Psychotic: antipsychotic response |
| PD vs Substance | Clean period behavior | Substance: variable | Substance: use-related | Substance: sobriety improvement |
| PD vs Anxiety | Pervasiveness | Anxiety: situational | Anxiety: specific triggers | Anxiety: CBT/medication response |
| PD vs Medical | Organic timeline | Medical: coincident | Medical: progressive | Medical: treat underlying condition |
- Structured interviews: SCID-II increases diagnostic reliability by 30-40%
- Longitudinal tracking: Mood charts over 3-6 months reveal patterns
- Collateral information: Family history and developmental timeline crucial
- Treatment trials: Response patterns provide diagnostic information
High-Risk Misdiagnosis Scenarios:
- Adolescent presentations: Personality disorder diagnosis requires caution before age 18
- Acute crisis states: Stress-related symptoms can mimic personality pathology
- Cultural considerations: Behavior patterns must be culturally inappropriate
- Cognitive impairment: Dementia or intellectual disability can confound assessment
This systematic approach to differential diagnosis prevents the 30-40% misdiagnosis rate seen in personality disorders, ensuring appropriate treatment selection and improved patient outcomes.
⚖️ The Differential Diagnosis Matrix: Separating Signal from Noise
🎯 Treatment Architecture: Building Therapeutic Frameworks
Treatment Hierarchy follows the STRUCTURE principle:
📌 Remember: STRUCTURE - Safety first, Therapeutic alliance, Regulation skills, Underlying patterns, Coping strategies, Trauma processing, Understanding relationships, Relapse prevention, Ending therapy
Evidence-Based Psychotherapy Approaches:
Dialectical Behavior Therapy (DBT) for Borderline PD:
- Efficacy: 77% reduction in suicide attempts over 1 year
- Components: 4 modules - mindfulness, distress tolerance, emotion regulation, interpersonal effectiveness
- Duration: 12-24 months intensive treatment
- Outcomes: 50% no longer meet BPD criteria at 2-year follow-up
Mentalization-Based Therapy (MBT) for severe personality disorders:
- Target: Improving capacity to understand mental states underlying behavior
- Format: Individual + group therapy combination
- Duration: 18-month minimum treatment course
- Results: 41% reduction in suicide attempts, 76% reduction in self-harm
Pharmacotherapy Principles:
Symptom-Domain Targeting rather than disorder-specific treatment:
- Emotional dysregulation: Mood stabilizers (lamotrigine 200mg, valproate 1000-1500mg)
- Impulsivity/aggression: Atypical antipsychotics (olanzapine 5-10mg, aripiprazole 10-15mg)
- Anxiety/depression: SSRIs (fluoxetine 20-40mg, sertraline 100-200mg)
- Cognitive symptoms: Low-dose antipsychotics (risperidone 0.5-2mg)
⭐ Clinical Pearl: Polypharmacy occurs in 60-80% of personality disorder patients. Regular medication reviews prevent dangerous interactions and unnecessary side effects.
Cluster-Specific Treatment Approaches:
Cluster A (Odd/Eccentric):
- Social skills training: 12-16 week programs show moderate improvement
- Cognitive remediation: Targets executive function deficits
- Low-dose antipsychotics: For cognitive-perceptual symptoms
- Prognosis: Limited improvement but functional stability achievable
Cluster B (Dramatic/Emotional):
- DBT: Gold standard for borderline PD (Level A evidence)
- Schema therapy: 18-month programs show superior outcomes to DBT for some patients
- Therapeutic communities: For antisocial PD with substance use
- Prognosis: Variable - borderline shows good response, antisocial shows poor response
Cluster C (Anxious/Fearful):
- CBT: 16-20 sessions show 60-70% improvement rates
- Exposure therapy: For avoidant PD social fears
- Assertiveness training: For dependent PD autonomy building
- Prognosis: Best overall outcomes among personality disorder clusters
💡 Master This: Therapeutic alliance predicts treatment outcome more strongly than specific intervention type. Invest 6-8 sessions in relationship building before intensive work.
| Treatment Modality | Target Population | Duration | Success Rate | Key Components |
|---|---|---|---|---|
| DBT | Borderline PD | 12-24 months | 60-77% | Skills training, individual therapy |
| MBT | Severe PD | 18+ months | 50-65% | Mentalization focus, group work |
| Schema Therapy | Chronic PD | 24-36 months | 45-60% | Early maladaptive schemas |
| CBT | Cluster C | 16-20 sessions | 60-70% | Thought/behavior modification |
| Therapeutic Community | ASPD + SUD | 12-18 months | 30-40% | Peer confrontation, structure |
- High dropout rates: 40-60% discontinue treatment prematurely
- Crisis management: 24/7 support systems reduce hospitalizations by 50%
- Therapist burnout: Regular supervision and case consultation essential
- Family involvement: Psychoeducation improves treatment adherence by 30%
Outcome Measurement:
- Functional improvement: GAF scores increase 15-20 points with successful treatment
- Symptom reduction: 50% decrease in target behaviors considered clinically significant
- Quality of life: Relationship stability and occupational functioning key markers
- Long-term follow-up: 5-year outcomes show sustained improvement in 40-50% of patients
This comprehensive treatment architecture provides the foundation for transforming entrenched personality patterns into adaptive functioning across multiple life domains.
🎯 Treatment Architecture: Building Therapeutic Frameworks
🔗 The Integration Matrix: Multi-System Clinical Mastery
Neurobiological Integration reveals the brain-behavior connections underlying personality pathology:
Prefrontal-Limbic Circuitry dysfunction creates the core features:
- Dorsolateral PFC: Executive function deficits → poor impulse control (30-40% volume reduction in Cluster B)
- Ventromedial PFC: Emotional regulation impairment → affective instability (reduced connectivity in 60% of BPD patients)
- Amygdala hyperactivity: Threat detection hypersensitivity → interpersonal reactivity (2-3x normal activation)
- Anterior cingulate: Social cognition deficits → empathy impairment (structural abnormalities in 70% of ASPD)
Genetic-Environmental Interactions shape personality development:
- Heritability: 40-60% for most personality disorders
- Gene-environment correlation: High-risk genes + adverse environments = exponential risk increase
- Epigenetic factors: Childhood trauma alters gene expression for decades
- Developmental timing: Critical periods during adolescence for personality consolidation
📌 Remember: BIOPSYCHOSOCIAL - Brain circuits, Inflammation markers, Oxytocin/cortisol, Psychological defenses, Social learning, Youth trauma, Cultural context, Hormonal influences, Occupational stress, Support systems, Other medical conditions, Cognitive patterns, Interpersonal patterns, Attachment styles, Life transitions
Comorbidity Patterns require integrated treatment approaches:
Personality Disorders + Substance Use (60-80% comorbidity):
- Self-medication hypothesis: Emotional dysregulation drives substance use
- Treatment sequence: Stabilize substance use before intensive personality work
- Integrated programs: Dual diagnosis treatment shows superior outcomes (40% vs 20% abstinence rates)
Personality Disorders + Trauma History (70-90% in Cluster B):
- Complex PTSD: Overlapping symptoms with personality pathology
- Treatment integration: Trauma-informed approaches essential
- Phase-based treatment: Stabilization → Trauma processing → Integration
⭐ Clinical Pearl: Medical comorbidities occur 2-3x more frequently in personality disorder patients. Screen for diabetes, cardiovascular disease, and autoimmune conditions - chronic stress creates systemic inflammation.
Cutting-Edge Research Integration:
Inflammation and Personality Disorders:
- Elevated CRP: 2-3x higher in Cluster B disorders
- Cytokine dysregulation: IL-6 and TNF-α correlate with emotional instability
- Treatment implications: Anti-inflammatory approaches show promising results
Oxytocin and Social Functioning:
- Reduced oxytocin: 40-50% lower in antisocial and narcissistic PD
- Intranasal oxytocin: Experimental treatment for empathy deficits
- Social cognition: Oxytocin receptor polymorphisms predict treatment response
Microbiome-Gut-Brain Axis:
- Dysbiosis: Altered gut bacteria in 60% of personality disorder patients
- Serotonin production: 90% occurs in gut - microbiome affects mood regulation
- Probiotic interventions: Emerging treatment for emotional dysregulation
💡 Master This: Personality disorders are system-level disorders requiring multi-modal interventions. Medication alone shows limited efficacy (<30% improvement), while integrated approaches achieve 60-70% improvement rates.
| Integration Domain | Key Interactions | Clinical Implications | Treatment Modifications |
|---|---|---|---|
| Neuro-Psychological | Brain circuits + cognition | Cognitive remediation needed | Add neurofeedback/cognitive training |
| Bio-Social | Genetics + environment | Family therapy essential | Include genetic counseling |
| Trauma-Personality | PTSD + personality features | Phase-based treatment | Trauma-informed modifications |
| Medical-Psychiatric | Physical + mental health | Integrated medical care | Collaborative treatment teams |
| Cultural-Individual | Society + personal patterns | Culturally adapted therapy | Modified treatment approaches |
- Neuropsychological testing: Executive function assessment guides treatment planning
- Biomarker panels: Inflammatory markers and stress hormones inform medication choices
- Attachment assessment: Adult Attachment Interview predicts therapeutic alliance
- Family assessment: Expressed emotion levels affect treatment outcomes
System-Level Interventions:
- Multidisciplinary teams: Psychiatrist, psychologist, social worker, case manager
- Family interventions: Psychoeducation and skills training for family members
- Community resources: Peer support groups and vocational rehabilitation
- Crisis systems: 24/7 support and brief hospitalization protocols
This integrated understanding transforms personality disorder treatment from symptom management into comprehensive system modification, addressing the multiple levels of dysfunction that maintain these complex conditions.
🔗 The Integration Matrix: Multi-System Clinical Mastery
🎯 Clinical Mastery Arsenal: Rapid Assessment and Intervention Tools
The 5-Minute Personality Screen for emergency and primary care settings:
📌 Remember: QUICK PD - Quick mood swings, Unstable relationships, Impulsive behaviors, Chronic emptiness, Key interpersonal problems, Persistent patterns, Distress/dysfunction
Rapid Cluster Identification:
- Cluster A: "Do you prefer being alone?" + "Do others think you're odd?" (85% sensitivity)
- Cluster B: "Do your emotions change rapidly?" + "Do you have relationship problems?" (90% sensitivity)
- Cluster C: "Are you often anxious or worried?" + "Do you avoid new situations?" (80% sensitivity)
Crisis Risk Stratification using the SAFER model:
- Suicide risk: BPD = 8-10% lifetime risk, immediate assessment required
- Aggression potential: ASPD = 4-8x violence risk, safety planning essential
- Functional impairment: GAF <50 indicates severe dysfunction
- Emergency contacts: Collateral information crucial for safety planning
- Resource activation: Crisis team, family support, hospitalization criteria
Essential Clinical Thresholds:
- Hospitalization criteria: Active suicidality + plan/means + poor impulse control
- Medication initiation: Functional impairment affecting ≥2 life domains
- Intensive therapy: Recurrent crises (≥3 per month) or self-harm behaviors
- Family involvement: High expressed emotion or enabling behaviors present
⭐ Clinical Pearl: Personality disorder patients consume 3-5x more healthcare resources than average. Early recognition and appropriate referral prevent costly crisis cycles.
Medication Quick Reference:
| Symptom Target | First-Line | Dose Range | Monitoring | Response Timeline |
|---|---|---|---|---|
| Emotional dysregulation | Lamotrigine | 100-200mg | Rash, mood | 6-8 weeks |
| Impulsivity/aggression | Aripiprazole | 10-15mg | Weight, EPS | 2-4 weeks |
| Anxiety/depression | Sertraline | 100-200mg | Suicidality | 4-6 weeks |
| Cognitive symptoms | Risperidone | 0.5-2mg | EPS, prolactin | 1-2 weeks |
| Sleep disturbance | Trazodone | 50-150mg | Sedation | 1-3 days |
- DBT: Borderline PD with recurrent self-harm or suicidality
- CBT: Cluster C disorders with anxiety/avoidance patterns
- Schema Therapy: Chronic, treatment-resistant personality disorders
- Group therapy: Social skills deficits or interpersonal problems
- Family therapy: Adolescent presentations or family dysfunction
💡 Master This: Therapeutic alliance forms within first 3 sessions and predicts treatment outcome more than diagnosis type. Invest early in relationship building and collaborative goal setting.
Documentation Essentials for medicolegal protection:
- Risk assessment: Specific factors evaluated and interventions implemented
- Capacity evaluation: Decision-making ability for treatment consent
- Safety planning: Detailed plan with specific triggers and coping strategies
- Collateral contacts: Family notification and release of information status
- Treatment recommendations: Specific referrals with urgency level indicated
Prognosis Indicators:
Good Prognosis Factors:
- Treatment motivation and insight present
- Stable housing and social support
- No active substance use
- Higher education and employment history
- Previous therapy experience
Poor Prognosis Factors:
- Antisocial features predominant
- Active substance abuse
- History of treatment non-compliance
- Severe childhood trauma
- Comorbid psychosis
Quality Metrics for personality disorder care:
- Diagnostic accuracy: >80% concordance with structured interviews
- Treatment retention: >60% complete 6-month treatment course
- Crisis reduction: 50% decrease in emergency visits within 1 year
- Functional improvement: 15-point increase in GAF scores
- Patient satisfaction: >70% report treatment helpfulness
System Integration Tools:
- Electronic alerts: Personality disorder flags in EMR systems
- Care coordination: Regular team meetings for complex cases
- Outcome tracking: Standardized measures at 3-month intervals
- Resource allocation: Intensive case management for high utilizers
This clinical mastery arsenal transforms personality disorder care from reactive crisis management into proactive, evidence-based intervention that optimizes patient outcomes while managing healthcare resources efficiently.
🎯 Clinical Mastery Arsenal: Rapid Assessment and Intervention Tools
Practice Questions: Personality disorders
Test your understanding with these related questions
A 55-year-old male was picked up by police in the public library for harassing the patrons and for public nudity. He displayed disorganized speech and believed that the books were the only way to his salvation. Identification was found on the man and his sister was called to provide more information. She described that he recently lost his house and got divorced within the same week although he seemed fine three days ago. The man was sedated with diazepam and chlorpromazine because he was very agitated. His labs returned normal and within three days, he appeared normal, had no recollection of the past several days, and discussed in detail how stressful the past two weeks of his life were. He was discharged the next day. Which of the following is the most appropriate diagnosis for this male?













