Motor disorders (tic disorders, stereotypic movement) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Motor disorders (tic disorders, stereotypic movement). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 1: An otherwise healthy 43-year-old woman comes to the physician because of several episodes of involuntary movements of her head over the past few months. They are sometimes associated with neck pain and last minutes to hours. Neurologic examination shows no abnormalities. During examination of the neck, the patient's head turns horizontally to the left. She states this movement is involuntary, and that she is unable to unturn her head. After 5 minutes, her head re-straightens. Which of the following best describes this patient's disorder?
- A. Dystonia (Correct Answer)
- B. Athetosis
- C. Akathisia
- D. Hemiballismus
- E. Chorea
Motor disorders (tic disorders, stereotypic movement) Explanation: ***Dystonia***
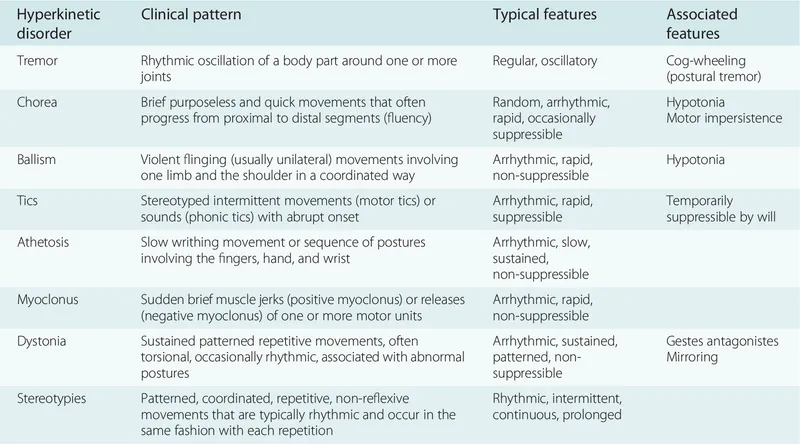
- This patient presents with **sustained, involuntary muscle contractions** causing repetitive, twisting movements and abnormal postures [1], which are characteristic features of **dystonia**, specifically **cervical dystonia (torticollis)**.
- The description of the head turning involuntarily to the left and inability to unturn it, lasting minutes to hours, fits the pattern of intermittent or spasmodic dystonia.
*Athetosis*
- **Athetosis** involves slow, sinuous, **writhing involuntary movements**, particularly affecting distal limbs [1].
- These movements are often continuous and slow, unlike the more sudden, sustained contractions seen in the patient.
*Akathisia*
- **Akathisia** is characterized by an internal feeling of **restlessness** and a strong urge to move, often described as an inability to sit still.
- It results in fidgeting and pacing, rather than sustained, involuntary posturing of a specific body part.
*Hemiballismus*
- **Hemiballismus** involves **large-amplitude, involuntary, flinging movements** of one side of the body [1].
- This symptom typically arises from lesions in the **subthalamic nucleus** and is distinct from the sustained, twisting movements described [1].
*Chorea*
- **Chorea** presents as **brief, irregular, rapid, and unpredictable involuntary movements** that flow randomly from one body part to another [1].
- Unlike the sustained, fixed posturing seen in dystonia, choreiform movements are often described as "dance-like" and are not maintained.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 2: A 5-year-old girl is brought to the physician because her mother has found her to be inattentive at home and has received multiple complaints from her teachers at school. She does not complete her assignments and does not listen to her teachers' instructions. She refuses to talk to her parents or peers. Her mother says, “She ignores everything I say to her!” She prefers playing alone, and her mother reports that she likes playing with 5 red toy cars, repeatedly arranging them in a straight line. She avoids eye contact with her mother and the physician throughout the visit. Physical and neurological examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Rett syndrome
- B. Conduct disorder
- C. Oppositional defiant disorder
- D. Attention deficit hyperactivity disorder
- E. Autism spectrum disorder (Correct Answer)
Motor disorders (tic disorders, stereotypic movement) Explanation: ***Autism spectrum disorder***
- The child exhibits core features of **autism spectrum disorder (ASD)**, including **social communication deficits** (refuses to talk, ignores parents, avoids eye contact) and **restricted, repetitive patterns of behavior** (playing with 5 red toy cars, repeatedly arranging them in a straight line).
- Her inattention and difficulty following instructions are also common in ASD, often related to focus on their specific interests rather than external demands, and **sensory processing differences** or **executive dysfunction**.
*Rett syndrome*
- This is a neurodevelopmental disorder almost exclusively affecting **females** and typically presents with a period of normal development followed by **regression of acquired skills**, especially **language and motor skills**.
- Key features include **stereotypic hand movements** (hand-wringing, squeezing), **gait abnormalities**, and **deceleration of head growth**, none of which are described in the patient.
*Conduct disorder*
- Characterized by a **persistent pattern of behavior** in which the basic rights of others or major age-appropriate societal norms or rules are violated, such as **aggression to people and animals**, **destruction of property**, deceitfulness or theft, and serious rule violations.
- The presented symptoms of social communication deficits and repetitive behaviors are not indicative of conduct disorder.
*Oppositional defiant disorder*
- Involves a pattern of **angry/irritable mood, argumentative/defiant behavior**, or **vindictiveness** lasting at least 6 months, often directed at authority figures.
- While the child may appear defiant by not listening, the broader constellation of **social communication deficits** and **repetitive behaviors** points away from ODD as the primary diagnosis.
*Attention deficit hyperactivity disorder*
- Presents with a persistent pattern of **inattention and/or hyperactivity-impulsivity** that interferes with functioning or development.
- Although the child is inattentive, the presence of **social communication difficulties** and **restricted, repetitive behaviors** are not characteristic of ADHD and are better explained by ASD.
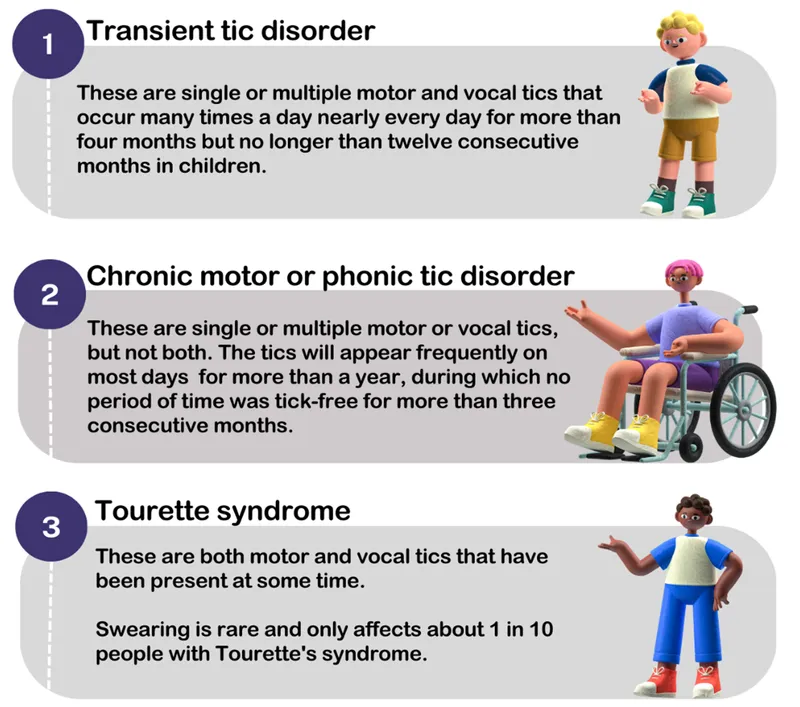
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 3: An 8-year-old girl is brought to the physician because of repetitive involuntary movements, including neck twisting, grimacing, grunting, and blinking, for the past 18 months. Her symptoms seem to improve with concentration and worsen with fatigue. During the past 3 months, they have become so severe that she has missed many school days. Her mother says she also has too much anxiety about her involuntary movements to see her friends and prefers staying home in her room. Her birth and development until 18 months ago were normal. Her father suffers from bipolar disorder. Vital signs are within normal limits. Mental status examination shows intact higher mental function and thought processes. Neurological examination shows multiple motor and vocal tics. Physical examination is otherwise within normal limits. Which of the following is the most appropriate initial pharmacotherapy for this condition?
- A. Fluoxetine
- B. Alprazolam
- C. Chlorpromazine
- D. Risperidone (Correct Answer)
- E. Buspirone
Motor disorders (tic disorders, stereotypic movement) Explanation: ***Risperidone***
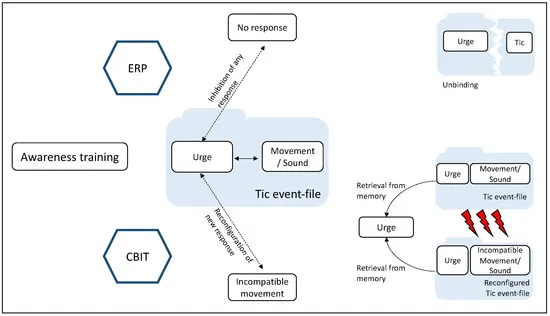
- This patient's symptoms are highly suggestive of **Tourette syndrome**, characterized by multiple motor and vocal tics persisting for over a year, and *risperidone*, an **atypical antipsychotic**, is a first-line treatment for severe tics.
- Risperidone works by blocking **D2 dopamine receptors**, which helps reduce the frequency and severity of tics, especially when symptoms cause functional impairment.
*Fluoxetine*
- *Fluoxetine* is a **selective serotonin reuptake inhibitor (SSRI)** primarily used to treat depression, anxiety, and obsessive-compulsive disorder.
- While comorbidities like anxiety or OCD are common in Tourette patients, *fluoxetine* would not directly address the **tics** themselves as a first-line agent.
*Alprazolam*
- *Alprazolam* is a **benzodiazepine** used for short-term relief of anxiety or panic disorders, working by enhancing *GABA*ergic activity.
- It does not effectively treat tics associated with Tourette syndrome and carries risks of **tolerance and dependence**.
*Chlorpromazine*
- *Chlorpromazine* is a **typical antipsychotic** that could reduce tics, but it has a higher risk of **extrapyramidal symptoms** and other side effects compared to atypical antipsychotics like *risperidone*.
- It is generally reserved for cases unresponsive to newer, better-tolerated agents.
*Buspirone*
- *Buspirone* is an **anxiolytic** that primarily affects serotonin receptors, used for generalized anxiety disorder.
- It does not have significant efficacy in treating the motor and vocal tics of **Tourette syndrome**.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 4: A 6-year-old boy presents to the pediatrician with his parents. He is fully vaccinated and met most developmental milestones. His fine motor milestones are delayed; at present, he cannot eat by himself and has difficulty in self-dressing. His intelligence quotient (IQ) is 65. He listens quietly while spoken to and engages in play with his classmates. He neither talks excessively nor remains mute, but engages in normal social conversation. There is no history of seizures and he is not on any long-term medical treatment. On his physical examination, his vital signs are stable. His height and weight are normal for his age and sex, but his occipitofrontal circumference is less than the 3rd percentile for his age and sex. His neurologic examination is also normal. Which of the following is the most likely diagnosis?
- A. Attention deficit hyperactivity disorder
- B. Autism
- C. Intellectual disability (Correct Answer)
- D. Obsessive-compulsive disorder
- E. Tic disorder
Motor disorders (tic disorders, stereotypic movement) Explanation: ***Intellectual disability***
- The boy's **IQ of 65** falls below the diagnostic threshold of 70 for intellectual disability, and he exhibits **adaptive deficits** in fine motor skills (difficulty eating and dressing) and **developmental delays**.
- His **microcephaly (occipitofrontal circumference less than 3rd percentile)** is also associated with certain forms of intellectual disability, further supporting this diagnosis.
*Attention deficit hyperactivity disorder*
- This condition is characterized by **inattention, hyperactivity, and impulsivity**, none of which are prominently described in the boy's presentation (he listens quietly and engages in normal conversation).
- While academic difficulties might occur, **significant adaptive and intellectual delays** as described are not typical primary features of ADHD.
*Autism*
- Autism spectrum disorder involves persistent deficits in **social communication and interaction** and **restricted, repetitive patterns of behavior, interests, or activities**.
- The boy's ability to engage in "normal social conversation" and play with classmates, along with an absence of repetitive behaviors or restricted interests, makes autism less likely.
*Obsessive-compulsive disorder*
- OCD is characterized by the presence of **obsessions (recurrent, persistent thoughts, urges, or images)** and/or **compulsions (repetitive behaviors or mental acts)**.
- The boy's symptoms do not include any mention of obsessions or compulsions.
*Tic disorder*
- Tic disorders involve **sudden, rapid, recurrent, nonrhythmic motor movements or vocalizations**.
- There is no mention of tics in the boy's presentation, making this diagnosis unlikely.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 5: A 44-year-old man presents to his primary care physician due to a tremor. His tremor has been progressively worsening over the course of several weeks and he feels embarrassed and anxious about going to social events. He says these movements are involuntary and denies having an urge to have these movements. Medical history is significant for depression which is being treated with escitalopram. His mother is currently alive and healthy but his father committed suicide and had a history of depression. Physical examination is remarkable for impaired saccade initiation and brief, abrupt, and non-stereotyped movements involved the right arm. He also has irregular finger tapping. Which of the following is the best treatment for this patient's symptoms?
- A. Cognitive behavioral therapy
- B. Switch to sertraline
- C. Valproic acid
- D. Deutetrabenazine (Correct Answer)
- E. Carbidopa-levodopa
Motor disorders (tic disorders, stereotypic movement) Explanation: ***Deutetrabenazine***
- This patient's symptoms of **abrupt, non-stereotyped movements**, **impaired saccade initiation**, irregular finger tapping, and a **family history of psychiatric illness** are highly suggestive of **Huntington's disease**. Deutetrabenazine is a **vesicular monoamine transporter 2 (VMAT2) inhibitor** approved for the treatment of **chorea** associated with Huntington's disease.
- VMAT2 inhibitors reduce the amount of dopamine released into the synapse, which helps alleviate the **hyperkinetic movements (chorea)** characteristic of Huntington's disease.
*Cognitive behavioral therapy*
- While **cognitive behavioral therapy (CBT)** can be beneficial for managing **anxiety** and **depression** often associated with chronic neurological conditions, it does not directly address the **neurological signs** and movement disorders themselves.
- CBT is a psychotherapy approach, not a pharmacological treatment for **chorea**.
*Switch to sertraline*
- Switching antidepressants from **escitalopram to sertraline** would primarily target the patient's **depressive symptoms**, but would not directly treat the **involuntary movements**.
- While some antidepressants can have mild effects on movement, they are not indicated as a primary treatment for **chorea** in Huntington's disease.
*Valproic acid*
- **Valproic acid** is an **anticonvulsant** and mood stabilizer primarily used for epilepsy, bipolar disorder, and migraine prevention.
- It does not have a primary role in the treatment of **chorea** associated with Huntington's disease.
*Carbidopa-levodopa*
- **Carbidopa-levodopa** is the cornerstone treatment for **Parkinson's disease**, aiming to increase dopamine levels in the brain to alleviate **bradykinesia** and rigidity.
- In Huntington's disease, the primary issue is **dopamine overactivity**, so increasing dopamine with carbidopa-levodopa would worsen, rather than improve, the **chorea**.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 6: A 4-year-old boy is brought to a pediatrician by his parents for a consultation after his teacher complained about his inability to focus or make friends at school. They mention that the boy does not interact well with others at home, school, or daycare. On physical examination, his vital signs are stable with normal weight, height, and head circumference for his age and sex. His general examination and neurologic examination are completely normal. A recent audiological evaluation shows normal hearing, and intellectual disability has been ruled out by a clinical psychologist. Which of the following investigations is indicated as part of his diagnostic evaluation at present?
- A. Magnetic resonance imaging (MRI) of brain
- B. Electroencephalography
- C. No further testing is needed
- D. Positron Emission Tomography (PET) scanning of head
- E. Autism spectrum disorder screening and developmental assessment (Correct Answer)
Motor disorders (tic disorders, stereotypic movement) Explanation: ***Autism spectrum disorder screening and developmental assessment***
- The clinical presentation (inability to focus, difficulty making friends, poor social interaction across multiple settings) is **highly suggestive of Autism Spectrum Disorder (ASD)**.
- After ruling out **hearing impairment and intellectual disability**, the next appropriate step is **formal ASD screening using validated tools** such as the **Modified Checklist for Autism in Toddlers (M-CHAT)**, **Autism Diagnostic Observation Schedule (ADOS)**, or **Autism Diagnostic Interview-Revised (ADI-R)**.
- According to **AAP guidelines**, when developmental concerns suggestive of ASD are identified, formal screening and comprehensive developmental assessment are **essential components of the diagnostic evaluation**.
- ASD diagnosis is primarily **clinical**, based on standardized screening tools and developmental assessments, not neuroimaging or electrophysiological studies.
*No further testing is needed*
- This is **incorrect** because the patient has not yet undergone **formal ASD-specific screening and developmental assessment**.
- While hearing and intellectual disability have been ruled out, **diagnostic confirmation of ASD** requires structured evaluation using validated assessment tools.
- Simply observing symptoms without formal screening is inadequate for establishing an ASD diagnosis.
*Magnetic resonance imaging (MRI) of brain*
- Brain MRI is **not routinely indicated** for ASD diagnosis as it typically shows **normal findings** in children with ASD.
- Neuroimaging is reserved for cases with **focal neurological signs, regression, or atypical features** suggesting structural abnormalities.
- This patient has a **normal neurological examination**, making MRI unnecessary.
*Electroencephalography*
- EEG is indicated only when there is suspicion of **seizure disorder** or other specific neurological conditions.
- The patient has a **normal neurological examination** with no seizure-like symptoms, making EEG unnecessary at this stage.
*Positron Emission Tomography (PET) scanning of head*
- PET scans are **not part of routine ASD diagnostic workup** and are typically used in research settings or for evaluating specific metabolic or neoplastic conditions.
- The **radiation exposure and invasiveness** make PET scanning inappropriate for initial diagnostic evaluation in a child with developmental concerns.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 7: A 25-year-old male medical student presents to student health with a chief complaint of picking at his skin. He states that at times he has urges to pick his skin that he struggles to suppress. Typically, he will participate in the act during finals or when he has "too many assignments to do." The patient states that he knows that his behavior is not helping his situation and is causing him harm; however, he has trouble stopping. He will often ruminate over all his responsibilities which make his symptoms even worse. The patient has a past medical history of surgical repair of his ACL two years ago. His current medications include melatonin. On physical exam you note a healthy young man with scars on his arms and face. His neurological exam is within normal limits. Which of the following is the best initial step in management?
- A. Fluoxetine (Correct Answer)
- B. Dialectical behavioral therapy
- C. Interpersonal psychotherapy
- D. Clomipramine
- E. Supportive psychotherapy
Motor disorders (tic disorders, stereotypic movement) Explanation: ***Fluoxetine***
- This patient's symptoms are consistent with **excoriation (skin-picking) disorder**, characterized by recurrent skin picking resulting in lesions and significant distress or impairment, often triggered by stress.
- **First-line treatment** is typically **cognitive-behavioral therapy (CBT)** with habit reversal training; however, among the options provided, **selective serotonin reuptake inhibitors (SSRIs)** like fluoxetine represent the most evidence-based pharmacological approach.
- **SSRIs** are considered when psychotherapy is unavailable or as adjunctive treatment for excoriation disorder and comorbid anxiety/OCD symptoms, though evidence is mixed.
- Fluoxetine is the best option listed for initial management in this clinical scenario.
*Dialectical behavioral therapy*
- **Dialectical behavioral therapy (DBT)** is primarily used for **borderline personality disorder** and chronic suicidality, focusing on emotion regulation and distress tolerance.
- While some of its techniques could be broadly helpful, it is not the primary or most effective treatment for excoriation disorder specifically.
- **CBT with habit reversal training** would be preferred over DBT for this condition.
*Interpersonal psychotherapy*
- **Interpersonal psychotherapy (IPT)** is an evidence-based treatment mainly for **depression** and some eating disorders, focusing on improving interpersonal relationships and social functioning.
- It does not directly target the compulsive behaviors or urge suppression central to excoriation disorder.
*Clomipramine*
- **Clomipramine**, a tricyclic antidepressant (TCA), is effective for **obsessive-compulsive disorder (OCD)**, but it has a less favorable side effect profile than SSRIs.
- Due to its side effects and lower tolerability, it is usually reserved for cases resistant to SSRIs, making it not the best initial pharmacologic step.
*Supportive psychotherapy*
- **Supportive psychotherapy** aims to alleviate symptoms, maintain self-esteem, and improve coping skills, offering a general supportive environment.
- While it can be helpful as an adjunct, it lacks the specific behavioral or pharmacological mechanisms needed for effective treatment of excoriation disorder.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 8: A 28-year-old medical student presents to the student health center with the complaint being unable to sleep. Although he is a very successful student, over the past few months he has become increasingly preoccupied with failing. The patient states that he wakes up 10-15 times per night to check his textbooks for factual recall. He has tried unsuccessfully to suppress these thoughts and actions, and he has become extremely anxious and sleep-deprived. He has no past medical history and family history is significant for a parent with Tourette's syndrome. He is started on cognitive behavioral therapy. He is also started on a first-line medication for his disorder, but after eight weeks of use, it is still ineffective. What drug, if added to his current regimen, may help improve his symptoms?
- A. Risperidone (Correct Answer)
- B. Sertraline
- C. Propranolol
- D. Methylphenidate
- E. Phenelzine
Motor disorders (tic disorders, stereotypic movement) Explanation: ***Risperidone***
- The patient presents with classic symptoms of **Obsessive-Compulsive Disorder (OCD)**, including intrusive thoughts (preoccupation with failing) and compulsive behaviors (checking textbooks). When a first-line SSRI is ineffective after an adequate trial (8-12 weeks), **augmentation with an atypical antipsychotic** is the evidence-based next step.
- **Risperidone** (along with aripiprazole) has the strongest evidence for augmenting SSRIs in treatment-resistant OCD. It helps reduce the severity of **obsessive thoughts** and **compulsive actions** by modulating dopamine and serotonin pathways.
- The family history of **Tourette's syndrome** further supports this choice, as both conditions share genetic links and respond to dopamine modulation.
*Sertraline*
- **Sertraline** is a **first-line selective serotonin reuptake inhibitor (SSRI)** for OCD. The patient in the vignette has already been on a first-line medication for eight weeks, implying an initial SSRI was ineffective.
- Adding another SSRI like sertraline when one has already failed is generally not the next step in managing refractory OCD; augmentation with a different class of medication (atypical antipsychotic) is the preferred strategy.
*Propranolol*
- **Propranolol** is a **beta-blocker** primarily used to manage symptoms of anxiety such as **tremors**, **palpitations**, and **social anxiety** by reducing peripheral adrenergic effects.
- It does not directly address the core obsessive thoughts or compulsive behaviors characteristic of OCD and is not considered a primary treatment or augmentation strategy for this disorder.
*Methylphenidate*
- **Methylphenidate** is a **stimulant** medication primarily used to treat **Attention-Deficit/Hyperactivity Disorder (ADHD)** and **narcolepsy**.
- It is not indicated for the treatment of OCD and could potentially exacerbate anxiety or sleep disturbances in this patient.
*Phenelzine*
- **Phenelzine** is a **monoamine oxidase inhibitor (MAOI)**, an older class of antidepressants. While MAOIs can be effective for some anxiety disorders, they are not first-line for OCD due to their significant side effect profile and dietary restrictions (**tyramine-free diet**).
- MAOIs are generally reserved for highly refractory cases of depression or anxiety and are not a standard augmentation strategy when an SSRI has failed for OCD, especially before trying atypical antipsychotics.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 9: A 33-year-old man presents to his physician with a 3-year history of gradually worsening tics and difficulty walking. He was last seen by the physician 5 years ago for anxiety, and he has been buying anti-anxiety medications from an internet website without a prescription as he cannot afford to pay for doctor’s visits. Now, the patient notes that his anxiety is somewhat controlled, but motor difficulties are making it difficult for him to work and socialize. Family history is unobtainable as his parents died in an accident when he was an infant. He grew up in foster care and was always a bright child. An MRI of the brain is ordered; it shows prominent atrophy of the caudate nucleus. Repeats of which of the following trinucleotides are most likely responsible for this patient’s disorder?
- A. CCG
- B. CTG
- C. CGG
- D. CAG (Correct Answer)
- E. GAA
Motor disorders (tic disorders, stereotypic movement) Explanation: ***CAG***
- The clinical presentation of **worsening tics**, **difficulty walking** (suggesting motor dysfunction), and the MRI finding of **caudate nucleus atrophy** are classic signs of **Huntington's disease**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder caused by an unstable expansion of **CAG trinucleotide repeats** within the *HTT* gene.
*CCG*
- Expansions of **CCG repeats** are associated with conditions like **fragile X-associated tremor/ataxia syndrome (FXTAS)**.
- While FXTAS involves neurological symptoms, the specific presentation of prominent tics and caudate atrophy points more strongly to Huntington's.
*CTG*
- **CTG trinucleotide repeat** expansions are characteristic of **myotonic dystrophy type 1 (DM1)**.
- Myotonic dystrophy primarily manifests with muscle weakness, myotonia, and cataracts, which are not the primary presenting symptoms here.
*CGG*
- Expansions of **CGG repeats** are the genetic basis of **Fragile X syndrome**, the most common inherited cause of intellectual disability.
- While Fragile X syndrome can have neurological features, it typically presents with developmental delay and distinctive physical features, rather than adult-onset tics and caudate atrophy.
*GAA*
- An expansion of **GAA trinucleotide repeats** is responsible for **Friedreich's ataxia**.
- Friedreich's ataxia is characterized by progressive ataxia, dysarthria, and loss of proprioception, which differ from the motor tics and specific caudate atrophy seen in this patient.
Motor disorders (tic disorders, stereotypic movement) US Medical PG Question 10: A 33-year-old man presents to a physician with a 3-year history of gradually worsening tics and difficulty walking. He was last seen by the physician 5 years ago for anxiety and has been purchasing anti-anxiety medications from an internet website without a prescription because he cannot afford to pay for the office visits. Now he says his anxiety is somewhat controlled, but the motor difficulties are making it difficult for him to work and socialize. His family history is unknown because his parents died in an automobile accident when he was an infant. He grew up in foster care and was always a bright child. An MRI of the brain is ordered, which shows prominent atrophy of the caudate nucleus. Repeats of which of the following trinucleotides are most likely responsible for this patient’s disorder?
- A. GAA
- B. CGG
- C. CTG
- D. CCG
- E. CAG (Correct Answer)
Motor disorders (tic disorders, stereotypic movement) Explanation: ***CAG***
- The constellation of **gradually worsening tics**, **difficulty walking** (motor difficulties), **anxiety**, and **caudate nucleus atrophy** on MRI is pathognomonic for **Huntington's disease (HD)**.
- Huntington's disease is caused by an expansion of **CAG trinucleotide repeats** in the *HTT* gene on chromosome 4, leading to production of mutant huntingtin protein with an abnormally long polyglutamine tract.
- CAG repeats >36 cause HD; normal alleles have <27 repeats.
*GAA*
- An abnormal expansion of **GAA repeats** in the *FXN* gene causes **Friedreich's ataxia**, which presents with progressive gait ataxia, dysarthria, loss of proprioception, and cardiomyopathy.
- Friedreich's ataxia primarily affects the **spinal cord dorsal columns**, **cerebellum**, and **peripheral nerves**, not the caudate nucleus.
- Onset is typically in childhood/adolescence, earlier than this case.
*CGG*
- An increased number of **CGG repeats** in the *FMR1* gene causes **Fragile X syndrome**, the most common inherited cause of intellectual disability.
- Fragile X presents with developmental delay, intellectual disability, autism spectrum features, and characteristic facial features (long face, large ears).
- It does not cause caudate atrophy, adult-onset motor tics, or progressive neurodegeneration.
*CTG*
- An expansion of **CTG repeats** in the *DMPK* gene causes **myotonic dystrophy type 1** (DM1).
- DM1 presents with **myotonia** (delayed muscle relaxation), progressive muscle weakness, cataracts, cardiac conduction defects, and frontal balding.
- It does not cause the prominent tics, chorea, or caudate atrophy characteristic of Huntington's disease.
*CCG*
- **CCG repeats** are not associated with a major trinucleotide repeat disorder that presents with the specific clinical features described.
- This option does not explain the caudate atrophy, progressive motor tics, and neurodegenerative course seen in this patient.
More Motor disorders (tic disorders, stereotypic movement) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.