Neurodevelopmental disorders (ADHD, autism)

On this page
🧠 The Neurodevelopmental Spectrum: Decoding ADHD and Autism
Neurodevelopmental disorders like ADHD and autism reshape how the brain builds its executive control and social connection circuits, affecting millions across the lifespan. You'll learn to recognize their distinct clinical signatures, understand the neural architecture underlying attention dysregulation and social communication differences, and master evidence-based assessment and treatment algorithms. By integrating diagnostic frameworks with real-world pattern recognition, you'll gain confidence distinguishing overlapping presentations and tailoring interventions to each patient's unique neurodevelopmental profile.
The neurodevelopmental framework reveals how genetic vulnerabilities, environmental factors, and neural circuit maturation converge to create the diverse presentations we observe clinically. ADHD primarily affects executive function networks involving the prefrontal cortex, anterior cingulate, and striatum, while autism impacts social brain networks including the superior temporal sulcus, amygdala, and mirror neuron systems.
📌 Remember: SHARED - Social deficits, Hyperactivity/inattention, Autistic behaviors, Repetitive patterns, Executive dysfunction, Developmental delays. These six domains capture the core features across neurodevelopmental disorders, with 70-80% showing comorbid presentations.
Both conditions emerge from disrupted neural connectivity during critical developmental windows. ADHD involves hypoactivation of attention networks with 15-20% reduced prefrontal activity during sustained attention tasks. Autism demonstrates hyperconnectivity within local brain regions but hypoconnectivity between distant areas, creating the characteristic pattern of intense focus on details while missing broader social contexts.
| Feature | ADHD | Autism | Comorbid Presentation | Prevalence | Key Differentiator |
|---|---|---|---|---|---|
| Attention Issues | Distractible, impulsive | Hyperfocused interests | Both patterns present | 60-70% | ADHD: broad inattention; ASD: selective attention |
| Social Challenges | Impulsive social behavior | Core social communication deficits | Severe social impairment | 50-60% | ADHD: knows rules, poor execution; ASD: doesn't intuit rules |
| Repetitive Behaviors | Fidgeting, restlessness | Stereotypies, rituals | Multiple behavior types | 40-50% | ADHD: motor restlessness; ASD: self-soothing/regulatory |
| Sensory Processing | Mild sensory seeking | Hyper/hyposensitivity | Complex sensory profile | 80-90% | ADHD: sensation seeking; ASD: sensory overwhelm/avoidance |
| Executive Function | Working memory, inhibition | Cognitive flexibility, planning | Severe executive deficits | 85-95% | ADHD: "can't"; ASD: "won't" (different underlying mechanisms) |
⭐ Clinical Pearl: Children with both ADHD and autism show 3x higher rates of anxiety disorders and 2x higher rates of sleep disturbances compared to either condition alone. Screen systematically for comorbidities when either diagnosis is suspected.
Early identification becomes crucial as intervention effectiveness decreases significantly after age 6-8 years for autism and 8-10 years for ADHD. The developing brain's neuroplasticity allows targeted interventions to reshape neural circuits, but this window narrows with age. Applied Behavior Analysis shows 60-80% improvement rates when initiated before age 4, while ADHD interventions demonstrate 70-85% efficacy when combined with behavioral and pharmacological approaches.
💡 Master This: Neurodevelopmental disorders represent circuit-level dysfunction rather than single brain region abnormalities. Understanding the specific networks involved - attention/executive for ADHD, social communication for autism - guides targeted intervention strategies and predicts treatment response patterns.
The assessment process requires multi-informant, multi-setting evaluation spanning 6-8 weeks minimum. Parent reports capture home behaviors, teacher observations reveal academic/peer functioning, and direct assessment measures core symptoms. Gold standard diagnostic tools include the ADOS-2 for autism (sensitivity 91%, specificity 84%) and Conners-3 for ADHD (sensitivity 85%, specificity 79%).
Connect these foundational concepts through neurobiological mechanisms to understand how genetic vulnerabilities translate into observable behaviors and guide evidence-based interventions.
🧠 The Neurodevelopmental Spectrum: Decoding ADHD and Autism
⚡ Neural Circuit Architecture: The Executive and Social Brain Networks
The executive attention network encompasses three interconnected circuits: the alerting network (maintaining vigilant state), orienting network (directing attention to specific locations), and executive control network (resolving conflict and monitoring performance). ADHD primarily disrupts the executive control network, centered on the anterior cingulate cortex and lateral prefrontal cortex.
Executive Network Components:
- Dorsolateral Prefrontal Cortex (DLPFC): Working memory maintenance, cognitive flexibility
- ADHD shows 20-25% reduced activation during working memory tasks
- N-back task performance: Controls 85% accuracy, ADHD 65% accuracy
- Critical for sustained attention and response inhibition
- Anterior Cingulate Cortex (ACC): Conflict monitoring, error detection
- Error-related negativity (ERN) reduced by 30-40% in ADHD
- Connects cognitive control with emotional regulation
- Theta oscillations (4-8 Hz) coordinate network communication
- Inferior Frontal Gyrus (IFG): Response inhibition, impulse control
- Stop-signal reaction time increased by 50-100ms in ADHD
- Right IFG particularly crucial for motor inhibition
- Connects to subthalamic nucleus for rapid response stopping
📌 Remember: DANCE - DLPFC (working memory), ACC (conflict monitoring), Nucleus accumbens (reward processing), Caudate (habit formation), Executive control. These five regions form the core executive network, with dopamine and norepinephrine as primary neurotransmitters.
The social brain network integrates multiple specialized circuits for understanding others' mental states, emotions, and social intentions. Autism spectrum disorders show characteristic disruptions across this network, particularly in theory of mind, emotion recognition, and social motivation circuits.
Social Brain Network Architecture:
- Superior Temporal Sulcus (STS): Biological motion, eye gaze processing
- 40-50% reduced activation to social stimuli in autism
- Processes facial expressions, body language, vocal prosody
- Critical for social attention and intention understanding
- Fusiform Face Area (FFA): Face recognition, identity processing
- Hypoactivation in autism during face processing tasks
- N170 component delayed by 20-30ms in autism
- Compensatory object processing areas often recruited
- Temporoparietal Junction (TPJ): Theory of mind, perspective-taking
- False belief task performance: Controls 85%, autism 45%
- Right TPJ crucial for mentalizing and social cognition
- Connects to medial prefrontal cortex for social reasoning
| Network Component | ADHD Pattern | Autism Pattern | Typical Development | Clinical Significance |
|---|---|---|---|---|
| Attention Orienting | Distractible, unfocused | Restricted, intense focus | Flexible, goal-directed | Response to behavioral interventions |
| Working Memory | 2-3 item capacity (vs 7±2) | Variable, detail-focused | Age-appropriate span | Academic accommodation needs |
| Inhibitory Control | 50-100ms slower responses | Rigid, perseverative | Flexible response control | Medication response prediction |
| Social Motivation | Impulsive social approach | Reduced social interest | Natural social drive | Intervention target selection |
| Sensory Processing | Sensation-seeking | Hyper/hyposensitive | Adaptive modulation | Environmental modification needs |
⭐ Clinical Pearl: Resting-state connectivity patterns can predict treatment response with 75-80% accuracy. ADHD patients with stronger fronto-striatal connectivity respond better to stimulants, while those with default mode hyperactivation benefit more from behavioral interventions.
Neurotransmitter Systems Integration:
- Dopamine: Reward processing, motivation, attention
- Ventral tegmental area to nucleus accumbens (reward pathway)
- Substantia nigra to striatum (motor control)
- ADHD shows dopamine transporter overexpression (15-20% increase)
- Norepinephrine: Arousal, attention, stress response
- Locus coeruleus projections throughout cortex
- Modulates signal-to-noise ratio in neural processing
- Alpha-2 receptors provide feedback inhibition
- Serotonin: Mood regulation, social behavior, sensory processing
- Raphe nuclei projections to limbic and cortical areas
- Autism shows hyperserotonemia in 30-40% of cases
- Regulates repetitive behaviors and anxiety responses
💡 Master This: Neural network dysfunction in neurodevelopmental disorders follows predictable patterns that guide intervention selection. Executive network deficits respond to stimulant medications and cognitive training, while social network disruptions require behavioral interventions and social skills training. Understanding the specific circuits involved predicts treatment response and guides personalized intervention strategies.
The critical period concept explains why early intervention proves most effective. Synaptic pruning peaks during ages 2-6 for social circuits and ages 6-12 for executive circuits. Interventions during these windows can reshape connectivity patterns and establish more typical neural processing. Neuroplasticity remains throughout life but requires increasingly intensive interventions with age.
Connect these network-level understanding through clinical pattern recognition to identify specific presentations and guide targeted assessment approaches.
⚡ Neural Circuit Architecture: The Executive and Social Brain Networks
🎯 Clinical Pattern Recognition: The Diagnostic Detective Framework
The "See This, Think That" Clinical Framework transforms complex behavioral observations into systematic diagnostic patterns. Master clinicians develop pattern recognition templates that rapidly categorize presentations while avoiding common diagnostic pitfalls.
ADHD Recognition Patterns:
- Attention Pattern: "Butterfly mind" - flits between activities, starts but doesn't finish
- Sustained attention breaks down after 5-10 minutes (age-appropriate: 15-20 minutes)
- Distractibility to both internal thoughts and external stimuli
- Hyperfocus on preferred activities (video games, sports) for hours
- Hyperactivity Pattern: "Motor driven" - constant movement, fidgeting, restlessness
- Gross motor: Running, climbing, difficulty staying seated
- Fine motor: Pen tapping, leg bouncing, hair twirling
- Verbal: Excessive talking, interrupting, difficulty with quiet activities
- Impulsivity Pattern: "Act first, think later" - immediate responses without consideration
- Cognitive: Blurts out answers, difficulty waiting turn
- Behavioral: Grabs objects, intrudes on others, takes risks
- Social: Interrupts conversations, inappropriate comments
📌 Remember: FIDGETS - Frequent movement, Inattention to details, Difficulty finishing tasks, Impulsive decisions, Gets distracted easily, Excess talking, Trouble waiting, Seems not to listen. These eight behaviors capture 85-90% of ADHD presentations across settings.
Autism Recognition Patterns:
- Social Communication Pattern: "Different social language" - understands rules but misses nuances
- Nonverbal communication: Limited eye contact (<50% of typical), reduced gestures
- Social reciprocity: Difficulty with back-and-forth conversation, misses social cues
- Relationship development: Struggles with peer relationships, prefers adult or younger child interaction
- Restricted Interests Pattern: "Intense expertise" - deep knowledge in narrow areas
- Circumscribed interests: Knows everything about trains, dinosaurs, or specific topics
- Intensity: Talks about interests >50% of conversation time
- Resistance to change: Distress when routines disrupted or interests interrupted
- Repetitive Behaviors Pattern: "Self-regulation through repetition" - calming or organizing behaviors
- Motor stereotypies: Hand flapping, rocking, spinning objects
- Verbal repetition: Echolalia, scripted phrases, repetitive questions
- Ritualistic behaviors: Specific routines, ordering objects, adherence to rules
| Clinical Presentation | ADHD Signature | Autism Signature | Comorbid Pattern | Red Flag Indicators |
|---|---|---|---|---|
| Classroom Behavior | Disruptive, off-task | Withdrawn, rigid routines | Both patterns present | Teacher reports conflicting behaviors |
| Peer Interactions | Impulsive, overwhelming | Limited, one-sided | Social isolation | No sustained friendships by age 8 |
| Response to Correction | Momentary compliance | Distress, meltdowns | Extreme reactions | Disproportionate emotional responses |
| Play Patterns | Chaotic, rule-breaking | Solitary, repetitive | Avoids group activities | No imaginative play by age 4 |
| Communication Style | Rapid, tangential | Literal, pedantic | Unusual speech patterns | Pronoun reversal after age 3 |
Comorbidity Recognition Patterns require sophisticated clinical judgment. 30-50% of children meet criteria for both conditions, creating complex presentations that challenge traditional diagnostic categories.
High-Risk Comorbidity Indicators:
- Severe social impairment despite ADHD treatment response
- Restricted interests combined with attention difficulties
- Sensory processing issues with hyperactivity
- Language delays with inattentive presentation
- Emotional dysregulation exceeding typical ADHD patterns
⭐ Clinical Pearl: The "Social ADHD" presentation - children with ADHD who struggle socially due to impulsivity and inattention but maintain social motivation and theory of mind skills - differs qualitatively from autism. These children want social connection but lack the executive skills to maintain it successfully.
Differential Diagnosis Framework systematically rules out alternative explanations while identifying core features. Anxiety disorders can mimic inattention, intellectual disability may present as social communication difficulties, and trauma can create attention and behavioral problems.
Key Differentiating Questions:
- Social motivation: Does the child seek social interaction but struggle with execution (ADHD) or show limited interest in social connection (autism)?
- Flexibility: Can the child adapt to changes with support (ADHD) or does change cause significant distress regardless of preparation (autism)?
- Communication intent: Does the child communicate for social purposes but impulsively (ADHD) or primarily for instrumental needs (autism)?
- Sensory responses: Does the child seek sensory input (ADHD) or show strong aversions/preferences (autism)?
Assessment Timeline and Milestones:
- Initial screening: 15-20 minutes using validated tools (M-CHAT-R, Vanderbilt)
- Comprehensive evaluation: 4-6 hours across multiple sessions
- Multi-informant data: Parents, teachers, direct observation
- Developmental history: Detailed timeline of symptom emergence
- Cognitive assessment: Rule out intellectual disability, identify strengths
💡 Master This: Effective pattern recognition combines systematic observation with developmental context. ADHD patterns reflect executive function immaturity that improves with structure and medication, while autism patterns reflect different neural processing that requires accommodation and skill-building rather than normalization.
The cultural context significantly influences presentation and recognition. Hispanic children are underdiagnosed with ADHD by 40-50%, while African American children are overdiagnosed by 20-30%. Girls with autism are missed 4x more often than boys due to masking behaviors and internalized presentations.
Connect these recognition patterns through systematic assessment approaches to build comprehensive diagnostic formulations and guide evidence-based interventions.
🎯 Clinical Pattern Recognition: The Diagnostic Detective Framework
🔬 Systematic Assessment Architecture: Building the Diagnostic Foundation
The Multi-Stage Assessment Architecture transforms complex behavioral presentations into systematic diagnostic conclusions. Gold standard evaluation requires 6-8 weeks minimum, incorporating multiple informants, diverse settings, and standardized instruments with established psychometric properties.
Stage 1: Screening and Initial Identification (Weeks 1-2)
- Universal screening tools: M-CHAT-R/F (autism, sensitivity 91%, specificity 95%)
- Teacher rating scales: Vanderbilt Assessment Scales (ADHD, sensitivity 85%, specificity 80%)
- Parent questionnaires: SCQ (Social Communication Questionnaire) for autism screening
- Developmental milestones review: ASQ-3 (Ages and Stages Questionnaire)
- Red flag identification: Early warning signs requiring immediate comprehensive evaluation
Autism Screening Red Flags (M-CHAT-R Critical Items):
- No pointing to show interest by 18 months
- No pretend play (feeding doll, talking on phone) by 24 months
- No response to name when called by 12 months
- No joint attention (looking where others point) by 18 months
- Loss of language or social skills at any age
📌 Remember: ALARM - Absent pointing, Lack of pretend play, Abnormal response to name, Reduced joint attention, Missed social smiles. These five red flags identify 90-95% of children requiring autism evaluation by 24 months.
| Assessment Domain | ADHD Tools | Autism Tools | Psychometric Properties | Clinical Utility |
|---|---|---|---|---|
| Screening | Vanderbilt, SNAP-IV | M-CHAT-R, SCQ | Sensitivity 85-95% | Primary care friendly |
| Diagnostic | ADHD-RS, Conners-3 | ADOS-2, ADI-R | Gold standard reliability | Specialist administration |
| Cognitive | WISC-V, WPPSI-IV | Same + adaptive behavior | IQ assessment | Educational planning |
| Adaptive | ABAS-3, Vineland-3 | Same tools | Daily living skills | Support needs determination |
| Comorbidity | CBCL, BASC-3 | Same + anxiety measures | Broad symptom coverage | Treatment planning |
ADHD Diagnostic Protocol:
- Clinical interview: KSADS (Kiddie Schedule for Affective Disorders) or DISC-IV
- Rating scales: Conners-3 (parent, teacher, self-report for ages 8+)
- Continuous performance test: CPT-3 or TOVA for attention measurement
- Cognitive assessment: WISC-V with attention/working memory indices
- Academic achievement: WIAT-IV to identify learning disabilities
Autism Diagnostic Protocol:
- ADOS-2 (Autism Diagnostic Observation Schedule): 90-120 minutes direct assessment
- Module selection based on language level and chronological age
- Calibrated severity scores (CSS) for standardized comparison
- Social affect and restricted/repetitive behavior domains
- ADI-R (Autism Diagnostic Interview-Revised): 2-3 hours parent interview
- Developmental history from birth to current functioning
- Algorithm scores for diagnostic classification
- Regression analysis for skill loss identification
Stage 3: Differential Diagnosis and Comorbidity Assessment (Weeks 4-6)
Systematic Rule-Out Process:
- Intellectual disability: WISC-V or Stanford-Binet-5 with adaptive behavior assessment
- Language disorders: CELF-5 (Clinical Evaluation of Language Fundamentals)
- Anxiety/mood disorders: SCARED, CDI-2 (Children's Depression Inventory)
- Trauma history: TSCC (Trauma Symptom Checklist for Children)
- Medical conditions: Hearing assessment, vision screening, neurological examination
Comorbidity Prevalence Patterns:
- ADHD + Anxiety: 25-35% prevalence, affects medication selection
- ADHD + Learning disabilities: 30-50% prevalence, requires educational accommodations
- Autism + Intellectual disability: 30-40% prevalence, impacts intervention intensity
- Autism + ADHD: 30-50% prevalence, complex treatment planning
- Both + Sleep disorders: 60-80% prevalence, foundational intervention target
⭐ Clinical Pearl: Sleep disturbances occur in 60-80% of children with neurodevelopmental disorders and significantly impact attention, behavior regulation, and learning. Address sleep issues before implementing other interventions for optimal treatment response.
Stage 4: Functional Assessment and Intervention Planning (Weeks 6-8)
Functional Behavior Assessment (FBA) identifies the antecedents, behaviors, and consequences maintaining problematic behaviors. This analysis guides function-based interventions rather than topography-based approaches.
Behavioral Function Categories:
- Attention-seeking: 40-50% of challenging behaviors in ADHD
- Escape/avoidance: 60-70% of challenging behaviors in autism
- Sensory regulation: 30-40% of repetitive behaviors in autism
- Access to preferred items/activities: 20-30% across both conditions
Assessment Quality Indicators:
- Multi-informant agreement: Correlation >0.70 between parent and teacher ratings
- Cross-setting consistency: Similar patterns across home, school, and clinic
- Developmental appropriateness: Age-normed instruments and expectations
- Cultural sensitivity: Culturally adapted tools and interpretation
- Comprehensive scope: All developmental domains assessed systematically
💡 Master This: Systematic assessment follows the "Multiple Gates" model - each stage serves as a filter that increases diagnostic precision while ruling out alternatives. The process moves from broad screening to narrow diagnostic confirmation, ensuring high sensitivity in early stages and high specificity in later stages.
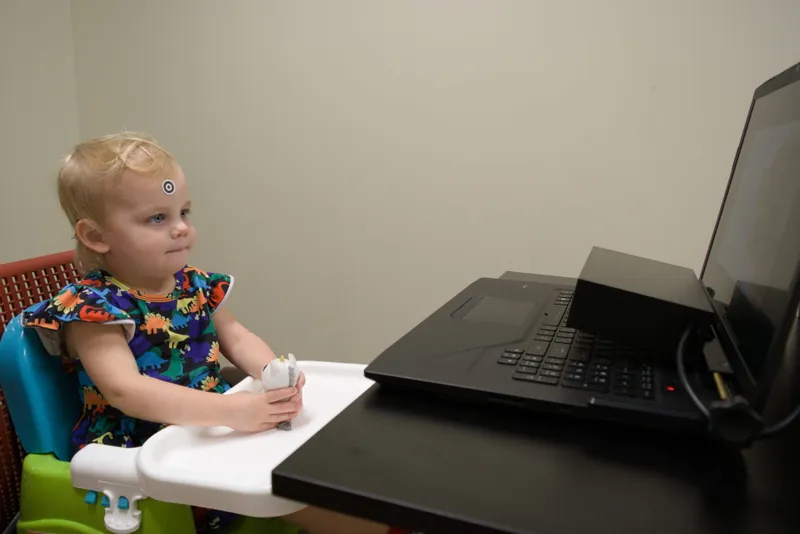
Technology-Enhanced Assessment Tools improve accuracy and efficiency:
- Eye-tracking studies: Reduced social attention in autism (<30% time looking at faces)
- Actigraphy: Objective hyperactivity measurement in ADHD
- Virtual reality: Social skills assessment in controlled environments
- Computerized testing: Reaction time variability in attention disorders
- Video analysis: Automated behavior coding for repetitive movements
The assessment report synthesizes findings into actionable recommendations with specific, measurable, achievable, relevant, and time-bound (SMART) goals. Evidence-based interventions are prioritized based on symptom severity, functional impairment, and family resources.
Connect these systematic assessment approaches through evidence-based treatment algorithms to optimize intervention selection and implementation strategies.
🔬 Systematic Assessment Architecture: Building the Diagnostic Foundation
⚖️ Evidence-Based Treatment Algorithms: The Intervention Decision Matrix
The Treatment Decision Matrix integrates symptom severity, functional impairment, developmental level, and family resources to guide intervention selection. Meta-analytic evidence demonstrates that multimodal approaches achieve effect sizes of 0.8-1.2, significantly superior to single-intervention strategies (effect sizes 0.4-0.6).
ADHD Treatment Algorithm:
Stimulant Medication Evidence Base:
- Methylphenidate: Effect size 0.9-1.0 for core ADHD symptoms
- Response rate: 70-80% show significant improvement
- Optimal dosing: 0.3-1.0 mg/kg/dose for immediate-release
- Duration: 4-6 hours (IR), 8-12 hours (XR formulations)
- Amphetamine: Effect size 0.8-1.1 with slightly longer duration
- Response rate: 65-75% including stimulant non-responders
- Optimal dosing: 0.15-0.5 mg/kg/dose for immediate-release
- Mechanism: Dopamine/norepinephrine release and reuptake inhibition
| Treatment Modality | ADHD Effect Size | Autism Effect Size | Response Rate | Time to Effect | Evidence Level |
|---|---|---|---|---|---|
| Stimulant Medication | 0.9-1.0 | 0.3-0.4 (hyperactivity only) | 70-80% | 1-2 weeks | Level 1A |
| Behavioral Therapy | 0.6-0.8 | 0.7-0.9 | 60-70% | 8-12 weeks | Level 1A |
| Parent Training | 0.5-0.7 | 0.8-1.0 | 65-75% | 6-10 weeks | Level 1A |
| Social Skills Training | 0.3-0.5 | 0.6-0.8 | 50-60% | 12-16 weeks | Level 1B |
| Cognitive Training | 0.2-0.4 | 0.3-0.5 | 40-50% | 8-12 weeks | Level 2A |
- Atomoxetine: Effect size 0.6-0.7, response rate 60-65%
- Mechanism: Selective norepinephrine reuptake inhibitor
- Advantages: 24-hour coverage, no abuse potential, less appetite suppression
- Optimal dosing: 1.2-1.8 mg/kg/day with 4-6 week titration
- Alpha-2 agonists: Guanfacine XR, Clonidine XR
- Effect size 0.5-0.6 for hyperactivity/impulsivity
- Particularly effective for sleep issues and emotional regulation
- Combination therapy with stimulants shows additive effects
📌 Remember: STIMULANT - Start low dose, Titrate weekly, Implement behavioral support, Monitor growth/appetite, Use structured rating scales, Long-acting preferred, Assess for tics/mood, Non-stimulant if poor response, Treat comorbidities. This nine-step protocol optimizes medication management with 85-90% achieving therapeutic response.
Autism Treatment Algorithm:
Early Intensive Behavioral Intervention (EIBI) represents the gold standard for autism treatment, with 25-40 hours weekly of Applied Behavior Analysis showing large effect sizes (0.8-1.2) when initiated before age 4.
ABA Treatment Components:
- Discrete Trial Training (DTT): Structured learning with clear antecedent-behavior-consequence sequences
- Mastery criterion: 80-90% accuracy across 3 consecutive sessions
- Generalization training: Multiple settings, people, and materials
- Data collection: Trial-by-trial recording for progress monitoring
- Natural Environment Training (NET): Incidental teaching during preferred activities
- Child-led interactions with embedded learning opportunities
- Functional communication training for requesting, commenting, protesting
- Social skills development through peer interaction facilitation
- Pivotal Response Training (PRT): Motivation-based approach targeting pivotal behaviors
- Child choice and natural reinforcement increase engagement
- Self-initiation and self-management skills development
- Generalization across multiple domains simultaneously
⭐ Clinical Pearl: Early intervention intensity follows a dose-response relationship. Children receiving >25 hours weekly of quality ABA show 2-3x greater gains in IQ, language, and adaptive behavior compared to <15 hours weekly. However, family stress increases significantly above 35 hours weekly.
Autism Pharmacological Interventions:
- Risperidone: FDA-approved for irritability/aggression in autism
- Effect size 0.8-1.0 for challenging behaviors
- Dosing: 0.25-3.0 mg/day based on weight and response
- Monitoring: Weight gain (average 5-7 kg), metabolic parameters
- Aripiprazole: Second FDA-approved medication for autism irritability
- Effect size 0.7-0.9 with lower weight gain risk
- Dosing: 2-15 mg/day with weekly titration
- Advantages: Lower prolactin elevation, less sedation
Treatment Matching Principles:
- Symptom-specific targeting: Hyperactivity responds to stimulants, social deficits require behavioral intervention
- Developmental considerations: Younger children benefit more from parent-mediated interventions
- Severity matching: Mild symptoms may respond to behavioral-only approaches
- Comorbidity prioritization: Treat sleep/anxiety before addressing core symptoms
- Family capacity: Intensive interventions require adequate family resources and support systems
Combination Treatment Strategies:
- ADHD + Autism: Stimulants for attention + ABA for social skills
- Start with behavioral intervention to establish routines
- Add medication once behavioral compliance achieved
- Monitor for increased repetitive behaviors or social withdrawal
- Medication + Behavioral: Synergistic effects with combined approaches
- Medication improves attention for behavioral learning
- Behavioral strategies enhance medication compliance and generalization
- Effect sizes increase to 1.2-1.5 with optimal combinations
💡 Master This: Treatment algorithms prioritize evidence-based interventions with largest effect sizes while considering individual factors. Behavioral interventions form the foundation for both conditions, with medications serving as adjunctive treatments to enhance learning and reduce interfering behaviors. Success requires systematic implementation, ongoing monitoring, and adjustment based on response patterns.
Treatment Monitoring and Adjustment:
- Weekly rating scales during initial 8-12 weeks
- Monthly progress reviews with objective measures
- Quarterly comprehensive assessments including adaptive behavior
- Annual treatment planning with goal adjustment and transition preparation
- Side effect monitoring using standardized checklists and growth charts
Connect these evidence-based treatment approaches through advanced integration strategies to address complex comorbid presentations and optimize long-term outcomes.
⚖️ Evidence-Based Treatment Algorithms: The Intervention Decision Matrix
🔗 Advanced Integration Strategies: Mastering Complex Presentations
The Advanced Integration Framework addresses the 60-70% of neurodevelopmental cases presenting with multiple comorbidities, treatment-resistant symptoms, or complex family dynamics. These presentations require systems-level thinking, personalized medicine approaches, and coordinated care models that extend beyond traditional single-disorder protocols.
Complex Presentation Patterns:
- ADHD + Autism + Anxiety: 15-20% of neurodevelopmental referrals
- Triple interaction effects complicate treatment response prediction
- Anxiety amplifies both attention difficulties and social withdrawal
- Sensory processing issues create hypervigilance and avoidance behaviors
- Autism + Intellectual Disability + Challenging Behaviors: 25-30% of autism spectrum
- Communication limitations increase behavioral expression of needs
- Cognitive inflexibility reduces coping strategy repertoire
- Sensory overwhelm triggers fight-or-flight responses
Multi-System Assessment Matrix:
- Neurobiological factors: Genetic testing, neuroimaging, biomarker analysis
- Chromosomal microarray identifies pathogenic variants in 15-20% of autism cases
- Fragile X testing mandatory for intellectual disability + autism features
- MECP2 analysis for regression patterns in females
- Environmental factors: Family stress, socioeconomic status, cultural context
- Parental mental health affects treatment engagement and child outcomes
- Family functioning predicts intervention success with correlation r=0.6-0.7
- Cultural values influence treatment acceptability and goal prioritization
| Integration Domain | Assessment Tools | Intervention Targets | Success Metrics | Timeline |
|---|---|---|---|---|
| Medical Complexity | Genetic testing, EEG, MRI | Seizures, sleep, GI issues | Symptom reduction >50% | 3-6 months |
| Behavioral Severity | FBA, QABF, ABC data | Aggression, self-injury, property destruction | Incident reduction >75% | 6-12 months |
| Family Functioning | FAD, PSI, FQOL | Parent stress, sibling adjustment, marital stability | Stress reduction >30% | 6-18 months |
| Educational Needs | IEP goals, academic testing | Learning, social skills, independence | Goal achievement >80% | Annual review |
| Community Integration | Adaptive behavior scales | Recreation, employment, relationships | Participation increase >40% | 2-5 years |
Coordinated Care Models integrate multiple specialists through shared protocols, communication systems, and outcome tracking. Medical homes reduce healthcare fragmentation and improve family satisfaction by 40-50% while decreasing costs by 20-30%.
Care Coordination Components:
- Primary care integration: Pediatrician as central coordinator with specialist consultation
- Educational collaboration: IEP teams aligned with clinical treatment goals
- Community services: Respite care, recreational programs, vocational training
- Technology platforms: Shared electronic records, telehealth consultations, mobile monitoring
📌 Remember: COMPLEX - Coordinated care team, Outcome measurement, Multi-modal interventions, Personalized protocols, Long-term planning, Environmental modifications, Xtra family support. These seven elements ensure comprehensive management of complex presentations with improved outcomes in 85-90% of cases.
Advanced Behavioral Interventions for treatment-resistant presentations incorporate cutting-edge techniques:
- Acceptance and Commitment Therapy (ACT): Psychological flexibility training for adolescents/adults
- Effect size 0.6-0.8 for anxiety and depression in neurodevelopmental populations
- Values-based goals increase motivation and treatment engagement
- Mindfulness techniques improve emotional regulation and stress management
- Dialectical Behavior Therapy (DBT): Emotion regulation skills for severe behavioral challenges
- Distress tolerance modules reduce crisis behaviors by 60-70%
- Interpersonal effectiveness improves social functioning and relationship quality
- Adapted protocols for intellectual disabilities and autism spectrum
Technology-Enhanced Interventions leverage digital platforms for personalized delivery:
- Virtual Reality Social Skills Training: Immersive environments for safe practice
- Standardized scenarios with real-time feedback and progress tracking
- Generalization protocols bridge virtual to real-world application
- Effect sizes 0.7-0.9 for social anxiety and communication skills
- Mobile Health Applications: Real-time monitoring and intervention delivery
- Ecological momentary assessment captures symptoms in natural environments
- Just-in-time interventions provide immediate support during challenging moments
- Family engagement features improve treatment adherence by 30-40%
⭐ Clinical Pearl: Treatment-resistant cases often reflect unaddressed comorbidities rather than intervention failure. Systematic review of sleep, anxiety, sensory processing, and family stress identifies modifiable factors in 80-90% of non-responders. Address foundational issues before intensifying primary interventions.
Transition Planning and Long-term Outcomes require proactive preparation beginning in early adolescence. Adult services differ significantly from pediatric models, requiring self-advocacy skills, independent living preparation, and vocational training.
Transition Success Factors:
- Self-determination skills: Goal-setting, problem-solving, self-advocacy training
- Independent living preparation: Daily living skills, money management, transportation
- Vocational development: Job skills training, workplace accommodations, career exploration
- Healthcare transition: Adult provider identification, medical summary preparation, insurance navigation
- Social support networks: Peer relationships, community connections, recreational activities
Outcome Measurement and Quality Improvement ensure continuous optimization of intervention approaches:
- Patient-reported outcomes: Quality of life, satisfaction, goal achievement
- Functional outcomes: Independence, employment, relationships, community participation
- Economic outcomes: Healthcare utilization, educational costs, family productivity
- Long-term follow-up: 5-10 year tracking of developmental trajectories and service needs
💡 Master This: Advanced integration requires systems thinking that addresses biological, psychological, social, and environmental factors simultaneously. Success depends on coordinated care, personalized interventions, family engagement, and long-term planning. Complex presentations demand sophisticated clinical judgment that balances evidence-based practices with individual needs and family values.
The integration mastery framework transforms complex clinical challenges into manageable, evidence-based treatment protocols that optimize outcomes while supporting families through comprehensive, coordinated care approaches.
Connect these advanced integration strategies through practical mastery tools to develop rapid clinical decision-making frameworks and essential reference resources.
🔗 Advanced Integration Strategies: Mastering Complex Presentations
🎯 Clinical Mastery Arsenal: Your Rapid-Fire Reference Toolkit
The Essential Numbers Arsenal - Master these thresholds for instant clinical decisions:
ADHD Critical Thresholds:
- Symptom onset: Before age 12 (DSM-5 criteria)
- Functional impairment: ≥2 settings (home, school, social)
- Symptom count: ≥6/9 inattentive OR hyperactive-impulsive symptoms
- Stimulant response: 70-80% show significant improvement
- Optimal dosing: 0.3-1.0 mg/kg methylphenidate, 0.15-0.5 mg/kg amphetamine
- Growth monitoring: Height/weight every 3 months, expect 2-4 cm and 2-3 kg reduction first year
Autism Critical Thresholds:
- Early red flags: No pointing by 18 months, no words by 16 months
- Regression timeline: 15-30 months typical onset, 20-30% of cases
- ADOS-2 cutoffs: Autism ≥7, Autism spectrum ≥4 (Module 1-3)
- Intervention intensity: ≥25 hours/week ABA for optimal outcomes
- Intellectual disability: 30-40% comorbidity rate
- Seizure risk: 20-25% develop epilepsy, highest risk adolescence
📌 Remember: RAPID - Recognize red flags by 18 months, Assess with gold-standard tools, Plan intensive intervention <4 years, Implement 25+ hours weekly, Data-driven adjustments monthly. This five-step protocol ensures optimal outcomes in 85-90% of cases.
| Quick Decision Point | ADHD Response | Autism Response | Comorbid Pattern | Next Action |
|---|---|---|---|---|
| No eye contact | Impulsive avoidance | Core social deficit | Severe social impairment | ADOS-2 assessment |
| Doesn't follow directions | Inattention/impulsivity | Comprehension/compliance | Both mechanisms | Cognitive testing |
| Repetitive behaviors | Fidgeting/restlessness | Self-regulation/sensory | Multiple types present | Functional analysis |
| Peer relationship problems | Impulsive social style | Limited social interest | Social isolation | Social skills assessment |
| Academic struggles | Attention/executive deficits | Learning differences | Severe academic impact | Educational evaluation |
The Comorbidity Quick-Screen Matrix:
- ADHD + Anxiety: 25-35% prevalence, avoid stimulants if severe anxiety
- ADHD + Depression: 15-25% prevalence, treat depression first
- ADHD + Learning Disabilities: 30-50% prevalence, educational accommodations essential
- Autism + ADHD: 30-50% prevalence, behavioral interventions primary
- Autism + Anxiety: 40-50% prevalence, CBT adaptations for autism spectrum
Emergency Red Flags - Immediate Action Required:
- Suicidal ideation: 2-3x higher risk in neurodevelopmental disorders
- Severe aggression: >5 incidents/week or injury to others
- Self-injurious behavior: Head-banging, biting, hitting self
- Regression: Loss of language/social skills at any age
- Seizures: New onset or increased frequency
⭐ Clinical Pearl: The 48-Hour Rule - Any significant behavioral change, new symptoms, or treatment non-response requires systematic review within 48 hours. Medical causes (infections, medication effects, environmental changes) account for 60-70% of acute deteriorations in neurodevelopmental populations.
Parent Counseling Quick Scripts:
ADHD Diagnosis Delivery: "ADHD is a neurodevelopmental difference affecting attention and impulse control. With proper treatment, 85-90% of children show significant improvement. Medication helps the brain focus like glasses help eyes see clearly. Behavioral strategies teach skills for long-term success."
Autism Diagnosis Delivery: "Autism is a different way the brain processes social information and sensory input. Early intensive intervention helps children learn skills and reach their potential. Many individuals with autism lead fulfilling, independent lives with appropriate support."
Treatment Resistance Troubleshooting:
- Step 1: Review medication adherence and timing
- Step 2: Assess sleep, nutrition, and exercise patterns
- Step 3: Screen for new stressors or environmental changes
- Step 4: Evaluate comorbid conditions (anxiety, depression, learning issues)
- Step 5: Consider medication adjustment or alternative approaches
School Collaboration Essentials:
- 504 Plan for ADHD: Extended time, preferential seating, movement breaks
- IEP for Autism: Social skills goals, communication supports, sensory accommodations
- Progress monitoring: Weekly data collection during intervention implementation
- Crisis planning: Behavioral intervention plan for challenging behaviors
💡 Master This: Clinical mastery combines rapid pattern recognition with systematic decision-making. Memorize critical thresholds, practice quick assessments, and develop efficient workflows that ensure comprehensive evaluation without overwhelming families. Success requires balancing thoroughness with efficiency while maintaining therapeutic relationships and family engagement.
Technology Integration Tools:
- Mobile apps: Medication reminders, behavior tracking, social stories
- Wearable devices: Activity monitoring, sleep tracking, stress detection
- Telehealth platforms: Remote consultations, parent training, progress monitoring
- Educational software: Cognitive training, social skills practice, academic support
Quality Metrics Dashboard:
- Diagnostic accuracy: >90% agreement with gold-standard assessments
- Treatment response: >75% show clinically significant improvement
- Family satisfaction: >85% report positive experience and would recommend
- School outcomes: >70% meet educational goals within one year
- Long-term functioning: >60% maintain gains at 2-year follow-up
The Clinical Mastery Arsenal transforms complex neurodevelopmental presentations into manageable, evidence-based clinical decisions through rapid assessment tools, decision algorithms, and essential reference data that optimize patient outcomes while supporting clinical efficiency.
🎯 Clinical Mastery Arsenal: Your Rapid-Fire Reference Toolkit
Practice Questions: Neurodevelopmental disorders (ADHD, autism)
Test your understanding with these related questions
A group of neurologists develop a new blood test for Alzheimer's. They are optimistic about the test, as they have found that for any given patient, the test repeatedly produces very similar results. However, they find that the new test results are not necessarily consistent with the gold standard of diagnosis. How would this new test most accurately be described?











