Premenstrual dysphoric disorder US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Premenstrual dysphoric disorder. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Premenstrual dysphoric disorder US Medical PG Question 1: A previously healthy 13-year-old girl is brought to the physician by her mother because of a change in behavior. The mother reports that over the past 6 months, her daughter has had frequent mood swings. Sometimes, she is irritable for several days and loses her temper easily. In between these episodes, she behaves “normal,” spends time with her friends, and participates in gymnastics training twice a week. The mother has also noticed that her daughter needs more time than usual to get ready for school. Sometimes, she puts on excessive make-up. One month ago, her teacher had informed the parents that their daughter had skipped school and was seen at the local mall with one of her classmates instead. The patient reports that she often feels tired, especially when she has to wake up early for school. On the weekends, she sleeps until 1 pm. Menses have occurred at 15- to 45-day intervals since menarche at the age of 12 years; they are not associated with abdominal discomfort or functional impairment. Physical examination shows no abnormalities. Which of the following is the most likely explanation for the patient's behavior?
- A. Major depressive disorder
- B. Premenstrual syndrome
- C. Borderline personality disorder
- D. Normal behavior (Correct Answer)
- E. Bipolar disorder
Premenstrual dysphoric disorder Explanation: ***Normal behavior***
* The patient's behavior, including **mood swings**, irritability, increased sleep, and occasional boundary-testing (skipping school), is consistent with typical **adolescent development** and the challenges of this developmental stage.
* The absence of significant functional impairment, her continued engagement in activities like gymnastics, and the intermittent nature of the symptoms suggest that her behavior falls within the **normal range of adolescent growth and exploration**.
*Major depressive disorder*
* **Major depressive disorder** would typically involve more persistent and pervasive symptoms of **depressed mood** or **anhedonia** (loss of interest or pleasure) for at least two weeks, along with other symptoms like significant weight changes, insomnia/hypersomnia, psychomotor agitation/retardation, fatigue, feelings of worthlessness/guilt, difficulty concentrating, or recurrent thoughts of death.
* While she experiences tiredness and increased sleep, her ability to engage in gymnastics and spend time with friends, along with periods of "normal" behavior, does not align with the diagnostic criteria for **major depressive disorder**, which implies more constant functional impairment.
*Premenstrual syndrome*
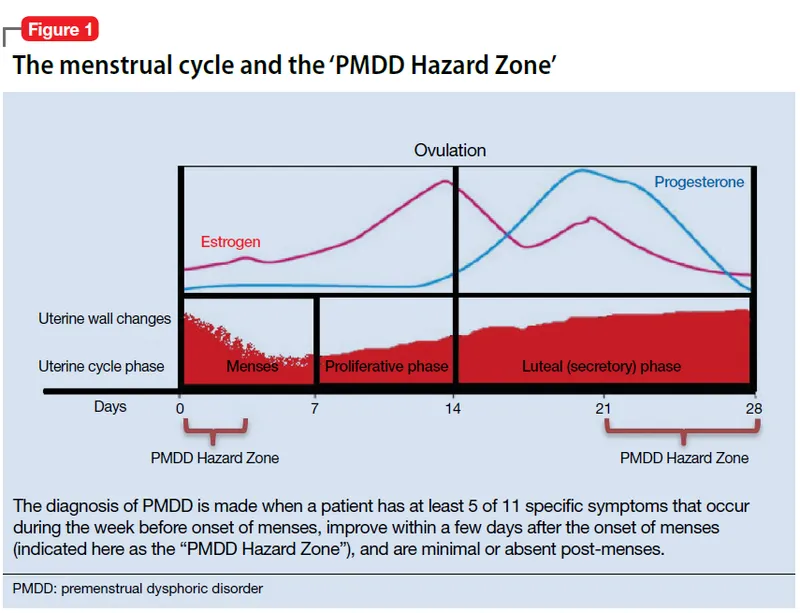
* **Premenstrual syndrome (PMS)** symptoms are directly linked to the **luteal phase** of the menstrual cycle, consistently resolving with menstruation or shortly thereafter.
* The patient's mood swings and other behavioral changes are reported over a 6-month period and are not explicitly tied to her 15- to 45-day menstrual cycle, making **PMS** less likely.
*Borderline personality disorder*
* **Borderline personality disorder** is characterized by a pervasive pattern of **instability of interpersonal relationships**, self-image, affects, and marked impulsivity, often including features like frantic efforts to avoid abandonment, unstable self-image or sense of self, impulsivity in at least two areas that are potentially self-damaging, recurrent suicidal behavior or self-mutilation, affective instability, chronic feelings of emptiness, intense anger, and transient stress-related paranoid ideation or severe dissociative symptoms.
* While mood swings are present, the overall clinical picture does not align with the severe and persistent functional impairment and specific diagnostic criteria for **borderline personality disorder**, especially in adolescence where such a diagnosis is made with caution.
*Bipolar disorder*
* **Bipolar disorder** involves distinct periods of elevated, expansive, or irritable mood (manic or hypomanic episodes) alternating with depressive episodes.
* While the patient experiences mood swings and irritability, the description lacks the sustained and severe euphoric, expansive, or irritable mood, increased energy/activity, decreased need for sleep (rather than increased), and other classic symptoms (e.g., grandiosity, flight of ideas, risky behaviors) that define a **manic** or **hypomanic episode**, making **bipolar disorder** an unlikely diagnosis.
Premenstrual dysphoric disorder US Medical PG Question 2: A 26-year-old woman thinks poorly of herself and is extremely sensitive to criticism. She is socially inhibited and has never had a romantic relationship, although she desires one. Which of the following is the most likely diagnosis?
- A. Schizoid personality disorder
- B. Paranoid personality disorder
- C. Depression
- D. Dysthymia
- E. Avoidant personality disorder (Correct Answer)
Premenstrual dysphoric disorder Explanation: ***Avoidant personality disorder***
- Characterized by **social inhibition**, feelings of **inadequacy**, and **hypersensitivity to negative evaluation**, leading to avoidance of social interactions despite a desire for connection.
- The patient's self-perception, sensitivity to criticism, and absence of romantic relationships are classic signs.
*Schizoid personality disorder*
- Individuals with schizoid personality disorder exhibit a pervasive pattern of **detachment from social relationships** and a restricted range of emotional expression.
- Unlike avoidant personality disorder, they typically **do not desire social connection** and are indifferent to criticism or praise.
*Paranoid personality disorder*
- Marked by pervasive **distrust and suspiciousness of others**, interpreting their motives as malevolent.
- This patient's symptoms are more focused on self-perception and social anxiety rather than paranoid ideation.
*Depression*
- Depression involves a sustained period of **low mood**, loss of interest or pleasure, and other vegetative symptoms, which are not explicitly described as the primary, long-standing issue here.
- While feelings of worthlessness can occur in depression, the chronic, pervasive social inhibition and desire for relationships point away from a primary depressive episode as the sole diagnosis.
*Dysthymia*
- Dysthymia, or persistent depressive disorder, is characterized by a chronically depressed mood for at least two years, but it usually includes more pervasive depressive symptoms like low energy and anhedonia.
- While it can involve poor self-esteem, it doesn't fully explain the specific pattern of social avoidance and hypersensitivity to criticism, especially the patient's desire for social connection, which is often dampened in dysthymia.
Premenstrual dysphoric disorder US Medical PG Question 3: A 24-year-old male comes into the psychiatric clinic complaining of consistent sadness. He endorses feelings of worthlessness, anxiety, and anhedonia for the past couple months but denies feeling suicidal. He further denies any past episodes of feeling overly energetic with racing thoughts. Confident of the diagnosis, you recommend frequent talk therapy along with a long-term prescription of a known first-line medication for this disorder. What is the drug and what are some of the most frequently encountered side effects?
- A. Selective serotonin reuptake inhibitor; hypomania, suicidal thoughts
- B. Tricyclic antidepressants; hypomania, suicidal thoughts
- C. Selective serotonin reuptake inhibitor; anorgasmia, insomnia (Correct Answer)
- D. Monoamine oxidase inhibitors; Orthostatic hypotension, weight gain
- E. Tricyclic antidepressants; Orthostatic hypotension, anticholinergic effects
Premenstrual dysphoric disorder Explanation: ***Selective serotonin reuptake inhibitor; anorgasmia, insomnia***
- The patient presents with classic symptoms of **major depressive disorder**, including persistent sadness, worthlessness, anxiety, and anhedonia, without any history of manic or hypomanic episodes. **SSRIs** are considered first-line pharmacotherapy for this condition.
- Common side effects of SSRIs include **sexual dysfunction** (e.g., anorgasmia, decreased libido) and **insomnia** or agitation, especially during the initial weeks of treatment.
*Selective serotonin reuptake inhibitor; hypomania, suicidal thoughts*
- While SSRIs are the correct drug class, **hypomania** is not a frequent side effect in patients without bipolar disorder. For patients with bipolar disorder, antidepressant monotherapy can induce hypomania or mania, but this patient denies such episodes.
- **Suicidal thoughts** can occur, particularly in young adults, during the initial phase of antidepressant treatment, but it is less common to frame it as a *frequently encountered side effect* in the general population compared to sexual dysfunction or sleep disturbances.
*Tricyclic antidepressants; hypomania, suicidal thoughts*
- **Tricyclic antidepressants (TCAs)** are generally not first-line due to their less favorable side effect profile compared to SSRIs, including significant anticholinergic effects and cardiovascular risks.
- As with SSRIs, **hypomania** is not a typical frequent side effect in unipolar depression, and while **suicidal thoughts** are a concern with antidepressants, TCAs carry a higher risk of lethality in overdose, making them less preferred initially.
*Monoamine oxidase inhibitors; Orthostatic hypotension, weight gain*
- **Monoamine oxidase inhibitors (MAOIs)** are effective but are typically reserved for **refractory depression** due to their significant drug and food interactions (e.g., tyramine-induced hypertensive crisis).
- While **orthostatic hypotension** and **weight gain** are known side effects of MAOIs, this class is not considered a first-line treatment for major depressive disorder.
*Tricyclic antidepressants; Orthostatic hypotension, anticholinergic effects*
- **TCAs** are indeed associated with side effects such as **orthostatic hypotension** and prominent **anticholinergic effects** (e.g., dry mouth, constipation, blurred vision, urinary retention).
- However, because of these more burdensome side effects and higher toxicity in overdose, TCAs are not generally considered the first-line medication choice, especially when SSRIs are available and safer.
Premenstrual dysphoric disorder US Medical PG Question 4: A 26-year-old man being treated for major depressive disorder returns to his psychiatrist complaining that he has grown weary of the sexual side effects. Which other medication used to treat major depressive disorder may be appropriate as a stand-alone or add-on therapy?
- A. Venlafaxine
- B. Cyproheptadine
- C. Aripiprazole
- D. Bupropion (Correct Answer)
- E. Paroxetine
Premenstrual dysphoric disorder Explanation: ***Bupropion***
- **Bupropion** is an antidepressant that works via **norepinephrine-dopamine reuptake inhibition**, and unlike most common antidepressants, it is **not associated with sexual dysfunction**.
- It can be used as a **stand-alone treatment** or as an **add-on therapy** to counteract sexual side effects from other antidepressants like SSRIs.
- This makes it the ideal choice for this patient.
*Venlafaxine*
- **Venlafaxine** is a **serotonin-norepinephrine reuptake inhibitor (SNRI)**, and like SSRIs, it can cause or worsen **sexual dysfunction**.
- It is unlikely to resolve the patient's complaint of sexual side effects.
*Cyproheptadine*
- **Cyproheptadine** is an **antihistamine** with **serotonin antagonist** properties that is sometimes used **off-label to treat SSRI-induced sexual dysfunction**.
- However, it is **not an antidepressant** itself and therefore would not be appropriate as a **stand-alone therapy** for major depressive disorder.
- The question specifically asks for "medication used to treat major depressive disorder," which excludes cyproheptadine despite its utility for sexual side effects.
*Aripiprazole*
- **Aripiprazole** is an **atypical antipsychotic** that is approved as an **adjunctive treatment** for major depressive disorder.
- While it can be an add-on, it is **not typically used to mitigate sexual side effects** and can sometimes have its own sexual side effects.
*Paroxetine*
- **Paroxetine** is an **SSRI** that is notoriously associated with a **high incidence of sexual side effects**, including decreased libido, delayed orgasm, and anorgasmia.
- Using paroxetine would likely **exacerbate** rather than alleviate the patient's complaint.
Premenstrual dysphoric disorder US Medical PG Question 5: A 28-year-old woman presents with weight gain and a milky-white discharge from her breasts. Patient says she noticed herself gaining weight and a milky white discharge from her breasts. Past medical history is significant for schizophrenia, recently diagnosed and treated with risperidone. No history of headache, nausea, and vomiting. No other current medications. Her last menstrual period was 2 months ago. Review of systems is significant for decreased libido. Patient is afebrile and vital signs are within normal limits. On physical examination, patient had a weight gain of 3 kg (6.6 lb) over the past month. There is bilateral breast tenderness present. A urine pregnancy test is negative. Which of the following is the most likely etiology of this patient’s symptoms?
- A. Increase in dopamine activity in mesolimbic pathway
- B. Decrease in dopamine activity in mesolimbic pathway
- C. Decrease in dopamine activity in tuberoinfundibular pathway (Correct Answer)
- D. Decrease in dopamine activity in nigrostriatal pathway
- E. Increase in dopamine activity in tuberoinfundibular pathway
Premenstrual dysphoric disorder Explanation: ***Decrease in dopamine activity in tuberoinfundibular pathway***
- The patient is taking **risperidone**, an antipsychotic that blocks **dopamine D2 receptors**. This blockade in the **tuberoinfundibular pathway** leads to increased prolactin secretion.
- Elevated **prolactin** levels cause **galactorrhea** (milky discharge), **amenorrhea** (missed periods), **weight gain**, and **decreased libido**.
*Increase in dopamine activity in mesolimbic pathway*
- An **increase in dopamine activity** in the **mesolimbic pathway** is associated with the positive symptoms of **schizophrenia** (e.g., hallucinations, delusions).
- Antipsychotics like risperidone aim to decrease this activity, not increase it, and this pathway is not directly involved in prolactin regulation.
*Decrease in dopamine activity in mesolimbic pathway*
- A **decrease in dopamine activity** in the **mesolimbic pathway** is the desired therapeutic effect of antipsychotics like risperidone, reducing psychotic symptoms.
- While it explains the treatment of schizophrenia, it does not explain the specific side effects of hyperprolactinemia.
*Decrease in dopamine activity in nigrostriatal pathway*
- A **decrease in dopamine activity** in the **nigrostriatal pathway** is responsible for **extrapyramidal symptoms** (EPS) such as parkinsonism (tremor, rigidity), akathisia, and dystonia.
- While antipsychotics can cause EPS, these are not the predominant symptoms (galactorrhea, weight gain, amenorrhea) described in the patient.
*Increase in dopamine activity in tuberoinfundibular pathway*
- An **increase in dopamine activity** in the **tuberoinfundibular pathway** would lead to a decrease in prolactin secretion, as dopamine is a **prolactin-inhibiting hormone**.
- This would result in symptoms opposite to what the patient is experiencing, such as no galactorrhea or even hypoprolactinemia.
Premenstrual dysphoric disorder US Medical PG Question 6: A 42-year-old woman comes to the physician for evaluation of a 6-month history of irregular menstrual periods. Her last period was 3 months ago. Previously, her periods occurred at regular 28-day intervals and lasted 4–5 days with moderate flow. She has also noticed breast tenderness and scant nipple discharge. She has type 2 diabetes mellitus and refractory bipolar I disorder. Current medications include metformin, glipizide, lithium, and risperidone. Physical examination shows no abnormalities. A urine pregnancy test is negative. Which of the following is the most likely cause of the changes in her menstrual cycle?
- A. Dysregulation of theca and granulosa cell steroidogenesis
- B. Failure of ovaries to respond to gonadotropins
- C. Impaired production and release of thyroxine
- D. Blockade of pituitary dopamine receptors (Correct Answer)
- E. Reduced renal elimination of prolactin
Premenstrual dysphoric disorder Explanation: ***Blockade of pituitary dopamine receptors***
- The patient's symptoms of **irregular menstrual periods**, **breast tenderness**, and **scant nipple discharge** are classic for **drug-induced hyperprolactinemia**.
- **Risperidone**, an atypical antipsychotic, blocks **dopamine D2 receptors** in the **tuberoinfundibular pathway** of the hypothalamus-pituitary axis.
- Normally, dopamine from the hypothalamus **inhibits prolactin release** from lactotrophs in the anterior pituitary. When dopamine receptors are blocked, this tonic inhibition is removed, causing **elevated prolactin levels**.
- Hyperprolactinemia suppresses **GnRH pulsatility**, leading to decreased FSH/LH, which causes **menstrual irregularities** and **hypogonadism**. Elevated prolactin also directly causes **galactorrhea** and **breast tenderness**.
*Dysregulation of theca and granulosa cell steroidogenesis*
- This describes the pathophysiology of **polycystic ovarian syndrome (PCOS)**, which presents with irregular periods, hyperandrogenism, and polycystic ovaries.
- While PCOS causes menstrual irregularities, it does **not** cause nipple discharge or galactorrhea, making it less likely in this case.
*Failure of ovaries to respond to gonadotropins*
- This describes **premature ovarian insufficiency (POI)**, characterized by elevated FSH/LH and low estrogen, leading to irregular or absent menses.
- POI typically presents with **hot flashes** and **vaginal dryness** due to estrogen deficiency, not galactorrhea or breast tenderness.
*Impaired production and release of thyroxine*
- **Primary hypothyroidism** can cause menstrual irregularities and, in severe cases, hyperprolactinemia due to elevated TRH (which stimulates both TSH and prolactin release).
- However, hypothyroidism would typically present with **fatigue**, **weight gain**, **cold intolerance**, and **constipation**, none of which are mentioned in this case.
*Reduced renal elimination of prolactin*
- **Chronic kidney disease** can impair prolactin clearance, leading to hyperprolactinemia and similar symptoms.
- However, there is **no evidence of renal dysfunction** in this patient (no mention of elevated creatinine, proteinuria, or CKD history), and the patient is on metformin (which requires dose adjustment in renal impairment), making drug-induced hyperprolactinemia the more likely cause.
Premenstrual dysphoric disorder US Medical PG Question 7: A 14-year-old girl is brought to the pediatrician by her mother. The girl's mother states that she began having her period 6 months ago. The patient states that after her first period she has had a period every 10 to 40 days. Her menses have ranged from very light flow to intense and severe symptoms. Otherwise, the patient is doing well in school, is on the track team, and has a new boyfriend. Her temperature is 98.1°F (36.7°C), blood pressure is 97/58 mmHg, pulse is 90/min, respirations are 14/min, and oxygen saturation is 99% on room air. Physical exam demonstrates an obese girl but is otherwise within normal limits. Which of the following is the most likely diagnosis?
- A. Normal development (Correct Answer)
- B. Pregnancy
- C. Polycystic ovarian syndrome
- D. Premenstrual tension
- E. Premenstrual dysphoric disorder
Premenstrual dysphoric disorder Explanation: ***Normal development***
- In the first 1-2 years after **menarche**, menstrual cycles are often **irregular** due to the immaturity of the hypothalamic-pituitary-ovarian (HPO) axis, leading to anovulatory cycles.
- The patient's presentation of varied cycle lengths (10-40 days) and flow intensity within 6 months of menarche is consistent with this common physiological phenomenon.
*Pregnancy*
- Although **amenorrhea** is a hallmark of pregnancy, the patient is experiencing periods, albeit irregular.
- There are no other signs or symptoms suggestive of pregnancy like nausea, breast tenderness, or abdominal enlargement.
*Polycystic ovarian syndrome*
- While **irregular menses** and **obesity** are features of PCOS, the patient's symptoms have only been present for a short time (6 months post-menarche).
- PCOS typically involves additional signs of **hyperandrogenism** (e.g., hirsutism, acne, alopecia) or characteristic ovarian morphology on ultrasound, which are not mentioned here.
*Premenstrual tension*
- **Premenstrual tension (PMT)**, often referred to as PMS, involves a constellation of emotional and physical symptoms that cyclically occur in the late luteal phase of the menstrual cycle and resolve with menses.
- The primary concern in this case is the **irregularity of her periods** and menstrual symptoms, rather than a consistent pattern of premenstrual mood or physical complaints separate from the flow itself.
*Premenstrual dysphoric disorder*
- **Premenstrual dysphoric disorder (PMDD)** is a severe form of PMS characterized by significant mood disturbances such as irritability, depression, and anxiety that profoundly affect daily functioning.
- The patient's reported symptoms focus on variability in her menstrual cycle and flow, not on severe, debilitating mood shifts occurring consistently before her menses, and she is otherwise noted to be "doing well."
Premenstrual dysphoric disorder US Medical PG Question 8: A 27-year-old woman presents to your office complaining of right arm numbness and weakness. Her past medical history is unremarkable. Her family history, however, is significant for the unexpected death of both her parents at age 59 in a motor vehicle accident last week. On physical exam, her bicep, brachioradialis, and patellar reflexes are 2+ bilaterally. CNS imaging shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Amyotrophic lateral sclerosis
- B. Multiple sclerosis
- C. Conversion disorder (Correct Answer)
- D. Arnold-Chiari malformation
- E. Vitamin B12 deficiency
Premenstrual dysphoric disorder Explanation: ***Conversion disorder***
- The patient's presentation of **numbness and weakness** following a significant **psychological stressor** (parents' deaths) with a normal neurological exam and imaging is classic for conversion disorder.
- In conversion disorder, neurological symptoms are inconsistent with known neurological pathways or conditions, and symptoms are often out of patient's conscious control.
*Amyotrophic lateral sclerosis*
- This condition involves both **upper and lower motor neuron signs**, such as **spasticity, hyperreflexia**, and muscle atrophy, which are not described in this patient's presentation.
- ALS typically progresses over time, and the patient's symptoms are acute and without objective neurological findings.
*Multiple sclerosis*
- MS is characterized by **demyelinating lesions in the CNS** leading to various neurological deficits, which would be visible on CNS imaging.
- The patient's normal CNS imaging and unremarkable medical history make MS less likely.
*Arnold-Chiari malformation*
- This is a structural defect in the cerebellum and brainstem that can cause a range of neurological symptoms, often present from birth or early childhood.
- However, typical MRI findings for Chiari malformation would be present, and the acute onset after psychological stress is not characteristic.
*Vitamin B12 deficiency*
- Can cause **neurological symptoms** such as **paresthesias, weakness, and ataxia**, but it would likely present with other systemic effects like anemia and would typically involve abnormal neurological findings or lab values.
- The acute, localized symptoms following stress, absence of other signs, and normal imaging make this diagnosis unlikely.
Premenstrual dysphoric disorder US Medical PG Question 9: An 11-year-old boy is brought to the clinic by his parents for poor academic performance. The patient’s parents say that his teacher told them that he may have to repeat a grade because of his lack of progress, as he does not pay attention to the lessons, tends to fidget about in his seat, and often blurts out comments when it is someone else’s turn to speak. Furthermore, his after-school karate coach says the patient no longer listens to instructions and has a hard time focusing on the activity at hand. The patient has no significant past medical history and is currently not on any medications. The patient has no known learning disabilities and has been meeting all developmental milestones. The parents are vehemently opposed to using any medication with a potential for addiction. Which of the following medications is the best course of treatment for this patient?
- A. Sertraline
- B. Diazepam
- C. Olanzapine
- D. Methylphenidate
- E. Atomoxetine (Correct Answer)
Premenstrual dysphoric disorder Explanation: ***Atomoxetine***
- This medication is a **non-stimulant** selective norepinephrine reuptake inhibitor. It is a good choice for **ADHD patients** whose parents are opposed to any medication with a potential for addiction because it does not have the same addictive potential as stimulants.
- It works by increasing the levels of **norepinephrine** in the brain, improving attention and hyperactivity symptoms typically seen in ADHD.
*Sertraline*
- This is a **selective serotonin reuptake inhibitor (SSRI)** and is primarily used to treat depression, anxiety disorders, and obsessive-compulsive disorder.
- Sertraline would not be effective for ADHD symptoms like inattention and hyperactivity.
*Diazepam*
- This is a **benzodiazepine** primarily used for anxiety, seizures, and muscle spasms due to its sedative and anxiolytic properties.
- It would likely worsen the patient's inattention and academic performance due to its **sedative effects** and has a significant potential for addiction.
*Olanzapine*
- This is an **atypical antipsychotic** medication used to treat conditions like schizophrenia and bipolar disorder.
- Olanzapine is not indicated for ADHD and could cause severe side effects like **sedation, weight gain, and metabolic issues**.
*Methylphenidate*
- This is a **stimulant medication** commonly used to treat ADHD and is highly effective in improving attention and reducing hyperactivity.
- While effective, methylphenidate has a **potential for abuse and addiction**, which the patient's parents are explicitly against.
Premenstrual dysphoric disorder US Medical PG Question 10: A 36-year-old woman comes to the physician because of an 8-month history of occasional tremor. The tremor is accompanied by sudden restlessness and nausea, which disrupts her daily work as a professional violinist. The symptoms worsen shortly before upcoming concerts but also appear when she goes for a walk in the city. She is concerned that she might have a neurological illness and have to give up her career. The patient experiences difficulty falling asleep because she cannot stop worrying that a burglar might break into her house. Her appetite is good. She drinks one glass of wine before performances "to calm her nerves" and otherwise drinks 2–3 glasses of wine per week. The patient takes daily multivitamins as prescribed. She appears nervous. Her temperature is 36.8°C (98.2°F), pulse is 92/min, and blood pressure is 135/80 mm Hg. Mental status examination shows a full range of affect. On examination, a fine tremor on both hands is noted. She exhibits muscle tension. The remainder of the neurological exam shows no abnormalities. Which of the following is the most likely explanation for this patient's symptoms?
- A. Atypical depressive disorder
- B. Adjustment disorder
- C. Generalized anxiety disorder (Correct Answer)
- D. Panic disorder
- E. Essential tremor
Premenstrual dysphoric disorder Explanation: ***Generalized anxiety disorder***
- The patient exhibits persistent and excessive worry about various life circumstances (performance, burglaries, general anxiety), accompanied by physical symptoms like **restlessness**, muscle tension, and sleep disturbances, which are hallmark features of **Generalized Anxiety Disorder (GAD)**.
- The symptoms have been present for **8 months**, exceed the diagnostic duration for GAD (at least 6 months), and are not clearly tied to a specific stressor or episodic panic attacks.
*Atypical depressive disorder*
- Atypical depression is characterized by mood reactivity, increased appetite/weight gain, hypersomnia, leaden paralysis, and interpersonal rejection sensitivity.
- This patient reports difficulty sleeping (*insomnia*) and primarily presents with anxiety symptoms, not depressive mood.
*Adjustment disorder*
- **Adjustment disorder** involves emotional or behavioral symptoms in response to an identifiable stressor, occurring within 3 months of the stressor's onset, and usually resolving within 6 months after the stressor or its consequences have ceased.
- The patient's symptoms are chronic (8 months), excessive, and not solely linked to *one* identifiable recent stressor, but rather a pervasive pattern of worry.
*Panic disorder*
- **Panic disorder** is characterized by recurrent unexpected **panic attacks** with sudden onset of intense fear and physical symptoms (e.g., palpitations, dyspnea, dizziness).
- While she experiences sudden restlessness and nausea related to performances, these are specific triggers and not unexpected, unprovoked panic attacks. The primary pattern is persistent worry, not recurrent panic attacks.
*Essential tremor*
- **Essential tremor** is a neurological condition causing an *action tremor*, often visible when performing daily tasks, and typically improves with alcohol.
- While she has a tremor that improves with alcohol, the presence of marked and pervasive psychological symptoms like severe worrying, restlessness, and insomnia point to an underlying anxiety disorder, not solely an isolated neurological tremor.
More Premenstrual dysphoric disorder US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.