Geriatric mood disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Geriatric mood disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Geriatric mood disorders US Medical PG Question 1: A 59-year-old man with a history of major depressive disorder, asthma, and erectile dysfunction presents to his family physician complaining of depressed mood, amotivation, overeating, and anhedonia. He currently takes no medications. The patient has a 3 pack-year smoking history and would like to quit but has been unsuccessful in the past. His BMI is 29 kg/m^2. The physician suggests starting an antidepressant for the patient's mood symptoms. The patient is reluctant, as he used to take sertraline, but stopped it after his erectile dysfunction worsened. Which of the following antidepressants would be most appropriate for this patient?
- A. Citalopram
- B. Bupropion (Correct Answer)
- C. Sertraline
- D. Mirtazapine
- E. Amitriptyline
Geriatric mood disorders Explanation: **Bupropion**
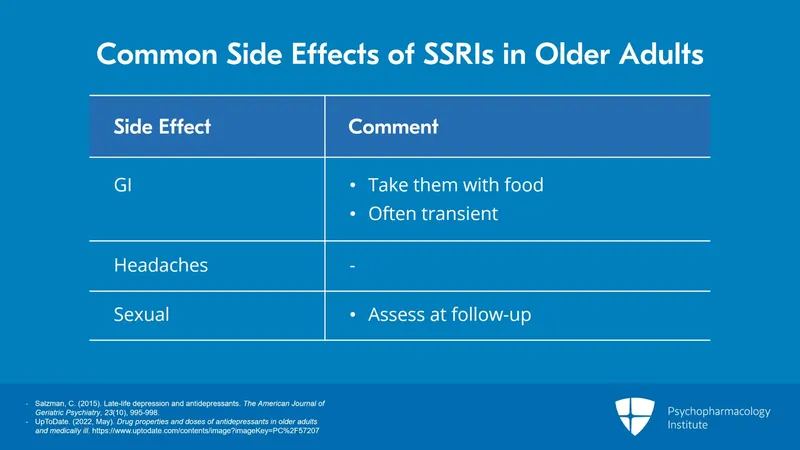
- **Bupropion** is an antidepressant that does not typically cause **sexual dysfunction** and can aid in **smoking cessation**, addressing two key concerns for this patient.
- It acts by inhibiting the reuptake of **norepinephrine** and **dopamine**, which can also help with **amotivation** and **anhedonia**.
*Citalopram*
- **Citalopram** is an **SSRI** (selective serotonin reuptake inhibitor), a class of drugs commonly associated with causing or worsening **sexual dysfunction**, which is a significant concern for this patient.
- While effective for depression, it does not offer the additional benefit of aiding in **smoking cessation**.
*Sertraline*
- The patient previously stopped **sertraline** due to worsening **erectile dysfunction**, indicating that this **SSRI** is not a suitable option for him.
- Reintroducing **sertraline** would likely lead to similar adverse effects and patient non-adherence.
*Mirtazapine*
- **Mirtazapine** is an antidepressant that can cause **weight gain** and **sedation**, which would be undesirable for a patient with a BMI of 29 kg/m^2 who also needs to quit smoking.
- Although it has a lower incidence of sexual dysfunction compared to SSRIs, it does not offer benefits for **smoking cessation**.
*Amitriptyline*
- **Amitriptyline** is a **tricyclic antidepressant (TCA)** known for significant side effects such as **anticholinergic effects** (e.g., dry mouth, constipation, urinary retention), **sedation**, and **cardiac toxicity** in overdose.
- Given the patient's age and history, a TCA would likely be poorly tolerated and poses higher risks compared to other options.
Geriatric mood disorders US Medical PG Question 2: A case-control study with a focus on risk factors that may influence the development of depression was conducted among the elderly population in one tertiary hospital in Malaysia. The study involved 150 elderly patients diagnosed with depressive illness from the psychiatry ward, as well as another group of 150 elderly patients without any history of depressive illness (but hospitalized for other reasons) at the same ward. The data were collected through questionnaires, and 2 principal investigators (who were also the patients’ attending physicians) acted as interviewers after proper training for the purposes of this study. Multivariate analyses of logistic regression with independent variables were employed to determine the adjusted odds ratio for the risk of developing depression. The study results showed that a lower level of social support, lack of education, and the presence of chronic illnesses highly correlated with depression. In order to maximally avoid bias that may stem from this kind of study design, what should the researchers have done differently to increase the validity of their results?
- A. Used open-ended questions
- B. Blinded the investigators (Correct Answer)
- C. Included more interviewers
- D. Used closed testing procedures on the data
- E. Used Bonferroni correction on data
Geriatric mood disorders Explanation: ***Blinded the investigators***
- Blinding the investigators (interviewers) would prevent them from knowing which patients were cases (depressed) and which were controls (non-depressed). This reduces the risk of **interviewer bias**, where their preconceptions or knowledge of participants' status might influence how they ask questions or interpret responses, thereby distorting the results.
- Given that the principal investigators were also the patients' attending physicians, they likely had prior knowledge of the patients' depressive status, which could lead to **detection bias** or information bias. Blinding would help standardize data collection.
*Used open-ended questions*
- While open-ended questions can provide rich qualitative data, they can introduce **variability and subjectivity** in responses and interpretation, potentially making comparisons more challenging and increasing the investigator's influence on data collection.
- For a case-control study focused on quantifiable risk factors, **structured questionnaires** are often preferred for consistency and easier statistical analysis, although a mix can be optimal.
*Included more interviewers*
- Simply including more interviewers does not inherently improve validity; it could even increase **inter-rater variability** if they are not adequately trained and standardized.
- The critical aspect is the **standardization of data collection** and the avoidance of bias, not merely the number of individuals collecting data.
*Used closed testing procedures on the data*
- "Closed testing procedures on the data" is not a standard term in research methodology in this context. Assuming it refers to using a **pre-defined set of statistical tests**, this does not directly address potential biases in data collection or patient selection.
- The issue here is related to **information bias** and **selection bias** stemming from the study design and interviewer role, not primarily the statistical analysis procedures.
*Used Bonferroni correction on data*
- **Bonferroni correction** is used to adjust the p-values when performing multiple statistical comparisons on the same data set to reduce the chance of making a **Type I error** (false positive).
- This correction addresses issues in **statistical analysis** (minimizing spurious findings due to multiple testing), not biases that arise during the design, data collection, or participant identification phases of a study.
Geriatric mood disorders US Medical PG Question 3: A 66-year-old man is brought into the emergency department by his daughter for a change in behavior. Yesterday the patient seemed more confused than usual and was asking the same questions repetitively. His symptoms have not improved over the past 24 hours, thus the decision to bring him in today. Last year, the patient was almost completely independent but he then suffered a "series of falls," after which his ability to care for himself declined. After this episode he was no longer able to cook for himself or pay his bills but otherwise had been fine up until this episode. The patient has a past medical history of myocardial infarction, hypertension, depression, diabetes mellitus type II, constipation, diverticulitis, and peripheral neuropathy. His current medications include metformin, insulin, lisinopril, hydrochlorothiazide, sodium docusate, atorvastatin, metoprolol, fluoxetine, and gabapentin. On exam you note a confused man who is poorly kept. He has bruises over his legs and his gait seems unstable. He is alert to person and place, and answers some questions inappropriately. The patient's pulse is 90/minute and his blood pressure is 170/100 mmHg. Which of the following is the most likely diagnosis?
- A. Normal aging
- B. Lewy body dementia
- C. Vascular dementia (Correct Answer)
- D. Pseudodementia (depression-related cognitive impairment)
- E. Alzheimer's dementia
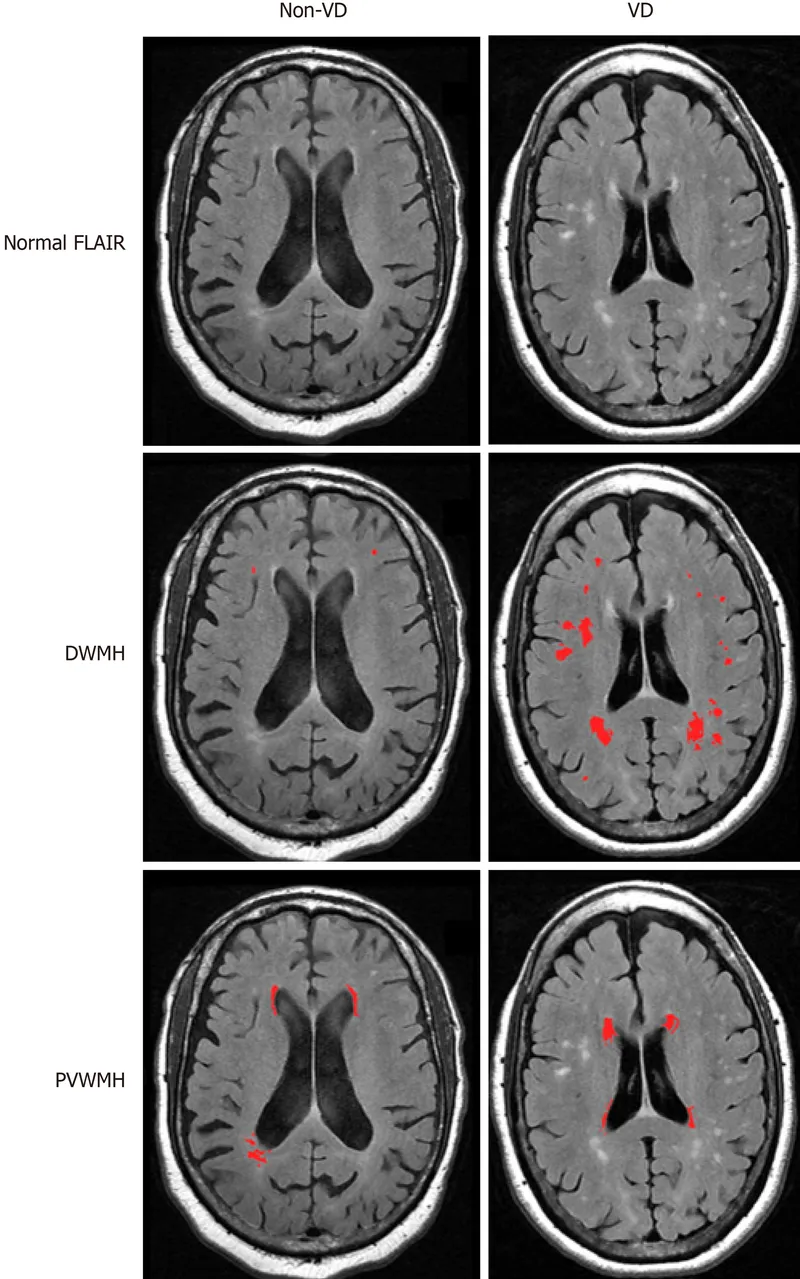
Geriatric mood disorders Explanation: ***Vascular dementia***
- This diagnosis is strongly supported by the patient's **stepwise decline** in cognitive function following a "series of falls" (likely small strokes or transient ischemic attacks) and his extensive history of **vascular risk factors** including hypertension, diabetes, and previous myocardial infarction.
- The acute worsening of confusion over 24 hours, coupled with pre-existing impaired executive function (inability to cook or pay bills), is characteristic of **vascular dementia's fluctuating course** and presentation often linked to new cerebrovascular events.
*Incorrect: Normal aging*
- **Normal aging** involves a very gradual and mild decline in cognitive functions, primarily affecting processing speed and memory recall, without significant impairment in daily activities.
- This patient's rapid, stepwise decline and inability to perform instrumental activities of daily living (IADLs) such as cooking and managing finances go beyond what is considered normal cognitive changes with aging.
*Incorrect: Lewy body dementia*
- **Lewy body dementia** is characterized by prominent **fluctuations in attention and alertness**, recurrent visual hallucinations, and spontaneous parkinsonism, none of which are explicitly mentioned as primary features in this patient's presentation.
- While fluctuations in confusion are present, the history of a clear stepwise decline post-falls and significant vascular risk factors points away from Lewy body dementia as the most likely primary cause.
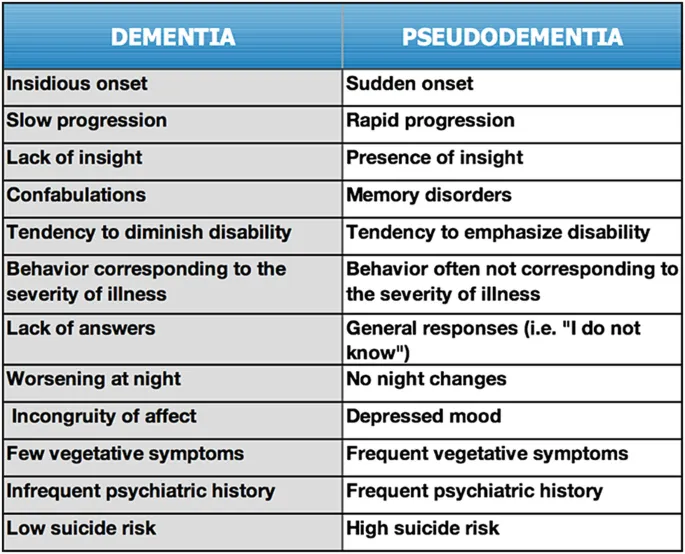
*Incorrect: Pseudodementia (depression-related cognitive impairment)*
- **Pseudodementia** refers to cognitive impairment that occurs in the context of **major depression**, where patients may exhibit poor concentration, memory difficulties, and psychomotor slowing that mimics dementia.
- While this patient is on fluoxetine for depression, the **stepwise decline** after clear vascular events (falls), multiple vascular risk factors, and impaired executive function point to a true neurodegenerative process rather than depression-induced cognitive changes, which typically improve with treatment of the underlying mood disorder.
*Incorrect: Alzheimer's dementia*
- **Alzheimer's dementia** typically presents with a **gradual and progressive decline** in memory, particularly episodic memory, followed by other cognitive domains over several years.
- The patient's history of a clear **stepwise decline** in function after acute events (falls) and the strong presence of **vascular risk factors** make vascular dementia a more fitting diagnosis than Alzheimer's, which is not typically associated with such a sudden, step-like progression.
Geriatric mood disorders US Medical PG Question 4: An 82-year-old woman comes to the physician because of difficulty sleeping and increasing fatigue. Over the past 3 months she has been waking up early and having trouble falling asleep at night. During this period, she has had a decreased appetite and a 3.2-kg (7-lb) weight loss. Since the death of her husband one year ago, she has been living with her son and his wife. She is worried and feels guilty because she does not want to impose on them. She has stopped going to meetings at the senior center because she does not enjoy them anymore and also because she feels uncomfortable asking her son to give her a ride, especially since her son has had a great deal of stress lately. She is 155 cm (5 ft 1 in) tall and weighs 51 kg (110 lb); BMI is 21 kg/m2. Vital signs are within normal limits. Physical examination shows no abnormalities. On mental status examination, she is tired and has a flattened affect. Cognition is intact. Which of the following is the most appropriate initial step in management?
- A. Begin mirtazapine therapy
- B. Begin cognitive-behavioral therapy
- C. Notify adult protective services
- D. Assess for suicidal ideation (Correct Answer)
- E. Recommend relocation to a nursing home
Geriatric mood disorders Explanation: ***Assess for suicidal ideation***
- The patient exhibits several **risk factors for depression**, including **insomnia**, **early morning awakening**, **anorexia**, **weight loss**, and significant **anhedonia** (lack of enjoyment in activities).
- Given her age, recent loss of her husband, social withdrawal, feelings of guilt, and significant emotional distress, it is crucial to first assess for **suicidal ideation** before initiating other treatments.
- **Elderly patients with depression have elevated suicide risk**, especially with recent bereavement and social isolation. Safety assessment is the **mandatory first step** in managing any patient with major depressive symptoms.
*Begin mirtazapine therapy*
- While **mirtazapine** is an effective antidepressant that could address several of her symptoms (insomnia, poor appetite, depression), it should only be considered after a **thorough safety assessment**, particularly for suicide risk.
- Starting medication without assessing for immediate danger may overlook critical safety concerns.
*Begin cognitive-behavioral therapy*
- **Cognitive-behavioral therapy (CBT)** is an effective treatment for depression and could be beneficial for this patient.
- However, similar to medication, it is a subsequent treatment step. The immediate priority is to rule out **suicidal intent** given the severity of her depressive symptoms.
*Notify adult protective services*
- There is no direct evidence of **abuse or neglect** in the provided information that would warrant involving adult protective services.
- Her feelings of guilt and worry about burdening her family, while contributing to her depression, do not indicate that her son or daughter-in-law are harming her.
*Recommend relocation to a nursing home*
- While the patient is elderly and potentially depressed, there is no medical or social necessity presented that indicates she requires or would benefit from a **nursing home** at this stage.
- This step would be premature and does not address the immediate mental health concerns or potential safety issues.
Geriatric mood disorders US Medical PG Question 5: A 26-year-old man being treated for major depressive disorder returns to his psychiatrist complaining that he has grown weary of the sexual side effects. Which other medication used to treat major depressive disorder may be appropriate as a stand-alone or add-on therapy?
- A. Venlafaxine
- B. Cyproheptadine
- C. Aripiprazole
- D. Bupropion (Correct Answer)
- E. Paroxetine
Geriatric mood disorders Explanation: ***Bupropion***
- **Bupropion** is an antidepressant that works via **norepinephrine-dopamine reuptake inhibition**, and unlike most common antidepressants, it is **not associated with sexual dysfunction**.
- It can be used as a **stand-alone treatment** or as an **add-on therapy** to counteract sexual side effects from other antidepressants like SSRIs.
- This makes it the ideal choice for this patient.
*Venlafaxine*
- **Venlafaxine** is a **serotonin-norepinephrine reuptake inhibitor (SNRI)**, and like SSRIs, it can cause or worsen **sexual dysfunction**.
- It is unlikely to resolve the patient's complaint of sexual side effects.
*Cyproheptadine*
- **Cyproheptadine** is an **antihistamine** with **serotonin antagonist** properties that is sometimes used **off-label to treat SSRI-induced sexual dysfunction**.
- However, it is **not an antidepressant** itself and therefore would not be appropriate as a **stand-alone therapy** for major depressive disorder.
- The question specifically asks for "medication used to treat major depressive disorder," which excludes cyproheptadine despite its utility for sexual side effects.
*Aripiprazole*
- **Aripiprazole** is an **atypical antipsychotic** that is approved as an **adjunctive treatment** for major depressive disorder.
- While it can be an add-on, it is **not typically used to mitigate sexual side effects** and can sometimes have its own sexual side effects.
*Paroxetine*
- **Paroxetine** is an **SSRI** that is notoriously associated with a **high incidence of sexual side effects**, including decreased libido, delayed orgasm, and anorgasmia.
- Using paroxetine would likely **exacerbate** rather than alleviate the patient's complaint.
Geriatric mood disorders US Medical PG Question 6: A 77-year-old Caucasian woman presents to her primary care provider for a general checkup. The patient is with her daughter who brought her to this appointment. The patient states that she is doing well and has some minor joint pain in both hips. She states that sometimes she is sad because her husband recently died. She lives alone and follows a vegan diet. The patient's daughter states that she has noticed her mother struggling with day to day life. It started 2 years ago with her forgetting simple instructions or having difficulty running errands. Now the patient has gotten to the point where she can no longer pay her bills. Sometimes the patient forgets how to get home. The patient has a past medical history of obesity, hypertension, gastroesophageal reflux disease (GERD) controlled with pantoprazole, and diabetes mellitus. Her temperature is 99.5°F (37.5°C), blood pressure is 158/108 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 98% on room air. Which of the following will most likely help with this patient's presentation?
- A. Vitamin B12 and discontinue pantoprazole
- B. No intervention needed
- C. Donepezil (Correct Answer)
- D. Fluoxetine and cognitive behavioral therapy
- E. Lisinopril and metoprolol
Geriatric mood disorders Explanation: ***Correct: Donepezil***
- This patient presents with **progressive dementia**, most consistent with **Alzheimer's disease**: gradual cognitive decline over 2 years, short-term memory loss (forgetting instructions), executive dysfunction (unable to pay bills), impaired navigation (getting lost), and functional decline in activities of daily living (ADLs).
- **Donepezil**, an **acetylcholinesterase inhibitor**, is first-line pharmacotherapy for mild-to-moderate Alzheimer's disease, improving cognitive function by increasing acetylcholine availability in the brain.
- Key differentiator: The **progressive, global cognitive impairment** with functional decline over years distinguishes this from reversible causes or mood disorders.
*Incorrect: Vitamin B12 and discontinue pantoprazole*
- While **vitamin B12 deficiency** can cause cognitive impairment and this patient has risk factors (vegan diet, chronic PPI use with pantoprazole), the **severity, duration, and progressive nature** of her symptoms indicate a **neurodegenerative process** rather than a reversible nutritional deficiency.
- B12 deficiency typically presents with more prominent neurological signs (peripheral neuropathy, subacute combined degeneration) and would be expected to show improvement with supplementation.
- Though checking B12 levels would be part of the dementia workup, it would not be the **primary treatment** for this presentation.
*Incorrect: No intervention needed*
- This patient has **significant functional impairment** with safety concerns (getting lost, inability to manage finances), requiring immediate intervention.
- Progressive cognitive decline causing loss of independence in ADLs is never "normal aging" and always warrants medical evaluation and treatment.
- Failure to intervene risks patient safety and further deterioration.
*Incorrect: Fluoxetine and cognitive behavioral therapy*
- While the patient reports sadness related to her husband's death (suggesting **grief** or possible **depression**), her **predominant symptoms are cognitive and functional**, not primarily mood-related.
- **Key differentiation**: Depression can cause "pseudodementia" with cognitive complaints, but true dementia shows objective functional decline (inability to pay bills, getting lost) that progresses regardless of mood, whereas depression-related cognitive symptoms typically improve with mood treatment.
- The **2-year progressive course** with worsening executive function points to **organic dementia**, not a primary mood disorder.
- Fluoxetine and CBT target depression but would not address the underlying neurodegenerative process.
*Incorrect: Lisinopril and metoprolol*
- The patient's blood pressure is elevated (158/108 mmHg), indicating uncontrolled **hypertension** that should be managed.
- While controlling vascular risk factors is important in dementia management (to prevent vascular dementia progression), treating hypertension would not address her **current cognitive symptoms** or provide symptomatic relief.
- The **primary issue** is dementia requiring acetylcholinesterase inhibitor therapy; blood pressure management is secondary.
Geriatric mood disorders US Medical PG Question 7: A 27-year old gentleman presents to the primary care physician with the chief complaint of "feeling down" for the last 6 weeks. He describes trouble falling asleep at night, decreased appetite, and recent feelings of intense guilt regarding the state of his personal relationships. He says that everything "feels slower" than it used to. He endorses having a similar four-week period of feeling this way last year. He denies thoughts of self-harm or harm of others. He also denies racing thoughts or delusions of grandeur. Which of the following would be an INAPPROPRIATE first line treatment for him?
- A. Paroxetine
- B. Electroconvulsive therapy (Correct Answer)
- C. Citalopram
- D. Psychotherapy
- E. Sertraline
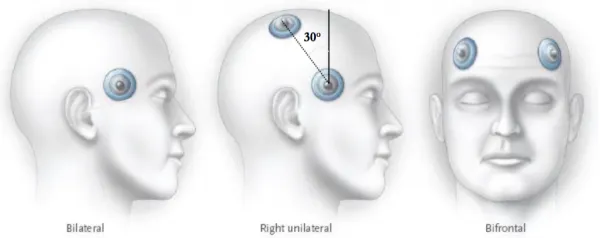
Geriatric mood disorders Explanation: ***Electroconvulsive therapy***
- This is generally reserved for **severe depression** that is unresponsive to other treatments or for depression with **psychotic features**, severe suicidality, or catatonia.
- Given the patient's presentation, **ECT** would be an overly aggressive **first-line** treatment choice.
*Paroxetine*
- **Paroxetine** is a **SSRI** and is considered a **first-line antidepressant** for major depressive disorder.
- It works by increasing serotonin levels in the brain to improve mood.
*Citalopram*
- **Citalopram** is an **SSRI** and is also a **first-line treatment option** for major depressive disorder, often well-tolerated.
- It helps regulate mood and alleviate symptoms like those described by the patient.
*Psychotherapy*
- **Psychotherapy**, particularly **cognitive-behavioral therapy (CBT)** or **interpersonal therapy (IPT)**, is often a **first-line treatment**, either alone or in combination with medication, for depression.
- It can help the patient address negative thought patterns and coping mechanisms.
*Sertraline*
- **Sertraline** is another **SSRI** commonly used as a **first-line agent** for major depressive disorder due to its efficacy and relatively favorable side-effect profile.
- It helps to improve symptoms such as low mood, sleep disturbances, and decreased appetite.
Geriatric mood disorders US Medical PG Question 8: A 29-year-old man is being monitored at the hospital after cutting open his left wrist. He has a long-standing history of unipolar depressive disorder and multiple trials of antidepressants. The patient expresses thoughts of self-harm and does not deny suicidal intent. A course of electroconvulsive therapy is suggested. His medical history is not significant for other organic illness. Which of the following complications of this therapy is this patient at greatest risk for?
- A. Acute kidney injury
- B. Acute coronary syndrome
- C. Anterograde amnesia
- D. Intracranial hemorrhage
- E. Retrograde amnesia (Correct Answer)
Geriatric mood disorders Explanation: ***Retrograde amnesia***
- **Retrograde amnesia**, specifically memory loss for events occurring prior to the treatment, is a common and often transient side effect of **electroconvulsive therapy (ECT)**.
- While generally temporary, it can be distressing for patients and is a significant consideration when recommending ECT, especially in patients with otherwise healthy brains.
*Acute kidney injury*
- **Acute kidney injury (AKI)** is not a typical direct complication of **ECT**.
- While fluid and electrolyte imbalances or certain medications used during ECT (e.g., muscle relaxants) could theoretically impact renal function in predisposed individuals, it is not a primary concern in a patient with no significant history of organic illness.
*Acute coronary syndrome*
- **Acute coronary syndrome (ACS)** is a potential risk associated with the physiological stress of **ECT**, which can include transient **hypertension** and **tachycardia**.
- However, in a 29-year-old with no significant medical history, the risk is considerably lower compared to older patients or those with pre-existing cardiovascular disease.
*Anterograde amnesia*
- **Anterograde amnesia**, the inability to form new memories after the treatment, is typically less common and usually milder than retrograde amnesia following **ECT**.
- While some patients may experience transient difficulty recalling new information immediately post-ECT, it is usually less pronounced than the impact on remote memories.
*Intracranial hemorrhage*
- **Intracranial hemorrhage** is an extremely rare and severe complication of **ECT**, typically associated with pre-existing cerebral vascular abnormalities or uncontrolled hypertension during the procedure.
- In a young patient with no organic illness, the risk of this complication is exceedingly low.
Geriatric mood disorders US Medical PG Question 9: A 26-year-old female college student is brought back into the university clinic for acting uncharacteristically. The patient presented to the same clinic 6 weeks ago with complaints of depressed mood, insomnia, and weightloss. She had been feeling guilty for wasting her parent’s money by doing so poorly at the university. She felt drained for at least 2 weeks before presenting to the clinic for the first time. She was placed on an antidepressant and was improving but now presents with elevated mood. She is more talkative with a flight of ideas and is easily distractible. Which of the following statements is most likely true regarding this patient’s condition?
- A. The patient may have psychotic features.
- B. Her diagnosis of unipolar depression is incorrect. (Correct Answer)
- C. The patient may have a history of mania.
- D. Antidepressants are inappropriate.
- E. Her new symptoms need to last at least 7 days.
Geriatric mood disorders Explanation: ***Correct: Her diagnosis of unipolar depression is incorrect.***
The patient initially presented with symptoms consistent with a **depressive episode**, but the subsequent emergence of **elevated mood, increased talkativeness, flight of ideas, and distractibility after antidepressant use** strongly suggests a shift to a **manic or hypomanic episode**. This antidepressant-induced mood switch is a hallmark feature revealing **bipolar disorder** that was initially misdiagnosed as unipolar depression. This statement most directly addresses **what is true about this patient's condition** - that the fundamental diagnosis is incorrect. Once we establish the correct diagnosis of bipolar disorder, all treatment and management decisions follow from this.
*Incorrect: The patient may have psychotic features.*
While patients with severe **mania** can develop **psychotic features** (e.g., delusions, hallucinations), the provided symptoms (elevated mood, increased talkativeness, flight of ideas, distractibility) do not describe psychotic symptoms. There is no information suggesting the presence of **delusions or hallucinations**, which are necessary to diagnose psychotic features. The word "may" makes this theoretically possible but not supported by the clinical presentation described.
*Incorrect: The patient may have a history of mania.*
While patients with bipolar disorder often have previous undiagnosed episodes, this statement is speculative about her **past history** rather than addressing what is most directly evident from the **current presentation**. The vignette focuses on the antidepressant-induced mood switch, which immediately reveals that the current diagnosis of unipolar depression is incorrect. Whether or not she had previous manic episodes is less relevant than recognizing the misdiagnosis now.
*Incorrect: Antidepressants are inappropriate.*
This statement is clinically **true in principle** - antidepressants as monotherapy are generally inappropriate for bipolar disorder due to the risk of inducing mania or hypomania. However, this option addresses **treatment implications** rather than directly stating what is true about **the patient's condition itself**. The more fundamental and direct truth is that **her diagnosis is wrong** (bipolar, not unipolar depression). Once the correct diagnosis is established, then the inappropriateness of antidepressant monotherapy follows. Additionally, at the time of initial presentation with pure depressive symptoms, the antidepressant prescription was reasonable based on the information available - the inappropriateness only became clear retrospectively after the mood switch occurred.
*Incorrect: Her new symptoms need to last at least 7 days.*
For a diagnosis of **mania**, symptoms must last at least **one week** (or any duration if hospitalization is required). However, for **hypomania**, symptoms need to last only **4 consecutive days**. The vignette does not specify whether this is mania or hypomania, nor does it clearly state the duration of the current symptoms beyond "now presents." Therefore, we cannot definitively say a 7-day duration is required - it could be hypomania requiring only 4 days. This statement is not necessarily true.
Geriatric mood disorders US Medical PG Question 10: Ten days after the vaginal delivery of a healthy infant girl, a 27-year-old woman is brought to the physician by her husband because of frequent mood changes. She has been tearful and anxious since she went home from the hospital 2 days after delivery. She says that she feels overwhelmed with her new responsibilities and has difficulties taking care of her newborn because she feels constantly tired. She only sleeps for 2 to 3 hours nightly because the baby “is keeping her awake.” Sometimes, the patient checks on her daughter because she thinks she heard her cry but finds her sleeping quietly. Her husband says that she is afraid that something could happen to the baby. She often gets angry at him and has yelled at him when he picks up the baby without using a hand sanitizer beforehand. She breastfeeds the baby without any problems. The patient's mother has bipolar disorder with psychotic features. The patient's vital signs are within normal limits. Physical examination shows an involuting uterus consistent in size with her postpartum date. Mental status examination shows a labile affect with no evidence of homicidal or suicidal ideation. Laboratory studies show a hemoglobin concentration of 13 g/dL and a thyroid-stimulating hormone level of 3.1 μU/mL. Which of the following is the most appropriate next step in management?
- A. Risperidone therapy
- B. Bupropion therapy
- C. Cognitive behavioral therapy
- D. Reassurance (Correct Answer)
- E. Sertraline therapy
Geriatric mood disorders Explanation: ***Reassurance***
- The patient exhibits symptoms of **"baby blues"**, including tearfulness, anxiety, mood swings, and feeling overwhelmed, which are common within the first two weeks postpartum and typically resolve spontaneously.
- Given the transient nature of **baby blues** and the absence of more severe symptoms like psychosis or significant functional impairment, **reassurance** and supportive care are the most appropriate initial steps.
*Risperidone therapy*
- **Risperidone** is an **antipsychotic** medication used for conditions like psychosis or severe mood disorders, which are not present in this patient's mild, transient symptoms of baby blues.
- Initiating antipsychotic therapy for **self-limiting baby blues** is unnecessary and could lead to unwanted side effects.
*Bupropion therapy*
- **Bupropion** is an **antidepressant** primarily used for major depressive disorder and seasonal affective disorder, and is not indicated for the mild, transient symptoms of **baby blues**.
- Its mechanism of action involves dopamine and norepinephrine reuptake inhibition, differing from typical SSRIs often considered for postpartum depression.
*Cognitive behavioral therapy*
- While **CBT** is an effective treatment for **postpartum depression** and anxiety disorders, the patient's symptoms are consistent with **baby blues**, which are self-limiting and resolve with supportive care in most cases.
- CBT would be more appropriate if the symptoms were severe, persistent beyond two weeks, or indicative of a more significant mood disorder.
*Sertraline therapy*
- **Sertraline** is an **SSRI antidepressant** commonly used for **postpartum depression** and anxiety, but it is not indicated for the transient and mild symptoms of **baby blues**.
- Antidepressants are typically reserved for more severe and persistent symptoms characteristic of postpartum depression, which usually lasts longer than two weeks.
More Geriatric mood disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.