Comorbidities with mood disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Comorbidities with mood disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Comorbidities with mood disorders US Medical PG Question 1: A 19-year-old woman is brought to the physician by her parents because of irritable mood that started 5 days ago. Since then, she has been staying up late at night working on a secret project. She is energetic despite sleeping less than 4 hours per day. Her parents report that she seems easily distracted. She is usually very responsible, but this week she spent her paycheck on supplies for her project. She has never had similar symptoms before. In the past, she has had episodes where she felt too fatigued to go to school and slept until 2 pm every day for 2 weeks at a time. During those times, her parents noticed that she cried excessively, was very indecisive, and expressed feelings of worthlessness. Two months ago, she had an asthma exacerbation and was treated with bronchodilators and steroids. She tried cocaine once in high school but has not used it since. Vital signs are within normal limits. On mental status examination, she is irritable but cooperative. Her speech is pressured and her thought process is linear. Which of the following is the most likely diagnosis?
- A. Major depressive disorder
- B. Bipolar I disorder
- C. Bipolar II disorder (Correct Answer)
- D. Schizoaffective disorder
- E. Substance abuse
Comorbidities with mood disorders Explanation: ***Bipolar II disorder***
- This patient exhibits symptoms consistent with both **hypomania** (increased energy, decreased need for sleep, irritability, distractibility, spending sprees) and past episodes of **major depression** (fatigue, hypersomnia, crying, indecisiveness, worthlessness). The key distinction for Bipolar II is the presence of at least one hypomanic episode and one major depressive episode, without a full manic episode.
- The current symptoms of increased energy and decreased need for sleep for 5 days, along with a significant change in behavior (spending paycheck on a "secret project"), indicate a level of impairment consistent with hypomania, rather than a full-blown mania as the thought process is described as linear.
*Major depressive disorder*
- While the patient has a history of depressive episodes, the current presentation with **elevated mood, increased energy, and decreased need for sleep** is inconsistent with a unipolar depressive episode.
- Major depressive disorder does not involve periods of elevated or irritable mood or increased activity.
*Bipolar I disorder*
- Bipolar I disorder requires the occurrence of at least one **manic episode**. While the patient's current symptoms are suggestive of a mood elevation, they do not meet the criteria for full mania, which typically involves severe impairment, psychotic features, or hospitalization.
- The patient's speech is pressured but her thought process is described as **linear**, which is less typical for a full manic episode where **flight of ideas** or **tangential/disorganized thinking** might be present.
*Schizoaffective disorder*
- Schizoaffective disorder involves a period of uninterrupted illness during which there is a **major mood episode (depressive or manic) concurrent with symptoms of schizophrenia**, such as delusions or hallucinations.
- The patient's symptoms are primarily mood-related, and there is no mention of psychotic symptoms independent of the mood disturbance.
*Substance abuse*
- Although the patient used cocaine once in high school, there is no evidence of recent substance use that would explain the current symptoms. The symptoms are sustained over days and include a history of recurrent mood disturbances.
- While the patient received steroid treatment 2 months ago (which can precipitate mood episodes), the timing and clinical presentation are more consistent with a primary mood disorder rather than a substance/medication-induced disorder.
Comorbidities with mood disorders US Medical PG Question 2: A 29-year-old woman is hospitalized due to depression and suicidal ideation. She has a 5-year history of chaotic relationships that last only a few short weeks or months. Each relationship has left her feeling abandoned, empty, and extremely upset. During these periods, the patient confesses to shopping and making big purchases on impulse. She says she gets bored easily and moves on to the next adventure. The patient denies any changes in appetite, energy level, or concentration. On examination, multiple linear lacerations of varying phases of healing were noted on her forearms and trunk. Following consultation, she praises physicians to be ‘the best people on the planet’, but when the nurse came in to take her blood, she furiously stated that ‘all nurses are incompetent and cruel’. Which of the following is the most likely diagnosis?
- A. Borderline personality disorder (Correct Answer)
- B. Histrionic personality disorder
- C. Major depressive disorder (MDD)
- D. Bipolar I disorder
- E. Factitious disorder
Comorbidities with mood disorders Explanation: ***Borderline personality disorder***
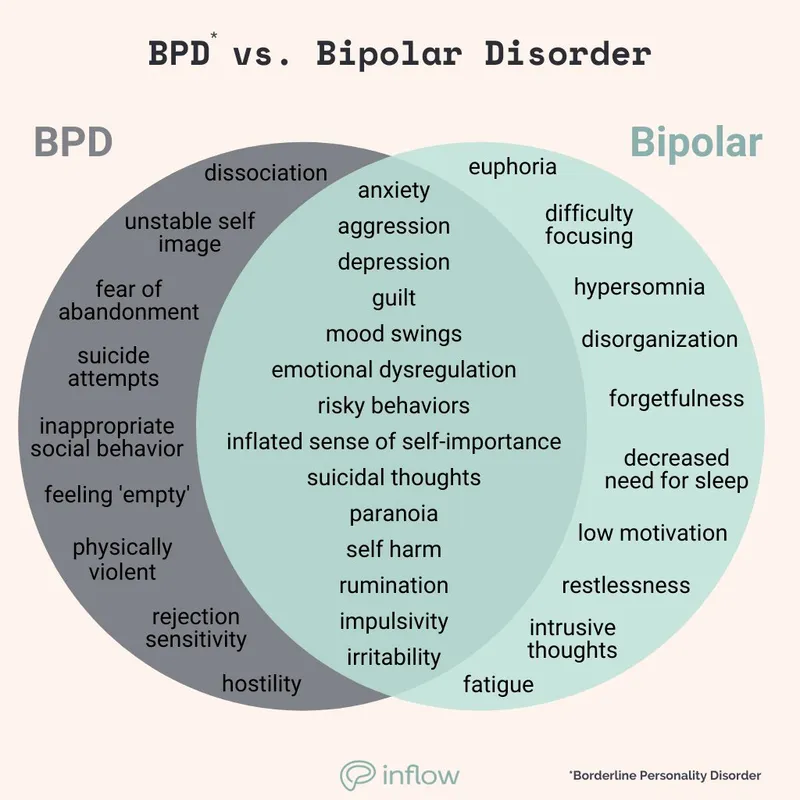
- This condition is characterized by a pervasive pattern of **instability in interpersonal relationships**, **self-image**, and **affects**, along with marked impulsivity, as evidenced by chaotic relationships, feelings of abandonment, and impulsive shopping.
- The patient's rapid shift from idealizing physicians to devaluing nurses (the "best people" to "incompetent and cruel") is characteristic of **splitting**, a common defense mechanism in borderline personality disorder, and the self-inflicted lacerations indicate **self-harm**, another hallmark feature.
*Histrionic personality disorder*
- Characterized by **excessive emotionality** and **attention-seeking behavior**, often through dramatic and sexually provocative means.
- While there may be some superficial overlap in relationship instability, the primary symptoms of splitting, impulsivity (shopping), and self-harm are less prominent here than in borderline personality disorder.
*Major depressive disorder (MDD)*
- While the patient exhibits **depression and suicidal ideation**, MDD typically involves core symptoms like persistent sadness, anhedonia, and changes in appetite, sleep, and energy, which the patient denies ("denies any changes in appetite, energy level, or concentration").
- The long-standing pattern of chaotic relationships, impulsivity, and splitting points away from MDD as the primary diagnosis, suggesting a more pervasive personality difficulty.
*Bipolar I disorder*
- This disorder is characterized by distinct periods of **mania or hypomania** alternating with depressive episodes.
- While impulsivity can be seen in hypomanic/manic states, the patient's symptoms are described as persistent emotional instability and chaotic relationships present for five years, rather than episodic changes in mood and energy, and she denies changes in appetite or energy.
*Factitious disorder*
- Involves **falsification of physical or psychological signs or symptoms**, or induction of injury or disease, associated with identified deception, to assume the sick role.
- Although the patient has self-inflicted lacerations, this behavior is more consistent with **self-harm** seen in borderline personality disorder as a coping mechanism for emotional distress, rather than a deliberate attempt to deceive medical professionals for secondary gain.
Comorbidities with mood disorders US Medical PG Question 3: A 35-year-old man with no past medical history presents to his primary care physician with complaints of fatigue. He states that his life has been hectic lately and that everything seems to be falling apart. He is scared that he will lose his job, that his wife will leave him, and that his children will not be able to afford to go to college. His worries are severe enough that they have begun to interfere with his daily activities. His wife is also present and states that he has a very secure job and that they are well off financially. She says that he has always worried about something since she met him years ago. What medication would benefit this patient long term?
- A. Risperidone
- B. Escitalopram (Correct Answer)
- C. Lithium
- D. No treatment recommended
- E. Diazepam
Comorbidities with mood disorders Explanation: ***Escitalopram***
- The patient exhibits symptoms consistent with **Generalized Anxiety Disorder (GAD)**, characterized by excessive, uncontrollable worry about multiple events or activities. **SSRIs like escitalopram** are first-line agents for long-term treatment of GAD.
- The patient's long-standing pattern of worry, despite a secure job and financial stability, and his wife's observation that he "has always worried about something," further support a diagnosis of GAD, for which escitalopram provides effective long-term symptom management.
*Risperidone*
- **Risperidone** is an **antipsychotic medication** primarily used for conditions like schizophrenia, bipolar disorder, and agitation.
- It is not indicated as a first-line or long-term treatment for Generalized Anxiety Disorder and carries a higher risk of side effects compared to SSRIs.
*Lithium*
- **Lithium** is a **mood stabilizer** primarily used in the management of bipolar disorder.
- This patient's symptoms are indicative of an anxiety disorder, not a mood disorder like bipolar disorder, making lithium an inappropriate choice.
*No treatment recommended*
- The patient's worries are severe enough to **interfere with his daily activities**, indicating a significant functional impairment.
- Therefore, treatment is warranted to alleviate symptoms and improve his quality of life.
*Diazepam*
- **Diazepam** is a **benzodiazepine**, effective for acute anxiety relief due to its rapid onset of action.
- However, it is generally **not recommended for long-term management** due to the risk of dependence, tolerance, and withdrawal symptoms.
Comorbidities with mood disorders US Medical PG Question 4: A 55-year-old man with a history of myocardial infarction 3 months ago presents with feelings of depression. He says that he has become detached from his friends and family and has daily feelings of hopelessness. He says he has started to avoid strenuous activities and is no longer going to his favorite bar where he used to spend a lot of time drinking with his buddies. The patient says these symptoms have been ongoing for the past 6 weeks, and his wife is starting to worry about his behavior. He notes that he continues to have nightmares that he is having another heart attack. He says he is even more jumpy than he used to be, and he startles very easily. Which of the following is the most likely diagnosis in this patient?
- A. Major depressive disorder
- B. Post-traumatic stress disorder (Correct Answer)
- C. Acute stress disorder
- D. Alcohol withdrawal
- E. Midlife crisis
Comorbidities with mood disorders Explanation: ***Post-traumatic stress disorder***
- The patient's symptoms, including **nightmares** about another heart attack, **hypervigilance** (being jumpy and easily startled), **avoidance behaviors** (strenuous activities, bar), **detachment**, and feelings of **hopelessness**, are characteristic of **PTSD** following a traumatic event like a myocardial infarction.
- The symptoms have persisted for **6 weeks**, exceeding the 1-month duration required for a PTSD diagnosis.
*Major depressive disorder*
- While feelings of **hopelessness** and **detachment** are present, the pervasive **recurrent nightmares**, **hypervigilance**, and **avoidance specifically related to the traumatic event** (MI) point more strongly to PTSD.
- A diagnosis of MDD would not fully encompass the trauma-specific symptoms described.
*Acute stress disorder*
- This diagnosis is considered when symptoms similar to PTSD (intrusion, negative mood, dissociation, avoidance, arousal) occur within **3 days to 1 month** after a traumatic event.
- Since the patient's symptoms have been ongoing for **6 weeks**, exceeding the 1-month timeframe, acute stress disorder is ruled out.
*Alcohol withdrawal*
- Symptoms of alcohol withdrawal typically include **tremors, hallucinations, seizures, and delirium**, often developing rapidly after a reduction in alcohol intake.
- The patient's symptoms of **nightmares related to his MI**, **hypervigilance**, and emotional detachment are not characteristic of alcohol withdrawal.
*Midlife crisis*
- This is a non-clinical term describing a period of **emotional turmoil and self-doubt** that may occur in middle age, often involving questioning life choices and goals.
- While the patient is in midlife, his specific symptom constellation, particularly the trauma-related nightmares and hypervigilance, aligns with a diagnosable mental health condition rather than a general life transition.
Comorbidities with mood disorders US Medical PG Question 5: A mental health volunteer is interviewing locals as part of a community outreach program. A 46-year-old man discloses that he has felt sad for as long as he can remember. He feels as though his life is cursed and if something terrible can happen to him, it usually will. He has difficulty making decisions and feels hopeless. He also feels that he has had worsening suicidal ideations, guilt from past problems, decreased energy, and poor concentration over the past 2 weeks. He is otherwise getting enough sleep and able to hold a job. Which of the following statement best describes this patient's condition?
- A. The patient may have symptoms of mania or psychosis.
- B. The patient is likely to show anhedonia.
- C. The patient likely has paranoid personality disorder.
- D. The patient has double depression. (Correct Answer)
- E. The patient should be started on an SSRI.
Comorbidities with mood disorders Explanation: ***The patient has double depression.***
- The patient describes **chronic low-grade depressive symptoms** ("felt sad for as long as he can remember," "life is cursed," "difficulty making decisions," "hopeless") consistent with **persistent depressive disorder (dysthymia)**, which requires at least 2 years of symptoms.
- The recent worsening of symptoms over the past two weeks, including "worsening suicidal ideations, guilt from past problems, decreased energy, and poor concentration," indicates an additional **major depressive episode (MDE) superimposed on dysthymia**, a condition known as **double depression**.
- This patient currently meets criteria for both conditions simultaneously, not just at risk for developing them.
*The patient may have symptoms of mania or psychosis.*
- There are no symptoms mentioned that suggest **mania**, such as elevated mood, increased energy, decreased need for sleep, grandiosity, or racing thoughts.
- While suicidal ideation is present, there is no evidence of **psychotic features** like hallucinations or delusions.
*The patient is likely to show anhedonia.*
- **Anhedonia** (inability to feel pleasure) is a common symptom of depression and may well be present in this patient.
- However, the patient's presentation specifically highlights the pattern of **chronic dysthymia with a superimposed major depressive episode**, making **double depression** a more precise, comprehensive, and diagnostically specific description of his current condition.
- While anhedonia might be present, it is a symptom rather than a diagnostic formulation.
*The patient likely has paranoid personality disorder.*
- **Paranoid personality disorder** is characterized by pervasive distrust and suspicion of others, interpreting their motives as malevolent, without sufficient basis.
- The patient's feelings of being "cursed" and that "something terrible can happen" reflect **depressive pessimism and negative cognitive distortions**, not paranoid ideation about others' intentions.
- This is consistent with the hopelessness seen in depression.
*The patient should be started on an SSRI.*
- While an **SSRI (selective serotonin reuptake inhibitor)** combined with psychotherapy would likely be appropriate treatment for double depression, making a specific treatment recommendation is premature without comprehensive clinical assessment.
- The question asks for the **best statement describing the patient's condition** (diagnosis), not for treatment recommendations.
Comorbidities with mood disorders US Medical PG Question 6: A 24-year-old male comes into the psychiatric clinic complaining of consistent sadness. He endorses feelings of worthlessness, anxiety, and anhedonia for the past couple months but denies feeling suicidal. He further denies any past episodes of feeling overly energetic with racing thoughts. Confident of the diagnosis, you recommend frequent talk therapy along with a long-term prescription of a known first-line medication for this disorder. What is the drug and what are some of the most frequently encountered side effects?
- A. Selective serotonin reuptake inhibitor; hypomania, suicidal thoughts
- B. Tricyclic antidepressants; hypomania, suicidal thoughts
- C. Selective serotonin reuptake inhibitor; anorgasmia, insomnia (Correct Answer)
- D. Monoamine oxidase inhibitors; Orthostatic hypotension, weight gain
- E. Tricyclic antidepressants; Orthostatic hypotension, anticholinergic effects
Comorbidities with mood disorders Explanation: ***Selective serotonin reuptake inhibitor; anorgasmia, insomnia***
- The patient presents with classic symptoms of **major depressive disorder**, including persistent sadness, worthlessness, anxiety, and anhedonia, without any history of manic or hypomanic episodes. **SSRIs** are considered first-line pharmacotherapy for this condition.
- Common side effects of SSRIs include **sexual dysfunction** (e.g., anorgasmia, decreased libido) and **insomnia** or agitation, especially during the initial weeks of treatment.
*Selective serotonin reuptake inhibitor; hypomania, suicidal thoughts*
- While SSRIs are the correct drug class, **hypomania** is not a frequent side effect in patients without bipolar disorder. For patients with bipolar disorder, antidepressant monotherapy can induce hypomania or mania, but this patient denies such episodes.
- **Suicidal thoughts** can occur, particularly in young adults, during the initial phase of antidepressant treatment, but it is less common to frame it as a *frequently encountered side effect* in the general population compared to sexual dysfunction or sleep disturbances.
*Tricyclic antidepressants; hypomania, suicidal thoughts*
- **Tricyclic antidepressants (TCAs)** are generally not first-line due to their less favorable side effect profile compared to SSRIs, including significant anticholinergic effects and cardiovascular risks.
- As with SSRIs, **hypomania** is not a typical frequent side effect in unipolar depression, and while **suicidal thoughts** are a concern with antidepressants, TCAs carry a higher risk of lethality in overdose, making them less preferred initially.
*Monoamine oxidase inhibitors; Orthostatic hypotension, weight gain*
- **Monoamine oxidase inhibitors (MAOIs)** are effective but are typically reserved for **refractory depression** due to their significant drug and food interactions (e.g., tyramine-induced hypertensive crisis).
- While **orthostatic hypotension** and **weight gain** are known side effects of MAOIs, this class is not considered a first-line treatment for major depressive disorder.
*Tricyclic antidepressants; Orthostatic hypotension, anticholinergic effects*
- **TCAs** are indeed associated with side effects such as **orthostatic hypotension** and prominent **anticholinergic effects** (e.g., dry mouth, constipation, blurred vision, urinary retention).
- However, because of these more burdensome side effects and higher toxicity in overdose, TCAs are not generally considered the first-line medication choice, especially when SSRIs are available and safer.
Comorbidities with mood disorders US Medical PG Question 7: A 45-year-old man is brought to the physician by his wife because of difficulty sleeping and poor appetite for the past 4 weeks. During this period, he also has had persistent sadness and difficulty concentrating on tasks, because of which he has been reprimanded at work for poor performance. Over the past 3 years, he has often had such phases, with a maximum symptom-free gap of one month between each of them. His behavior is causing a strain in his relationships with his wife and children. His mother died 4 months ago from breast cancer. Physical examination shows no abnormalities. Mental status examination shows a depressed mood and constricted affect. What is the most likely diagnosis in this patient?
- A. Persistent complex bereavement disorder
- B. Persistent depressive disorder
- C. Major depressive disorder (Correct Answer)
- D. Bipolar affective disorder
- E. Adjustment disorder with depressed mood
Comorbidities with mood disorders Explanation: ***Major depressive disorder***
- The patient presents with **recurrent depressive episodes** over a 3-year period, with the current episode lasting 4 weeks and including multiple depressive symptoms (insomnia, poor appetite, persistent sadness, difficulty concentrating).
- The key feature is the **episodic pattern** with symptom-free intervals (maximum 1 month between episodes), indicating **recurrent major depressive disorder** rather than chronic continuous depression.
- Each episode meets criteria for MDD: at least 2 weeks of depressive symptoms causing significant functional impairment (reprimanded at work, strained relationships).
- The recurrent nature with clear remission periods between episodes distinguishes this from persistent depressive disorder.
*Persistent depressive disorder*
- Requires **chronic depressed mood** present for most of the day, more days than not, for **at least 2 years** in adults, with symptom-free periods lasting **no longer than 2 months**.
- This patient has a **recurrent episodic pattern** with distinct phases separated by symptom-free periods (up to 1 month), not the continuous or near-continuous symptoms characteristic of persistent depressive disorder (dysthymia).
- The presentation describes discrete episodes of depression with remissions between them, which is inconsistent with the persistent/chronic nature required for this diagnosis.
*Persistent complex bereavement disorder*
- This disorder involves **persistent yearning** for the deceased, intense sorrow, emotional pain, and preoccupation with the deceased, along with significant functional impairment, lasting for more than 12 months after the death.
- While the patient's mother died 4 months ago, his depressive symptoms began **3 years ago** (predating the death), and the presentation lacks grief-specific features such as yearning for or preoccupation with the deceased.
- The **3-year history of recurrent depressive phases** indicates a primary mood disorder rather than a bereavement-related condition.
*Bipolar affective disorder*
- Characterized by the presence of at least one **manic or hypomanic episode**, which involves abnormally and persistently elevated, expansive, or irritable mood with increased activity or energy.
- The patient's presentation describes **only recurrent depressive episodes** without any mention of manic or hypomanic symptoms such as grandiosity, decreased need for sleep, pressured speech, racing thoughts, or reckless behavior.
- Absence of any mood elevation episodes rules out bipolar disorder.
*Adjustment disorder with depressed mood*
- Involves emotional or behavioral symptoms developing within **3 months** of an identifiable stressor, with significant distress or functional impairment.
- This diagnosis typically resolves within **6 months** after the stressor or its consequences have terminated.
- The patient's **3-year history** of recurrent depressive episodes far exceeds this time frame and predates his mother's recent death, indicating a primary mood disorder rather than a stress-related adjustment reaction.
Comorbidities with mood disorders US Medical PG Question 8: A 24-year-old woman presents to her primary care physician for a wellness exam. She currently has no acute concerns but has been feeling hopeless, has a poor appetite, difficulty with concentration, and trouble with sleep. She says that she has poor self-esteem and that her symptoms have been occurring for the past 3 years. She has had moments where she felt better, but it lasted a few weeks out of the year. She currently lives alone and does not pursue romantic relationships because she feels she is not attractive. She has a past medical history of asthma. Her mother is alive and healthy. Her father committed suicide and suffered from major depressive disorder. On physical exam, the patient has a gloomy demeanor and appears restless and anxious. Which of the following is the most likely diagnosis?
- A. Major depressive disorder
- B. Cyclothymia
- C. Persistent depressive disorder (Correct Answer)
- D. Seasonal affective disorder
- E. Disruptive mood dysregulation disorder
Comorbidities with mood disorders Explanation: ***Persistent depressive disorder***
- The patient exhibits chronic symptoms of depression (poor appetite, poor self-esteem, difficulty with concentration, trouble with sleep, hopelessness) lasting for at least **2 years**, with symptom-free periods lasting no more than **2 months**.
- Her long-standing symptoms (3 years) and the intermittent improvement, but never full resolution for extended periods, are characteristic of **persistent depressive disorder** (formerly dysthymia).
*Major depressive disorder*
- While the patient has many symptoms of depression, **major depressive disorder** is characterized by distinct episodes of at least 2 weeks, with significant functional impairment. The chronic, fluctuating course over 3 years is less typical.
- The presence of depressive symptoms for 3 years, with only brief periods of improvement, points away from episodic major depressive disorder alone and more towards a chronic form.
*Cyclothymia*
- **Cyclothymia** involves numerous periods of hypomanic symptoms and numerous periods of depressive symptoms for at least 2 years, with periods of stability lasting no more than 2 months. The patient describes only depressive symptoms, not hypomanic episodes.
- There is no mention of elevated mood, increased energy, or decreased need for sleep, which are characteristic of **hypomanic episodes** in cyclothymia.
*Seasonal affective disorder*
- **Seasonal affective disorder** is a type of depressive disorder that occurs during a specific season (most commonly winter) and resolves during other seasons; the patient's symptoms are year-round and chronic.
- The patient's symptoms are not described as tied to a particular season, making this diagnosis less likely.
*Disruptive mood dysregulation disorder*
- Predominantly diagnosed in **children and adolescents**, this disorder is characterized by severe recurrent temper outbursts and persistently irritable or angry mood between outbursts.
- The patient's age (24 years old) and the absence of temper outbursts make this diagnosis inappropriate.
Comorbidities with mood disorders US Medical PG Question 9: A 29-year-old man comes to the physician with his wife because she has noticed a change in his behavior over the past 2 weeks. His wife reports that he is very distracted and irritable. His colleagues have voiced concerns that he has not been turning up for work regularly and behaves erratically when he does. Previously, her husband had been a reliable and reasonable person. The patient says that he feels “fantastic”; he only needs 4 hours of sleep each night and wakes up cheerful and full of energy each morning. He thinks that his wife is overreacting. The patient has been healthy except for a major depressive episode 5 years ago that was treated with paroxetine. He currently takes no medications. His pulse is 98/min, respirations are 12/min, and blood pressure is 128/62 mm Hg. Mental status examination shows frenzied speech and a flight of ideas. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Advanced paternal age
- B. Genetic predisposition (Correct Answer)
- C. Higher socioeconomic class
- D. Maternal obstetric complications
- E. Being married
Comorbidities with mood disorders Explanation: ***Genetic predisposition***
- A strong **genetic predisposition** is a primary predisposing factor for bipolar disorder, as evidenced by a significantly higher concordance rate in monozygotic twins compared to dizygotic twins or the general population.
- The patient's presentation with **manic symptoms** (decreased need for sleep, euphoria, irritability, frenzied speech, flight of ideas, erratic behavior) following a history of a **major depressive episode** is highly suggestive of **bipolar I disorder**.
*Advanced paternal age*
- While advanced paternal age has been associated with an increased risk of some neurodevelopmental disorders like **schizophrenia** and **autism spectrum disorder**, its link to bipolar disorder is less robust and not considered the strongest predisposing factor.
- The primary risk factor for bipolar disorder involves heritability rather than specific parental age.
*Higher socioeconomic class*
- There is **no consistent evidence** to suggest that higher socioeconomic class is a predisposing factor for bipolar disorder.
- Bipolar disorder affects individuals across all socioeconomic levels.
*Maternal obstetric complications*
- Maternal obstetric complications, such as **prenatal infections** or **hypoxia**, have been implicated in the development of certain psychiatric disorders, particularly **schizophrenia**.
- However, for bipolar disorder, genetic factors play a far more significant and direct role than obstetric complications.
*Being married*
- **Marital status** does not serve as a predisposing factor for the development of bipolar disorder.
- While relationship challenges can be a consequence or stressor for individuals with bipolar disorder, marriage itself is not a cause.
Comorbidities with mood disorders US Medical PG Question 10: A 28-year-old woman presents with depressed mood lasting for most days of the week for the past month. She also mentions that she has lost her appetite for the past 3 weeks. She adds that her job performance has significantly deteriorated because of these symptoms, and she feels like she will have to quit her job soon. Upon asking about her hobbies, she says that she used to enjoy dancing and music but does not have any desire to do them anymore. The patient’s husband says that she has had many sleepless nights last month. The patient denies any history of smoking, alcohol intake, or use of illicit substances. No significant past medical history. Physical examination is unremarkable. Routine laboratory tests are all within normal limits. Which of the following clinical features must be present, in addition to this patient’s current symptoms, to confirm the diagnosis of a major depressive episode?
- A. Intense fear of losing control
- B. Lack of concentration (Correct Answer)
- C. Weight loss
- D. Anterograde amnesia
- E. Nightmares
Comorbidities with mood disorders Explanation: ***Lack of concentration***
- The diagnostic criteria for a **major depressive episode** (DSM-5) require at least **5 out of 9 cardinal symptoms** present for at least 2 weeks, with at least one being either **depressed mood** or **anhedonia**.
- This patient currently has **4 symptoms**: (1) depressed mood, (2) anhedonia (loss of interest in dancing/music), (3) appetite disturbance (loss of appetite), and (4) sleep disturbance (insomnia).
- To meet diagnostic criteria, she needs **one more symptom** from the remaining options: fatigue, feelings of worthlessness/guilt, **diminished ability to concentrate or indecisiveness**, psychomotor changes, or suicidal ideation.
- **Lack of concentration** is one of the DSM-5 diagnostic criteria and would bring her total to 5 symptoms, confirming the diagnosis.
*Intense fear of losing control*
- This symptom is characteristic of **panic disorder** or anxiety disorders, where individuals experience sudden, intense episodes of fear with accompanying physical and cognitive symptoms.
- While anxiety can co-occur with depression, intense fear of losing control is **not a DSM-5 diagnostic criterion** for major depressive episode.
*Weight loss*
- The patient already has **loss of appetite**, which satisfies the weight/appetite criterion for major depressive episode.
- **Weight loss and appetite changes are part of the same diagnostic criterion**, not separate ones. Therefore, weight loss would not add an additional criterion to reach the required 5 symptoms.
- While clinically significant weight loss can occur in depression, it would not provide the "additional" criterion needed in this case.
*Anterograde amnesia*
- **Anterograde amnesia** (inability to form new memories) is associated with neurological conditions such as **hippocampal damage**, **Korsakoff syndrome**, or **traumatic brain injury**.
- It is **not a DSM-5 diagnostic criterion** for major depressive episode, though some cognitive impairment (concentration difficulties) may occur.
*Nightmares*
- The patient already has **insomnia** (sleep disturbance), which is one of the DSM-5 diagnostic criteria.
- While nightmares may occur in depression, they are not a separate diagnostic criterion and would not add to the symptom count since sleep disturbance is already present.
More Comorbidities with mood disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.