Child and adolescent mood disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Child and adolescent mood disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Child and adolescent mood disorders US Medical PG Question 1: A previously healthy 13-year-old girl is brought to the physician by her mother because of a change in behavior. The mother reports that over the past 6 months, her daughter has had frequent mood swings. Sometimes, she is irritable for several days and loses her temper easily. In between these episodes, she behaves “normal,” spends time with her friends, and participates in gymnastics training twice a week. The mother has also noticed that her daughter needs more time than usual to get ready for school. Sometimes, she puts on excessive make-up. One month ago, her teacher had informed the parents that their daughter had skipped school and was seen at the local mall with one of her classmates instead. The patient reports that she often feels tired, especially when she has to wake up early for school. On the weekends, she sleeps until 1 pm. Menses have occurred at 15- to 45-day intervals since menarche at the age of 12 years; they are not associated with abdominal discomfort or functional impairment. Physical examination shows no abnormalities. Which of the following is the most likely explanation for the patient's behavior?
- A. Major depressive disorder
- B. Premenstrual syndrome
- C. Borderline personality disorder
- D. Normal behavior (Correct Answer)
- E. Bipolar disorder
Child and adolescent mood disorders Explanation: ***Normal behavior***
* The patient's behavior, including **mood swings**, irritability, increased sleep, and occasional boundary-testing (skipping school), is consistent with typical **adolescent development** and the challenges of this developmental stage.
* The absence of significant functional impairment, her continued engagement in activities like gymnastics, and the intermittent nature of the symptoms suggest that her behavior falls within the **normal range of adolescent growth and exploration**.
*Major depressive disorder*
* **Major depressive disorder** would typically involve more persistent and pervasive symptoms of **depressed mood** or **anhedonia** (loss of interest or pleasure) for at least two weeks, along with other symptoms like significant weight changes, insomnia/hypersomnia, psychomotor agitation/retardation, fatigue, feelings of worthlessness/guilt, difficulty concentrating, or recurrent thoughts of death.
* While she experiences tiredness and increased sleep, her ability to engage in gymnastics and spend time with friends, along with periods of "normal" behavior, does not align with the diagnostic criteria for **major depressive disorder**, which implies more constant functional impairment.
*Premenstrual syndrome*
* **Premenstrual syndrome (PMS)** symptoms are directly linked to the **luteal phase** of the menstrual cycle, consistently resolving with menstruation or shortly thereafter.
* The patient's mood swings and other behavioral changes are reported over a 6-month period and are not explicitly tied to her 15- to 45-day menstrual cycle, making **PMS** less likely.
*Borderline personality disorder*
* **Borderline personality disorder** is characterized by a pervasive pattern of **instability of interpersonal relationships**, self-image, affects, and marked impulsivity, often including features like frantic efforts to avoid abandonment, unstable self-image or sense of self, impulsivity in at least two areas that are potentially self-damaging, recurrent suicidal behavior or self-mutilation, affective instability, chronic feelings of emptiness, intense anger, and transient stress-related paranoid ideation or severe dissociative symptoms.
* While mood swings are present, the overall clinical picture does not align with the severe and persistent functional impairment and specific diagnostic criteria for **borderline personality disorder**, especially in adolescence where such a diagnosis is made with caution.
*Bipolar disorder*
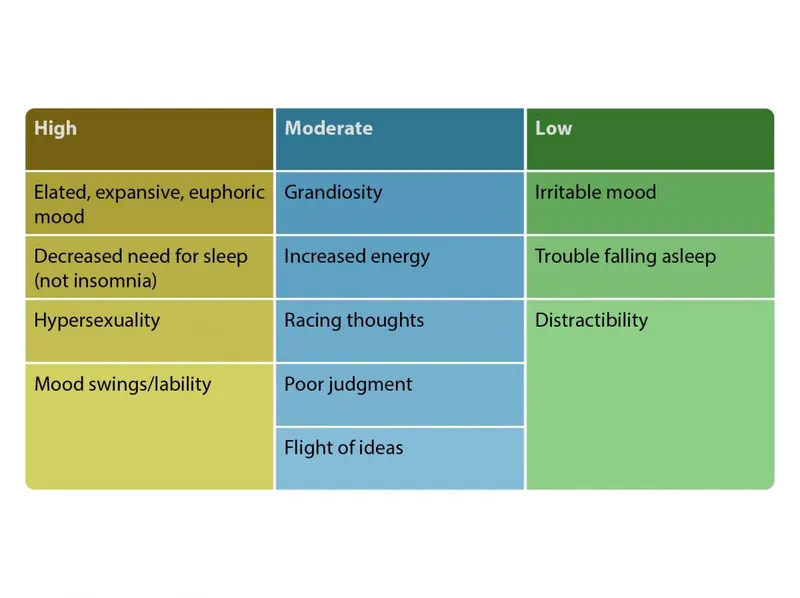
* **Bipolar disorder** involves distinct periods of elevated, expansive, or irritable mood (manic or hypomanic episodes) alternating with depressive episodes.
* While the patient experiences mood swings and irritability, the description lacks the sustained and severe euphoric, expansive, or irritable mood, increased energy/activity, decreased need for sleep (rather than increased), and other classic symptoms (e.g., grandiosity, flight of ideas, risky behaviors) that define a **manic** or **hypomanic episode**, making **bipolar disorder** an unlikely diagnosis.
Child and adolescent mood disorders US Medical PG Question 2: A 45-year-old man is brought to the physician by his wife for the evaluation of abnormal sleep patterns that began 10 days ago. She reports that he has only been sleeping 2–3 hours nightly during this time and has been jogging for long periods of the night on the treadmill. The patient has also been excessively talkative and has missed work on several occasions to write emails to his friends and relatives to convince them to invest in a new business idea that he has had. He has chronic kidney disease requiring hemodialysis, but he has refused to take his medications because he believes that he is cured. Eight months ago, he had a 3-week long period of persistent sadness and was diagnosed with major depressive disorder. Mental status examination shows psychomotor agitation and pressured speech. Treatment of this patient's condition should include which of the following drugs?
- A. Triazolam
- B. Valproate (Correct Answer)
- C. Mirtazapine
- D. Fluoxetine
- E. Bupropion
Child and adolescent mood disorders Explanation: ***Valproate***
- This patient presents with classic features of a **manic episode** (decreased need for sleep, psychomotor agitation, pressured speech, grandiosity, increased goal-directed activity, impaired judgment) occurring after a prior depressive episode, indicating **bipolar I disorder**.
- **Mood stabilizers** are first-line treatment for acute mania. While **lithium** is traditionally considered the gold standard, this patient has **chronic kidney disease requiring hemodialysis**, making lithium relatively **contraindicated** due to its renal excretion and narrow therapeutic index.
- **Valproate** is an excellent alternative mood stabilizer for acute mania and maintenance therapy in bipolar disorder, and it is **hepatically metabolized**, making it safer in patients with **renal impairment**.
- Other options include atypical antipsychotics (e.g., olanzapine, quetiapine, aripiprazole), but valproate is the appropriate mood stabilizer choice given this clinical context.
*Triazolam*
- **Triazolam** is a short-acting benzodiazepine used for **insomnia**.
- While it may provide symptomatic relief for sleep disturbance, it does **not treat the underlying manic episode** and is not indicated as primary therapy for bipolar mania.
- Benzodiazepines may be used as adjunctive agents for acute agitation but are not definitive treatment.
*Mirtazapine*
- **Mirtazapine** is a tetracyclic antidepressant used for **major depressive disorder**.
- Antidepressant monotherapy in bipolar disorder can **precipitate or worsen manic episodes** and is contraindicated during an acute manic phase.
- If antidepressants are needed for bipolar depression, they should be combined with mood stabilizers.
*Fluoxetine*
- **Fluoxetine** is a selective serotonin reuptake inhibitor (SSRI) antidepressant.
- Like other antidepressants, using fluoxetine as monotherapy in a patient with bipolar disorder can **induce or exacerbate manic episodes**.
- It is inappropriate for treating acute mania.
*Bupropion*
- **Bupropion** is an atypical antidepressant (norepinephrine-dopamine reuptake inhibitor) used for depression and smoking cessation.
- It carries a **higher risk of inducing mania** compared to other antidepressants due to its dopaminergic activity.
- It is not appropriate for acute mania treatment and could worsen the patient's current symptoms.
Child and adolescent mood disorders US Medical PG Question 3: A 32-year-old woman is brought to the physician by her husband, who is concerned about her ability to care for herself. Three weeks ago, she quit her marketing job to start a clothing company. Since then, she has not slept more than 4 hours per night because she has been working on her business plans. She used a significant portion of their savings to fund business trips to Switzerland in order to buy “only the best quality fabrics in the world.” She has not showered and has eaten little during the past 3 days. She has had 2 similar episodes a few years back that required hospitalization and treatment in a psychiatry unit. She has also suffered from periods of depression. She is currently not taking any medications. She appears unkempt and agitated, pacing up and down the room. She speaks very fast without interruption about her business ideas. She has no suicidal ideation or ideas of self-harm. Toxicology screening is negative. Which of the following is the most appropriate pharmacotherapy for the management of this patient?
- A. Clonazepam therapy for one year
- B. Long-term lithium therapy (Correct Answer)
- C. Sertraline therapy for one year
- D. Long-term risperidone therapy
- E. Long-term clozapine therapy
Child and adolescent mood disorders Explanation: ***Long-term lithium therapy***
- This patient presents with classic symptoms of **mania** (decreased need for sleep, grandiosity, compulsive spending, rapid speech) and a history of both manic and depressive episodes, consistent with **bipolar I disorder**.
- **Lithium** is a first-line agent for the **long-term maintenance treatment** of **bipolar I disorder**, particularly effective in preventing both manic and depressive episodes.
*Clonazepam therapy for one year*
- **Clonazepam** is a **benzodiazepine** primarily used for short-term management of acute agitation or severe insomnia, not for long-term mood stabilization in bipolar disorder.
- Long-term use of benzodiazepines carries risks of **tolerance** and **dependence**, making it inappropriate for chronic maintenance treatment.
*Sertraline therapy for one year*
- **Sertraline** is an **antidepressant** (SSRI) that, when used as monotherapy in bipolar disorder, can induce **mania** or **rapid cycling**.
- While periods of depression are mentioned, the current presentation is manic, and mood stabilizers are the priority for long-term management.
*Long-term risperidone therapy*
- **Risperidone** is a **second-generation antipsychotic** effective in treating acute mania and can be used for maintenance in bipolar disorder, often as an adjunct or in patients who cannot tolerate lithium.
- However, for long-term monotherapy in bipolar I disorder, **lithium** is generally considered more effective and is the preferred first-line agent, especially given the history of recurrent episodes.
*Long-term clozapine therapy*
- **Clozapine** is an **atypical antipsychotic** reserved for **treatment-resistant schizophrenia** and **refractory bipolar disorder**, often due to its significant side effect profile, including **agranulocytosis**.
- While it can be effective for severe or refractory cases of bipolar disorder, it is not a first-line long-term treatment given its risks and the availability of safer alternatives.
Child and adolescent mood disorders US Medical PG Question 4: A 29-year-old man comes to the physician with his wife because she has noticed a change in his behavior over the past 2 weeks. His wife reports that he is very distracted and irritable. His colleagues have voiced concerns that he has not been turning up for work regularly and behaves erratically when he does. Previously, her husband had been a reliable and reasonable person. The patient says that he feels “fantastic”; he only needs 4 hours of sleep each night and wakes up cheerful and full of energy each morning. He thinks that his wife is overreacting. The patient has been healthy except for a major depressive episode 5 years ago that was treated with paroxetine. He currently takes no medications. His pulse is 98/min, respirations are 12/min, and blood pressure is 128/62 mm Hg. Mental status examination shows frenzied speech and a flight of ideas. Which of the following is the strongest predisposing factor for this patient's condition?
- A. Advanced paternal age
- B. Genetic predisposition (Correct Answer)
- C. Higher socioeconomic class
- D. Maternal obstetric complications
- E. Being married
Child and adolescent mood disorders Explanation: ***Genetic predisposition***
- A strong **genetic predisposition** is a primary predisposing factor for bipolar disorder, as evidenced by a significantly higher concordance rate in monozygotic twins compared to dizygotic twins or the general population.
- The patient's presentation with **manic symptoms** (decreased need for sleep, euphoria, irritability, frenzied speech, flight of ideas, erratic behavior) following a history of a **major depressive episode** is highly suggestive of **bipolar I disorder**.
*Advanced paternal age*
- While advanced paternal age has been associated with an increased risk of some neurodevelopmental disorders like **schizophrenia** and **autism spectrum disorder**, its link to bipolar disorder is less robust and not considered the strongest predisposing factor.
- The primary risk factor for bipolar disorder involves heritability rather than specific parental age.
*Higher socioeconomic class*
- There is **no consistent evidence** to suggest that higher socioeconomic class is a predisposing factor for bipolar disorder.
- Bipolar disorder affects individuals across all socioeconomic levels.
*Maternal obstetric complications*
- Maternal obstetric complications, such as **prenatal infections** or **hypoxia**, have been implicated in the development of certain psychiatric disorders, particularly **schizophrenia**.
- However, for bipolar disorder, genetic factors play a far more significant and direct role than obstetric complications.
*Being married*
- **Marital status** does not serve as a predisposing factor for the development of bipolar disorder.
- While relationship challenges can be a consequence or stressor for individuals with bipolar disorder, marriage itself is not a cause.
Child and adolescent mood disorders US Medical PG Question 5: An 11-year-old boy’s parents brought him to a psychologist upon referral from the boy’s school teacher. The boy frequently bullies his younger classmates despite having been punished several times for this. His mother also reported that a year prior, she received complaints that the boy shoplifted from local shops in his neighborhood. The boy frequently stays out at night despite strict instructions by his parents to return home by 10 PM. Detailed history reveals that apart from such behavior, he is usually not angry or irritable. Although his abnormal behavior continues despite warnings and punishments, he neither argues with his parents nor teachers and does not display verbal or physical aggression. Which of the following is the most likely diagnosis?
- A. Attention-deficit/hyperactivity disorder, hyperactivity-impulsivity type
- B. Disruptive mood dysregulation disorder
- C. Intermittent explosive disorder
- D. Conduct disorder (Correct Answer)
- E. Oppositional defiant disorder
Child and adolescent mood disorders Explanation: ***Conduct disorder***
- The boy's behaviors, including **bullying**, **shoplifting**, and **violating rules** (staying out past curfew), represent a persistent pattern of behavior that violates the basic rights of others or major age-appropriate societal norms, which are core features of **conduct disorder**.
- The history indicates these behaviors have been ongoing for at least a year and are not just isolated incidents, fulfilling the diagnostic criteria for **duration and pervasiveness**.
*Attention-deficit/hyperactivity disorder, hyperactivity-impulsivity type*
- While ADHD involves **hyperactivity** and **impulsivity**, it does not typically manifest with deliberate violations of others' rights or societal norms like **bullying** and **shoplifting**.
- There is no mention of symptoms such as **difficulty sustaining attention**, **fidgeting**, or **excessive talking** which are characteristic of ADHD.
*Disruptive mood dysregulation disorder*
- This disorder is characterized by **severe recurrent temper outbursts** and persistent **irritable or angry mood** between outbursts.
- The case explicitly states the boy is "not angry or irritable" and "neither argues with his parents nor teachers," ruling out this diagnosis.
*Intermittent explosive disorder*
- This disorder involves recurrent behavioral outbursts representing a failure to control aggressive impulses, often with verbal aggression or physical aggression toward property, animals, or other individuals.
- The boy does not display verbal or physical aggression and is not noted to have anger or irritability, which are central to this diagnosis.
*Oppositional defiant disorder*
- ODD involves a pattern of **angry/irritable mood**, **argumentative/defiant behavior**, or **vindictiveness**.
- While violating rules is present, **bullying** and **shoplifting** (which violate the basic rights of others) are more severe behaviors that go beyond the scope of ODD and are characteristic of conduct disorder.
Child and adolescent mood disorders US Medical PG Question 6: A previously healthy 16-year-old boy is brought to the physician by his parents for evaluation because of extreme irritability, fatigue, and loss of appetite for 3 weeks. Five months ago, his grandfather, whom he was very close to, passed away from chronic lymphocytic leukemia. He used to enjoy playing soccer but quit his soccer team last week. When he comes home from school he goes straight to bed and sleeps for 11–12 hours each night. He previously had good grades, but his teachers report that he has been disrespectful and distracted in class and failed an exam last week. He tried alcohol twice at a party last year and he has never smoked cigarettes. Vital signs are within normal limits. On mental status examination, he avoids making eye contact but cooperates with the exam. His affect is limited and he describes an irritable mood. He is easily distracted and has a difficult time focusing for an extended conversation. Which of the following is the most likely diagnosis?
- A. Attention deficit hyperactivity disorder
- B. Major depressive disorder (Correct Answer)
- C. Persistent depressive disorder
- D. Substance abuse
- E. Adjustment disorder with depressed mood
Child and adolescent mood disorders Explanation: ***Major depressive disorder***
- The patient exhibits classic symptoms of **major depressive disorder**, including **extreme irritability**, fatigue, loss of appetite, anhedonia (quitting soccer), **hypersomnia**, academic decline, and social withdrawal.
- These symptoms have been present for **3 weeks** and represent a significant change from his baseline functioning.
- The severity and duration of symptoms meet **DSM-5 criteria** for a major depressive episode.
*Attention deficit hyperactivity disorder*
- While he shows *distractibility* and *difficulty focusing*, the **sudden onset** of multiple depressive symptoms and a clear change from his previous functioning make ADHD less likely.
- ADHD is characterized by a pervasive pattern of **inattention** and/or **hyperactivity-impulsivity** typically present from childhood, not a recent decline with mood and neurovegetative symptoms.
*Persistent depressive disorder*
- Persistent depressive disorder (dysthymia) requires symptoms that persist for **at least 2 years** (1 year in children/adolescents) and are generally milder.
- This patient's symptoms are both severe and of relatively recent onset (3 weeks), indicative of an **acute** and **major depressive episode** rather than chronic low-grade depression.
*Substance abuse*
- Although adolescents may use substances as coping mechanisms, there is **no evidence** of current substance use, only a history of trying alcohol twice over a year ago.
- The constellation of specific depressive symptoms points away from substance abuse being the **primary diagnosis**.
*Adjustment disorder with depressed mood*
- Adjustment disorder requires symptoms to occur within **3 months** of an identifiable stressor and not meet full criteria for a major depressive episode.
- The grandfather's death occurred **5 months ago**, which is **outside the 3-month window** for adjustment disorder.
- More importantly, this patient's symptoms—including **anhedonia**, **hypersomnia**, and significant functional impairment—are severe enough to meet full criteria for a **major depressive episode**, exceeding the diagnostic threshold for adjustment disorder.
Child and adolescent mood disorders US Medical PG Question 7: A mother brings her 3-year-old son to his pediatrician because he is having tantrums. The boy has no history of serious illness and is on track with developmental milestones. His mother recently returned to work 2 weeks ago. She explains that, since then, her son has had a tantrum roughly every other morning, usually when she is getting him dressed or dropping him off at daycare. He cries loudly for about 5 minutes, saying that he does not want to go to daycare while thrashing his arms and legs. According to the daycare staff, he is well-behaved during the day. In the evenings, he has tantrums about twice per week, typically when he is told he must finish his dinner or that it is time for bed. These tantrums have been occurring for about 6 months. The mother is concerned her son may have a behavioral disorder. Which of the following is the most likely cause of the boy's behavior?
- A. Autism spectrum disorder
- B. Disruptive mood dysregulation disorder
- C. Conduct disorder
- D. Normal development (Correct Answer)
- E. Attention deficit hyperactivity disorder
Child and adolescent mood disorders Explanation: **Normal development**
- **Tantrums** are a normal part of development for 2-5-year-olds as they learn to express their independence and emotions.
- The child's tantrums are situation-specific (daycare, bedtime, dinner), of limited duration (5 minutes), and he is otherwise **well-behaved** at daycare, which aligns with typical developmental behaviors.
*Autism spectrum disorder*
- This disorder involves persistent deficits in **social communication** and interaction, and **restricted, repetitive patterns of behavior**, which are not described in the child's presentation.
- The child is reported to be on track with **developmental milestones** and is only 3 years old, making this diagnosis less likely.
*Disruptive mood dysregulation disorder*
- This diagnosis requires **severe, recurrent temper outbursts** that are grossly out of proportion in intensity or duration to the situation, occurring **3 or more times per week** for at least 12 months.
- The child's tantrums are less frequent than required for this diagnosis and do not meet the duration criteria, affecting children typically over 6 years of age.
*Conduct disorder*
- This disorder involves a repetitive and persistent pattern of behavior in which the **basic rights of others or major age-appropriate societal norms or rules are violated**.
- The child's behavior does not include aggression towards people or animals, destruction of property, deceitfulness, or theft, which are core features of conduct disorder.
*Attention deficit hyperactivity disorder*
- This disorder is characterized by persistent patterns of **inattention** and/or **hyperactivity-impulsivity** that interfere with functioning or development.
- The child's primary issue is tantrums, not problems with attention, focus, or excessive motor activity in various settings.
Child and adolescent mood disorders US Medical PG Question 8: A 24-year-old woman presents to her primary care physician for a wellness exam. She currently has no acute concerns but has been feeling hopeless, has a poor appetite, difficulty with concentration, and trouble with sleep. She says that she has poor self-esteem and that her symptoms have been occurring for the past 3 years. She has had moments where she felt better, but it lasted a few weeks out of the year. She currently lives alone and does not pursue romantic relationships because she feels she is not attractive. She has a past medical history of asthma. Her mother is alive and healthy. Her father committed suicide and suffered from major depressive disorder. On physical exam, the patient has a gloomy demeanor and appears restless and anxious. Which of the following is the most likely diagnosis?
- A. Major depressive disorder
- B. Cyclothymia
- C. Persistent depressive disorder (Correct Answer)
- D. Seasonal affective disorder
- E. Disruptive mood dysregulation disorder
Child and adolescent mood disorders Explanation: ***Persistent depressive disorder***
- The patient exhibits chronic symptoms of depression (poor appetite, poor self-esteem, difficulty with concentration, trouble with sleep, hopelessness) lasting for at least **2 years**, with symptom-free periods lasting no more than **2 months**.
- Her long-standing symptoms (3 years) and the intermittent improvement, but never full resolution for extended periods, are characteristic of **persistent depressive disorder** (formerly dysthymia).
*Major depressive disorder*
- While the patient has many symptoms of depression, **major depressive disorder** is characterized by distinct episodes of at least 2 weeks, with significant functional impairment. The chronic, fluctuating course over 3 years is less typical.
- The presence of depressive symptoms for 3 years, with only brief periods of improvement, points away from episodic major depressive disorder alone and more towards a chronic form.
*Cyclothymia*
- **Cyclothymia** involves numerous periods of hypomanic symptoms and numerous periods of depressive symptoms for at least 2 years, with periods of stability lasting no more than 2 months. The patient describes only depressive symptoms, not hypomanic episodes.
- There is no mention of elevated mood, increased energy, or decreased need for sleep, which are characteristic of **hypomanic episodes** in cyclothymia.
*Seasonal affective disorder*
- **Seasonal affective disorder** is a type of depressive disorder that occurs during a specific season (most commonly winter) and resolves during other seasons; the patient's symptoms are year-round and chronic.
- The patient's symptoms are not described as tied to a particular season, making this diagnosis less likely.
*Disruptive mood dysregulation disorder*
- Predominantly diagnosed in **children and adolescents**, this disorder is characterized by severe recurrent temper outbursts and persistently irritable or angry mood between outbursts.
- The patient's age (24 years old) and the absence of temper outbursts make this diagnosis inappropriate.
Child and adolescent mood disorders US Medical PG Question 9: A 25-year-old woman comes to the physician because of sadness that started 3 weeks after her daughter was born. Her daughter is now 9 months old and usually sleeps through the night, but the patient still has difficulty staying asleep. She has not returned to work since the birth. She is easily distracted from normal daily tasks. She used to enjoy cooking, but only orders delivery or take-out now. She says that she always feels too exhausted to do so and does not feel hungry much anyway. The pregnancy of the patient's child was complicated by gestational diabetes. The child was born at 36-weeks' gestation and has had no medical issues. The patient has no contact with the child's father. She is not sexually active. She does not smoke, drink alcohol, or use illicit drugs. She is 157 cm (5 ft 1 in) tall and weighs 47 kg (105 lb); BMI is 20 kg/m2. Vital signs are within normal limits. She is alert and cooperative but makes little eye contact. Physical examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Adjustment disorder
- B. Major depressive disorder
- C. Normal behavior
- D. Disruptive mood dysregulation disorder
- E. Depression with peripartum-onset (Correct Answer)
Child and adolescent mood disorders Explanation: ***Depression with peripartum-onset***
- The patient exhibits classic symptoms of **major depressive disorder**, including **anhedonia** (loss of enjoyment in cooking), **fatigue**, **insomnia**, and **changes in appetite/weight**, all appearing within 3 weeks post-childbirth and persisting for 9 months.
- According to **DSM-5-TR**, the **peripartum onset specifier** is applied when a major depressive episode begins during pregnancy or **within 4 weeks after delivery**.
- This patient's symptoms began at 3 weeks postpartum, meeting criteria for the peripartum onset specifier, which is clinically important for risk assessment (including infanticide risk) and treatment planning.
- The severity and duration of symptoms (persistent anhedonia, significant fatigue, insomnia despite adequate opportunity for sleep, appetite changes, functional impairment lasting months) clearly meet criteria for a **major depressive episode**.
*Adjustment disorder*
- This diagnosis involves emotional or behavioral symptoms in response to an identifiable stressor that do **not meet criteria for a major depressive episode**.
- The severity, number, and duration of symptoms (anhedonia, significant fatigue, insomnia, appetite changes, functional impairment lasting 9 months) exceed what is seen in adjustment disorder and meet full criteria for **major depressive disorder**.
*Major depressive disorder*
- While this patient's symptoms fully meet criteria for **Major Depressive Disorder (MDD)**, the onset within 4 weeks postpartum requires the addition of the **"with peripartum onset" specifier** per DSM-5-TR.
- Using the peripartum onset specifier is essential for clinical management, as it alerts clinicians to specific risks (including thoughts of harming the infant) and may influence treatment selection (e.g., considerations for breastfeeding-compatible medications).
*Normal behavior*
- The patient's symptoms—including **persistent sadness lasting 9 months**, **anhedonia**, **insomnia despite adequate sleep opportunity**, **significant fatigue**, **appetite loss**, and **inability to return to work**—represent severe functional impairment.
- These symptoms far exceed normal postpartum adjustment or transient "baby blues" (which typically resolve within 2 weeks postpartum) and indicate a serious mood disorder requiring treatment.
*Disruptive mood dysregulation disorder*
- This disorder is diagnosed **only in children and adolescents aged 6-18 years** and is characterized by persistent irritability and frequent, severe temper outbursts disproportionate to the situation.
- It is **not applicable to adults** and does not describe this patient's presentation of persistent depressed mood and neurovegetative symptoms.
Child and adolescent mood disorders US Medical PG Question 10: A 12-year-old boy is brought in by his parents as they are concerned about his behavior. He is constantly arguing with his parents and blatantly defying their every request. In school, he is known for being intentionally tardy and for defying his teachers. Upon further questioning of the patient you learn about some of his recent behaviors such as beginning smoking to bother his parents. You also notice that he is disrespectful towards you. You then learn that he has also gotten into weekly fights with his peers at school with no apparent cause. In addition, last week he was seen hitting one of the local neighborhood cats with a baseball bat trying to kill it. The patient lives at home with his two parents in a pre-World War II house that was recently renovated. Physical exam is unremarkable.
Laboratory values are as follows:
Na: 140 mmol/L
K: 4.5 mmol/L
Cl: 100 mmol/L
Glucose: 80 mg/dL
Ca: 10 mmol/L
Mg: 3 mEq/L
Cr: 0.8 mg/dL
BUN: 10 mg/dL
Serum lead: < .01 µg/dL
Hb: 15 g/dL
Hct: 45%
MCV: 95
Urine toxicology: negative
As the patient leaves the office you notice him stealing all of the candy from the office candy bowl. The patient seems unconcerned about his behavior overall. Which of the following statements is most likely to be true in this patient?
- A. This patient will likely function normally despite continuing to defy authority figures
- B. Environmental exposures are likely causing this patient's behavior
- C. The patient's symptoms could progress to antisocial personality disorder (Correct Answer)
- D. This patient is suffering from antisocial personality disorder and will likely be incarcerated in adulthood
- E. Strong D2 antagonists are first-line pharmacotherapy
Child and adolescent mood disorders Explanation: ***The patient's symptoms could progress to antisocial personality disorder***
- The patient's pattern of **aggression towards people and animals**, **deceitfulness or theft**, and **serious violations of rules** (e.g., truancy, defying authority) are all diagnostic criteria for **conduct disorder**.
- If conduct disorder symptoms persist into adulthood (age 18 or older), it can lead to a diagnosis of **antisocial personality disorder (ASPD)**, as ASPD requires evidence of conduct disorder before age 15.
*This patient will likely function normally despite continuing to defy authority figures*
- The described behaviors go beyond simple defiance; they include **aggression, severe rule violations, and lack of remorse**. These are significant indicators of a **conduct disorder**, which is associated with poor long-term outcomes and functional impairment, not normal functioning.
- Undiagnosed and untreated conduct disorder can lead to **academic difficulties, substance abuse, legal problems, and inability to maintain relationships**, making normal functioning unlikely.
*Environmental exposures are likely causing this patient's behavior*
- While environmental factors can contribute, the **severity and widespread nature** of the behaviors (at home, school, with peers, and animals), coupled with the **lack of remorse and intentional malice**, point more strongly to an underlying psychiatric diagnosis like conduct disorder rather than solely environmental causes.
- The provided lab results rule out common environmental toxins like **lead poisoning**, and the recent house renovation doesn't provide direct evidence of a toxic exposure causing these specific behavioral manifestations.
*This patient is suffering from antisocial personality disorder and will likely be incarcerated in adulthood*
- **Antisocial personality disorder (ASPD)** cannot be diagnosed before age 18. This patient is 12 years old, making ASPD an incorrect diagnosis at this stage, although his current behaviors are consistent with **conduct disorder**, which is a precursor.
- While there is an increased risk of incarceration for individuals with ASPD, stating it as a **definitive outcome** or that he "will likely be incarcerated" is deterministic and not universally true, as interventions can impact outcomes.
*Strong D2 antagonists are first-line pharmacotherapy*
- **First-line treatment for conduct disorder** typically involves **psychosocial interventions**, such as parent management training, cognitive behavioral therapy, and multisystemic therapy.
- While **D2 antagonists** (antipsychotics) may be used in severe cases, particularly for **aggression and impulsivity** when other treatments fail or if there are comorbid conditions, they are not considered **first-line pharmacotherapy** for conduct disorder itself.
More Child and adolescent mood disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.