Mood Disorders

On this page
🧠 The Mood Spectrum: Decoding Emotional Architecture
Mood disorders reshape how patients experience reality itself, turning the brain's emotional thermostat into a source of profound suffering that touches every domain of human function. You'll master the neurobiological underpinnings that drive depression and bipolar disorder, sharpen your diagnostic precision through pattern recognition that distinguishes subtypes, and command evidence-based treatment algorithms that integrate pharmacology, psychotherapy, and systems-level care. This lesson builds your clinical radar to catch what others miss and intervene with confidence when emotional architecture collapses.
📌 Remember: MOOD SPECTRUM - Major depression, Other specified disorders, Organic causes, Dysthymia, Seasonal patterns, Persistent symptoms, Episodic bipolar, Cyclothymia, Treatment-resistant, Recurrent episodes, Unspecified disorders, Mixed features
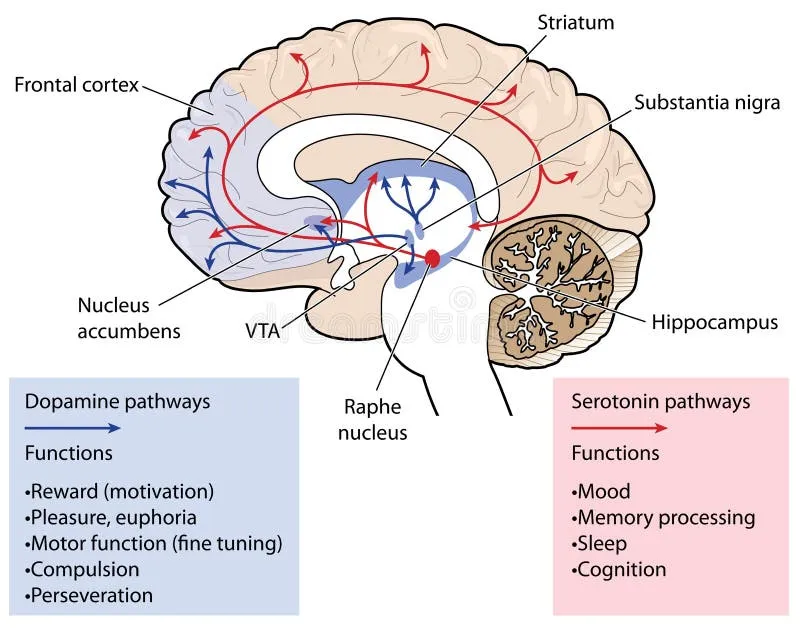
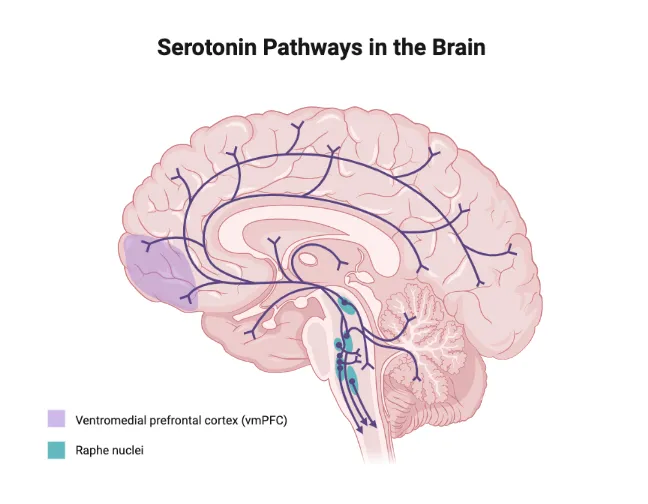
The neurobiological foundation involves three primary neurotransmitter systems: serotonin (5-HT), norepinephrine (NE), and dopamine (DA). Serotonin dysfunction affects 90% of mood disorder cases, while norepinephrine dysregulation contributes to 75% of treatment-resistant depression. The prefrontal cortex, limbic system, and hypothalamic-pituitary-adrenal axis form the core neural networks governing emotional processing.
-
Major Depressive Disorder (MDD)
- Lifetime prevalence: 16.6% in adults
- Female-to-male ratio: 2:1
- Average age of onset: 32 years
- First episode before age 18: 25% of cases
- Recurrence rate: 85% within 15 years
- Treatment response rate: 65-70% with first-line therapy
-
Bipolar Disorder Spectrum
- Bipolar I prevalence: 1.0% globally
- Bipolar II prevalence: 1.1% globally
- Average diagnostic delay: 9.5 years
- Misdiagnosis rate: 69% initially diagnosed as unipolar depression
- Suicide attempt rate: 25-50% lifetime risk
- Functional impairment: 30% experience significant disability
| Disorder Type | Prevalence | Age of Onset | Episode Duration | Recurrence Risk | Treatment Response |
|---|---|---|---|---|---|
| Major Depression | 16.6% | 32 years | 6-12 months | 85% | 65-70% |
| Bipolar I | 1.0% | 18 years | 3-6 months | 90% | 60-80% |
| Bipolar II | 1.1% | 22 years | 2-4 months | 95% | 50-70% |
| Dysthymia | 2.5% | 21 years | 2+ years | 70% | 55-65% |
| Cyclothymia | 0.4% | 16 years | Chronic | 85% | 45-60% |
The diagnostic framework requires understanding five core domains: mood symptoms, neurovegetative changes, cognitive alterations, psychomotor disturbances, and functional impairment. Neurovegetative symptoms include sleep disturbances (90% of depressed patients), appetite changes (75%), and energy loss (85%).
💡 Master This: Mood disorders follow the monoamine hypothesis where decreased serotonin, norepinephrine, and dopamine create depressive symptoms, while excessive dopamine and norepinephrine contribute to manic episodes. Understanding this neurochemical foundation predicts medication selection and treatment response patterns.
Connect these foundational concepts through neurobiological mechanisms to understand how disrupted brain circuits manifest as clinical presentations.
🧠 The Mood Spectrum: Decoding Emotional Architecture
⚡ Neurochemical Command Centers: The Brain's Mood Machinery
📌 Remember: NEUROTRANSMITTER TRIO - Serotonin for mood stability (5-HT), Norepinephrine for energy/attention (NE), Dopamine for motivation/pleasure (DA). Deficiency patterns: Sad mood (5-HT), No energy (NE), Diminished pleasure (DA).
Serotonin System Dysfunction:
- Raphe nuclei contain 90% of brain serotonin neurons
- 5-HT1A receptor downregulation occurs in 85% of depressed patients
- Tryptophan depletion reduces serotonin by 60-80% within 6 hours
- SSRI response correlates with 5-HTTLPR gene polymorphisms in 65% of patients
-
Norepinephrine Circuitry
- Locus coeruleus origin with widespread projections
- Alpha-2 autoreceptors provide negative feedback
- Reuptake transporter (NET) targeted by SNRIs
- Norepinephrine levels decrease 40-60% in depression
- Stress response involves 300% increase in NE release
- Sleep architecture disrupted by NE dysregulation
-
Dopamine Reward Pathways
- Ventral tegmental area (VTA) to nucleus accumbens
- Substantia nigra to striatum for motor function
- Prefrontal cortex projections for executive function
- Anhedonia correlates with 50% reduction in DA activity
- Motivation deficits linked to D2 receptor downregulation
- Psychomotor symptoms reflect nigrostriatal dysfunction
| Neurotransmitter | Primary Function | Deficiency Symptoms | Excess Symptoms | Receptor Subtypes | Half-life |
|---|---|---|---|---|---|
| Serotonin (5-HT) | Mood, sleep, appetite | Depression, anxiety, insomnia | Serotonin syndrome | 14 subtypes | 1-2 hours |
| Norepinephrine | Energy, attention, arousal | Fatigue, concentration loss | Anxiety, agitation | α1, α2, β1, β2 | 2-3 minutes |
| Dopamine | Motivation, reward, movement | Anhedonia, psychomotor slowing | Psychosis, mania | D1-D5 | 1-2 minutes |
| GABA | Inhibition, anxiety control | Anxiety, agitation | Sedation, ataxia | GABA-A, GABA-B | 30-60 minutes |
| Glutamate | Excitation, learning | Cognitive impairment | Excitotoxicity | NMDA, AMPA | 5-10 minutes |
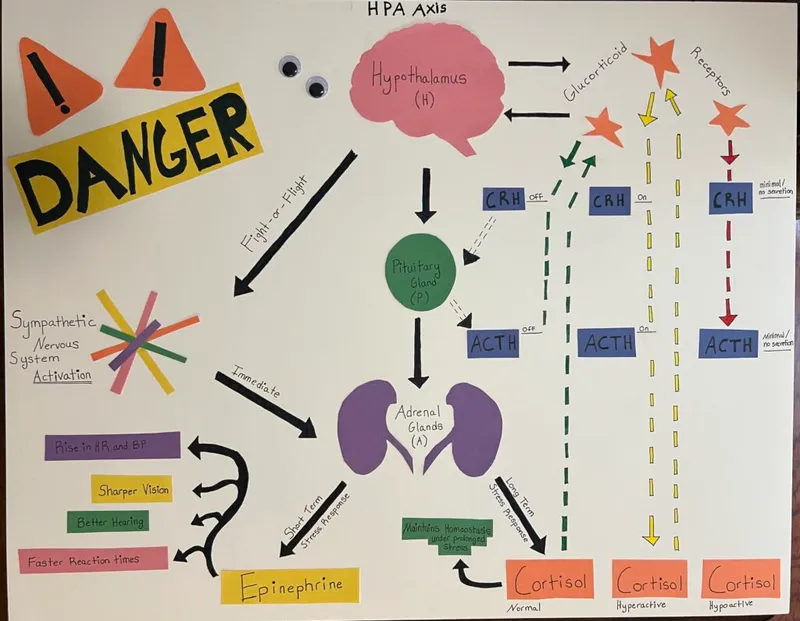
Neural Circuit Integration: The default mode network (DMN) shows hyperactivity in depression, with 25% increased connectivity in the subgenual anterior cingulate cortex. Amygdala hyperreactivity occurs in 90% of mood disorder patients, while prefrontal cortex hypoactivity correlates with executive dysfunction in 75% of cases.
💡 Master This: Mood disorders result from network-level dysfunction rather than single neurotransmitter deficits. The tripartite model involves: (1) limbic hyperactivity creating emotional dysregulation, (2) prefrontal hypoactivity reducing cognitive control, and (3) neurotransmitter imbalance disrupting signal transmission between regions.
Connect these neurochemical foundations through clinical pattern recognition to understand how biochemical disruptions manifest as observable symptoms and treatment targets.
⚡ Neurochemical Command Centers: The Brain's Mood Machinery
🎯 Clinical Pattern Recognition: The Diagnostic Radar System
📌 Remember: DEPRESSION CORE - Depressed mood, Energy loss, Pleasure loss (anhedonia), Restlessness/retardation, Eating changes, Sleep disturbance, Suicidal thoughts, Interest loss, Optimism loss, Neurovegetative symptoms. At least 5 symptoms required for ≥2 weeks.
Major Depressive Episode Recognition:
- Core symptoms (≥1 required): Depressed mood or anhedonia
- Neurovegetative cluster: Sleep, appetite, energy, psychomotor
- Cognitive cluster: Concentration, worthlessness, suicidal ideation
- Severity markers: Functional impairment in ≥2 life domains
-
Manic Episode Identification
- Elevated/irritable mood for ≥7 days (or hospitalization)
- Distractibility, Indiscretion, Grandiosity, Flight of ideas
- Activity increase, Sleep decrease, Talkativeness (DIG FAST mnemonic)
- Hospitalization rate: 75% of first manic episodes
- Psychotic features: 60% of severe mania cases
- Mixed features: 40% include depressive symptoms
-
Hypomanic Episode Criteria
- Same symptoms as mania but ≥4 days duration
- No hospitalization or severe impairment
- Observable change but functional capacity maintained
- Recognition delay: Average 9.5 years for bipolar II
- Misdiagnosis rate: 69% initially called unipolar depression
- Substance abuse comorbidity: 60% of bipolar patients
| Episode Type | Duration | Severity | Hospitalization | Psychosis | Functional Impact |
|---|---|---|---|---|---|
| Major Depression | ≥2 weeks | Moderate-Severe | 15-20% | 15-20% | Significant impairment |
| Manic | ≥7 days | Severe | 75% | 60% | Marked impairment |
| Hypomanic | ≥4 days | Mild-Moderate | 0% | 0% | Minimal impairment |
| Mixed | ≥2 weeks | Severe | 80% | 70% | Severe impairment |
| Rapid Cycling | 4+ episodes/year | Variable | 40% | 30% | Chronic impairment |
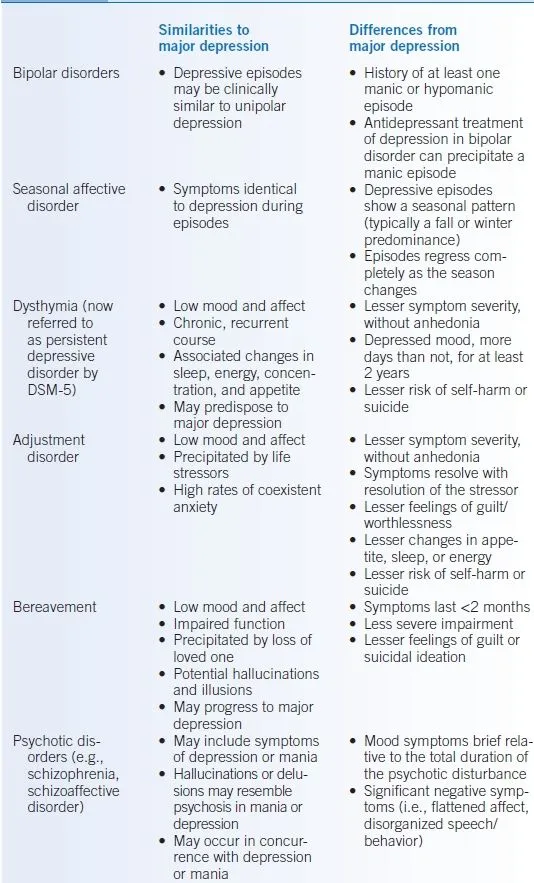
Differential Diagnosis Framework: The "Rule of Threes" guides systematic evaluation: (1) Medical causes (thyroid, neurological, medications), (2) Substance-related (intoxication, withdrawal, induced), (3) Primary psychiatric (mood, anxiety, psychotic disorders).
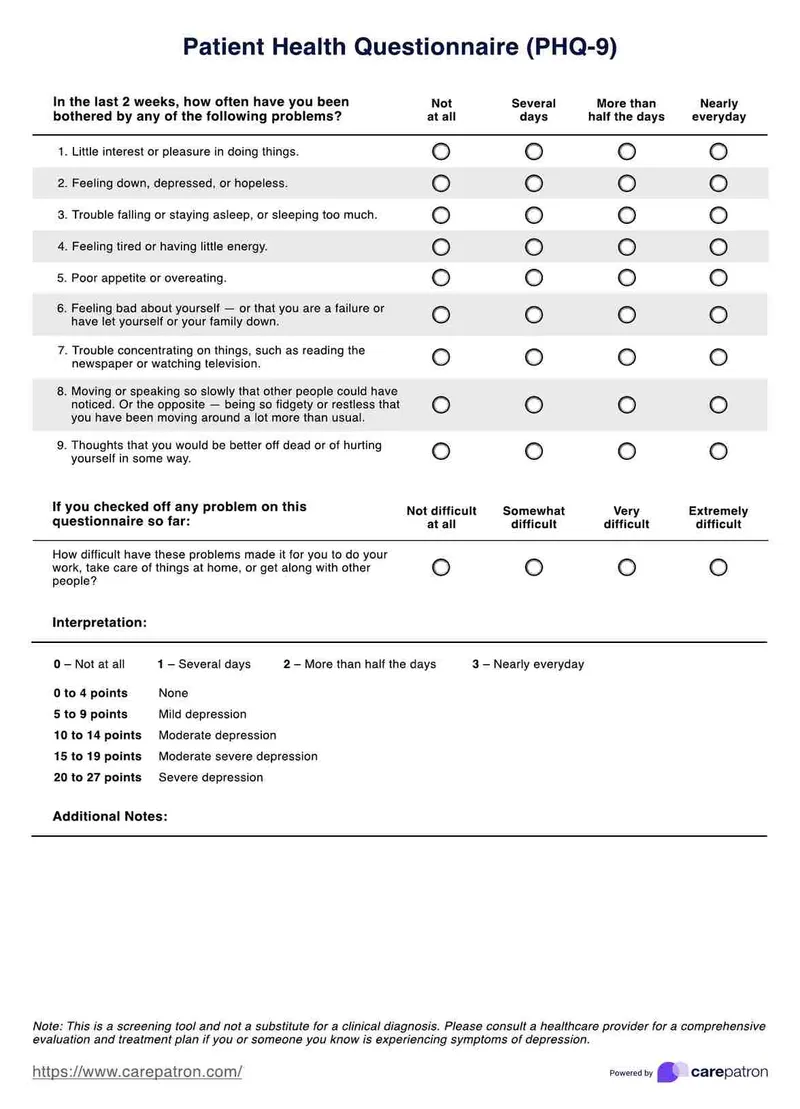
Severity Assessment Tools:
- PHQ-9: Scores 1-4 (minimal), 5-9 (mild), 10-14 (moderate), 15-19 (moderately severe), ≥20 (severe)
- Hamilton Depression Rating Scale: 0-7 (normal), 8-13 (mild), 14-18 (moderate), 19-22 (severe), ≥23 (very severe)
- Young Mania Rating Scale: 0-12 (remission), 13-19 (mild), 20-25 (moderate), ≥26 (severe)
💡 Master This: Pattern recognition requires integrating temporal course (episodic vs. chronic), polarity (unipolar vs. bipolar), and severity (mild vs. severe) with functional assessment. The "3 P's" framework evaluates Precipitants (triggers), Predisposing factors (genetics, trauma), and Perpetuating factors (stress, substance use) to guide treatment planning.
Connect these recognition patterns through systematic discrimination to understand how similar presentations require different therapeutic approaches.
🎯 Clinical Pattern Recognition: The Diagnostic Radar System
🔬 Diagnostic Precision: The Clinical Laboratory
📌 Remember: BIPOLAR HIERARCHY - Bipolar I (mania + depression), Bipolar II (hypomania + depression), Cyclothymic (chronic mild mood swings), Other specified (subthreshold), Unspecified (insufficient information). One manic episode = Bipolar I for life.
Specifier Applications for Diagnostic Precision:
- Severity specifiers: Mild, moderate, severe based on symptom count and functional impairment
- Course specifiers: Single episode, recurrent, in partial/full remission
- Feature specifiers: Psychotic, catatonic, melancholic, atypical, anxious distress
- Pattern specifiers: Rapid cycling, seasonal, peripartum onset
-
Major Depressive Disorder Variants
- Melancholic features: Anhedonia + ≥3 of: morning worsening, early awakening, psychomotor changes, weight loss, guilt
- Atypical features: Mood reactivity + ≥2 of: hypersomnia, hyperphagia, leaden paralysis, rejection sensitivity
- Psychotic features: Delusions/hallucinations in 15-20% of severe episodes
- Melancholic subtype: 25% of major depression cases
- Treatment resistance: 40% higher in melancholic depression
- Suicide risk: 2x higher with psychotic features
-
Bipolar Disorder Subtypes
- Bipolar I: ≥1 manic episode (may include depression)
- Bipolar II: ≥1 hypomanic + ≥1 major depressive episode
- Cyclothymic: ≥2 years of hypomanic and depressive periods
- Conversion rate: 15-50% of Bipolar II converts to Bipolar I
- Rapid cycling: ≥4 episodes/year in 20% of patients
- Ultra-rapid cycling: ≥4 episodes/month in 5% of cases
| Diagnostic Category | Key Distinguishing Features | Duration Requirements | Exclusion Criteria | Prevalence | Prognosis |
|---|---|---|---|---|---|
| Major Depression | ≥5 symptoms, no mania history | ≥2 weeks | No manic/hypomanic episodes | 16.6% | 65% response rate |
| Bipolar I | Manic episode history | ≥7 days mania | Substance/medical exclusion | 1.0% | 60-80% response |
| Bipolar II | Hypomania + depression | ≥4 days hypomania | No manic episodes | 1.1% | 50-70% response |
| Cyclothymia | Chronic mood instability | ≥2 years | No major episodes | 0.4% | 45-60% response |
| Persistent Depression | Chronic low-grade depression | ≥2 years | May include major episodes | 2.5% | 55-65% response |
Secondary Mood Disorder Evaluation: The medical workup includes thyroid function (TSH, T3, T4), complete metabolic panel, vitamin B12/folate, inflammatory markers (ESR, CRP), and neuroimaging when indicated. Medication-induced mood episodes occur with corticosteroids (60% risk), interferon (45% risk), and isotretinoin (15% risk).
Comorbidity Assessment: Anxiety disorders co-occur in 75% of mood disorder patients, substance use disorders in 40%, and personality disorders in 30%. Anxious distress specifier applies when ≥2 anxiety symptoms (tension, restlessness, concentration difficulty, fear of losing control, physical symptoms) occur during mood episodes.
💡 Master This: Diagnostic precision requires temporal mapping of mood episodes, polarity assessment (unipolar vs. bipolar), severity grading (mild/moderate/severe), and specifier application (psychotic, mixed, rapid cycling). The "TEMPS" framework evaluates Temporal course, Episode characteristics, Medical factors, Psychosocial stressors, and Substance use to achieve diagnostic accuracy.
Connect these diagnostic distinctions through evidence-based treatment algorithms to understand how precise diagnosis guides therapeutic selection and outcome prediction.
🔬 Diagnostic Precision: The Clinical Laboratory
⚖️ Treatment Command Center: Evidence-Based Therapeutic Algorithms
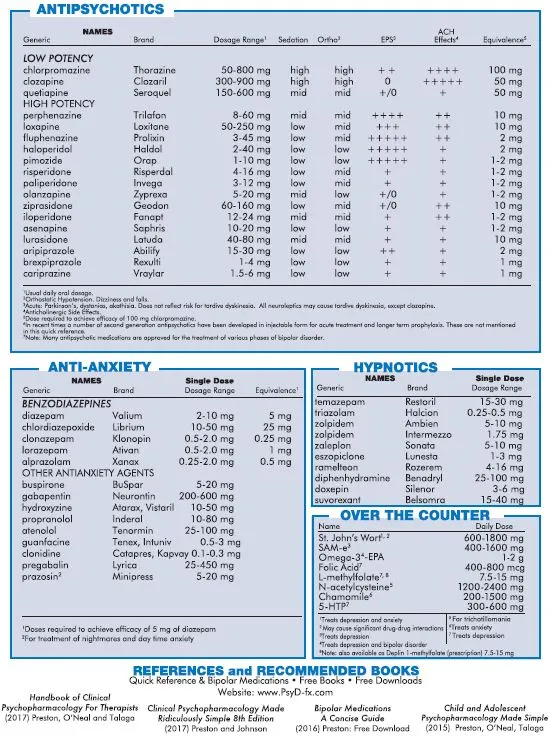
📌 Remember: TREATMENT TIERS - Therapy first-line (CBT/IPT), Rx medications (SSRI/SNRI), Enhancement (augmentation), Advanced (TMS/ECT), Treatment-resistant (MAOIs/combinations), Maintenance (long-term), Emergency (hospitalization), Neuromodulation (DBS), Targeted (pharmacogenomics).
Major Depression Treatment Algorithm:
- First-line: SSRI/SNRI monotherapy with psychotherapy
- Partial response (4-6 weeks): Dose optimization or augmentation
- Non-response (8-12 weeks): Switch medication class
- Treatment-resistant: Combination therapy or neuromodulation
-
SSRI Selection and Dosing
- Sertraline: 50-200mg daily, half-life 26 hours
- Escitalopram: 10-20mg daily, most selective 5-HT reuptake
- Fluoxetine: 20-80mg daily, longest half-life (4-6 days)
- Response rate: 65% at 6 weeks with adequate dosing
- Remission rate: 35% in first trial, 67% with optimization
- Side effects: Sexual dysfunction (60%), weight gain (25%), activation (15%)
-
Bipolar Disorder Treatment Protocols
- Acute mania: Lithium or valproate + antipsychotic
- Bipolar depression: Lithium + lamotrigine or quetiapine
- Maintenance: Mood stabilizer monotherapy or combination
- Lithium levels: 0.8-1.2 mEq/L acute, 0.6-0.8 mEq/L maintenance
- Valproate levels: 50-125 mcg/mL therapeutic range
- Relapse prevention: 70% reduction with maintenance therapy
| Medication Class | First-Line Options | Response Rate | Time to Response | Common Side Effects | Monitoring Required |
|---|---|---|---|---|---|
| SSRI | Sertraline, Escitalopram | 65% | 4-6 weeks | Sexual, GI, activation | Minimal |
| SNRI | Venlafaxine, Duloxetine | 70% | 4-6 weeks | HTN, sexual, withdrawal | Blood pressure |
| Mood Stabilizers | Lithium, Valproate | 60-80% | 1-3 weeks | Tremor, weight gain | Levels, renal, thyroid |
| Atypical Antipsychotics | Quetiapine, Aripiprazole | 55-75% | 1-2 weeks | Metabolic, sedation | Weight, glucose, lipids |
| MAOIs | Phenelzine, Tranylcypromine | 75% | 3-6 weeks | Hypertensive crisis | Dietary restrictions |
Psychotherapy Integration: Cognitive Behavioral Therapy (CBT) shows equivalent efficacy to medications for mild-moderate depression with 16-20 sessions over 12-16 weeks. Interpersonal Therapy (IPT) targets relationship patterns and shows 60% response rates. Combination therapy (medication + psychotherapy) achieves 75% response rates versus 50% for monotherapy.
Neuromodulation Approaches:
- Transcranial Magnetic Stimulation (TMS): 50% response rate, 33% remission rate in treatment-resistant depression
- Electroconvulsive Therapy (ECT): 80-90% response rate in severe depression, 6-12 treatments over 3-4 weeks
- Deep Brain Stimulation (DBS): Subgenual cingulate targeting shows 60% response in ultra-treatment-resistant cases
💡 Master This: Treatment success requires algorithm-driven selection based on symptom profile, episode pattern, and patient factors. The "MATCH" principle guides decisions: Medication selection by neurotransmitter target, Augmentation for partial response, Therapy integration, Combination strategies for resistance, High-intensity interventions (ECT/TMS) for severe cases.
Connect these treatment algorithms through multi-system integration to understand how comprehensive care addresses the complex neurobiological and psychosocial aspects of mood disorders.
⚖️ Treatment Command Center: Evidence-Based Therapeutic Algorithms
🌐 The Mood Ecosystem: Multi-System Integration Mastery
📌 Remember: INTEGRATION MATRIX - Individual factors (genetics, personality), Neurobiological (neurotransmitters, circuits), Treatment response (medications, therapy), Environmental (stress, trauma), Genetic testing (pharmacogenomics), Risk factors (medical, substance), Assessment tools (rating scales), Timing (episode patterns), Intervention (multimodal), Outcomes (functional recovery), Network support (family, social).
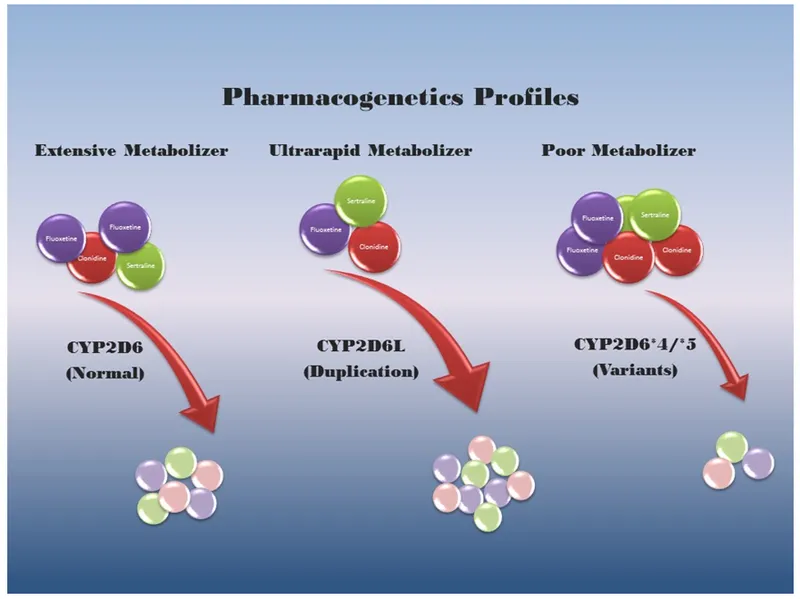
Pharmacogenomic Integration:
- CYP2D6 variants affect 25% of psychiatric medications
- CYP2C19 poor metabolizers (7% of population) show increased side effects with SSRIs
- MTHFR polymorphisms predict L-methylfolate augmentation response
- HLA-B*5701 testing prevents carbamazepine hypersensitivity in 5-15% of patients
-
Medical Comorbidity Management
- Cardiovascular disease: 30% higher risk in depression
- Diabetes: 2x prevalence in mood disorders
- Chronic pain: 50% comorbidity with depression
- Integrated care models improve outcomes by 40%
- Collaborative care reduces costs by 25%
- Measurement-based care increases remission rates to 60%
-
Substance Use Integration
- Alcohol use disorders: 40% comorbidity with mood disorders
- Cannabis use: 25% prevalence in bipolar patients
- Stimulant use: 15% in treatment-seeking mood disorder patients
- Dual diagnosis treatment improves abstinence rates to 55%
- Integrated therapy reduces hospitalization by 35%
- Medication interactions require dose adjustments in 60% of cases
| Integration Domain | Prevalence | Impact on Outcomes | Evidence-Based Interventions | Success Metrics |
|---|---|---|---|---|
| Medical Comorbidity | 75% | 40% worse outcomes | Collaborative care | 40% improvement |
| Substance Use | 40% | 60% worse outcomes | Integrated treatment | 55% abstinence |
| Anxiety Disorders | 75% | 50% worse outcomes | Combined therapy | 65% response |
| Personality Disorders | 30% | 70% worse outcomes | Dialectical behavior therapy | 45% improvement |
| Trauma History | 60% | 45% worse outcomes | Trauma-focused therapy | 60% response |
Precision Medicine Applications: Biomarker research identifies inflammatory markers (IL-6, TNF-α, CRP) elevated in 30% of depressed patients, predicting anti-inflammatory augmentation response. Neuroimaging biomarkers using fMRI connectivity patterns predict CBT response with 80% accuracy and medication response with 75% accuracy.
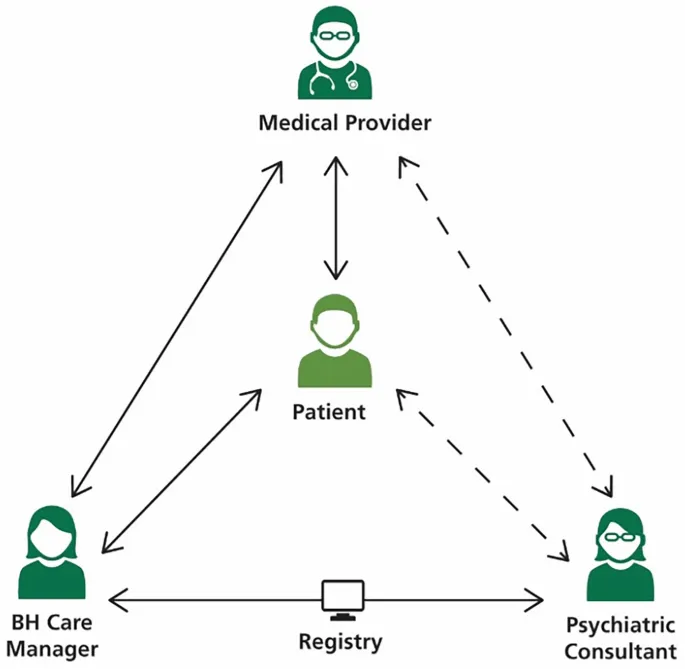
Digital Health Integration: Smartphone apps with mood tracking and medication reminders improve adherence by 35%. Telepsychiatry shows equivalent outcomes to in-person care with 90% patient satisfaction. AI-powered risk prediction models identify suicide risk with 85% sensitivity using electronic health record data.
Recovery-Oriented Care: Functional recovery extends beyond symptom remission to include occupational functioning, social relationships, and quality of life. Peer support programs reduce rehospitalization by 30% and improve medication adherence by 25%. Wellness Recovery Action Plans (WRAP) empower patient self-management and reduce crisis episodes by 40%.
💡 Master This: Systems integration requires coordinating biological treatments (medications, neuromodulation), psychological interventions (therapy, skills training), social supports (family, peers, community), and medical care (primary care, specialists). The "BIOPSYCHOSOCIAL-PLUS" model adds spiritual, cultural, and digital health dimensions to create comprehensive, personalized treatment plans that address whole-person recovery.
Connect these integration principles through rapid mastery frameworks to develop practical tools for immediate clinical application and long-term treatment optimization.
🌐 The Mood Ecosystem: Multi-System Integration Mastery
🎯 Clinical Mastery Arsenal: Rapid-Fire Diagnostic and Treatment Tools
📌 Remember: RAPID ASSESSMENT - Risk evaluation (suicide, violence), Affect and mood state, Psychosis screening, Impairment level, Duration and course, Alcohol/substance use, Severity markers, Support systems, Episode characteristics, Specifiers present, Systemic factors, Medical causes, Emergency indicators, Needs assessment, Treatment history.
Essential Clinical Arsenal:
-
5-Minute Diagnostic Screen
- Mood episodes: "Worst 2+ weeks of depression?" "Best 4+ days of elevated mood?"
- Functional impairment: "Unable to work/relationships/self-care?"
- Suicide risk: "Thoughts of death/dying/suicide?" Columbia Scale if positive
- Positive screen requires full assessment within 24 hours
- Immediate risk factors: Plan, means, intent, timeline
- Protective factors: Reasons for living, social support, treatment engagement
-
Treatment Selection Matrix
- First episode depression: SSRI + psychotherapy
- Recurrent depression: Previous effective medication or SNRI
- Bipolar depression: Mood stabilizer + lamotrigine/quetiapine
- Treatment-resistant: Augmentation or switch class
- Response timeline: 2 weeks (early signs), 6 weeks (significant), 12 weeks (full trial)
- Dose optimization: Maximum tolerated before switching
- Augmentation options: Lithium, T3, antipsychotics, stimulants
| Clinical Scenario | First-Line Treatment | Response Rate | Monitoring | Red Flags |
|---|---|---|---|---|
| First Depression Episode | SSRI + CBT | 70% | PHQ-9 q2weeks | Suicidal ideation |
| Recurrent Depression | Previous effective Rx | 75% | Side effects | Treatment resistance |
| Bipolar Depression | Mood stabilizer + lamotrigine | 60% | Mood charts | Switching to mania |
| Mixed Episode | Mood stabilizer + antipsychotic | 65% | Daily monitoring | Rapid cycling |
| Treatment-Resistant | Augmentation/ECT | 50% | Specialized care | Chronic suicidality |
Crisis Management Protocols:
- Suicidal ideation: Safety planning, means restriction, emergency contacts
- Manic episode: Hospitalization if poor judgment, psychosis, agitation
- Mixed episode: Highest risk period - intensive monitoring required
- Rapid cycling: Mood stabilizer optimization, trigger identification
Medication Quick Reference:
Essential Numbers for Clinical Practice:
- Lithium therapeutic range: 0.6-1.2 mEq/L
- Valproate therapeutic range: 50-125 mcg/mL
- SSRI response timeline: 2-6 weeks for effect, 12 weeks for full trial
- ECT response rate: 80-90% in severe depression
- TMS response rate: 50% in treatment-resistant depression
- Suicide risk: 15x higher in mood disorders, 25% attempt rate in bipolar
Monitoring and Follow-up Framework:
- Weekly visits for first 4 weeks of new medication
- Bi-weekly for weeks 4-12 during optimization
- Monthly for stable patients on maintenance therapy
- Rating scales at every visit: PHQ-9, GAD-7, YMRS
- Laboratory monitoring: Lithium levels q3months, metabolic panel for antipsychotics
💡 Master This: Clinical mastery combines rapid pattern recognition with systematic assessment and evidence-based treatment selection. The "FAST TRACK" approach: Functional assessment, Affect evaluation, Suicide screening, Treatment history, Timing of episodes, Risk factors, Augmentation needs, Crisis planning, Key monitoring parameters. Master these tools, and you possess the clinical arsenal for optimal mood disorder management across all practice settings.
🎯 Clinical Mastery Arsenal: Rapid-Fire Diagnostic and Treatment Tools
Practice Questions: Mood Disorders
Test your understanding with these related questions
A researcher is investigating whether there is an association between the use of social media in teenagers and bipolar disorder. In order to study this potential relationship, she collects data from people who have bipolar disorder and matched controls without the disorder. She then asks how much on average these individuals used social media in the 3 years prior to their diagnosis. This continuous data is divided into 2 groups: those who used more than 2 hours per day and those who used less than 2 hours per day. She finds that out of 1000 subjects, 500 had bipolar disorder of which 300 used social media more than 2 hours per day. She also finds that 400 subjects who did not have the disorder also did not use social media more than 2 hours per day. Which of the following is the odds ratio for development of bipolar disorder after being exposed to more social media?













