Inborn Errors of Metabolism US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Inborn Errors of Metabolism. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Inborn Errors of Metabolism US Medical PG Question 1: An infant presents with vomiting after feeding. Benedict's test was positive for a non-glucose reducing substance. What is the most likely diagnosis?
- A. Galactosemia due to GAL-1-P Uridyl Transferase enzyme deficiency (Correct Answer)
- B. Fructosuria due to Fructokinase deficiency
- C. Hereditary fructose intolerance due to Aldolase B deficiency
- D. Primary lactose intolerance
- E. Glycogen storage disease due to Glucose-6-phosphatase deficiency
Inborn Errors of Metabolism Explanation: ***Galactosemia due to GAL-1-P Uridyl Transferase enzyme deficiency***
- Vomiting after feeding in an infant, coupled with a **positive Benedict's test** for a **non-glucose reducing substance**, is highly indicative of galactosemia. The accumulation of **galactose-1-phosphate** and **galactitol** leads to toxicity and symptoms.
- This enzyme deficiency, causing **classic galactosemia**, prevents the proper metabolism of **galactose**, leading to its buildup.
*Fructosuria due to Fructokinase deficiency*
- This condition is a **benign metabolic disorder** with no significant clinical symptoms.
- While it would lead to fructose in the urine, the infant would not typically present with **vomiting after feeding**.
*Hereditary fructose intolerance due to Aldolase B deficiency*
- Symptoms usually appear after the introduction of **fructose-containing foods** into the diet, causing severe hypoglycemia and vomiting.
- The positive Benedict's test in this scenario would typically indicate a reducing substance in the urine, while fructose intolerance is characterized by **hypoglycemia** and metabolic crises upon fructose ingestion.
*Glycogen storage disease due to Glucose-6-phosphatase deficiency*
- This disorder primarily causes **hypoglycemia** and liver enlargement, not primarily vomiting after feeding due to a **non-glucose reducing substance**.
- Glucose-6-phosphatase deficiency (Von Gierke's disease) leads to an inability to release **glucose from glycogen** and causes severe hypoglycemia, often requiring frequent feeding.
*Primary lactose intolerance*
- While lactose intolerance can cause vomiting and gastrointestinal symptoms, it is **extremely rare in infants** (primary lactose intolerance is a late-onset condition).
- Lactose would be a reducing sugar, but the key differentiator is that **galactose** (from galactosemia) is the non-glucose reducing substance detected in this case, along with the typical **toxic presentation** in neonates.
Inborn Errors of Metabolism US Medical PG Question 2: Congenital lactic acidosis is primarily due to a defect in which enzyme?
- A. Branched chain alpha-ketoacid dehydrogenase
- B. Isocitrate dehydrogenase (IDH)
- C. Transketolase
- D. Pyruvate dehydrogenase (Correct Answer)
Inborn Errors of Metabolism Explanation: ***Pyruvate dehydrogenase***
- A defect in **pyruvate dehydrogenase (PDH)** complex prevents the conversion of **pyruvate to acetyl-CoA**, shunting pyruvate to **lactate production**.
- This leads to an accumulation of **lactic acid** in the body, causing **congenital lactic acidosis**.
*Branched chain alpha-ketoacid dehydrogenase*
- A defect in **branched-chain alpha-ketoacid dehydrogenase** is responsible for **Maple Syrup Urine Disease**, not congenital lactic acidosis.
- This enzyme is crucial for the metabolism of **branched-chain amino acids** (leucine, isoleucine, and valine).
*Isocitrate dehydrogenase (IDH)*
- **Isocitrate dehydrogenase (IDH)** is an enzyme in the **Krebs cycle** that converts isocitrate to alpha-ketoglutarate.
- Defects or mutations in IDH enzymes are associated with certain **cancers**, but not primarily with congenital lactic acidosis.
*Transketolase*
- **Transketolase** is an enzyme involved in the **pentose phosphate pathway**, which generates NADPH and C5 sugars.
- A deficiency in transketolase is associated with **Wernicke-Korsakoff syndrome** due to thiamine deficiency, not congenital lactic acidosis.
Inborn Errors of Metabolism US Medical PG Question 3: Tay-Sachs disease is due to a deficiency of which enzyme?
- A. Hexosaminidase B
- B. α-galactosidase
- C. Hexosaminidase A (Correct Answer)
- D. Sphingomyelinase
Inborn Errors of Metabolism Explanation: ***Hexosaminidase A***
- **Tay-Sachs disease** is caused by a genetic deficiency in the lysosomal enzyme **hexosaminidase A (HexA)**.
- This deficiency leads to the accumulation of **GM2 ganglioside** in neuronal cells, particularly in the brain, causing progressive neurodegeneration.
*Hexosaminidase B*
- A deficiency in **hexosaminidase B** is associated with **Sandhoff disease**, a lysosomal storage disorder similar to Tay-Sachs but typically more severe.
- While HexA is composed of alpha and beta subunits, a deficiency specifically in the beta subunit is characteristic of Sandhoff disease.
*α-galactosidase*
- A deficiency in **α-galactosidase** is responsible for **Fabry disease**, an X-linked lysosomal storage disorder.
- It leads to the accumulation of **globotriaosylceramide (Gb3)**, primarily affecting the kidneys, heart, and nervous system, and does not present with the neurological symptoms of Tay-Sachs.
*Sphingomyelinase*
- A deficiency in **sphingomyelinase** causes **Niemann-Pick disease (Type A and B)**, another lysosomal storage disorder.
- This leads to the accumulation of **sphingomyelin** in various organs, resulting in hepatosplenomegaly, neurodegeneration (in Type A), and lung disease, distinct from Tay-Sachs.
Inborn Errors of Metabolism US Medical PG Question 4: Which amino acids accumulate in maple syrup urine disease?
- A. Valine
- B. Leucine
- C. Isoleucine
- D. All branched-chain amino acids (Correct Answer)
Inborn Errors of Metabolism Explanation: ***All branched-chain amino acids***
- Maple syrup urine disease (MSUD) is characterized by a deficiency in the **branched-chain alpha-keto acid dehydrogenase complex**, which is responsible for the breakdown of branched-chain amino acids (BCAAs).
- This deficiency leads to the accumulation of **leucine, isoleucine, and valine**, along with their corresponding alpha-keto acids, in the blood and urine.
- The distinctive **maple syrup odor** in the urine is caused by the accumulation of branched-chain keto acids derived from all three BCAAs.
*Leucine*
- While leucine is one of the BCAAs that accumulates in MSUD, it is not the *only* amino acid involved.
- The accumulation of **leucine** is particularly associated with the severe neurological symptoms seen in MSUD, as it is the most neurotoxic of the three BCAAs.
*Valine*
- Valine is another BCAA that accumulates due to the metabolic block in MSUD.
- However, the disease involves the accumulation of all three BCAAs, not just valine in isolation.
*Isoleucine*
- Isoleucine is the third BCAA that accumulates in MSUD due to the defective enzyme.
- Like leucine and valine, isoleucine and its corresponding keto acid accumulate in blood and urine when the branched-chain alpha-keto acid dehydrogenase complex is deficient.
Inborn Errors of Metabolism US Medical PG Question 5: In type IA Maple Syrup Urine Disease, which gene mutation is responsible?
- A. BCKDHB
- B. DBT
- C. DLD
- D. BCKDHA (Correct Answer)
Inborn Errors of Metabolism Explanation: ***BCKDHA***
- **Maple Syrup Urine Disease (MSUD)** type IA is caused by a mutation in the **BCKDHA gene**, which codes for the E1α subunit of the **branched-chain α-keto acid dehydrogenase (BCKD) complex**.
- This **enzyme complex** is crucial for the metabolism of **branched-chain amino acids (BCAAs)**: leucine, isoleucine, and valine.
*BCKDHB*
- The **BCKDHB gene** codes for the E1β subunit of the **BCKD complex**.
- Mutations in **BCKDHB** are associated with **type IB MSUD**, not type IA.
*DBT*
- The **DBT gene** codes for the E2 subunit (dihydrolipoyl transacylase) of the **BCKD complex**.
- Mutations in **DBT** are responsible for **type II MSUD**.
*DLD*
- The **DLD gene** codes for the E3 subunit (dihydrolipoyl dehydrogenase), which is a component shared by several **α-keto acid dehydrogenase complexes**.
- Mutations in the **DLD gene** lead to **type III MSUD** and other pyruvate dehydrogenase complex deficiencies, rather than type IA.
Inborn Errors of Metabolism US Medical PG Question 6: The enzyme deficient in Galactosemia is:-
- A. Galactose-1-phosphate uridyltransferase (GALT) (Correct Answer)
- B. Sphingomyelinase
- C. Glucocerebrosidase
- D. Hexosaminidase
Inborn Errors of Metabolism Explanation: ***Galactose-1-phosphate uridyltransferase (GALT)***
- Deficiency of **GALT** leads to the accumulation of **galactose-1-phosphate** in tissues, which is toxic and causes the symptoms of **classical galactosemia**.
- This enzyme is crucial for the second step in the Leloir pathway, converting **galactose-1-phosphate** and UDP-glucose into UDP-galactose and glucose-1-phosphate.
*Sphingomyelinase (associated with Niemann-Pick disease)*
- Deficiency in **sphingomyelinase** causes the accumulation of **sphingomyelin**, leading to **Niemann-Pick disease**, characterized by hepatosplenomegaly and neurological deterioration.
- This enzyme is involved in the catabolism of lipids, distinct from carbohydrate metabolism.
*Glucocerebrosidase (associated with Gaucher's disease)*
- Deficiency of **glucocerebrosidase** results in the accumulation of **glucocerebroside**, leading to **Gaucher's disease**, which affects the spleen, liver, bone marrow, and sometimes the brain.
- This is a lysosomal storage disorder involving glycosphingolipids, not galactose metabolism.
*Hexosaminidase (associated with Tay-Sachs disease)*
- Deficiency of **hexosaminidase A** causes the accumulation of **GM2 ganglioside**, resulting in **Tay-Sachs disease**, a severe neurodegenerative disorder.
- This enzyme primarily functions in the breakdown of gangliosides, which are complex lipids, not galactose.
Inborn Errors of Metabolism US Medical PG Question 7: Neonatal tyrosinemia is due to deficiency of which enzyme?
- A. Tyrosine transaminase
- B. Hydroxyphenyl pyruvate hydroxylase (Correct Answer)
- C. Fumarylacetoacetate hydroxylase
- D. Tyrosinase
Inborn Errors of Metabolism Explanation: ***Hydroxyphenyl pyruvate hydroxylase***
- **Neonatal (transient) tyrosinemia** is caused by delayed maturation or deficiency of **hydroxyphenylpyruvate hydroxylase** (also called 4-hydroxyphenylpyruvate dioxygenase or HPPD).
- This enzyme converts 4-hydroxyphenylpyruvate to homogentisic acid in tyrosine catabolism.
- Common in **premature infants** and newborns, leading to elevated tyrosine levels in blood.
- The condition is **benign and self-limiting**, usually resolving with **vitamin C supplementation** or as the enzyme matures.
- Note: Severe hereditary deficiency of this enzyme causes **tyrosinemia type III**, a distinct and rare disorder.
*Fumarylacetoacetate hydroxylase*
- Deficiency of **fumarylacetoacetate hydroxylase (FAH)** causes **tyrosinemia type I** (hepatorenal tyrosinemia), NOT neonatal tyrosinemia.
- This is a severe hereditary disorder with liver failure, renal tubular dysfunction, and accumulation of toxic metabolites like succinylacetone.
- Distinct from the benign transient neonatal form.
*Tyrosine transaminase*
- Deficiency of **tyrosine transaminase** (tyrosine aminotransferase) causes **tyrosinemia type II** (Richner-Hanhart syndrome).
- Presents with corneal ulcers, palmoplantar hyperkeratosis, and sometimes intellectual disability.
*Tyrosinase*
- Deficiency of **tyrosinase** causes **albinism**, characterized by lack of melanin pigment in skin, hair, and eyes.
- Not involved in tyrosine catabolism but in melanin synthesis.
Inborn Errors of Metabolism US Medical PG Question 8: Amount of ORS to be given in the first 4 hours to a child with some dehydration is
- A. 75 ml/kg body wt. (Correct Answer)
- B. 50 ml/kg body wt.
- C. 100 ml/kg body wt.
- D. 200 ml/kg body wt.
Inborn Errors of Metabolism Explanation: ***75 ml/kg body wt.***
- For a child with **some dehydration**, the World Health Organization (WHO) and UNICEF recommend administering **75 mL/kg body weight** of ORS over the first 4 hours as part of Plan B.
- This volume is calculated to replenish lost fluids and electrolytes, addressing the estimated fluid deficit in **some dehydration**.
*50 ml/kg body wt.*
- A dose of **50 mL/kg** is generally insufficient for effective rehydration in a child presenting with **some dehydration**.
- This amount might be used in milder cases or for maintenance, but not for initial rehydration in the **first 4 hours** with signs of dehydration.
*100 ml/kg body wt.*
- Administering **100 mL/kg** body weight is typically used for **severe dehydration** (Plan C) when given as **intravenous fluids**.
- For **some dehydration** treated with ORS, the recommended dose is 75 mL/kg, not 100 mL/kg. This higher amount could lead to fluid overload if given orally in the first 4 hours.
*200 ml/kg body wt.*
- A dose of **200 mL/kg** body weight is excessive and potentially dangerous for a child with **some dehydration**.
- Such a large volume could lead to **fluid overload**, electrolyte imbalances, and other complications, especially in young children.
Inborn Errors of Metabolism US Medical PG Question 9: A 52-year-old man is admitted directly from the clinic for a serum glucose of 980 mg/dL. He has had type 2 diabetes for 16 years, for which he was prescribed metformin and glimepiride; however, he reports not having followed his prescription due to its high cost. For the past 12 days, he has had excess urination, and has lost 6 kg in weight. He has also noted a progressively worsening cough productive of greenish-brown sputum for approximately 20 days. His temperature is 38.9°C (102.02°F), blood pressure is 97/62 mm Hg, pulse is 97/minute and respiratory rate is 26/minute. On physical examination, he is somnolent, his eyes are sunken, and there are crackles at the left lung base.
Lab results are shown:
Arterial pH: 7.33
Serum sodium: 130 mEq/L
Serum potassium: 3 mEq/L
Serum osmolality: 325 mOsm/kg
Serum beta-hydroxybutyrate: negative
Urinalysis: trace ketones
Intravenous normal saline infusion is started. Which of the following is the best next step in this patient?
- A. Adding sodium bicarbonate infusion
- B. Starting basal-bolus insulin
- C. Adding dopamine infusion
- D. Adding potassium to the intravenous fluids (Correct Answer)
- E. Starting regular insulin infusion
Inborn Errors of Metabolism Explanation: ***Adding potassium to the intravenous fluids***
- This patient presents with **hypokalemia** (serum potassium 3 mEq/L) and is receiving aggressive fluid resuscitation, which will further dilute his potassium and drive potassium into cells, potentially worsening the hypokalemia. **Potassium replacement** is critical to prevent cardiac arrhythmias.
- While fluids and insulin will be necessary, **correcting potassium** should be initiated early, especially with symptoms of hypokalemia or if the level is <3.3 mEq/L, to prevent serious complications and before starting insulin.
*Adding sodium bicarbonate infusion*
- The patient's arterial pH of 7.33 indicates only **mild acidosis**, likely due to hypovolemic lactic acidosis or other underlying issues, but not severe enough to warrant bicarbonate infusion.
- Additionally, his serum beta-hydroxybutyrate is negative and ketones are only trace, ruling out **diabetic ketoacidosis (DKA)**, which is typically the primary indication for bicarbonate in diabetic emergencies.
*Starting basal-bolus insulin*
- The patient requires insulin for his **hyperglycemia**, but **basal-bolus insulin** is usually started once the patient is stable, able to eat, and out of the acute hyperosmolar state.
- In this emergency setting, **intravenous regular insulin infusion** is preferred for precise titration and rapid glucose control.
*Adding dopamine infusion*
- Dopamine is a **vasopressor** used to support blood pressure in cases of **hypotensive shock** refractory to fluid resuscitation.
- While the patient is hypotensive (BP 97/62 mm Hg), his primary problem is severe dehydration, so initial management focuses on **fluid resuscitation** with normal saline rather than immediate pressors.
*Starting regular insulin infusion*
- While **regular insulin infusion** is appropriate for managing severe hyperglycemia in hyperosmolar hyperglycemic state (HHS), it should be initiated **after initial fluid resuscitation** and after ensuring potassium is ≥3.3 mEq/L.
- Administering insulin without adequate potassium replacement could precipitate severe and life-threatening **hypokalemia**, as insulin drives potassium into cells.
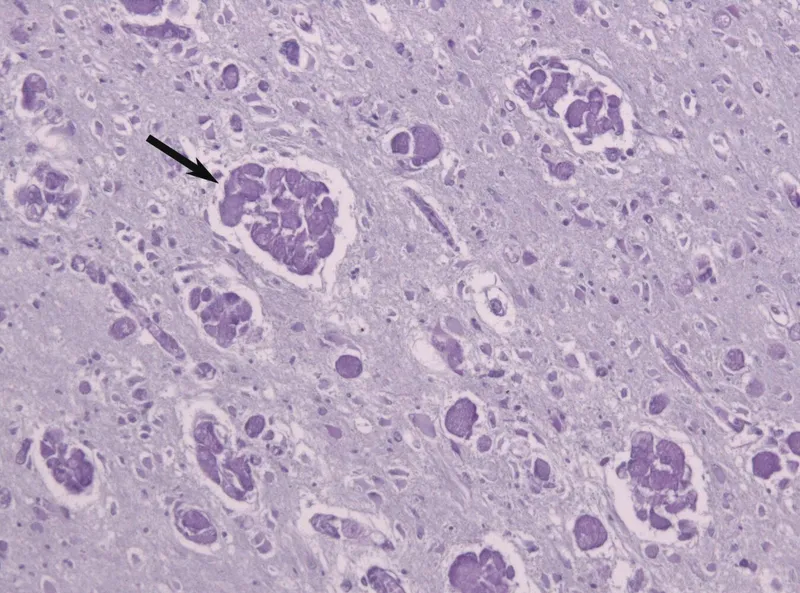
Inborn Errors of Metabolism US Medical PG Question 10: An 11-year-old boy was brought to the outpatient clinic with intention tremor and poor scholastic performance. His sister has similar complaints. On examination, hepatomegaly is seen. The eye finding is shown in the image. What is the probable diagnosis?
- A. Glutaric aciduria
- B. Wilson's disease (Correct Answer)
- C. Hepatitis A
- D. Huntington's chorea
Inborn Errors of Metabolism Explanation: ***Wilson's disease***
- The combination of **intention tremor**, **poor scholastic performance** (indicating neurological involvement), **hepatomegaly**, and the **eye finding** (Kayser-Fleischer ring seen in the image) points strongly to Wilson's disease. The sister having similar complaints suggests an **autosomal recessive** inheritance pattern, consistent with Wilson's disease.
- The image shows **Kayser-Fleischer ring**, a golden-brown ring at the corneal limbus due to **copper deposition in Descemet's membrane**, which is pathognomonic for Wilson's disease with neurological involvement.
- Wilson's disease is caused by mutations in the **ATP7B gene**, leading to impaired copper excretion and accumulation in the liver, brain, and cornea.
*Glutaric aciduria*
- This is a rare **autosomal recessive metabolic disorder** that primarily affects the brain, leading to **dystonia** and **developmental delay**.
- While it can cause neurological symptoms, it typically does not present with **hepatomegaly** or **Kayser-Fleischer rings** as prominent features.
*Hepatitis A*
- **Hepatitis A** is an acute viral infection of the liver, causing symptoms like fever, fatigue, nausea, vomiting, and **jaundice**.
- However, it typically does not cause **intention tremor**, **poor scholastic performance**, or have a familial pattern suggesting an inherited neurological disorder. It also does not cause Kayser-Fleischer rings.
*Huntington's chorea*
- **Huntington's chorea** is an **autosomal dominant neurodegenerative disorder** characterized by **chorea**, psychiatric symptoms, and cognitive decline, typically manifesting in adulthood.
- It does not present with **hepatomegaly** or **Kayser-Fleischer rings** at this age and is not associated with the constellation of liver and neurological symptoms described.
More Inborn Errors of Metabolism US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 oka
oka