Psychotherapy approaches for depression US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Psychotherapy approaches for depression. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Psychotherapy approaches for depression US Medical PG Question 1: A 30-year-old woman comes to the physician because of difficulty sleeping. She is afraid of falling asleep and gets up earlier than desired. Four months ago, she was the driver in a car accident that resulted in the death of her unborn child. She has vivid nightmares of the event and reports that she frequently re-experiences the accident. She blames herself for the death of her child, has stopped working as an accountant, avoids driving in cars, and has withdrawn from her parents and close friends. Which of the following is the most likely diagnosis?
- A. Acute stress disorder
- B. Normal grief
- C. Major depressive disorder
- D. Adjustment disorder
- E. Post-traumatic stress disorder (Correct Answer)
Psychotherapy approaches for depression Explanation: ***Post-traumatic stress disorder***
- The patient's symptoms, including **re-experiencing the trauma** (nightmares, flashbacks), avoidance behaviors (avoiding driving, withdrawing from social interactions), and negative alterations in cognition and mood (difficulty sleeping, self-blame), persisting for **four months** after a traumatic event, are characteristic of PTSD.
- The severity and chronicity of these symptoms, significantly impacting her daily functioning, align with the diagnostic criteria for PTSD.
*Acute stress disorder*
- This diagnosis also involves exposure to a traumatic event and similar symptoms (intrusive thoughts, negative mood, avoidance) but is diagnosed only when symptoms last for a minimum of **3 days and a maximum of 1 month** after the trauma.
- Since the patient's symptoms have persisted for **four months**, acute stress disorder is ruled out.
*Normal grief*
- While grief is a natural response to loss, the patient's symptoms extend beyond typical grief, involving specific **trauma-related re-experiencing** and **avoidance behaviors** that are not primarily focused on the deceased, but rather on the traumatic event itself.
- Normal grief typically does not involve the severe, persistent avoidance and intrusive symptoms of a traumatic nature seen here.
*Major depressive disorder*
- Although the patient exhibits symptoms that could overlap with depression (difficulty sleeping, withdrawal, loss of interest), the primary driver of her symptoms is the **traumatic event** and its associated re-experiencing and avoidance.
- A diagnosis of MDD would be considered if the depressive symptoms are paramount and not better explained by the trauma response, but in this case, the **trauma-specific symptoms** are central.
*Adjustment disorder*
- This disorder is characterized by the development of emotional or behavioral symptoms in response to an identifiable stressor, occurring within **3 months of the stressor**.
- While a traumatic event could be a stressor, adjustment disorder is diagnosed when the symptoms **do not meet the criteria for another specific mental disorder**, like PTSD, and are generally less severe and pervasive than what is described in this patient.
Psychotherapy approaches for depression US Medical PG Question 2: During a psychotherapy session, a psychiatrist notes transference. Which of the following is an example of this phenomenon?
- A. The patient feels powerless to change and blames his problems on the situation into which he was born
- B. The doctor feels that the patient's unwillingness to change is frustrating as it is similar to the feelings the doctor has towards his/her child with behavior problems
- C. The patient feels that her father is too controlling and interferes with all aspects of her life
- D. The patient is annoyed by the doctor because he feels the doctor is lecturing like his mother used to do (Correct Answer)
- E. The doctor has feelings of sexual attraction towards the patient
Psychotherapy approaches for depression Explanation: ***The patient is annoyed by the doctor because he feels the doctor is lecturing like his mother used to do***
- This is a classic example of **transference**, where the patient unconsciously projects feelings and attitudes from significant past relationships (like with a parent) onto the therapist.
- The patient is reacting to the doctor not based on the doctor's current behavior, but through the lens of past experiences with their **mother's lecturing style**.
*The patient feels powerless to change and blames his problems on the situation into which he was born*
- This describes an **external locus of control** and possibly a sense of learned helplessness, but it doesn't involve projecting past relational patterns onto the therapist.
- While it's a patient's feeling, it's about their life situation rather than their perception of the therapist based on past figures.
*The doctor feels that the patient's unwillingness to change is frustrating as it is similar to the feelings the doctor has towards his/her child with behavior problems*
- This scenario describes **countertransference**, where the **therapist's** unresolved issues or feelings towards significant others (like their child) are projected onto the patient.
- Transference specifically refers to the patient's projection, not the therapist's.
*The patient feels that her father is too controlling and interferes with all aspects of her life*
- This is a direct statement about the patient's current relationship with her father, or a past experience, and does not involve projecting these feelings onto the **therapist**.
- While it might be a topic explored in therapy, it's not a manifestation of transference *within* the therapeutic relationship itself.
*The doctor has feelings of sexual attraction towards the patient*
- This is an example of **countertransference**, as it describes the **therapist's** feelings towards the patient, rather than the patient's feelings towards the therapist.
- Such feelings, especially sexual attraction, are considered unethical in therapy and need to be managed by the therapist.
Psychotherapy approaches for depression US Medical PG Question 3: A mental health volunteer is interviewing locals as part of a community outreach program. A 46-year-old man discloses that he has felt sad for as long as he can remember. He feels as though his life is cursed and if something terrible can happen to him, it usually will. He has difficulty making decisions and feels hopeless. He also feels that he has had worsening suicidal ideations, guilt from past problems, decreased energy, and poor concentration over the past 2 weeks. He is otherwise getting enough sleep and able to hold a job. Which of the following statement best describes this patient's condition?
- A. The patient may have symptoms of mania or psychosis.
- B. The patient is likely to show anhedonia.
- C. The patient likely has paranoid personality disorder.
- D. The patient has double depression. (Correct Answer)
- E. The patient should be started on an SSRI.
Psychotherapy approaches for depression Explanation: ***The patient has double depression.***
- The patient describes **chronic low-grade depressive symptoms** ("felt sad for as long as he can remember," "life is cursed," "difficulty making decisions," "hopeless") consistent with **persistent depressive disorder (dysthymia)**, which requires at least 2 years of symptoms.
- The recent worsening of symptoms over the past two weeks, including "worsening suicidal ideations, guilt from past problems, decreased energy, and poor concentration," indicates an additional **major depressive episode (MDE) superimposed on dysthymia**, a condition known as **double depression**.
- This patient currently meets criteria for both conditions simultaneously, not just at risk for developing them.
*The patient may have symptoms of mania or psychosis.*
- There are no symptoms mentioned that suggest **mania**, such as elevated mood, increased energy, decreased need for sleep, grandiosity, or racing thoughts.
- While suicidal ideation is present, there is no evidence of **psychotic features** like hallucinations or delusions.
*The patient is likely to show anhedonia.*
- **Anhedonia** (inability to feel pleasure) is a common symptom of depression and may well be present in this patient.
- However, the patient's presentation specifically highlights the pattern of **chronic dysthymia with a superimposed major depressive episode**, making **double depression** a more precise, comprehensive, and diagnostically specific description of his current condition.
- While anhedonia might be present, it is a symptom rather than a diagnostic formulation.
*The patient likely has paranoid personality disorder.*
- **Paranoid personality disorder** is characterized by pervasive distrust and suspicion of others, interpreting their motives as malevolent, without sufficient basis.
- The patient's feelings of being "cursed" and that "something terrible can happen" reflect **depressive pessimism and negative cognitive distortions**, not paranoid ideation about others' intentions.
- This is consistent with the hopelessness seen in depression.
*The patient should be started on an SSRI.*
- While an **SSRI (selective serotonin reuptake inhibitor)** combined with psychotherapy would likely be appropriate treatment for double depression, making a specific treatment recommendation is premature without comprehensive clinical assessment.
- The question asks for the **best statement describing the patient's condition** (diagnosis), not for treatment recommendations.
Psychotherapy approaches for depression US Medical PG Question 4: A 10-year-old child is sent to the school psychologist in May because he refuses to comply with the class rules. His teacher says this has been going on since school started back in August. He gets upset at the teacher regularly when he is told to complete a homework assignment in class. Sometimes he refuses to complete them altogether. Several of his teachers have reported that he intentionally creates noises in class to interrupt the class. He tells the psychologist that the teacher and his classmates are at fault. What is the most appropriate treatment?
- A. Cognitive-behavioral therapy (Correct Answer)
- B. Interpersonal therapy
- C. Administration of lithium
- D. Motivational interviewing
- E. Administration of clozapine
Psychotherapy approaches for depression Explanation: ***Cognitive-behavioral therapy***
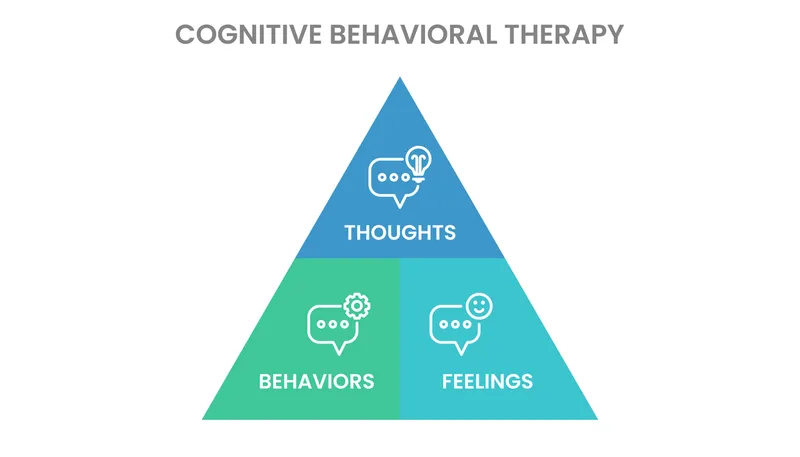
- This child exhibits symptoms consistent with **Oppositional Defiant Disorder (ODD)**, including persistent refusal to comply with rules, anger outbursts, and blaming others. **CBT** is a highly effective treatment for ODD, teaching children coping skills, anger management, and problem-solving.
- CBT helps children identify and change **maladaptive thought patterns** and behaviors, which is crucial for managing the defiant and argumentative behaviors seen in ODD.
*Interpersonal therapy*
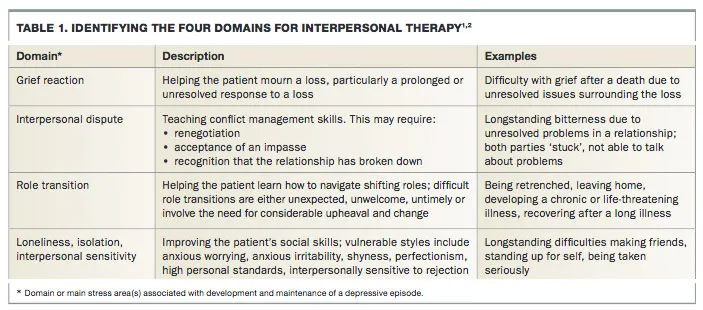
- **Interpersonal therapy (IPT)** primarily focuses on improving interpersonal relationships and communication patterns, often used for depression or eating disorders.
- While improved relationships might be a secondary benefit, IPT does not directly target the core **defiant behaviors** and **anger management** issues central to ODD.
*Administration of lithium*
- **Lithium** is a mood stabilizer primarily used in the treatment of **bipolar disorder** and severe mood dysregulation.
- There is no indication from the provided symptoms (defiance, anger, blaming others) that the child is experiencing a mood disorder that would warrant lithium.
*Motivational interviewing*
- **Motivational interviewing** is a counseling approach that helps individuals resolve ambivalence to change, often used in substance abuse or health behavior change.
- While it can be useful in encouraging willingness to engage in therapy, it is not a direct therapeutic modality for addressing the specific **behavioral challenges** and **underlying cognitive distortions** of ODD.
*Administration of clozapine*
- **Clozapine** is an antipsychotic medication reserved for severe mental illnesses like **treatment-resistant schizophrenia** due to its significant side effects.
- The child's symptoms of defiance and rule-breaking are not indicative of a psychotic disorder requiring antipsychotic medication.
Psychotherapy approaches for depression US Medical PG Question 5: A 20-year-old college student comes to the physician because she has been extremely sad for the past 3 weeks and has to cry constantly. Three weeks ago, her boyfriend left her after they were together for 4 years. She has no appetite and has had a 2.3-kg (5.1-lb) weight loss. She has missed several classes because she could not stop crying or get out of bed. She thinks about her ex-boyfriend all the time. She says that she experienced similar symptoms for about 2 months after previous relationships ended. The patient is 158 cm (5 ft 2 in) tall and weighs 45 kg (100 lb); BMI is 18 kg/m2. Her temperature is 36.1°C (97°F), pulse is 65/min, and blood pressure is 110/60 mm Hg. Physical examination shows no abnormalities. On mental status examination she appears sad and cries easily. Which of the following is the most likely diagnosis?
- A. Bereavement
- B. Anorexia nervosa
- C. Major depressive disorder
- D. Acute stress disorder
- E. Adjustment disorder with depressed mood (Correct Answer)
Psychotherapy approaches for depression Explanation: ***Adjustment disorder with depressed mood***
- This diagnosis is most likely as the patient’s symptoms (sadness, crying, loss of appetite, weight loss, difficulty getting out of bed) developed in response to an **identifiable stressor** (breakup with boyfriend) and occurred within **3 months** of its onset.
- The patient's history of similar, time-limited reactions to previous relationship endings supports an adjustment disorder pattern, where symptoms are **maladaptive** but resolve once the stressor is removed or a new level of adaptation is achieved, making it distinct from major depression due to its direct and timely link to a stressor.
*Bereavement*
- Bereavement involves the natural and expected emotional responses to the **death of a loved one**, which is not the case here as her boyfriend left her.
- While symptoms can overlap with depression, the precipitating event (death vs. breakup) distinguishes it from adjustment disorder.
*Anorexia nervosa*
- Anorexia nervosa is characterized by an **intense fear of gaining weight** or becoming fat, a distorted body image, and a persistent restriction of energy intake leading to a significantly low body weight.
- The patient's weight loss and poor appetite are attributed to her sadness and crying spells following a breakup, not primarily driven by a desire to be thin or body image preoccupation.
*Major depressive disorder*
- Major depressive disorder requires symptoms to be present for **at least 2 weeks** and significantly impair functioning, but the key differentiator here is the **clear and recent precipitating stressor** (breakup) and the history of similar, time-limited responses to past relationship endings.
- While the symptoms are severe, they are directly and clearly linked to the stressor, and the patient's pattern of response suggests an adjustment disorder rather than an endogenous depressive episode.
*Acute stress disorder*
- Acute stress disorder occurs in response to exposure to actual or threatened **death, serious injury, or sexual violence**, either directly or indirectly.
- The patient's stressor (a breakup) does not meet the criteria for a traumatic event required for acute stress disorder.
Psychotherapy approaches for depression US Medical PG Question 6: A 40-year-old woman comes to the therapist for weekly psychotherapy. She was diagnosed with major depressive disorder and anxiety after her divorce 1 year ago. During last week's appointment, she spoke about her ex-husband's timidity and lack of advancement at work; despite her urging, he never asked for a raise. Today, when the therapist asks how she is doing, she replies, “If there's something you want to know, have the courage to ask me! I have no respect for a man who won't speak his mind!” The patient's behavior can be best described as an instance of which of the following?
- A. Passive aggression
- B. Displacement
- C. Projection
- D. Reaction formation
- E. Transference (Correct Answer)
Psychotherapy approaches for depression Explanation: ***Transference***
- **Transference** occurs when a patient unconsciously redirects feelings and attitudes from a past significant relationship (e.g., with a parent or ex-spouse) onto the therapist.
- The patient is treating the therapist as if he were her ex-husband, reacting to the therapist with the same frustration and criticism she felt toward her ex-husband's perceived timidity and lack of assertiveness.
- This emotional re-enactment of past relationship dynamics with the therapist is the hallmark of transference in psychotherapy.
*Passive aggression*
- **Passive aggression** involves indirect resistance to the demands of others and an avoidance of direct confrontation.
- The patient's statement is a direct and confrontational expression of her feelings, not an indirect form of resistance.
*Displacement*
- **Displacement** is a defense mechanism where undesired feelings or impulses are directed from a threatening target to a safer, less threatening one.
- While feelings are being redirected, the core issue is the patient's emotional re-enactment of past relationship dynamics with the therapist, which is more characteristic of transference than simple displacement.
*Projection*
- **Projection** is a defense mechanism where an individual attributes their own unacceptable thoughts, feelings, or impulses to another person.
- The patient is not attributing her own unacknowledged timidity or lack of assertiveness to the therapist; rather, she is reacting to the therapist as if the therapist were her ex-husband.
*Reaction formation*
- **Reaction formation** is a defense mechanism in which a person represses unacceptable thoughts or feelings and outwardly expresses the opposite.
- There is no indication that the patient is repressing certain feelings and acting in an opposing manner; her statement directly reflects her underlying frustration.
Psychotherapy approaches for depression US Medical PG Question 7: A 35-year-old man comes to the Veterans Affairs hospital because of a 2-month history of anxiety. He recently returned from his third deployment to Iraq, where he served as a combat medic. He has had difficulty readjusting to civilian life. He works as a taxi driver but had to take a leave of absence because of difficulties with driving. Last week, he hit a stop sign because he swerved out of the way of a grocery bag that was in the street. He has difficulty sleeping because of nightmares about the deaths of some of the other soldiers in his unit and states, “it's my fault, I could have saved them. Please help me.” Mental status examination shows a depressed mood and a restricted affect. There is no evidence of suicidal ideation. Which of the following is the most appropriate initial step in treatment?
- A. Dialectical behavioral therapy
- B. Venlafaxine therapy
- C. Cognitive behavioral therapy (Correct Answer)
- D. Motivational interviewing
- E. Prazosin therapy
Psychotherapy approaches for depression Explanation: ***Cognitive behavioral therapy***
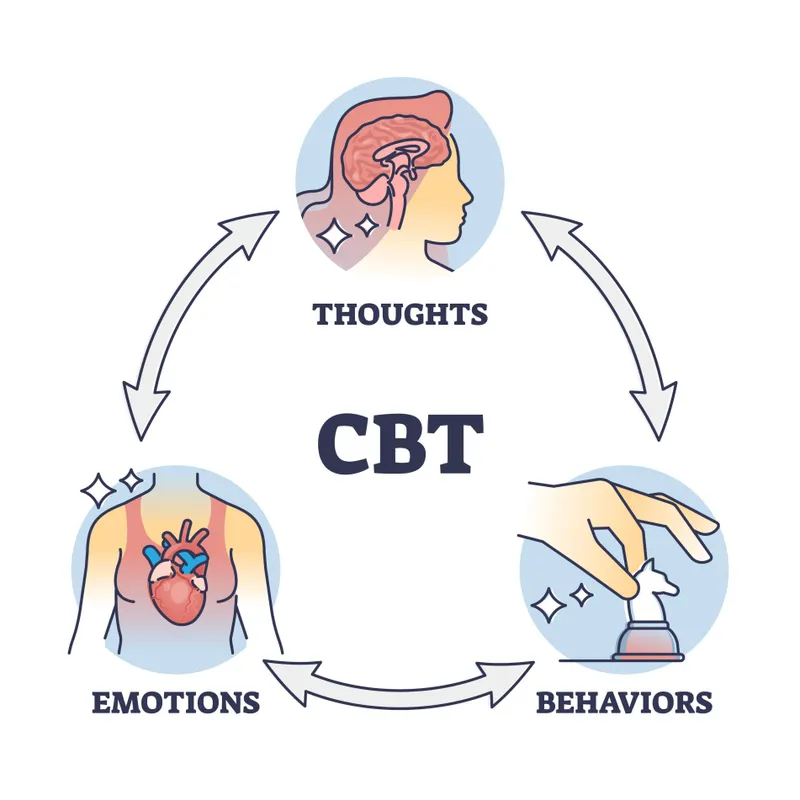
- **Cognitive Behavioral Therapy (CBT)** is considered a first-line psychological treatment for **Post-Traumatic Stress Disorder (PTSD)**, which the patient's symptoms (deployments, intrusive thoughts, nightmares, avoidance, guilt) strongly suggest.
- CBT helps individuals identify and challenge **maladaptive thought patterns** and behaviors related to the trauma, fostering new coping mechanisms.
*Dialectical behavioral therapy*
- **Dialectical Behavioral Therapy (DBT)** is primarily used for individuals with **Borderline Personality Disorder** or severe emotional dysregulation.
- While it can help with emotional regulation, it is not the **first-line therapy** specifically targeting trauma-related cognitive distortions and avoidance behaviors seen in PTSD.
*Venlafaxine therapy*
- **Venlafaxine**, an SNRI, is an antidepressant that can be effective for PTSD symptoms. However, current guidelines recommend **psychotherapy (like CBT)** as the initial step, especially when feasible.
- While pharmacotherapy can be used, it's typically considered **adjunctive** or for cases where psychotherapy alone is insufficient or not preferred.
*Motivational interviewing*
- **Motivational interviewing** is a patient-centered counseling style used to address ambivalence and enhance a person's **intrinsic motivation** for change.
- It is often utilized in substance abuse treatment or when patients are resistant to treatment, but it is not a primary, standalone treatment for the core symptoms of PTSD.
*Prazosin therapy*
- **Prazosin** is an alpha-1 antagonist used off-label to treat **PTSD-related nightmares** and sleep disturbances.
- While it can be helpful for a specific symptom, it does not address the broader spectrum of PTSD symptoms, such as intrusive thoughts, avoidance, or negative cognitions.
Psychotherapy approaches for depression US Medical PG Question 8: A 20-year-old man comes to the physician because of decreasing academic performance at his college for the past 6 months. He reports a persistent fear of “catching germs” from his fellow students and of contracting a deadly disease. He finds it increasingly difficult to attend classes. He avoids handshakes and close contact with other people. He states that when he tries to think of something else, the fears “keep returning” and that he has to wash himself for at least an hour when he returns home after going outside. Afterwards he cleans the shower and has to apply disinfectant to his body and to the bathroom. He does not drink alcohol. He used to smoke cannabis but stopped one year ago. His vital signs are within normal limits. He appears anxious. On mental status examination, he is oriented to person, place, and time. In addition to starting an SSRI, which of the following is the most appropriate next step in management?
- A. Cognitive-behavioral therapy (Correct Answer)
- B. Psychodynamic psychotherapy
- C. Motivational interviewing
- D. Interpersonal therapy
- E. Group therapy
Psychotherapy approaches for depression Explanation: **Cognitive-behavioral therapy**
- **Cognitive-behavioral therapy (CBT)**, specifically **Exposure and Response Prevention (ERP)**, is the most effective psychotherapy for **obsessive-compulsive disorder (OCD)**, which this patient's symptoms strongly suggest.
- CBT helps patients challenge distorted thoughts and gradually expose themselves to feared situations while preventing compulsive rituals, thus breaking the cycle of obsessions and compulsions.
*Psychodynamic psychotherapy*
- This therapy focuses on **unconscious conflicts** and **past experiences** to understand current symptoms.
- While it can be helpful for some mental health conditions, it is generally **less effective** than CBT for the specific, highly ritualized symptoms of OCD.
*Motivational interviewing*
- **Motivational interviewing** is a patient-centered counseling style designed to address **ambivalence about change** and enhance intrinsic motivation.
- It is often used in substance abuse or lifestyle changes, but it does not directly teach coping skills for OCD symptoms or address the underlying thought patterns.
*Interpersonal therapy*
- **Interpersonal therapy (IPT)** focuses on the patient's **current interpersonal relationships** and social functioning.
- While social difficulties can arise from OCD, IPT does not directly target the obsessions and compulsions that are central to the disorder.
*Group therapy*
- **Group therapy** can provide support and a sense of community, but for a severe condition like OCD, **individual therapy** (especially CBT/ERP) is typically recommended first due to the highly individualized nature of obsessions and compulsions.
- It may be a complementary approach, but usually not the most appropriate initial next step given the intensity of the patient's symptoms.
Psychotherapy approaches for depression US Medical PG Question 9: A 25-year-old woman is brought to the emergency department by EMS after being found naked in a busy downtown square. The patient stated that she is liberating people from material desires and was found destroying objects. Her temperature is 99.5°F (37.5°C), blood pressure is 127/68 mmHg, pulse is 120/min, respirations are 22/min, and oxygen saturation is 98% on room air. Physical exam is deferred due to patient combativeness. The patient is given diphenhydramine and haloperidol and transferred to the psychiatric ward. On day 1 on the ward, the patient is no longer aggressive or agitated and has calmed down. She states that she feels severely depressed and wants to kill herself. The patient is started on a medication and monitored closely. On day 3 of the patient's stay in the hospital she is found in her room drawing up plans and states that she has major plans to revamp the current energy problems in the country. Which of the following is the most likely medication that was started in this patient?
- A. Quetiapine
- B. Olanzapine
- C. Lamotrigine
- D. Sertraline (Correct Answer)
- E. Lithium
Psychotherapy approaches for depression Explanation: ***Sertraline***
- This patient exhibits classic **bipolar I disorder** with rapid mood cycling from **mania** (naked in public, grandiose delusions, destroying objects) to **severe depression** (suicidal ideation on Day 1) and back to **mania** (grandiose plans on Day 3).
- The key clinical clue is the **rapid return to mania by Day 3** after starting medication during the depressive phase. This suggests **antidepressant-induced mania/mood switch**, a well-known complication of using **SSRI antidepressants** (like sertraline) **without adequate mood stabilization** in bipolar disorder.
- **Antidepressants can precipitate manic episodes** within days in bipolar patients, which is why they should be avoided or used only with concomitant mood stabilizers. This question tests recognition of this critical psychiatric principle.
*Lithium*
- Lithium is a first-line **mood stabilizer** for bipolar disorder and would be appropriate for long-term management. However, lithium **prevents manic episodes** rather than causing them.
- Lithium takes **1-2 weeks to reach therapeutic levels**, so it would not explain the rapid mood switch to mania by Day 3. If lithium had been started, we would expect **stabilization or improvement**, not a return to mania.
*Quetiapine*
- Quetiapine is an **atypical antipsychotic** effective for both acute mania and bipolar depression. It can provide rapid mood stabilization.
- If quetiapine was started on Day 1, we would expect **mood stabilization or sedation**, not a switch back to mania. Quetiapine does **not precipitate manic episodes**.
*Olanzapine*
- Olanzapine is another **atypical antipsychotic** used for acute mania and maintenance in bipolar disorder.
- Like quetiapine, olanzapine would **stabilize mood** and reduce manic symptoms, not trigger them. It would not explain the return to mania on Day 3.
*Lamotrigine*
- Lamotrigine is a mood stabilizer particularly effective for **preventing depressive episodes** in bipolar disorder, though less effective for acute mania.
- Lamotrigine **does not precipitate manic episodes** and takes weeks to titrate to therapeutic doses due to risk of Stevens-Johnson syndrome. It would not explain the rapid mood switch observed here.
Psychotherapy approaches for depression US Medical PG Question 10: Ten days after the vaginal delivery of a healthy infant girl, a 27-year-old woman is brought to the physician by her husband because of frequent mood changes. She has been tearful and anxious since she went home from the hospital 2 days after delivery. She says that she feels overwhelmed with her new responsibilities and has difficulties taking care of her newborn because she feels constantly tired. She only sleeps for 2 to 3 hours nightly because the baby “is keeping her awake.” Sometimes, the patient checks on her daughter because she thinks she heard her cry but finds her sleeping quietly. Her husband says that she is afraid that something could happen to the baby. She often gets angry at him and has yelled at him when he picks up the baby without using a hand sanitizer beforehand. She breastfeeds the baby without any problems. The patient's mother has bipolar disorder with psychotic features. The patient's vital signs are within normal limits. Physical examination shows an involuting uterus consistent in size with her postpartum date. Mental status examination shows a labile affect with no evidence of homicidal or suicidal ideation. Laboratory studies show a hemoglobin concentration of 13 g/dL and a thyroid-stimulating hormone level of 3.1 μU/mL. Which of the following is the most appropriate next step in management?
- A. Risperidone therapy
- B. Bupropion therapy
- C. Cognitive behavioral therapy
- D. Reassurance (Correct Answer)
- E. Sertraline therapy
Psychotherapy approaches for depression Explanation: ***Reassurance***
- The patient exhibits symptoms of **"baby blues"**, including tearfulness, anxiety, mood swings, and feeling overwhelmed, which are common within the first two weeks postpartum and typically resolve spontaneously.
- Given the transient nature of **baby blues** and the absence of more severe symptoms like psychosis or significant functional impairment, **reassurance** and supportive care are the most appropriate initial steps.
*Risperidone therapy*
- **Risperidone** is an **antipsychotic** medication used for conditions like psychosis or severe mood disorders, which are not present in this patient's mild, transient symptoms of baby blues.
- Initiating antipsychotic therapy for **self-limiting baby blues** is unnecessary and could lead to unwanted side effects.
*Bupropion therapy*
- **Bupropion** is an **antidepressant** primarily used for major depressive disorder and seasonal affective disorder, and is not indicated for the mild, transient symptoms of **baby blues**.
- Its mechanism of action involves dopamine and norepinephrine reuptake inhibition, differing from typical SSRIs often considered for postpartum depression.
*Cognitive behavioral therapy*
- While **CBT** is an effective treatment for **postpartum depression** and anxiety disorders, the patient's symptoms are consistent with **baby blues**, which are self-limiting and resolve with supportive care in most cases.
- CBT would be more appropriate if the symptoms were severe, persistent beyond two weeks, or indicative of a more significant mood disorder.
*Sertraline therapy*
- **Sertraline** is an **SSRI antidepressant** commonly used for **postpartum depression** and anxiety, but it is not indicated for the transient and mild symptoms of **baby blues**.
- Antidepressants are typically reserved for more severe and persistent symptoms characteristic of postpartum depression, which usually lasts longer than two weeks.
More Psychotherapy approaches for depression US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.