Pharmacotherapy for depression US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pharmacotherapy for depression. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pharmacotherapy for depression US Medical PG Question 1: A 27-year-old woman presents to the psychiatrist due to feelings of sadness for the past 3 weeks. She was let go from her job 1 month ago, and she feels as though her whole life is coming to an end. She is unable to sleep well at night and also finds herself crying at times during the day. She has not been able to eat well and has been losing weight as a result. She has no will to go out and meet with her friends, who have been extremely supportive during this time. Her doctor gives her an antidepressant which blocks the reuptake of both serotonin and norepinephrine to help with these symptoms. One week later, she is brought to the emergency room by her friends who say that she was found to be in a state of euphoria. They mention bizarre behavior, one of which is booking a plane ticket to New York, even though she has 3 interviews lined up the same week. Her words cannot be understood as she is speaking very fast, and she is unable to sit in one place for the examination. Which of the following was most likely prescribed by her psychiatrist?
- A. Bupropion
- B. Venlafaxine (Correct Answer)
- C. Sertraline
- D. Fluvoxamine
- E. Lithium
Pharmacotherapy for depression Explanation: ***Venlafaxine***
- The patient's presentation of depression followed by a rapid shift to **euphoria**, **bizarre behavior**, **rapid speech**, and **psychomotor agitation** after starting an antidepressant strongly suggests **antidepressant-induced mania**.
- This response is characteristic of an underlying **bipolar disorder** unmasked by an antidepressant, particularly a **serotonin-norepinephrine reuptake inhibitor (SNRI)** like venlafaxine.
*Bupropion*
- Bupropion is a **norepinephrine-dopamine reuptake inhibitor (NDRI)**, not an SNRI, and is less commonly associated with inducing mania compared to SNRIs or SSRIs in vulnerable individuals.
- While it can be activating, its specific mechanism primarily targets dopamine and norepinephrine, with less direct serotonin reuptake blockade.
*Sertraline*
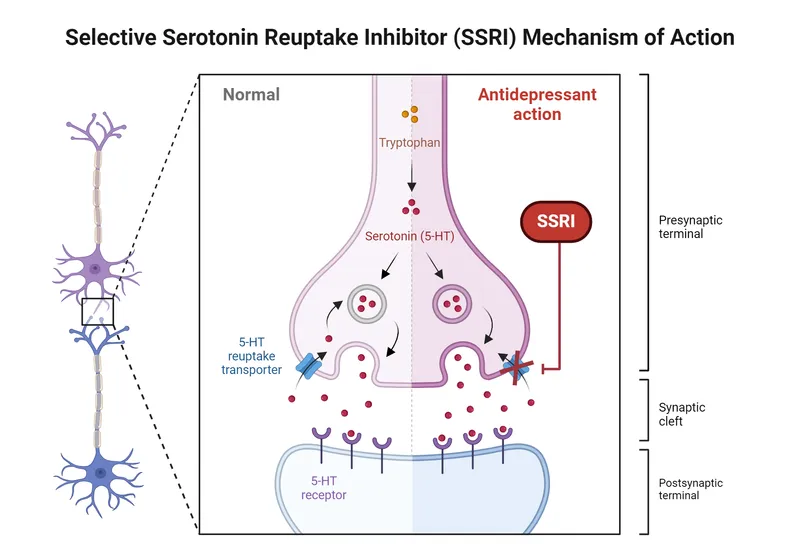
- Sertraline is a **selective serotonin reuptake inhibitor (SSRI)**, which primarily blocks serotonin reuptake.
- While SSRIs can induce mania in patients with undiagnosed bipolar disorder, the question specifically states the doctor prescribed an antidepressant that blocks the reuptake of **both serotonin and norepinephrine**.
*Fluvoxamine*
- Fluvoxamine is also a **selective serotonin reuptake inhibitor (SSRI)**, primarily targeting serotonin, not both serotonin and norepinephrine.
- As with other SSRIs, it can induce manic episodes in vulnerable individuals, but it does not fit the description of the prescribed drug's mechanism of action.
*Lithium*
- Lithium is a **mood stabilizer** primarily used for the treatment of bipolar disorder and prevention of manic/depressive episodes, not an antidepressant.
- It would be contraindicated as a first-line treatment for what initially presented as unipolar depression and is used to *treat* rather than *induce* mania.
Pharmacotherapy for depression US Medical PG Question 2: A 25-year-old woman presents to her college campus clinic with the complaint of being unable to get up for her morning classes. She says that, because of this, her grades are being affected. For the past 6 weeks, she says she has been feeling depressed because her boyfriend dumped her. She finds herself very sleepy, sleeping in most mornings, eating more snacks and fast foods, and feeling drained of energy. She is comforted by her friend’s efforts to cheer her up but still feels guarded around any other boy that shows interest in her. The patient says she had similar symptoms 7 years ago for which she was prescribed several selective serotonin reuptake inhibitors (SSRIs) and a tricyclic antidepressant (TCA). However, none of the medications provided any long-term relief. She has prescribed a trial of Phenelzine to treat her symptoms. Past medical history is significant for a long-standing seizure disorder well managed with phenytoin. Which of the following statements would most likely be relevant to this patient’s new medication?
- A. “This medication is known to cause anorgasmia during treatment.”
- B. “You will have a risk for cardiotoxicity from this medication.”
- C. “A common side effect of this medication is sedation.”
- D. “While taking this medication, you should avoid drinking red wine.” (Correct Answer)
- E. “While on this medication, you may have a decreased seizure threshold.”
Pharmacotherapy for depression Explanation: ***"While taking this medication, you should avoid drinking red wine."***
- Phenelzine is a **monoamine oxidase inhibitor (MAOI)**. MAOIs inhibit the breakdown of **tyramine**, an amine found in fermented foods like red wine, aged cheeses, cured meats, and pickled foods.
- Consuming tyramine-rich foods with an MAOI can lead to a **hypertensive crisis**, characterized by a sudden, severe increase in blood pressure which can cause headaches, palpitations, and potentially stroke.
- This dietary counseling is **essential and immediately actionable** patient education when starting an MAOI.
*"This medication is known to cause anorgasmia during treatment."*
- While sexual dysfunction can occur with many antidepressants, **anorgasmia** is much more common and severe with **SSRIs (Selective Serotonin Reuptake Inhibitors)** than with MAOIs.
- MAOIs like phenelzine have a different mechanism of action and generally have a lower incidence of sexual side effects compared to SSRIs.
*"You will have a risk for cardiotoxicity from this medication."*
- **Cardiotoxicity** is a significant concern with **tricyclic antidepressants (TCAs)**, especially in overdose, due to their effects on cardiac sodium channels and potential for arrhythmias.
- While MAOIs can cause **orthostatic hypotension**, direct cardiotoxicity is not a primary concern with phenelzine.
*"A common side effect of this medication is sedation."*
- Phenelzine is generally considered **activating** rather than sedating, and can sometimes lead to insomnia or agitation.
- The patient's current hypersomnia is a symptom of her **atypical depression**, not a predicted side effect of phenelzine. In fact, phenelzine may help improve this symptom.
*"While on this medication, you may have a decreased seizure threshold."*
- This statement is actually **medically accurate** - MAOIs including phenelzine can lower (decrease) the seizure threshold, meaning they increase seizure risk.
- This is relevant given the patient's seizure disorder managed with phenytoin and warrants monitoring.
- However, the **dietary tyramine restriction** is the more critical and immediately actionable counseling point when initiating MAOI therapy, as hypertensive crisis can occur with the very first exposure to tyramine-rich foods.
Pharmacotherapy for depression US Medical PG Question 3: A 24-year-old male comes into the psychiatric clinic complaining of consistent sadness. He endorses feelings of worthlessness, anxiety, and anhedonia for the past couple months but denies feeling suicidal. He further denies any past episodes of feeling overly energetic with racing thoughts. Confident of the diagnosis, you recommend frequent talk therapy along with a long-term prescription of a known first-line medication for this disorder. What is the drug and what are some of the most frequently encountered side effects?
- A. Selective serotonin reuptake inhibitor; hypomania, suicidal thoughts
- B. Tricyclic antidepressants; hypomania, suicidal thoughts
- C. Selective serotonin reuptake inhibitor; anorgasmia, insomnia (Correct Answer)
- D. Monoamine oxidase inhibitors; Orthostatic hypotension, weight gain
- E. Tricyclic antidepressants; Orthostatic hypotension, anticholinergic effects
Pharmacotherapy for depression Explanation: ***Selective serotonin reuptake inhibitor; anorgasmia, insomnia***
- The patient presents with classic symptoms of **major depressive disorder**, including persistent sadness, worthlessness, anxiety, and anhedonia, without any history of manic or hypomanic episodes. **SSRIs** are considered first-line pharmacotherapy for this condition.
- Common side effects of SSRIs include **sexual dysfunction** (e.g., anorgasmia, decreased libido) and **insomnia** or agitation, especially during the initial weeks of treatment.
*Selective serotonin reuptake inhibitor; hypomania, suicidal thoughts*
- While SSRIs are the correct drug class, **hypomania** is not a frequent side effect in patients without bipolar disorder. For patients with bipolar disorder, antidepressant monotherapy can induce hypomania or mania, but this patient denies such episodes.
- **Suicidal thoughts** can occur, particularly in young adults, during the initial phase of antidepressant treatment, but it is less common to frame it as a *frequently encountered side effect* in the general population compared to sexual dysfunction or sleep disturbances.
*Tricyclic antidepressants; hypomania, suicidal thoughts*
- **Tricyclic antidepressants (TCAs)** are generally not first-line due to their less favorable side effect profile compared to SSRIs, including significant anticholinergic effects and cardiovascular risks.
- As with SSRIs, **hypomania** is not a typical frequent side effect in unipolar depression, and while **suicidal thoughts** are a concern with antidepressants, TCAs carry a higher risk of lethality in overdose, making them less preferred initially.
*Monoamine oxidase inhibitors; Orthostatic hypotension, weight gain*
- **Monoamine oxidase inhibitors (MAOIs)** are effective but are typically reserved for **refractory depression** due to their significant drug and food interactions (e.g., tyramine-induced hypertensive crisis).
- While **orthostatic hypotension** and **weight gain** are known side effects of MAOIs, this class is not considered a first-line treatment for major depressive disorder.
*Tricyclic antidepressants; Orthostatic hypotension, anticholinergic effects*
- **TCAs** are indeed associated with side effects such as **orthostatic hypotension** and prominent **anticholinergic effects** (e.g., dry mouth, constipation, blurred vision, urinary retention).
- However, because of these more burdensome side effects and higher toxicity in overdose, TCAs are not generally considered the first-line medication choice, especially when SSRIs are available and safer.
Pharmacotherapy for depression US Medical PG Question 4: A 32-year-old man comes to the physician because of generalized fatigue for the past 4 months. He also has difficulty sleeping and concentrating. He says he does not enjoy his hobbies anymore and has stopped attending family events. Mental status examination shows psychomotor retardation and a flat affect along with some evidence of suicidal ideation. His speech is slow in rate and monotone in rhythm. Treatment with fluoxetine is initiated. One month later, he reports significant improvement in his motivation and mood but also delayed ejaculation and occasional anorgasmia. The physician decides to replace his current medication with another agent. It is most appropriate to switch the patient to which of the following drugs?
- A. Venlafaxine
- B. Trazodone
- C. Citalopram
- D. Tranylcypromine
- E. Bupropion (Correct Answer)
Pharmacotherapy for depression Explanation: ***Bupropion***
- Bupropion is a **norepinephrine-dopamine reuptake inhibitor** that is associated with a **lower incidence of sexual side effects** compared to SSRIs.
- It would be an appropriate switch for a patient experiencing sexual dysfunction (delayed ejaculation, anorgasmia) secondary to fluoxetine, while still effectively treating depression.
*Venlafaxine*
- Venlafaxine is a **serotonin-norepinephrine reuptake inhibitor (SNRI)**, and like SSRIs, it can also cause **sexual dysfunction** due to its serotonergic activity.
- Switching to venlafaxine would likely not resolve the patient's sexual side effects and might even worsen them.
*Trazodone*
- Trazodone is primarily used off-label for **insomnia** at low doses due to its strong **sedating effects** and antagonism of various receptors (e.g., histamine, alpha-1 adrenergic, serotonin 5-HT2A/C).
- While it has a lower risk of sexual dysfunction than SSRIs, its antidepressant efficacy as monotherapy for major depression is generally considered **weaker** than other first-line options, and its sedating profile might not be ideal given the patient's existing fatigue.
*Citalopram*
- Citalopram is an **SSRI** and belongs to the same class as fluoxetine, sharing similar mechanisms of action and side effect profiles.
- Switching to another SSRI like citalopram would likely result in persistent or similar **sexual dysfunction**, as this is a common class effect of SSRIs.
*Tranylcypromine*
- Tranylcypromine is a **monoamine oxidase inhibitor (MAOI)**, a class of antidepressants typically reserved for **refractory depression** due to their significant drug-drug and food-drug interactions.
- While MAOIs can be effective, they are associated with a much **higher risk of adverse effects** (e.g., hypertensive crisis with tyramine-rich foods) and are generally not a first-line alternative after intolerance to an SSRI, especially when the current issue is sexual dysfunction.
Pharmacotherapy for depression US Medical PG Question 5: A 26-year-old man being treated for major depressive disorder returns to his psychiatrist complaining that he has grown weary of the sexual side effects. Which other medication used to treat major depressive disorder may be appropriate as a stand-alone or add-on therapy?
- A. Venlafaxine
- B. Cyproheptadine
- C. Aripiprazole
- D. Bupropion (Correct Answer)
- E. Paroxetine
Pharmacotherapy for depression Explanation: ***Bupropion***
- **Bupropion** is an antidepressant that works via **norepinephrine-dopamine reuptake inhibition**, and unlike most common antidepressants, it is **not associated with sexual dysfunction**.
- It can be used as a **stand-alone treatment** or as an **add-on therapy** to counteract sexual side effects from other antidepressants like SSRIs.
- This makes it the ideal choice for this patient.
*Venlafaxine*
- **Venlafaxine** is a **serotonin-norepinephrine reuptake inhibitor (SNRI)**, and like SSRIs, it can cause or worsen **sexual dysfunction**.
- It is unlikely to resolve the patient's complaint of sexual side effects.
*Cyproheptadine*
- **Cyproheptadine** is an **antihistamine** with **serotonin antagonist** properties that is sometimes used **off-label to treat SSRI-induced sexual dysfunction**.
- However, it is **not an antidepressant** itself and therefore would not be appropriate as a **stand-alone therapy** for major depressive disorder.
- The question specifically asks for "medication used to treat major depressive disorder," which excludes cyproheptadine despite its utility for sexual side effects.
*Aripiprazole*
- **Aripiprazole** is an **atypical antipsychotic** that is approved as an **adjunctive treatment** for major depressive disorder.
- While it can be an add-on, it is **not typically used to mitigate sexual side effects** and can sometimes have its own sexual side effects.
*Paroxetine*
- **Paroxetine** is an **SSRI** that is notoriously associated with a **high incidence of sexual side effects**, including decreased libido, delayed orgasm, and anorgasmia.
- Using paroxetine would likely **exacerbate** rather than alleviate the patient's complaint.
Pharmacotherapy for depression US Medical PG Question 6: A 27-year-old man comes to the physician for a follow-up examination. Paroxetine therapy was initiated 6 weeks ago for a major depressive episode. He now feels much better and says he is delighted with his newfound energy. He gets around 8 hours of sleep nightly. His appetite has increased. Last year, he had two episodes of depressed mood, insomnia, and low energy during which he had interrupted his job training and stopped going to the gym. Now, he has been able to resume his job at a local bank. He also goes to the gym three times a week to work out and enjoys reading books again. His temperature is 36.5°C (97.7°F), pulse is 70/min, and blood pressure is 128/66 mm Hg. Physical and neurologic examinations show no abnormalities. On mental status examination, he describes his mood as "good." Which of the following is the most appropriate next step in management?
- A. Discontinue paroxetine
- B. Switch from paroxetine to venlafaxine therapy
- C. Continue paroxetine therapy for 6 months
- D. Continue paroxetine therapy for 2 years (Correct Answer)
- E. Switch from paroxetine to lithium therapy
Pharmacotherapy for depression Explanation: **Continue paroxetine therapy for 2 years**
- This patient has experienced **recurrent major depressive episodes**, with two episodes in the past year. Guidelines recommend continuing antidepressant therapy for **1-3 years or indefinitely** after a second or third episode to prevent relapse.
- Given his significant improvement and history of recurrent depression, long-term maintenance with paroxetine is the most appropriate strategy.
*Discontinue paroxetine*
- Discontinuing the antidepressant now would significantly increase the risk of a rapid **relapse** of major depressive disorder, especially given his history of multiple episodes.
- Antidepressants should not be abruptly stopped once symptoms resolve, particularly in patients with recurrent depression.
*Switch from paroxetine to venlafaxine therapy*
- There is no indication to switch to venlafaxine, as the patient has responded well to paroxetine and is currently in **remission**.
- Switching medications carries the risk of new side effects or a recurrence of depressive symptoms.
*Continue paroxetine therapy for 6 months*
- While 6 months of continuation therapy is standard after a **first episode** of major depressive disorder, it is insufficient for patients with **recurrent episodes**.
- Continuing for only 6 months heightens the risk of relapse for this patient given his history.
*Switch from paroxetine to lithium therapy*
- Lithium is typically used as a mood stabilizer for **bipolar disorder** or as an augmentation strategy for refractory depression.
- There is no evidence in the vignette to suggest bipolar disorder, and the patient has responded well to monotherapy with paroxetine.
Pharmacotherapy for depression US Medical PG Question 7: A 35-year-old banker is brought to a medical clinic by his concerned wife. For the past 3 weeks, he has not been eating well and has had a 10 kg (22 lb) weight loss. He wakes up very early in the mornings and feels extremely despondent. He no longer goes out on the weekends to hang out with his close friends nor does he go on date nights with his wife. He feels guilty for letting his friends and family down recently. He additionally has a history of fibromyalgia and deals with daily pain. What would be the most appropriate treatment plan for this patient?
- A. Amitriptyline
- B. Phenelzine
- C. Venlafaxine (Correct Answer)
- D. Electroconvulsive therapy
- E. Fluoxetine
Pharmacotherapy for depression Explanation: ***Venlafaxine***
- This patient presents with symptoms highly suggestive of **major depressive disorder**, including **anhedonia**, significant **weight loss**, **early morning awakening**, and **feelings of guilt**. His co-occurring **fibromyalgia** makes a **serotonin-norepinephrine reuptake inhibitor (SNRI)** like venlafaxine an excellent choice.
- SNRIs are effective for both depression and chronic pain conditions such as fibromyalgia, as they modulate both **serotonin** and **norepinephrine** pathways, which are implicated in both mood and pain perception.
*Amitriptyline*
- **Amitriptyline** is a **tricyclic antidepressant (TCA)** that can be used for both depression and chronic pain, including fibromyalgia.
- However, TCAs generally have a less favorable side effect profile (e.g., **anticholinergic effects**, **cardiac toxicity in overdose**) compared to SNRIs and SSRIs, making them less of a first-line choice unless other options fail or specific indications are present.
*Phenelzine*
- **Phenelzine** is a **monoamine oxidase inhibitor (MAOI)**, typically reserved for **atypical depression** or treatment-resistant depression due to its significant **food and drug interactions** (e.g., **hypertensive crisis** with tyramine-rich foods or sympathomimetics).
- Given this is likely a first-line treatment scenario, an MAOI would not be the most appropriate initial choice.
*Electroconvulsive therapy*
- **Electroconvulsive therapy (ECT)** is a highly effective treatment for severe depression, especially with **psychotic features**, **catatonia**, or **severe suicidality**, or in cases of **treatment resistance** where other modalities have failed.
- While the patient has significant symptoms of depression, there is no indication of immediate life-threatening severity (e.g., active suicidal intent with a plan) or treatment resistance to warrant ECT as a first-line option.
*Fluoxetine*
- **Fluoxetine** is a **selective serotonin reuptake inhibitor (SSRI)** and a common first-line treatment for major depressive disorder.
- While it would be effective for the patient's depression, it does not offer the additional specific benefit for **fibromyalgia pain** that an SNRI like venlafaxine provides through dual serotonin and norepinephrine reuptake inhibition.
Pharmacotherapy for depression US Medical PG Question 8: A 17-year-old white female with a history of depression is brought to your office by her parents because they are concerned that she is acting differently. She is quiet and denies any changes in her personality or drug use. After the parents step out so that you can speak alone, she begins crying. She states that school has been very difficult and has been very depressed for the past 2 months. She feels a lot of pressure from her parents and coaches and says she cannot handle it anymore. She says that she has been cutting her wrists for the past week and is planning to commit suicide. She instantly regrets telling you and begs you not to tell her parents. What is the most appropriate course of action?
- A. Prescribe an anti-depressant medication and allow her to return home
- B. Refer her to a psychiatrist
- C. Explain to her that she will have to be hospitalized as she is an acute threat to herself (Correct Answer)
- D. Tell her parents about the situation and allow them to handle it as a family
- E. Prescribe an anti-psychotic medication
Pharmacotherapy for depression Explanation: ***Explain to her that she will have to be hospitalized as she is an acute threat to herself***
- This patient is actively suicidal and engaging in **self-harm (cutting)**, which represents an immediate and serious risk to her life, necessitating **involuntary hospitalization** for her safety.
- In cases of acute suicidality, the ethical principle of **beneficence** (acting in the patient's best interest) and **non-maleficence** (avoiding harm) overrides confidentiality to ensure the patient's immediate safety.
*Prescribe an anti-depressant medication and allow her to return home*
- While an antidepressant may be part of long-term management, simply prescribing medication and sending her home is **inappropriate and dangerous** given her active suicidal ideation and self-harm.
- Antidepressants can have a delayed onset of action (2-4 weeks) and, in some adolescents, may initially increase the risk of **suicidal thoughts**, making close monitoring essential.
*Refer her to a psychiatrist*
- A referral to a psychiatrist is crucial for comprehensive evaluation and long-term treatment, but it does **not address the immediate danger** presented by her active suicidal plans and self-harm.
- An urgent psychiatric consultation or hospitalization is needed first, with a referral following stabilization.
*Tell her parents about the situation and allow them to handle it as a family*
- While parents must be informed, simply delegating the responsibility to them is **insufficient and potentially negligent** given the patient's acute suicidal risk.
- **Medical professionals** have a duty to ensure the safety of a suicidal minor, which often requires a higher level of intervention than parental supervision alone.
*Prescribe an anti-psychotic medication*
- There is **no indication of psychosis** in this patient's presentation; her symptoms are consistent with severe depression and acute suicidality.
- Prescribing an antipsychotic would be **inappropriate** and could cause unnecessary side effects without addressing the underlying depressive disorder or acute suicidal crisis.
Pharmacotherapy for depression US Medical PG Question 9: A 30-year-old man presents with fatigue and low energy. He says that he has been "feeling down" and tired on most days for the last 3 years. He also says that he has had difficulty concentrating and has been sleeping excessively. The patient denies any manic or hypomanic symptoms. He also denies any suicidal ideation or preoccupation with death. A physical examination is unremarkable. Laboratory findings are significant for the following:
Serum glucose (fasting) 88 mg/dL
Serum electrolytes Sodium 142 mEq/L; Potassium: 3.9 mEq/L; Chloride: 101 mEq/L
Serum creatinine 0.8 mg/dL
Blood urea nitrogen 10 mg/dL
Hemoglobin (Hb %) 15 g/dL
Mean corpuscular volume (MCV) 85 fl
Reticulocyte count 1%
Erythrocyte count 5.1 million/mm3
Thyroid-stimulating hormone 3.5 μU/mL
Medication is prescribed to this patient that increases norepinephrine neurotransmission. After 2 weeks, the patient returns for follow-up and complains of dizziness, dry mouth, and constipation. Which of the following drugs was most likely prescribed to this patient?
- A. Clonidine
- B. Lithium
- C. Paroxetine
- D. Venlafaxine (Correct Answer)
- E. Phenylephrine
Pharmacotherapy for depression Explanation: ***Venlafaxine***
- This patient likely suffers from **persistent depressive disorder (dysthymia)** given the chronic fatigue, low energy, and depressed mood for over 2 years without manic/hypomanic episodes.
- **Venlafaxine** is a **serotonin-norepinephrine reuptake inhibitor (SNRI)** that increases both serotonin and norepinephrine levels by blocking their reuptake at nerve terminals, thereby enhancing norepinephrine neurotransmission.
- Common side effects include **dizziness, dry mouth, and constipation** due to anticholinergic effects and increased noradrenergic activity.
*Clonidine*
- **Clonidine** is an **alpha-2 adrenergic agonist** that reduces sympathetic outflow by activating presynaptic alpha-2 receptors, effectively decreasing norepinephrine release, which is contrary to the question's premise of increasing norepinephrine neurotransmission.
- It is primarily used to treat **hypertension** and **ADHD**, and its side effects can include sedation and dry mouth, but it would not be prescribed to enhance norepinephrine activity.
*Lithium*
- **Lithium** is a mood stabilizer primarily used in the treatment of **bipolar disorder** and is not typically prescribed as a standalone antidepressant to increase norepinephrine neurotransmission.
- Its side effects include **tremor, polyuria, polydipsia, and thyroid dysfunction**, which do not match the described side effect profile.
*Paroxetine*
- **Paroxetine** is a **selective serotonin reuptake inhibitor (SSRI)**, primarily increasing serotonin levels. It does not significantly increase norepinephrine neurotransmission.
- While it can cause side effects like **dry mouth and constipation**, it would not fit the description of a drug that increases norepinephrine neurotransmission.
*Phenylephrine*
- **Phenylephrine** is an **alpha-1 adrenergic agonist** used as a decongestant or to increase blood pressure by directly stimulating postsynaptic alpha-1 receptors rather than enhancing neurotransmission through reuptake inhibition.
- It would not be used to treat depression, and its side effects include **hypertension and reflex bradycardia**, which are not reported in the patient.
Pharmacotherapy for depression US Medical PG Question 10: Benzodiazepines are clinically useful because of their inhibitory effects on the central nervous system. Which of the following correctly pairs the site of action of benzodiazepines with the molecular mechanism by which they exert their effects?
- A. GABA-A receptors; increasing the frequency of activation of a chloride ion channel (Correct Answer)
- B. GABA-B receptors; activating potassium channels
- C. GABA-A receptors; increasing the duration of activation of a chloride ion channel
- D. GABA-A receptors; blocking action of GABA
- E. GABA-B receptors; activating a G-protein coupled receptor
Pharmacotherapy for depression Explanation: ***GABA-A receptors; increasing the frequency of activation of a chloride ion channel***
- Benzodiazepines bind to a specific site on the **GABA-A receptor**, which is a **ligand-gated chloride ion channel**.
- Their binding enhances the effect of GABA by increasing the **frequency of channel opening**, leading to increased chloride influx and neuronal hyperpolarization.
*GABA-B receptors; activating potassium channels*
- Benzodiazepines **do not act on GABA-B receptors**, which are G-protein coupled receptors.
- GABA-B receptor activation typically leads to the activation of **potassium channels** or inhibition of calcium channels, not directly influenced by benzodiazepines.
*GABA-A receptors; increasing the duration of activation of a chloride ion channel*
- This describes the mechanism of action of **barbiturates**, not benzodiazepines.
- Barbiturates increase the **duration of chloride channel opening**, leading to a more pronounced and potentially dangerous central nervous system depression compared to benzodiazepines.
*GABA-A receptors; blocking action of GABA*
- Benzodiazepines are **agonists** (or positive allosteric modulators) of GABA's action, not blockers.
- They enhance, rather than inhibit, the inhibitory effects of GABA.
*GABA-B receptors; activating a G-protein coupled receptor*
- While GABA-B receptors are indeed **G-protein coupled receptors**, benzodiazepines do not exert their effects by activating these receptors.
- Their primary site of action is the **GABA-A receptor**.
More Pharmacotherapy for depression US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.