Neurobiological basis of depression US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neurobiological basis of depression. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neurobiological basis of depression US Medical PG Question 1: A 28-year-old woman presents with depressed mood lasting for most days of the week for the past month. She also mentions that she has lost her appetite for the past 3 weeks. She adds that her job performance has significantly deteriorated because of these symptoms, and she feels like she will have to quit her job soon. Upon asking about her hobbies, she says that she used to enjoy dancing and music but does not have any desire to do them anymore. The patient’s husband says that she has had many sleepless nights last month. The patient denies any history of smoking, alcohol intake, or use of illicit substances. No significant past medical history. Physical examination is unremarkable. Routine laboratory tests are all within normal limits. Which of the following clinical features must be present, in addition to this patient’s current symptoms, to confirm the diagnosis of a major depressive episode?
- A. Intense fear of losing control
- B. Lack of concentration (Correct Answer)
- C. Weight loss
- D. Anterograde amnesia
- E. Nightmares
Neurobiological basis of depression Explanation: ***Lack of concentration***
- The diagnostic criteria for a **major depressive episode** (DSM-5) require at least **5 out of 9 cardinal symptoms** present for at least 2 weeks, with at least one being either **depressed mood** or **anhedonia**.
- This patient currently has **4 symptoms**: (1) depressed mood, (2) anhedonia (loss of interest in dancing/music), (3) appetite disturbance (loss of appetite), and (4) sleep disturbance (insomnia).
- To meet diagnostic criteria, she needs **one more symptom** from the remaining options: fatigue, feelings of worthlessness/guilt, **diminished ability to concentrate or indecisiveness**, psychomotor changes, or suicidal ideation.
- **Lack of concentration** is one of the DSM-5 diagnostic criteria and would bring her total to 5 symptoms, confirming the diagnosis.
*Intense fear of losing control*
- This symptom is characteristic of **panic disorder** or anxiety disorders, where individuals experience sudden, intense episodes of fear with accompanying physical and cognitive symptoms.
- While anxiety can co-occur with depression, intense fear of losing control is **not a DSM-5 diagnostic criterion** for major depressive episode.
*Weight loss*
- The patient already has **loss of appetite**, which satisfies the weight/appetite criterion for major depressive episode.
- **Weight loss and appetite changes are part of the same diagnostic criterion**, not separate ones. Therefore, weight loss would not add an additional criterion to reach the required 5 symptoms.
- While clinically significant weight loss can occur in depression, it would not provide the "additional" criterion needed in this case.
*Anterograde amnesia*
- **Anterograde amnesia** (inability to form new memories) is associated with neurological conditions such as **hippocampal damage**, **Korsakoff syndrome**, or **traumatic brain injury**.
- It is **not a DSM-5 diagnostic criterion** for major depressive episode, though some cognitive impairment (concentration difficulties) may occur.
*Nightmares*
- The patient already has **insomnia** (sleep disturbance), which is one of the DSM-5 diagnostic criteria.
- While nightmares may occur in depression, they are not a separate diagnostic criterion and would not add to the symptom count since sleep disturbance is already present.
Neurobiological basis of depression US Medical PG Question 2: A mental health volunteer is interviewing locals as part of a community outreach program. A 46-year-old man discloses that he has felt sad for as long as he can remember. He feels as though his life is cursed and if something terrible can happen to him, it usually will. He has difficulty making decisions and feels hopeless. He also feels that he has had worsening suicidal ideations, guilt from past problems, decreased energy, and poor concentration over the past 2 weeks. He is otherwise getting enough sleep and able to hold a job. Which of the following statement best describes this patient's condition?
- A. The patient may have symptoms of mania or psychosis.
- B. The patient is likely to show anhedonia.
- C. The patient likely has paranoid personality disorder.
- D. The patient has double depression. (Correct Answer)
- E. The patient should be started on an SSRI.
Neurobiological basis of depression Explanation: ***The patient has double depression.***
- The patient describes **chronic low-grade depressive symptoms** ("felt sad for as long as he can remember," "life is cursed," "difficulty making decisions," "hopeless") consistent with **persistent depressive disorder (dysthymia)**, which requires at least 2 years of symptoms.
- The recent worsening of symptoms over the past two weeks, including "worsening suicidal ideations, guilt from past problems, decreased energy, and poor concentration," indicates an additional **major depressive episode (MDE) superimposed on dysthymia**, a condition known as **double depression**.
- This patient currently meets criteria for both conditions simultaneously, not just at risk for developing them.
*The patient may have symptoms of mania or psychosis.*
- There are no symptoms mentioned that suggest **mania**, such as elevated mood, increased energy, decreased need for sleep, grandiosity, or racing thoughts.
- While suicidal ideation is present, there is no evidence of **psychotic features** like hallucinations or delusions.
*The patient is likely to show anhedonia.*
- **Anhedonia** (inability to feel pleasure) is a common symptom of depression and may well be present in this patient.
- However, the patient's presentation specifically highlights the pattern of **chronic dysthymia with a superimposed major depressive episode**, making **double depression** a more precise, comprehensive, and diagnostically specific description of his current condition.
- While anhedonia might be present, it is a symptom rather than a diagnostic formulation.
*The patient likely has paranoid personality disorder.*
- **Paranoid personality disorder** is characterized by pervasive distrust and suspicion of others, interpreting their motives as malevolent, without sufficient basis.
- The patient's feelings of being "cursed" and that "something terrible can happen" reflect **depressive pessimism and negative cognitive distortions**, not paranoid ideation about others' intentions.
- This is consistent with the hopelessness seen in depression.
*The patient should be started on an SSRI.*
- While an **SSRI (selective serotonin reuptake inhibitor)** combined with psychotherapy would likely be appropriate treatment for double depression, making a specific treatment recommendation is premature without comprehensive clinical assessment.
- The question asks for the **best statement describing the patient's condition** (diagnosis), not for treatment recommendations.
Neurobiological basis of depression US Medical PG Question 3: A 46-year-old male presents with his wife to his primary care provider for depression and strange movements. His wife reports that her husband has not been himself for the last two months. Whereas he was previously outgoing and “the life of the party,” the patient is now irritable and withdrawn. He is a partner at an accounting firm, but his colleagues are threatening his job if he continues to perform poorly at work. The patient cannot explain the recent changes to his mood and tearfully admits he fears there is something seriously wrong with him. His wife says that she thinks he is getting worse. The patient’s past medical history is significant for hypertension, for which he takes lisinopril. His family history is unknown as he was adopted. The patient met his mother once, and never knew his father but was told he died in his 50's. He drinks a few glasses of wine per week and has never smoked. On physical exam, the patient has a flat affect with facial grimace and sudden jerky movements of his upper extremities.
Which of the following is most likely to be seen on further workup?
- A. Alpha-synuclein aggregates on brain biopsy
- B. Dorsal striatum atrophy on head CT (Correct Answer)
- C. Positive 14-3-3 CSF assay
- D. Neurofibrillary tangles on brain biopsy
- E. Frontotemporal atrophy on head CT
Neurobiological basis of depression Explanation: ***Dorsal striatum atrophy on head CT***
- The clinical presentation of **involuntary jerky movements (chorea)**, **psychiatric changes (depression, irritability, flat affect)**, and **cognitive decline (poor work performance)** in a relatively young patient with a family history suggestive of premature death points to **Huntington's disease**.
- **Huntington's disease** is characterized by preferential **atrophy of the caudate and putamen** (components of the dorsal striatum), which can be visualized on CT or MRI of the head.
*Alpha-synuclein aggregates on brain biopsy*
- **Alpha-synuclein aggregates** are characteristic of **Lewy body diseases**, such as **Parkinson's disease** and **dementia with Lewy bodies (DLB)**.
- While patients with these conditions can have cognitive and psychiatric symptoms, the prominent **chorea** described is not typical.
*Positive 14-3-3 CSF assay*
- A **positive 14-3-3 protein assay in CSF** is a marker for **Creutzfeldt-Jakob disease (CJD)**, a rapidly progressive prion disease.
- CJD typically presents with **rapidly progressive dementia, myoclonus**, and cerebellar dysfunction, which differs from the gradual onset of chorea and mood changes seen here.
*Neurofibrillary tangles on brain biopsy*
- **Neurofibrillary tangles**, composed of hyperphosphorylated tau protein, are a hallmark pathological feature of **Alzheimer's disease**.
- **Alzheimer's disease** is primarily characterized by progressive memory loss and other cognitive deficits, but typically does not present with prominent chorea as the initial motor symptom.
*Frontotemporal atrophy on head CT*
- **Frontotemporal atrophy** is characteristic of **frontotemporal dementia (FTD)**, which can present with behavioral changes, personality alterations, and language difficulties.
- While FTD can cause psychiatric symptoms, the presence of prominent **chorea** makes Huntington's disease a more likely diagnosis.
Neurobiological basis of depression US Medical PG Question 4: A 73-year-old woman is brought in by her daughter stating that her mom has become increasingly forgetful and has trouble remembering recent events. Her memory for remote events is remarkably intact. The patient is no longer able to cook for herself as she frequently leaves the stove on unattended. She has recently been getting lost in her neighborhood even though she has lived there for 30 years. Her mood is not depressed. Decreased activity in which of the following areas of the brain is known to be involved in the pathogenesis of Alzheimer's disease?
- A. Raphe nucleus
- B. Ventral tegmentum
- C. Nucleus basalis (Correct Answer)
- D. Locus ceruleus
- E. Nucleus accumbens
Neurobiological basis of depression Explanation: ***Nucleus basalis***
- The **nucleus basalis of Meynert** is a key cholinergic nucleus that projects widely to the cerebral cortex.
- **Loss of cholinergic neurons** in the nucleus basalis is a hallmark of Alzheimer's disease and is associated with cognitive decline, particularly in memory.
*Raphe nucleus*
- The raphe nuclei are the primary source of **serotonin** in the brain, playing a crucial role in mood, sleep, and appetite regulation.
- While serotonin dysregulation can occur in neurodegenerative diseases, core Alzheimer's pathology is not primarily linked to decreased activity here.
*Ventral tegmentum*
- The **ventral tegmental area (VTA)** is a major source of **dopamine** in the brain, involved in the reward system, motivation, and addiction.
- Decreased activity in the VTA is not a primary pathological feature of Alzheimer's disease, though dopaminergic pathways can be indirectly affected.
*Locus ceruleus*
- The **locus ceruleus** is the main source of **norepinephrine** in the brain, involved in arousal, attention, and stress responses.
- While it can be affected in Alzheimer's, especially later in the disease, primary pathogenesis is not attributed to its decreased activity.
*Nucleus accumbens*
- The **nucleus accumbens** is part of the **limbic system** and plays a central role in reward, pleasure, and motivation.
- While brain regions involved in motivation can be affected as dementia progresses, it is not a primary site of degeneration in Alzheimer's pathology.
Neurobiological basis of depression US Medical PG Question 5: A 24-year-old woman comes to the physician because she feels sad and has had frequent, brief episodes of crying for the last month. During this period, she sleeps in every morning and spends most of her time in bed playing video games or reading. She has not been spending time with friends but still attends a weekly book club and continues to plan her annual family reunion. She stopped going to the gym, eats more, and has gained 4 kg (8.8 lb) over the past 4 weeks. Three weeks ago, she also started to smoke marijuana a few times a week. She drinks one glass of wine daily and does not smoke cigarettes. She is currently unemployed; she lost her job as a physical therapist 3 months ago. Her vital signs are within normal limits. On mental status examination, she is calm, alert, and oriented to person, place, and time. Her mood is depressed; her speech is organized, logical, and coherent. She denies suicidal thoughts. Which of the following is the most likely diagnosis?
- A. Bipolar disorder
- B. Substance use disorder
- C. Major depressive disorder
- D. Adjustment disorder (Correct Answer)
- E. Persistent Depressive Disorder (Dysthymia)
Neurobiological basis of depression Explanation: ***Adjustment disorder***
- This diagnosis is characterized by the development of emotional or behavioral symptoms in response to an identifiable stressor (such as losing a job) occurring within **3 months** of the onset of the stressor.
- The patient exhibits depressive symptoms (sadness, crying, increased sleep, anhedonia, weight gain) that do not meet the full criteria for a major depressive episode and do not significantly impair social/occupational functioning, as evidenced by her continued participation in a book club and planning her family reunion.
*Bipolar disorder*
- This disorder typically involves episodes of **mania or hypomania** along with depressive episodes, neither of which are described in the patient's presentation.
- Her symptoms are consistently depressive in nature and linked to a specific stressor, without periods of elevated mood, increased energy, or decreased need for sleep.
*Substance use disorder*
- While the patient has recently started smoking marijuana and drinks alcohol, these behaviors developed *after* the onset of her depressive symptoms and a known stressor.
- Her marijuana use is still relatively recent ("a few times a week") and not yet described as causing significant impairment or dependence that would typically define a substance use disorder as the primary diagnosis.
*Major depressive disorder*
- This diagnosis requires a severe and pervasive depressive episode that lasts for at least **2 weeks** and significantly impairs functioning in multiple areas of life.
- Although she has several depressive symptoms, her continued ability to engage in some social activities (book club) and plan events (family reunion) suggests that the impairment is not as severe or pervasive as typically seen in MDD. Additionally, her symptoms are clearly linked to a recent life stressor, which points away from MDD as the primary diagnosis.
*Persistent Depressive Disorder (Dysthymia)*
- This disorder is characterized by a chronically depressed mood that lasts for at least **2 years** (or 1 year in children/adolescents), with symptoms that are generally milder than major depression but more persistent.
- The patient's symptoms have only been present for one month, which is far too short a duration to meet the diagnostic criteria for persistent depressive disorder.
Neurobiological basis of depression US Medical PG Question 6: A 29-year-old man presents to his primary care provider complaining of not being able to get enough rest at night. He goes to bed early enough and has otherwise good sleep hygiene but feels drained the next day. He feels he is unable to perform optimally at work, but he is still a valued employee and able to complete his share of the work. About a month ago his wife of 5 years asked for a divorce and quickly moved out. He has cut out coffee after 12 pm and stopped drinking alcohol. He also exercises 3 days per week. Today, his blood pressure is 120/80 mm Hg, heart rate is 95/min, respiratory rate is 25/min, and temperature is 37.0°C (98.6°F ). On physical exam, his heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. A CMP, CBC, and thyroid test are negative. Which of the following statements best describes this patient’s condition?
- A. Symptoms are usually self-limited and may persist for 2 years
- B. Symptoms typically resolve within 6 months after the stressor ends (Correct Answer)
- C. Symptoms develop within 3 months of the stressor
- D. Symptoms may be persistent if the stressor is chronic
- E. Symptoms represent a maladaptive response to an identifiable stressor
Neurobiological basis of depression Explanation: ***Symptoms typically resolve within 6 months after the stressor ends***
- This statement accurately describes the **temporal criterion for adjustment disorder** according to DSM-5. Once the stressor or its consequences have terminated, symptoms should resolve within 6 months.
- This patient experienced a clear stressor (divorce and wife moving out ~1 month ago) and developed symptoms in response. The diagnosis of adjustment disorder requires that these symptoms resolve within 6 months of the stressor's termination.
- His symptoms (poor sleep, feeling drained, suboptimal performance) represent a significant but not incapacitating response, consistent with adjustment disorder. Normal labs rule out medical causes.
- This temporal criterion distinguishes adjustment disorder from more chronic conditions and helps guide prognosis and treatment planning.
*Symptoms are usually self-limited and may persist for 2 years*
- Adjustment disorder symptoms should resolve within **6 months**, not 2 years, after the stressor or its consequences have ended.
- If symptoms persist beyond 6 months, this suggests either ongoing stressor consequences, a persistent subtype (for chronic stressors), or an alternative diagnosis should be considered.
*Symptoms develop within 3 months of the stressor*
- While this is a **correct diagnostic criterion** (symptoms must develop within 3 months of stressor onset), it only addresses timing of onset, not the complete picture.
- The question asks for the statement that "best describes" the condition, and the resolution timeline is more distinctive and prognostically important than onset timing alone.
*Symptoms may be persistent if the stressor is chronic*
- This describes the **persistent specifier** in DSM-5, which applies when the stressor or its consequences are ongoing (chronic stressor or enduring consequences).
- However, in this case, the stressor appears to be acute (wife moved out), not chronic, making this less applicable to the specific clinical scenario presented.
*Symptoms represent a maladaptive response to an identifiable stressor*
- This is a **core defining feature** of adjustment disorder - the development of emotional/behavioral symptoms in response to an identifiable stressor with marked distress or impairment.
- While accurate, this is a general characteristic shared across the definition and doesn't capture the specific **temporal criteria** (resolution within 6 months) that is most distinctive for adjustment disorder diagnosis and prognosis.
Neurobiological basis of depression US Medical PG Question 7: A 42-year-old female presents to her primary care provider for an annual checkup. She reports feeling sad over the past few months for no apparent reason. She has lost interest in swimming, which she previously found enjoyable. Additionally, she has had trouble getting a full night’s sleep and has had trouble concentrating during the day. She has lost 15 pounds since her last visit one year prior. Which of the following sets of neurotransmitter levels is associated with this patient’s condition?
- A. Decreased acetylcholine, normal serotonin, normal dopamine
- B. Decreased norepinephrine, decreased serotonin, decreased dopamine (Correct Answer)
- C. Decreased GABA, decreased acetylcholine, increased dopamine
- D. Increased norepinephrine, decreased serotonin, decreased GABA
- E. Increased acetylcholine, increased serotonin, decreased dopamine
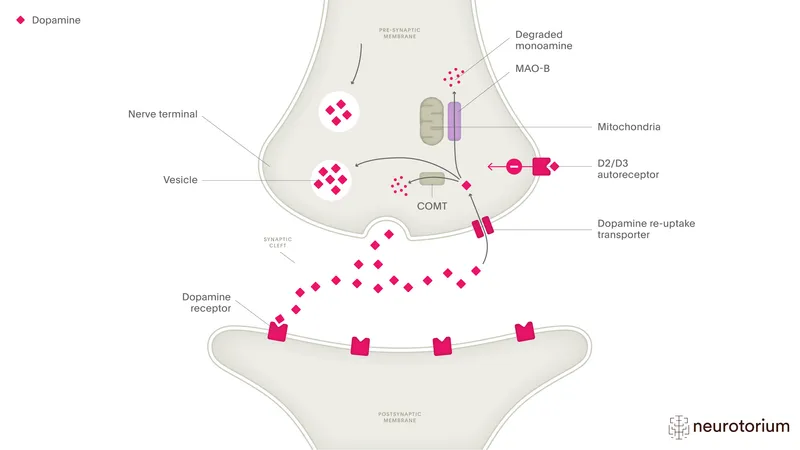
Neurobiological basis of depression Explanation: ***Decreased norepinephrine, decreased serotonin, decreased dopamine***
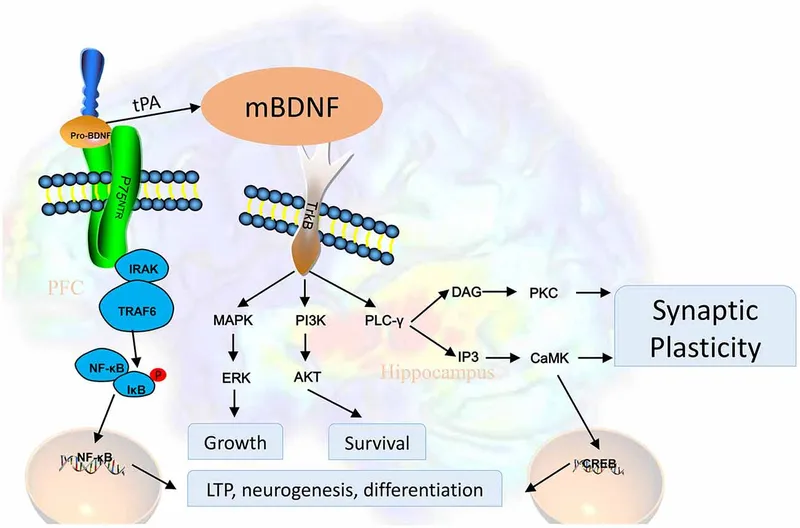
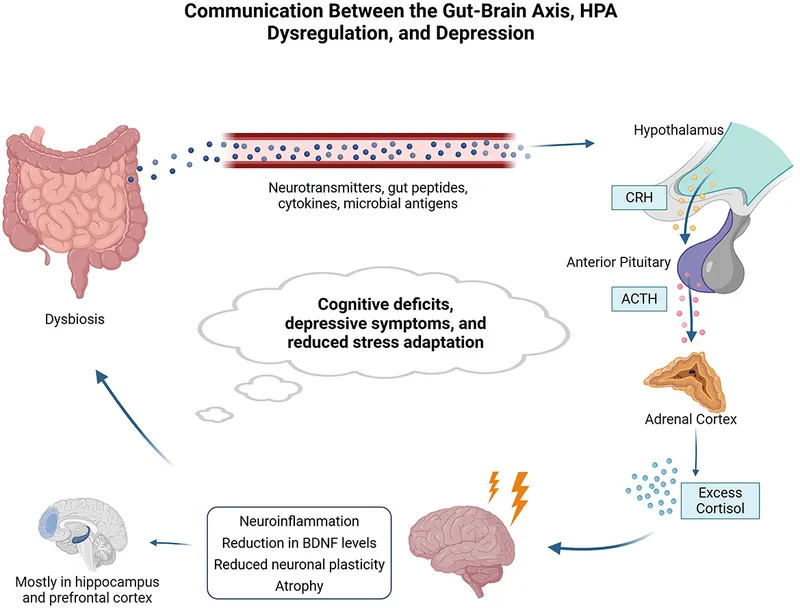
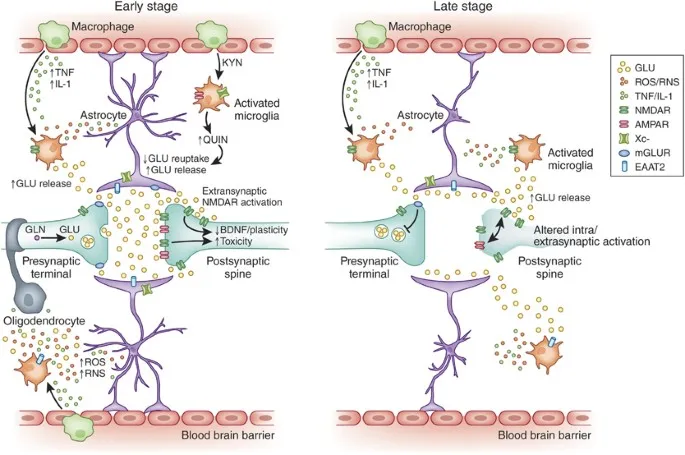
- The patient's symptoms of **sadness**, loss of interest (**anhedonia**), **insomnia**, **difficulty concentrating**, and **weight loss** are classic for **major depressive disorder**.
- **Depression** is strongly associated with deficiencies in **monoamine neurotransmitters**: **norepinephrine**, **serotonin**, and **dopamine**.
*Decreased acetylcholine, normal serotonin, normal dopamine*
- While **acetylcholine** is involved in mood regulation, its isolated decrease with normal serotonin and dopamine levels is not characteristic of generalized depression.
- More prominent roles for **acetylcholine dysfunction** are seen in conditions like **Alzheimer's disease** or **myasthenia gravis**.
*Decreased GABA, decreased acetylcholine, increased dopamine*
- **Decreased GABA** is often associated with **anxiety disorders** and seizures, not the primary presentation of depression here.
- **Increased dopamine** is more characteristic of conditions like **schizophrenia** or **mania**, which contrasts with the patient's depressive symptoms.
*Increased norepinephrine, decreased serotonin, decreased GABA*
- **Increased norepinephrine** is typically associated with **anxiety**, **stress**, or sometimes **mania**, which is inconsistent with this patient's depressive state.
- While **decreased serotonin** is correct for depression, the combination with increased norepinephrine and decreased GABA does not fit the typical neurotransmitter profile.
*Increased acetylcholine, increased serotonin, decreased dopamine*
- **Increased acetylcholine** is generally not associated with the full spectrum of depressive symptoms described.
- **Increased serotonin** is often the goal of antidepressant treatments (SSRIs), making an endogenous increase unlikely to cause depression.
Neurobiological basis of depression US Medical PG Question 8: A 33-year-old man visits his psychiatrist with feelings of sadness on most days of the week for the past 4 weeks. He says that he is unable to participate in his daily activities and finds it hard to get out of bed on most days. If he has nothing scheduled for the day, he sometimes sleeps for 10–12 hours at a stretch. He has also noticed that on certain days, his legs feel heavy and he finds it difficult to walk, as though there are bricks tied to his feet. However, he is still able to attend social events and also enjoys playing with his children when he comes home from work. Other than these simple pleasures, he has lost interest in most of the activities he previously enjoyed. Another troubling fact is that he had gained weight over the past month, mainly because he eats so much when overcome by these feelings of depression. His is prescribed a medication to treat his symptoms. Which of the following is the mechanism of action of the drug he was most likely prescribed?
- A. Activates the γ-aminobutyric acid receptors
- B. Inhibit the uptake of serotonin and norepinephrine at the presynaptic cleft (Correct Answer)
- C. Works as an antagonist at the dopamine and serotonin receptors
- D. Non-selectively inhibits monoamine oxidase A and B
- E. Stimulates the release of norepinephrine and dopamine in the presynaptic cleft
Neurobiological basis of depression Explanation: ***Inhibit the uptake of serotonin and norepinephrine at the presynaptic cleft***
- The patient presents with symptoms characteristic of **atypical depression**, including increased sleep (**hypersomnia**), increased appetite leading to weight gain, **leaden paralysis** (heavy feelings in the limbs), and **mood reactivity** (enjoying social events/playing with children).
- For initial treatment of atypical depression, **SSRIs** (e.g., fluoxetine, sertraline) and **SNRIs** (e.g., venlafaxine, duloxetine) are considered **first-line therapies** due to their favorable safety profile and efficacy.
- **SNRIs** address both serotonin and norepinephrine imbalances and are effective for atypical depression, particularly when there is significant fatigue or pain.
*Activates the γ-aminobutyric acid receptors*
- This mechanism describes **benzodiazepines** or other GABAergic drugs, which are typically used for anxiety, insomnia, or acute agitation.
- While they can provide symptomatic relief for anxiety associated with depression, they do not target the core depressive symptoms, lack antidepressant efficacy, and carry risk of dependence.
*Works as an antagonist at the dopamine and serotonin receptors*
- This mechanism describes **second-generation antipsychotics** (e.g., quetiapine, aripiprazole), which are primarily used to treat psychotic disorders or as adjuncts in severe depression with psychotic features or treatment-resistant depression.
- The patient's symptoms do not suggest psychotic features, and antipsychotics are not first-line treatment for uncomplicated atypical depression.
*Non-selectively inhibits monoamine oxidase A and B*
- This describes **non-selective MAOIs** (e.g., phenelzine, tranylcypromine), which are considered the **most effective** antidepressants for atypical depression based on clinical trials.
- However, MAOIs are typically reserved for **treatment-resistant depression** due to their significant side effect profile, dietary restrictions (tyramine-free diet to prevent **hypertensive crisis**), and drug interaction risks.
- Given this is an initial presentation without treatment failure, MAOIs would not be the first-line choice despite their superior efficacy.
*Stimulates the release of norepinephrine and dopamine in the presynaptic cleft*
- This mechanism could describe **amphetamines** or certain **wake-promoting agents**, which are not standard antidepressant treatments.
- **Bupropion** (an antidepressant) inhibits reuptake of norepinephrine and dopamine but does not directly stimulate their release.
- Stimulants are occasionally used as adjuncts for treatment-resistant depression but are not first-line monotherapy due to abuse potential and limited evidence for long-term efficacy in depression.
Neurobiological basis of depression US Medical PG Question 9: A 27-year-old woman visits a psychiatrist expressing her feelings of sadness which are present on most days of the week. She says that she has been feeling this way for about 2 to 3 years. During her first pregnancy 3 years ago, the fetus died in utero, and the pregnancy was terminated at 21 weeks. Ever since then, she hasn’t been able to sleep well at night and has difficulty concentrating on her tasks most of the time. However, for the past month, she has found it more difficult to cope. She says she has no will to have another child as she still feels guilty and responsible for the previous pregnancy. Over the past few days, she has completely lost her appetite and only eats once or twice a day. She doesn’t recall a single day in the last 3 years where she has not felt this way. The patient denies any past or current smoking, alcohol, or recreational drug use. Which of the following is the most likely diagnosis in this patient?
- A. Persistent depressive disorder (Correct Answer)
- B. Bipolar disorder
- C. Schizoaffective disorder
- D. Cyclothymia
- E. Major depressive disorder
Neurobiological basis of depression Explanation: ***Persistent depressive disorder***
- The patient exhibits classic symptoms of **persistent depressive disorder (dysthymia)**: chronic depressed mood for **at least two years**, accompanied by other depressive symptoms like **insomnia**, **difficulty concentrating**, and changes in appetite.
- The duration of her symptoms (2-3 years) and the consistent feeling of sadness support this diagnosis, fitting the diagnostic criteria for **dysthymia**.
*Bipolar disorder*
- Bipolar disorder involves distinct episodes of **mania or hypomania** alternating with depressive episodes.
- The patient's history does not indicate any periods of elevated mood, increased energy, or decreased need for sleep, which are characteristic of **bipolar disorder**.
*Schizoaffective disorder*
- Schizoaffective disorder is characterized by a combination of **mood symptoms** (like depression or mania) and **psychotic symptoms** (like delusions or hallucinations) occurring simultaneously or in distinct episodes.
- This patient presents with no evidence of **psychotic symptoms** such as hallucinations or delusions.
*Cyclothymia*
- Cyclothymia is a milder, chronic form of **bipolar disorder** involving numerous periods of **hypomanic symptoms** and numerous periods of **depressive symptoms** for at least two years.
- The patient's presentation lacks any history of **hypomanic episodes**, making cyclothymia an unlikely diagnosis.
*Major depressive disorder*
- While the patient is experiencing a **major depressive episode** currently (as suggested by increased severity in the last month and complete loss of appetite), the underlying chronic nature of her symptoms (2-3 years) and the fact that she has not been symptom-free for more than two months indicate **persistent depressive disorder**.
- A diagnosis of **major depressive disorder** would typically be given if the symptoms were acute (less than 2 years) and severe, without the chronic, pervasive depressive state described.
Neurobiological basis of depression US Medical PG Question 10: A 52-year-old man presents with a 1-month history of a depressed mood. He says that he has been “feeling low” on most days of the week. He also says he has been having difficulty sleeping, feelings of being worthless, difficulty performing at work, and decreased interest in reading books (his hobby). He has no significant past medical history. The patient denies any history of smoking, alcohol use, or recreational drug use. A review of systems is significant for a 7% unintentional weight gain over the past month. The patient is afebrile and his vital signs are within normal limits. A physical examination is unremarkable. The patient is prescribed sertraline 50 mg daily. On follow-up 4 weeks later, the patient says he is slightly improved but is still not feeling 100%. Which of the following is the best next step in the management of this patient?
- A. Switch to a different SSRI
- B. Continue sertraline (Correct Answer)
- C. Add buspirone
- D. Switch to an MAOI
- E. Add aripiprazole
Neurobiological basis of depression Explanation: ***Continue sertraline***
- Many antidepressants, including SSRIs like sertraline, require **4-6 weeks at a therapeutic dose** to achieve their full effect. Since the patient reports slight improvement after 4 weeks, continuing the current medication allows more time for optimal response.
- The goal is for the patient to feel "100%", which often takes longer than one month. **Gradual improvement** after initial therapy suggests the medication is working, but needs more time.
*Switch to a different SSRI*
- Switching to another SSRI is typically considered if there is **no improvement or significant intolerance** after an adequate trial (at least 4-6 weeks) at a therapeutic dose of the initial SSRI.
- This patient has shown *slight improvement*, indicating that sertraline may still be effective with more time.
*Add buspirone*
- Buspirone is an **anxiolytic medication** sometimes used as an augmentation strategy for depression, particularly if anxiety is a prominent symptom.
- However, it's generally added *after* an initial antidepressant has failed to achieve a full response, and typically *after* optimizing the dose and duration of the primary antidepressant.
*Switch to an MAOI*
- **Monoamine oxidase inhibitors (MAOIs)** are older antidepressants with a more challenging side effect profile and significant drug-drug and drug-food interactions.
- They are typically reserved for patients who have **failed multiple trials of other antidepressants** due to their safety concerns.
*Add aripiprazole*
- Aripiprazole, an **atypical antipsychotic**, is sometimes used as an augmentation strategy for **treatment-resistant depression**.
- This approach is usually considered when trials of several different antidepressant classes have failed or when the depression has not responded adequately to optimized antidepressant therapy.
More Neurobiological basis of depression US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.