Major depressive disorder diagnostic criteria US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Major depressive disorder diagnostic criteria. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Major depressive disorder diagnostic criteria US Medical PG Question 1: A 33-year-old woman is brought to the physician by her husband because of persistent sadness for the past 2 months. During this period, she also has had difficulty sleeping and an increased appetite. She had similar episodes that occurred 2 years ago and 9 months ago that each lasted for 4 months. Between these episodes, she reported feeling very energetic and rested after 3 hours of sleep. She often went for long periods of time without eating. She works as a stock market trader and received a promotion 5 months ago. She regularly attends yoga classes on the weekends with her friends. On mental status examination, she has a blunted affect. She denies suicidal thoughts and illicit drug use. Which of the following is the most likely diagnosis?
- A. Major depressive disorder with seasonal pattern
- B. Persistent depressive disorder
- C. Bipolar II disorder (Correct Answer)
- D. Major depressive disorder with atypical features
- E. Cyclothymic disorder
Major depressive disorder diagnostic criteria Explanation: ***Bipolar II disorder***
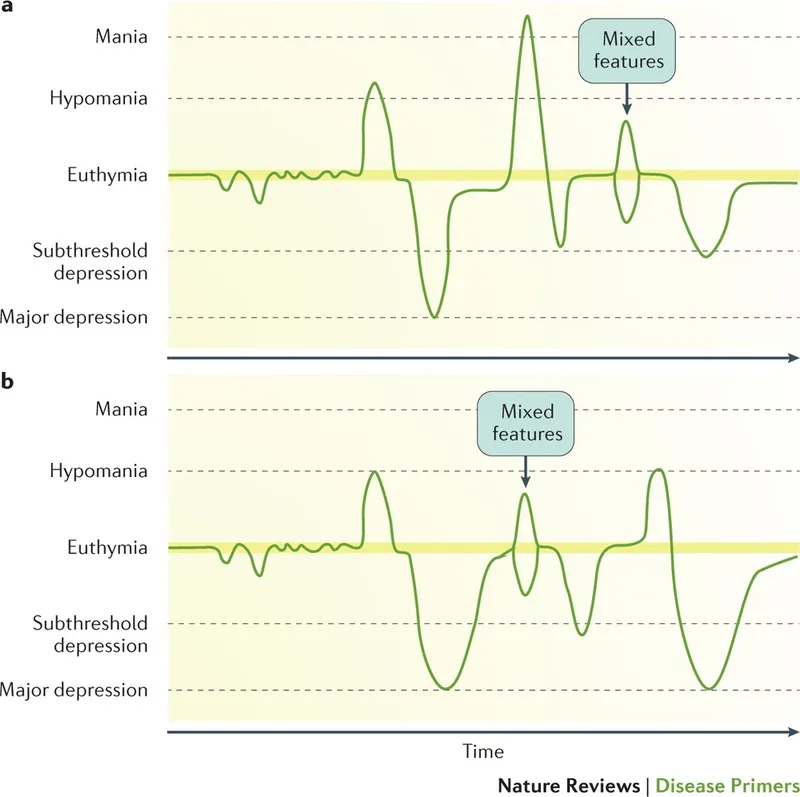
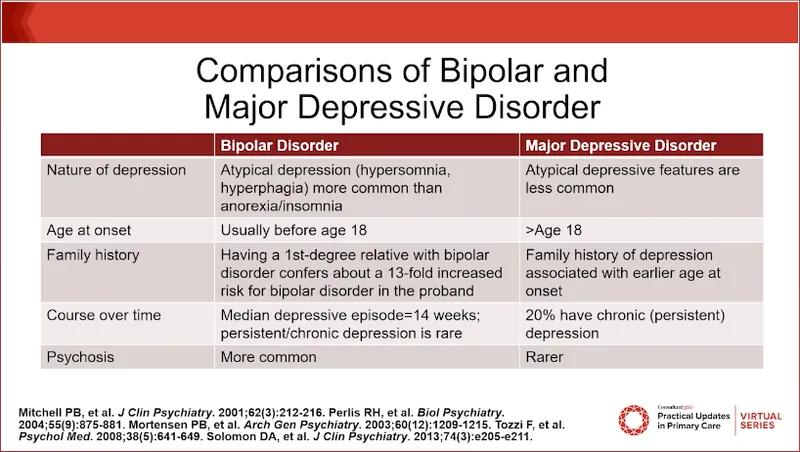
- The patient exhibits recurrent episodes of **major depression** (sadness, sleep difficulties, increased appetite) interspersed with periods of **hypomania** (energetic, reduced need for sleep, long periods without eating, successful work performance with promotion)
- This pattern is characteristic of **Bipolar II disorder**: major depressive episodes plus at least one hypomanic episode
- No evidence of **frank mania** (e.g., psychosis, severe impairment requiring hospitalization) is present, which distinguishes this from Bipolar I disorder
*Major depressive disorder with seasonal pattern*
- While the patient presents with depressive symptoms, the episodes of **hypomania** (increased energy, decreased need for sleep) rule out unipolar depression
- The history of episodes at various times (2 years ago, 9 months ago, current) does not fit a **seasonal pattern**
- The **hypomanic phases** between depressive episodes are inconsistent with any form of major depressive disorder
*Persistent depressive disorder*
- This condition involves **chronic depressive symptoms** lasting at least 2 years, but typically less severe than major depressive episodes
- The presence of distinct, severe **major depressive episodes** and recurrent **hypomanic periods** contradicts this diagnosis
- Persistent depressive disorder does not include hypomania or mood elevation
*Major depressive disorder with atypical features*
- Atypical features include **increased appetite**, **hypersomnia**, leaden paralysis, interpersonal rejection sensitivity, and mood reactivity
- While increased appetite is present during depressive phases, the alternating periods of **hypomania** exclude this from being major depressive disorder
- Any form of major depressive disorder is ruled out by the presence of hypomanic episodes
*Cyclothymic disorder*
- Cyclothymic disorder involves numerous periods of **hypomanic symptoms** and **depressive symptoms** for at least 2 years, but symptoms do not meet full criteria for major depressive or hypomanic episodes
- This patient explicitly experiences **major depressive episodes** (persistent sadness, neurovegetative symptoms lasting 4 months), which exceed the threshold for cyclothymia
- The severity and duration of depressive episodes make Bipolar II disorder the correct diagnosis
Major depressive disorder diagnostic criteria US Medical PG Question 2: A 25-year-old woman comes to the physician because of sadness that started 3 weeks after her daughter was born. Her daughter is now 9 months old and usually sleeps through the night, but the patient still has difficulty staying asleep. She has not returned to work since the birth. She is easily distracted from normal daily tasks. She used to enjoy cooking, but only orders delivery or take-out now. She says that she always feels too exhausted to do so and does not feel hungry much anyway. The pregnancy of the patient's child was complicated by gestational diabetes. The child was born at 36-weeks' gestation and has had no medical issues. The patient has no contact with the child's father. She is not sexually active. She does not smoke, drink alcohol, or use illicit drugs. She is 157 cm (5 ft 1 in) tall and weighs 47 kg (105 lb); BMI is 20 kg/m2. Vital signs are within normal limits. She is alert and cooperative but makes little eye contact. Physical examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Adjustment disorder
- B. Major depressive disorder
- C. Normal behavior
- D. Disruptive mood dysregulation disorder
- E. Depression with peripartum-onset (Correct Answer)
Major depressive disorder diagnostic criteria Explanation: ***Depression with peripartum-onset***
- The patient exhibits classic symptoms of **major depressive disorder**, including **anhedonia** (loss of enjoyment in cooking), **fatigue**, **insomnia**, and **changes in appetite/weight**, all appearing within 3 weeks post-childbirth and persisting for 9 months.
- According to **DSM-5-TR**, the **peripartum onset specifier** is applied when a major depressive episode begins during pregnancy or **within 4 weeks after delivery**.
- This patient's symptoms began at 3 weeks postpartum, meeting criteria for the peripartum onset specifier, which is clinically important for risk assessment (including infanticide risk) and treatment planning.
- The severity and duration of symptoms (persistent anhedonia, significant fatigue, insomnia despite adequate opportunity for sleep, appetite changes, functional impairment lasting months) clearly meet criteria for a **major depressive episode**.
*Adjustment disorder*
- This diagnosis involves emotional or behavioral symptoms in response to an identifiable stressor that do **not meet criteria for a major depressive episode**.
- The severity, number, and duration of symptoms (anhedonia, significant fatigue, insomnia, appetite changes, functional impairment lasting 9 months) exceed what is seen in adjustment disorder and meet full criteria for **major depressive disorder**.
*Major depressive disorder*
- While this patient's symptoms fully meet criteria for **Major Depressive Disorder (MDD)**, the onset within 4 weeks postpartum requires the addition of the **"with peripartum onset" specifier** per DSM-5-TR.
- Using the peripartum onset specifier is essential for clinical management, as it alerts clinicians to specific risks (including thoughts of harming the infant) and may influence treatment selection (e.g., considerations for breastfeeding-compatible medications).
*Normal behavior*
- The patient's symptoms—including **persistent sadness lasting 9 months**, **anhedonia**, **insomnia despite adequate sleep opportunity**, **significant fatigue**, **appetite loss**, and **inability to return to work**—represent severe functional impairment.
- These symptoms far exceed normal postpartum adjustment or transient "baby blues" (which typically resolve within 2 weeks postpartum) and indicate a serious mood disorder requiring treatment.
*Disruptive mood dysregulation disorder*
- This disorder is diagnosed **only in children and adolescents aged 6-18 years** and is characterized by persistent irritability and frequent, severe temper outbursts disproportionate to the situation.
- It is **not applicable to adults** and does not describe this patient's presentation of persistent depressed mood and neurovegetative symptoms.
Major depressive disorder diagnostic criteria US Medical PG Question 3: A 38-year-old man comes to the physician because of persistent sadness and difficulty concentrating for the past 6 weeks. During this period, he has also had difficulty sleeping. He adds that he has been “feeling down” most of the time since his girlfriend broke up with him 4 years ago. Since then, he has only had a few periods of time when he did not feel that way, but none of these lasted for more than a month. He reports having no problems with appetite, weight, or energy. He does not use illicit drugs or alcohol. Mental status examination shows a depressed mood and constricted affect. Which of the following is the most likely diagnosis?
- A. Persistent depressive disorder (Correct Answer)
- B. Adjustment disorder with depressed mood
- C. Major depressive disorder
- D. Bipolar affective disorder
- E. Cyclothymic disorder
Major depressive disorder diagnostic criteria Explanation: ***Persistent depressive disorder***
- This condition is characterized by a **chronically depressed mood** that lasts for at least two years in adults, with symptoms not remitting for more than two consecutive months.
- The patient's history of feeling "down" for four years, with only brief periods of relief (never exceeding one month), fits this chronic pattern and meets the diagnostic criteria for persistent depressive disorder (formerly dysthymia).
- Although the patient has had worsening symptoms over the past 6 weeks, the **predominant feature** is the chronic, low-grade depression lasting 4 years, making persistent depressive disorder the most likely primary diagnosis.
*Adjustment disorder with depressed mood*
- An adjustment disorder typically involves emotional or behavioral symptoms in response to an **identifiable stressor**, occurring within 3 months of the stressor's onset and lasting no longer than 6 months after the stressor or its consequences have ceased.
- The patient's symptoms have been ongoing for 4 years, far exceeding the typical duration for an adjustment disorder, which by definition should not persist beyond 6 months after the stressor ends.
*Major depressive disorder*
- Major depressive disorder involves discrete episodes of at least 2 weeks with **five or more symptoms** including depressed mood or anhedonia, plus symptoms such as changes in appetite/weight, sleep disturbance, psychomotor changes, fatigue, worthlessness/guilt, concentration difficulty, or suicidal ideation.
- While the patient has some symptoms that could suggest a current major depressive episode (6 weeks of sadness, concentration difficulty, sleep problems), the question emphasizes the **chronic 4-year course** of low-grade depressive symptoms as the predominant pattern, which is more consistent with persistent depressive disorder.
- Note that patients can have MDD superimposed on persistent depressive disorder ("double depression"), but the chronic pattern described here makes persistent depressive disorder the primary diagnosis.
*Bipolar affective disorder*
- This disorder is characterized by distinct periods of **mood episodes** that include at least one manic or hypomanic episode, in addition to depressive episodes.
- The patient's presentation does not describe any manic or hypomanic symptoms (e.g., elevated mood, increased energy, decreased need for sleep, grandiosity, increased talkativeness, or risky behavior) that are characteristic of bipolar disorder.
*Cyclothymic disorder*
- Cyclothymic disorder involves numerous periods of **hypomanic symptoms** and numerous periods of **depressive symptoms** for at least 2 years, but these symptoms are not severe enough to meet the criteria for a hypomanic or major depressive episode.
- The patient describes chronic low mood without any mention of alternating periods of elevated mood or hypomanic symptoms, which are essential for a diagnosis of cyclothymic disorder.
Major depressive disorder diagnostic criteria US Medical PG Question 4: A 24-year-old woman comes to the physician because she feels sad and has had frequent, brief episodes of crying for the last month. During this period, she sleeps in every morning and spends most of her time in bed playing video games or reading. She has not been spending time with friends but still attends a weekly book club and continues to plan her annual family reunion. She stopped going to the gym, eats more, and has gained 4 kg (8.8 lb) over the past 4 weeks. Three weeks ago, she also started to smoke marijuana a few times a week. She drinks one glass of wine daily and does not smoke cigarettes. She is currently unemployed; she lost her job as a physical therapist 3 months ago. Her vital signs are within normal limits. On mental status examination, she is calm, alert, and oriented to person, place, and time. Her mood is depressed; her speech is organized, logical, and coherent. She denies suicidal thoughts. Which of the following is the most likely diagnosis?
- A. Bipolar disorder
- B. Substance use disorder
- C. Major depressive disorder
- D. Adjustment disorder (Correct Answer)
- E. Persistent Depressive Disorder (Dysthymia)
Major depressive disorder diagnostic criteria Explanation: ***Adjustment disorder***
- This diagnosis is characterized by the development of emotional or behavioral symptoms in response to an identifiable stressor (such as losing a job) occurring within **3 months** of the onset of the stressor.
- The patient exhibits depressive symptoms (sadness, crying, increased sleep, anhedonia, weight gain) that do not meet the full criteria for a major depressive episode and do not significantly impair social/occupational functioning, as evidenced by her continued participation in a book club and planning her family reunion.
*Bipolar disorder*
- This disorder typically involves episodes of **mania or hypomania** along with depressive episodes, neither of which are described in the patient's presentation.
- Her symptoms are consistently depressive in nature and linked to a specific stressor, without periods of elevated mood, increased energy, or decreased need for sleep.
*Substance use disorder*
- While the patient has recently started smoking marijuana and drinks alcohol, these behaviors developed *after* the onset of her depressive symptoms and a known stressor.
- Her marijuana use is still relatively recent ("a few times a week") and not yet described as causing significant impairment or dependence that would typically define a substance use disorder as the primary diagnosis.
*Major depressive disorder*
- This diagnosis requires a severe and pervasive depressive episode that lasts for at least **2 weeks** and significantly impairs functioning in multiple areas of life.
- Although she has several depressive symptoms, her continued ability to engage in some social activities (book club) and plan events (family reunion) suggests that the impairment is not as severe or pervasive as typically seen in MDD. Additionally, her symptoms are clearly linked to a recent life stressor, which points away from MDD as the primary diagnosis.
*Persistent Depressive Disorder (Dysthymia)*
- This disorder is characterized by a chronically depressed mood that lasts for at least **2 years** (or 1 year in children/adolescents), with symptoms that are generally milder than major depression but more persistent.
- The patient's symptoms have only been present for one month, which is far too short a duration to meet the diagnostic criteria for persistent depressive disorder.
Major depressive disorder diagnostic criteria US Medical PG Question 5: A 42-year-old female presents to her primary care provider for an annual checkup. She reports feeling sad over the past few months for no apparent reason. She has lost interest in swimming, which she previously found enjoyable. Additionally, she has had trouble getting a full night’s sleep and has had trouble concentrating during the day. She has lost 15 pounds since her last visit one year prior. Which of the following sets of neurotransmitter levels is associated with this patient’s condition?
- A. Decreased acetylcholine, normal serotonin, normal dopamine
- B. Decreased norepinephrine, decreased serotonin, decreased dopamine (Correct Answer)
- C. Decreased GABA, decreased acetylcholine, increased dopamine
- D. Increased norepinephrine, decreased serotonin, decreased GABA
- E. Increased acetylcholine, increased serotonin, decreased dopamine
Major depressive disorder diagnostic criteria Explanation: ***Decreased norepinephrine, decreased serotonin, decreased dopamine***
- The patient's symptoms of **sadness**, loss of interest (**anhedonia**), **insomnia**, **difficulty concentrating**, and **weight loss** are classic for **major depressive disorder**.
- **Depression** is strongly associated with deficiencies in **monoamine neurotransmitters**: **norepinephrine**, **serotonin**, and **dopamine**.
*Decreased acetylcholine, normal serotonin, normal dopamine*
- While **acetylcholine** is involved in mood regulation, its isolated decrease with normal serotonin and dopamine levels is not characteristic of generalized depression.
- More prominent roles for **acetylcholine dysfunction** are seen in conditions like **Alzheimer's disease** or **myasthenia gravis**.
*Decreased GABA, decreased acetylcholine, increased dopamine*
- **Decreased GABA** is often associated with **anxiety disorders** and seizures, not the primary presentation of depression here.
- **Increased dopamine** is more characteristic of conditions like **schizophrenia** or **mania**, which contrasts with the patient's depressive symptoms.
*Increased norepinephrine, decreased serotonin, decreased GABA*
- **Increased norepinephrine** is typically associated with **anxiety**, **stress**, or sometimes **mania**, which is inconsistent with this patient's depressive state.
- While **decreased serotonin** is correct for depression, the combination with increased norepinephrine and decreased GABA does not fit the typical neurotransmitter profile.
*Increased acetylcholine, increased serotonin, decreased dopamine*
- **Increased acetylcholine** is generally not associated with the full spectrum of depressive symptoms described.
- **Increased serotonin** is often the goal of antidepressant treatments (SSRIs), making an endogenous increase unlikely to cause depression.
Major depressive disorder diagnostic criteria US Medical PG Question 6: A 28-year-old woman presents with continuous feelings of sadness and rejection. She says that over the past couple of weeks, she has been unable to concentrate on her job and has missed several days of work. She also has no interest in any activity and typically rejects invitations to go out with friends. She has no interest in food or playing with her dog. Her husband is concerned about this change in behavior. A few months ago, she was very outgoing and made many plans with her friends. She remembers being easily distracted and also had several ‘brilliant ideas’ on what she should be doing with her life. She did not sleep much during that week, but now all she wants to do is lie in bed all day. She denies any suicidal or homicidal ideations. She has no past medical history and has never been hospitalized. Laboratory tests were normal. Which of the following is the most likely diagnosis in this patient?
- A. Major depressive disorder
- B. Dysthymia
- C. Bipolar disorder, type II (Correct Answer)
- D. Schizoaffective disorder
- E. Bipolar disorder, type I
Major depressive disorder diagnostic criteria Explanation: ***Bipolar disorder, type II***
− This patient's current symptoms of profound **sadness, anhedonia, low energy, and social withdrawal** are indicative of a major depressive episode.
− The history of prior periods of **decreased need for sleep, brilliant ideas, and being easily distracted** suggests a hypomanic episode, a hallmark of bipolar disorder type II.
*Major depressive disorder*
− While the patient is currently experiencing a **major depressive episode**, the history of previous hypomanic symptoms rules out a diagnosis of unipolar major depressive disorder.
− **Major depressive disorder** does not include a history of manic or hypomanic episodes.
*Dysthymia*
− **Dysthymia** (persistent depressive disorder) is characterized by chronic, milder depressive symptoms lasting at least two years.
− The current episode is severe and marked by a clear change from a previous elevated mood state, which is inconsistent with dysthymia.
*Schizoaffective disorder*
− **Schizoaffective disorder** involves episodes of mood disturbance alongside symptoms of schizophrenia (e.g., hallucinations, delusions) that occur at least two weeks without prominent mood symptoms.
− This patient's symptoms are primarily mood-related and do not include psychotic features characteristic of schizophrenia.
*Bipolar disorder, type I*
− **Bipolar disorder type I** is characterized by the occurrence of at least one manic episode, which involves more severe symptoms, significant impairment, and often psychosis.
− The patient's previous "brilliant ideas" and decreased need for sleep describe a **hypomanic episode** rather than a full manic episode and are not associated with marked functional impairment or psychotic features.
Major depressive disorder diagnostic criteria US Medical PG Question 7: A 35-year-old banker is brought to a medical clinic by his concerned wife. For the past 3 weeks, he has not been eating well and has had a 10 kg (22 lb) weight loss. He wakes up very early in the mornings and feels extremely despondent. He no longer goes out on the weekends to hang out with his close friends nor does he go on date nights with his wife. He feels guilty for letting his friends and family down recently. He additionally has a history of fibromyalgia and deals with daily pain. What would be the most appropriate treatment plan for this patient?
- A. Amitriptyline
- B. Phenelzine
- C. Venlafaxine (Correct Answer)
- D. Electroconvulsive therapy
- E. Fluoxetine
Major depressive disorder diagnostic criteria Explanation: ***Venlafaxine***
- This patient presents with symptoms highly suggestive of **major depressive disorder**, including **anhedonia**, significant **weight loss**, **early morning awakening**, and **feelings of guilt**. His co-occurring **fibromyalgia** makes a **serotonin-norepinephrine reuptake inhibitor (SNRI)** like venlafaxine an excellent choice.
- SNRIs are effective for both depression and chronic pain conditions such as fibromyalgia, as they modulate both **serotonin** and **norepinephrine** pathways, which are implicated in both mood and pain perception.
*Amitriptyline*
- **Amitriptyline** is a **tricyclic antidepressant (TCA)** that can be used for both depression and chronic pain, including fibromyalgia.
- However, TCAs generally have a less favorable side effect profile (e.g., **anticholinergic effects**, **cardiac toxicity in overdose**) compared to SNRIs and SSRIs, making them less of a first-line choice unless other options fail or specific indications are present.
*Phenelzine*
- **Phenelzine** is a **monoamine oxidase inhibitor (MAOI)**, typically reserved for **atypical depression** or treatment-resistant depression due to its significant **food and drug interactions** (e.g., **hypertensive crisis** with tyramine-rich foods or sympathomimetics).
- Given this is likely a first-line treatment scenario, an MAOI would not be the most appropriate initial choice.
*Electroconvulsive therapy*
- **Electroconvulsive therapy (ECT)** is a highly effective treatment for severe depression, especially with **psychotic features**, **catatonia**, or **severe suicidality**, or in cases of **treatment resistance** where other modalities have failed.
- While the patient has significant symptoms of depression, there is no indication of immediate life-threatening severity (e.g., active suicidal intent with a plan) or treatment resistance to warrant ECT as a first-line option.
*Fluoxetine*
- **Fluoxetine** is a **selective serotonin reuptake inhibitor (SSRI)** and a common first-line treatment for major depressive disorder.
- While it would be effective for the patient's depression, it does not offer the additional specific benefit for **fibromyalgia pain** that an SNRI like venlafaxine provides through dual serotonin and norepinephrine reuptake inhibition.
Major depressive disorder diagnostic criteria US Medical PG Question 8: A previously healthy 56-year-old woman comes to the family physician for a 1-month history of sleep disturbance and sadness. The symptoms have been occurring since her husband died in a car accident. Before eventually falling asleep, she stays awake for multiple hours and has crying spells. Several times she has been woken up by the sound of her husband calling her name. She has lost 3 kg (6.6 lb) over the past month. She has 3 children with whom she still keeps regular contact and regularly attends church services with her friends. She expresses feeling a great feeling of loss over the death of her husband. She has no suicidal ideation. She is alert and oriented. Neurological exam shows no abnormalities. Which of the following is the most likely diagnosis for this patient's symptoms?
- A. Adjustment disorder with depressed mood
- B. Acute stress disorder
- C. Major depressive disorder
- D. Normal bereavement (Correct Answer)
- E. Schizoaffective disorder
Major depressive disorder diagnostic criteria Explanation: ***Normal bereavement***
- The patient's symptoms (sleep disturbance, sadness, weight loss, crying spells, auditory hallucinations of a loved one) are all **common and expected responses to the death of a loved one** within a short timeframe (1 month).
- Her continued social engagement and lack of suicidal ideation suggest that her grief, while intense, is within the range of **normal bereavement**, especially given the recent and traumatic loss.
*Adjustment disorder with depressed mood*
- This diagnosis is considered when symptoms in response to a stressor are **clinically significant** but do not meet criteria for a major depressive episode and cause significant impairment.
- However, in this case, the symptoms are directly related to the death of her husband, making **bereavement a more specific and appropriate diagnosis** if the symptoms are within normal grief.
*Acute stress disorder*
- This disorder typically involves exposure to actual or threatened **death, serious injury, or sexual violence**, followed by intrusive symptoms, negative mood, dissociation, avoidance, and arousal symptoms, and lasts from 3 days to 1 month.
- While there is a significant stressor (husband's death), her symptoms are more indicative of **grief and loss** rather than the specific dissociative, avoidance, and arousal symptom clusters required for acute stress disorder.
*Major depressive disorder*
- While some symptoms overlap (depressed mood, sleep disturbance, weight loss), several factors argue against MDD, such as the direct and recent link to a **major loss**, her **intact social functioning**, and the **absence of suicidal ideation** or pervasive anhedonia beyond grief.
- The **auditory hallucinations of her husband's voice** are also common in normal bereavement, especially shortly after a loss, and do not necessarily indicate a psychotic disorder or MDD with psychotic features in this context.
*Schizoaffective disorder*
- This diagnosis requires a **period of illness during which a major mood episode is present concurrently with Criterion A of schizophrenia** (delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, negative symptoms) and delusions or hallucinations for 2 or more weeks in the absence of a major mood episode.
- The patient's isolated auditory hallucination, occurring in the context of profound grief, does not meet the extensive criteria for schizophrenia or schizoaffective disorder, and there are **no other psychotic symptoms** or a history of such.
Major depressive disorder diagnostic criteria US Medical PG Question 9: A 22-year-old college student comes to the physician because of depressed mood and fatigue for the past 5 weeks. He has been feeling sad and unmotivated to attend his college classes. He finds it particularly difficult to get out of bed in the morning. He has difficulty concentrating during lectures and often feels that he is less intelligent compared to his classmates. In elementary school, he was diagnosed with attention deficit hyperactivity disorder and treated with methylphenidate; he stopped taking this medication 4 years ago because his symptoms had improved during high school. He has smoked two packs of cigarettes daily for 8 years; he feels guilty that he has been unable to quit despite numerous attempts. During his last attempt 3 weeks ago, he experienced increased appetite and subsequently gained 3 kg (6 lb 10 oz) in a week. Mental status examination shows psychomotor retardation and restricted affect. There is no evidence of suicidal ideation. Which of the following is the most appropriate pharmacotherapy?
- A. Amitriptyline
- B. Bupropion (Correct Answer)
- C. Lithium carbonate
- D. Fluoxetine
- E. Valproic acid
Major depressive disorder diagnostic criteria Explanation: ***Bupropion***
- Bupropion is an antidepressant that works as a **norepinephrine-dopamine reuptake inhibitor**. It is particularly effective for patients with **depressed mood, fatigue, and difficulty concentrating**, as seen in this patient.
- It is also beneficial for **nicotine cessation**, which aligns well with the patient's history of heavy smoking and failed attempts to quit.
*Amitriptyline*
- Amitriptyline is a **tricyclic antidepressant (TCA)** that can be sedating and has significant anticholinergic side effects, which might worsen the patient's fatigue and concentration difficulties.
- TCAs are generally **not first-line** due to their side effect profile and risk in overdose compared to newer antidepressants.
*Lithium carbonate*
- Lithium is primarily used as a **mood stabilizer** for **bipolar disorder** and is not a first-line treatment for major depressive disorder without manic or hypomanic symptoms.
- This patient's symptoms are indicative of depression, not bipolar illness.
*Fluoxetine*
- Fluoxetine is a **selective serotonin reuptake inhibitor (SSRI)**, a common first-line treatment for depression, but it might not be the most appropriate choice given this patient's specific presentation.
- SSRIs can sometimes cause **fatigue or sexual dysfunction**, and they don't offer the added benefit for smoking cessation that bupropion does.
*Valproic acid*
- Valproic acid is an **anticonvulsant** primarily used as a **mood stabilizer** for bipolar disorder or for seizure control, not as a primary antidepressant in unipolar depression.
- There is no indication in the patient's history or presentation to suggest bipolar disorder or a seizure disorder.
Major depressive disorder diagnostic criteria US Medical PG Question 10: A 22-year-old man comes to the physician because of generalized fatigue for the past 3 months. During this time, his grades have declined in his college courses because he has had difficulty focusing on assignments and sometimes sleeps in class. He no longer plays the drums for his band and has stopped attending family events. His temperature is 37°C (98.6°F), pulse is 60/min, and blood pressure is 130/80 mm Hg. Physical examination shows no abnormalities. On mental status examination, he describes his mood as “ok.” He has a flat affect. There is no evidence of suicidal ideation. His speech is slow in rate and monotone in rhythm, and his thought process is organized. He has no delusions or hallucinations. Which of the following is the most appropriate next step in treatment?
- A. Diazepam therapy
- B. Escitalopram therapy (Correct Answer)
- C. Phenelzine therapy
- D. Reassurance
- E. Amitriptyline therapy
Major depressive disorder diagnostic criteria Explanation: ***Escitalopram therapy***
- The patient presents with symptoms consistent with **major depressive disorder**: generalized fatigue, anhedonia (stopped playing drums, attending family events), poor concentration, and hypersomnia (sleeping in class) for 3 months.
- An **SSRI like escitalopram** is a first-line pharmacotherapy for MDD, particularly given its good tolerability profile and effectiveness in addressing core depressive symptoms.
*Diazepam therapy*
- **Diazepam is a benzodiazepine**, primarily used for acute anxiety or insomnia, and can be habit-forming.
- It is not indicated as a first-line treatment for major depressive disorder due to its addictive potential and lack of efficacy for core depressive symptoms.
*Phenelzine therapy*
- **Phenelzine is a MAOI (monoamine oxidase inhibitor)**, which are older antidepressants typically reserved for atypical depression or treatment-resistant depression due to their significant side effects and dietary restrictions.
- It is not appropriate as a first-line agent, especially given safer and equally effective options like SSRIs.
*Reassurance*
- The patient's symptoms are significant, persistent for 3 months, and causing functional impairment (decline in grades, social withdrawal); therefore, **simple reassurance is insufficient** and would delay appropriate treatment.
- These symptoms warrant a more proactive and evidence-based therapeutic approach.
*Amitriptyline therapy*
- **Amitriptyline is a TCA (tricyclic antidepressant)**, which are generally associated with a higher incidence of side effects, such as anticholinergic effects, sedation, and cardiac conduction abnormalities, compared to SSRIs.
- While effective for depression, it is typically not a first-line treatment due to its less favorable side effect profile compared to SSRIs like escitalopram.
More Major depressive disorder diagnostic criteria US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.