Depression with psychotic features US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Depression with psychotic features. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Depression with psychotic features US Medical PG Question 1: A 26-year-old man is brought to the emergency department by his wife because of bizarre and agitated behavior for the last 6 weeks. He thinks that the NSA is spying on him and controlling his mind. His wife reports that the patient has become withdrawn and at times depressed for the past 3 months. He lost his job because he stopped going to work 4 weeks ago. Since then, he has been working on an invention that will block people from being able to control his mind. Physical and neurologic examinations show no abnormalities. On mental status examination, he is confused and suspicious with marked psychomotor agitation. His speech is disorganized and his affect is labile. Which of the following is the most likely diagnosis?
- A. Brief psychotic disorder
- B. Schizophreniform disorder (Correct Answer)
- C. Schizotypal personality disorder
- D. Schizophrenia
- E. Delusional disorder
Depression with psychotic features Explanation: ***Schizophreniform disorder***
- The patient's symptoms, including **delusions** (fixed false beliefs that the NSA is spying and controlling his mind), **disorganized speech**, and **agitated behavior**, are consistent with a psychotic disorder.
- The duration of active psychotic symptoms (6 weeks), which is more than 1 month but less than 6 months, fits the diagnostic criteria for **schizophreniform disorder**.
- The prodromal phase (withdrawn and depressed for 3 months) plus the active phase does not yet meet the 6-month requirement for schizophrenia.
*Brief psychotic disorder*
- This disorder is characterized by a sudden onset of psychotic symptoms lasting less than 1 month, followed by a full return to premorbid functioning.
- The patient's active psychotic symptoms have persisted for 6 weeks, exceeding the maximum duration for brief psychotic disorder.
*Schizotypal personality disorder*
- This disorder primarily involves a pervasive pattern of social and interpersonal deficits marked by acute discomfort with close relationships, as well as cognitive or perceptual distortions and eccentricities.
- While there might be odd beliefs or magical thinking, it does not typically involve the persistent and severe delusions and disorganized speech seen in this case.
- This is a personality disorder, not a psychotic disorder.
*Schizophrenia*
- Schizophrenia requires continuous signs of disturbance for at least 6 months, which includes at least 1 month of active-phase symptoms (delusions, hallucinations, disorganized speech).
- The patient's total duration of illness (3 months of prodromal symptoms plus 6 weeks of active symptoms) totals approximately 4.5 months, which is less than the 6-month minimum duration required for a diagnosis of schizophrenia.
*Delusional disorder*
- The primary feature of delusional disorder is the presence of one or more delusions for at least 1 month, without other prominent psychotic symptoms such as disorganized speech or behavior.
- This patient exhibits prominent **disorganized speech**, **labile affect**, and **disorganized behavior** (bizarre invention work), which are not characteristic of delusional disorder.
- Functioning is more impaired than typically seen in delusional disorder.
Depression with psychotic features US Medical PG Question 2: A 32-year-old man comes to the physician because of a 2 month history of difficulty sleeping and worsening fatigue. During this time, he has also had difficulty concentrating and remembering tasks at work as well as diminished interest in his hobbies. He has no suicidal or homicidal ideation. He does not have auditory or visual hallucinations. Vital signs are normal. Physical examination shows no abnormalities. Mental status examination shows a depressed mood and flat affect with slowed thinking and speech. The physician prescribes sertraline. Three weeks later, the patient comes to the physician again with only minor improvements in his symptoms. Which of the following is the most appropriate next step in management?
- A. Augment with aripiprazole and continue sertraline
- B. Provide electroconvulsive therapy
- C. Continue sertraline for 3 more weeks (Correct Answer)
- D. Change medication to duloxetine
- E. Augment with phenelzine and continue sertraline
Depression with psychotic features Explanation: ***Continue sertraline for 3 more weeks***
- Antidepressants like **sertraline** typically require **4 to 6 weeks** to reach their full therapeutic effect.
- Since only three weeks have passed with minor improvements, the patient should continue the medication to allow time for the drug to work fully.
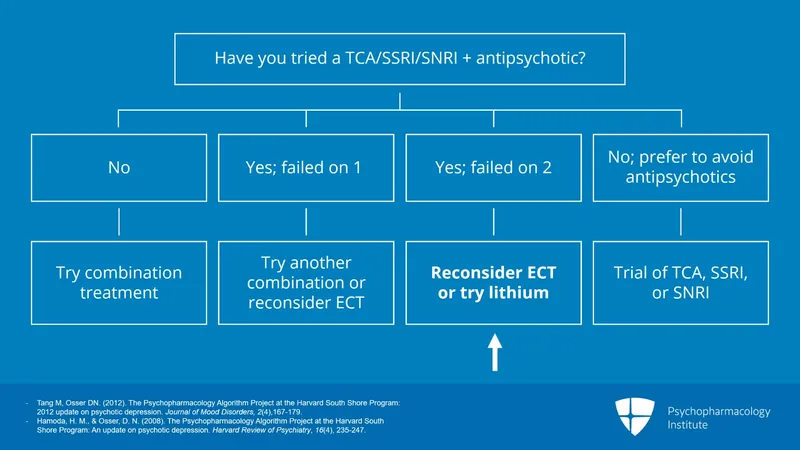
*Augment with aripiprazole and continue sertraline*
- **Augmentation** with an atypical antipsychotic like aripiprazole is considered if there is **no significant improvement after an adequate trial** (at least 6-8 weeks) of antidepressant monotherapy.
- It is too early to consider augmentation as the patient has not completed a sufficient trial of sertraline.
*Provide electroconvulsive therapy*
- **Electroconvulsive therapy (ECT)** is reserved for **severe, treatment-resistant depression**, depression with psychotic features, or when rapid response is required (e.g., severe suicidality).
- The patient's symptoms, while bothersome, do not meet criteria for severe, treatment-resistant depression or acute emergencies warranting ECT.
*Change medication to duloxetine*
- Changing antidepressants is usually considered if there is **minimal or no response** after an adequate trial of the initial medication.
- Switching medications before allowing sufficient time for the current treatment to work is premature and may delay effective treatment.
*Augment with phenelzine and continue sertraline*
- **Phenelzine** is a **monoamine oxidase inhibitor (MAOI)**, and using it in combination with an **SSRI like sertraline** is contraindicated due to the risk of **serotonin syndrome**.
- MAOIs are generally reserved for **refractory depression** due to their dietary restrictions and potential for severe drug interactions.
Depression with psychotic features US Medical PG Question 3: A 57-year-old man is brought to the emergency department by the police after he was found running around a local park naked and screaming late at night. During intake, the patient talks non-stop about the government spying on him and his family, but provides little useful information besides his name and date of birth. Occasionally he refers to himself in the third person. He refuses to eat anything and will only drink clear fluids because he is afraid of being poisoned. A medical records search reveals that the patient has been treated for psychotic behavior and occasional bouts of severe depression for several years. Today, his heart rate is 90/min, respiratory rate is 19/min, blood pressure is 135/85 mm Hg, and temperature is 37.0°C (98.6°F). On physical exam, he appears gaunt and anxious. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. CMP, CBC, and TSH are normal. A urine toxicology test is negative. What is the most likely diagnosis?
- A. Schizophrenia
- B. Major depressive disorder
- C. Schizoaffective disorder (Correct Answer)
- D. Brief psychotic disorder
- E. Bipolar 1 disorder
Depression with psychotic features Explanation: ***Schizoaffective disorder***
- The patient exhibits features of both a **mood disorder** (severe depression) and a **psychotic disorder** (delusions, disorganized behavior, referring to himself in the third person), which are key characteristics of schizoaffective disorder.
- The history of **psychotic behavior** and **severe depression** over several years, with current presentation involving both prominent mood symptoms (agitation, gaunt appearance suggesting poor self-care due to mood) and psychotic features (paranoia, disorganized speech), supports this diagnosis over other psychotic or mood disorders.
*Schizophrenia*
- While the patient exhibits **psychotic symptoms** (delusions, disorganization), the history of "occasional bouts of severe depression" suggests a more prominent and recurring mood component than typically seen in schizophrenia.
- In schizophrenia, mood symptoms are often confined to brief periods relative to the duration of the psychotic illness or are not a prominent and defining feature.
*Major depressive disorder*
- This diagnosis is incorrect because the patient displays clear and pervasive **psychotic symptoms** such as paranoia, disorganized speech, and bizarre behavior (running naked, screaming), which are beyond what is typically seen in major depressive disorder with psychotic features (where psychosis is congruent with the depressive theme).
- The historical pattern of **psychotic behavior** occurring separately from or alongside depressive episodes points away from a primary diagnosis of major depressive disorder.
*Brief psychotic disorder*
- This diagnosis is characterized by psychotic symptoms lasting **less than one month**, with an eventual full return to premorbid functioning.
- The patient's history of **several years** of psychotic behavior and severe depression rules out this acute and time-limited condition.
*Bipolar 1 disorder*
- While bipolar 1 disorder can feature **psychotic symptoms** during manic or depressive episodes, the presentation here emphasizes persistent psychotic features (delusions of being spied on, fear of poisoning) that are not always directly tied to mood episodes or are more enduring than typical for bipolar disorder.
- The long-standing history of both **psychotic and depressive episodes** suggests a more integrated condition of mood and psychosis rather than distinct episodes as seen in bipolar 1 disorder.
Depression with psychotic features US Medical PG Question 4: A 24-year-old woman is brought to the emergency department by her roommate because of bizarre behavior and incoherent talkativeness for the past week. Her roommate reports that the patient has been rearranging the furniture in her room at night and has ordered a variety of expensive clothes online. The patient says she feels “better than ever” and has a lot of energy. She had absence seizures as a child and remembers that valproate had to be discontinued because it damaged her liver. She has been otherwise healthy and is not taking any medication. She is sexually active with her boyfriend. She does not smoke, drink alcohol, or use illicit drugs. Physical and neurologic examinations show no abnormalities. Her pulse is 78/min, respirations are 13/min, and blood pressure is 122/60 mm Hg. Mental status examination shows pressured and disorganized speech, flight of ideas, lack of insight, and affective lability. Which of the following is the best initial step before deciding on a therapy for this patient's condition?
- A. Obtain CBC, liver function studies, and beta-HCG
- B. Obtain TSH, β-hCG, and serum creatinine concentration (Correct Answer)
- C. Obtain BMI, HbA1c, lipid levels, and prolactin levels
- D. Perform urine drug testing and begin cognitive behavior therapy
- E. Assess for suicidal ideation and obtain echocardiography
Depression with psychotic features Explanation: ***Obtain TSH, β-hCG, and serum creatinine concentration***
- This patient presents with symptoms highly suggestive of **mania** (bizarre behavior, incoherent talkativeness, grandiosity, increased energy, pressured speech, flight of ideas). Before initiating treatment, it's crucial to rule out other medical conditions that can **mimic mania**, such as **hyperthyroidism** (TSH), **pregnancy** (β-hCG), or **kidney dysfunction** (creatinine), which can impact medication choice and dosage.
- TSH levels are essential as **hyperthyroidism** can cause symptoms like agitation, rapid speech, and increased energy, mimicking mania. A **pregnancy test (β-hCG)** is critical for women of childbearing age to ensure that any potential psychiatric medications are safe for both the mother and fetus. **Serum creatinine** helps assess kidney function, which is important for dosing many psychotropic medications eliminated by the kidneys.
*Obtain CBC, liver function studies, and beta-HCG*
- While a **β-hCG** is appropriate, **CBC** and **liver function studies (LFTs)** are typically obtained if there are specific concerns for anemia, infection, or liver damage (which the patient mentions about valproate in childhood, but there's no immediate indication for current LFTs before diagnosis confirmation).
- Although LFTs are important for certain antidepressant or mood stabilizer monitoring (e.g., valproate, carbamazepine), they are not the most immediate initial screen for ruling out medical mimics of mania in this context as **TSH** and **renal function** are more critical.
*Obtain BMI, HbA1c, lipid levels, and prolactin levels*
- These tests are important for **monitoring long-term metabolic side effects** of certain antipsychotics and mood stabilizers, but they are not the best initial steps for ruling out acute medical causes of manic symptoms.
- **BMI, HbA1c, and lipid levels** are typically assessed *after* diagnosis and initiation of treatment to establish a baseline for future metabolic monitoring. **Prolactin levels** might be checked if there is concern for hyperprolactinemia, which is a side effect of some antipsychotics, but not usually a cause of acute mania.
*Perform urine drug testing and begin cognitive behavior therapy*
- While **urine drug testing** is often performed in acute psychiatric presentations to rule out substance-induced mania, it is not listed as the *best initial step* alone, as other medical conditions also need to be ruled out concurrently.
- **Cognitive behavioral therapy (CBT)** is not an appropriate initial treatment for acute mania due to the patient's severe symptoms, lack of insight, and disorganized thought processes. **Pharmacotherapy** is the cornerstone of acute mania management.
*Assess for suicidal ideation and obtain echocardiography*
- Assessing for **suicidal ideation** is crucial in every psychiatric evaluation, but it is a mental status component rather than a diagnostic lab test. While important for patient safety, it doesn't rule out medical mimics of mania.
- **Echocardiography** is not indicated in the initial work-up of acute mania unless there are specific cardiac symptoms or a history that suggests underlying heart disease.
Depression with psychotic features US Medical PG Question 5: A 31-year-old G1P0 woman is brought into the emergency room by the police after a failed suicide attempt. She jumped off a nearby bridge but was quickly rescued by some nearby locals. The height of the bridge was not significant, so the patient did not sustain any injuries. For the 3 weeks before this incident, the patient says she had been particularly down, lacking energy and unable to focus at home or work. She says she no longer enjoys her usual hobbies or favorite meals and is not getting enough sleep. Which of the following is the best course of treatment for this patient?
- A. Bupropion
- B. Paroxetine
- C. Combination of SSRI and SNRI
- D. Phenelzine
- E. Electroconvulsive therapy (Correct Answer)
Depression with psychotic features Explanation: ***Electroconvulsive therapy***
- This patient presents with **severe depression with suicidal ideation** (a failed suicide attempt), which warrants urgent intervention. **ECT** is highly effective for severe depression, especially when there is an acute suicide risk or psychotic features.
- ECT has a **rapid onset of action** compared to antidepressants, which is crucial for patients at high risk of self-harm, and is considered **safe in pregnancy**.
*Bupropion*
- **Bupropion** is an antidepressant that primarily inhibits the reuptake of norepinephrine and dopamine. While effective for depression, it has a slower onset of action than ECT and may not be sufficient for severe, acute suicidal ideation.
- It is often used for depression with atypical features or for patients who experience sexual side effects with SSRIs, but it is **contraindicated in patients with a history of seizures or eating disorders**.
*Paroxetine*
- **Paroxetine** is an SSRI commonly used for depression and anxiety disorders. Like other antidepressants, it has a delayed onset of action (several weeks) and may not be appropriate for the immediate management of a patient with recent, severe suicidal ideation.
- One of the major concerns with paroxetine in this patient population is that it has a **higher rate of teratogenicity and neonatal complications** compared to other SSRIs, which is relevant given the patient is G1P0.
*Combination of SSRI and SNRI*
- Combining an **SSRI and an SNRI** (e.g., fluoxetine and venlafaxine) is a strategy sometimes used for treatment-resistant depression. However, like monotherapy with these agents, it still has a delayed onset of action.
- The combination also carries a **higher risk of side effects** compared to monotherapy.
*Phenelzine*
- **Phenelzine** is a monoamine oxidase inhibitor (MAOI). MAOIs are effective antidepressants but are typically reserved for **treatment-resistant depression** due to their significant drug-drug and drug-food interactions (e.g., **hypertensive crisis with tyramine-rich foods or sympathomimetics**).
- Given the patient's acute suicidal risk, a treatment with a more rapid and safer profile, such as ECT, would be preferred over initiating an MAOI.
Depression with psychotic features US Medical PG Question 6: A 24-year-old woman is brought to the hospital by her mother because she has "not been herself" for the past 3 months. The patient says she hears voices in her head. The mother said that when she is talking to her daughter she can’t seem to make out what she is saying; it is as if her thoughts are disorganized. When talking with the patient, you notice a lack of energy and an apathetic affect. Which of the following is the most likely diagnosis for this patient?
- A. Major depressive disorder
- B. Schizophrenia
- C. Brief psychotic disorder
- D. Schizotypal disorder
- E. Schizophreniform disorder (Correct Answer)
Depression with psychotic features Explanation: ***Schizophreniform disorder***
- The patient exhibits core **psychotic symptoms** (hearing voices, disorganized thoughts) for a duration of **3 months**, which is characteristic of schizophreniform disorder (symptoms lasting **1 to 6 months**).
- Her **lack of energy** and **apathetic affect** align with the negative symptoms commonly seen in psychotic disorders.
*Major depressive disorder*
- While **lack of energy** and **apathetic affect** can be present, the prominent **hallucinations** (hearing voices) and **disorganized thoughts** are not primary features of major depressive disorder.
- A diagnosis of depression alone would not fully account for her psychotic symptoms.
*Schizophrenia*
- Schizophrenia requires symptoms to be present for **at least 6 months**, including at least one month of **active phase symptoms**. This patient's symptoms have only been present for 3 months.
- While the symptoms are consistent with schizophrenia, the **duration criterion** has not yet been met.
*Brief psychotic disorder*
- Brief psychotic disorder is characterized by psychotic symptoms lasting **less than 1 month**. This patient's symptoms have been ongoing for 3 months.
- The chronicity of symptoms makes this diagnosis unlikely.
*Schizotypal disorder*
- Schizotypal disorder is a **personality disorder** characterized by peculiar thoughts and behaviors, but typically **without overt psychotic episodes** or pronounced disorganized speech/hallucinations as described.
- While there may be odd beliefs or ideas of reference, the clear **auditory hallucinations** and **thought disorder** in this case point to a more severe psychotic condition.
Depression with psychotic features US Medical PG Question 7: A 42-year-old female presents to her primary care provider for an annual checkup. She reports feeling sad over the past few months for no apparent reason. She has lost interest in swimming, which she previously found enjoyable. Additionally, she has had trouble getting a full night’s sleep and has had trouble concentrating during the day. She has lost 15 pounds since her last visit one year prior. Which of the following sets of neurotransmitter levels is associated with this patient’s condition?
- A. Decreased acetylcholine, normal serotonin, normal dopamine
- B. Decreased norepinephrine, decreased serotonin, decreased dopamine (Correct Answer)
- C. Decreased GABA, decreased acetylcholine, increased dopamine
- D. Increased norepinephrine, decreased serotonin, decreased GABA
- E. Increased acetylcholine, increased serotonin, decreased dopamine
Depression with psychotic features Explanation: ***Decreased norepinephrine, decreased serotonin, decreased dopamine***
- The patient's symptoms of **sadness**, loss of interest (**anhedonia**), **insomnia**, **difficulty concentrating**, and **weight loss** are classic for **major depressive disorder**.
- **Depression** is strongly associated with deficiencies in **monoamine neurotransmitters**: **norepinephrine**, **serotonin**, and **dopamine**.
*Decreased acetylcholine, normal serotonin, normal dopamine*
- While **acetylcholine** is involved in mood regulation, its isolated decrease with normal serotonin and dopamine levels is not characteristic of generalized depression.
- More prominent roles for **acetylcholine dysfunction** are seen in conditions like **Alzheimer's disease** or **myasthenia gravis**.
*Decreased GABA, decreased acetylcholine, increased dopamine*
- **Decreased GABA** is often associated with **anxiety disorders** and seizures, not the primary presentation of depression here.
- **Increased dopamine** is more characteristic of conditions like **schizophrenia** or **mania**, which contrasts with the patient's depressive symptoms.
*Increased norepinephrine, decreased serotonin, decreased GABA*
- **Increased norepinephrine** is typically associated with **anxiety**, **stress**, or sometimes **mania**, which is inconsistent with this patient's depressive state.
- While **decreased serotonin** is correct for depression, the combination with increased norepinephrine and decreased GABA does not fit the typical neurotransmitter profile.
*Increased acetylcholine, increased serotonin, decreased dopamine*
- **Increased acetylcholine** is generally not associated with the full spectrum of depressive symptoms described.
- **Increased serotonin** is often the goal of antidepressant treatments (SSRIs), making an endogenous increase unlikely to cause depression.
Depression with psychotic features US Medical PG Question 8: A 20-year-old man is brought to the behavioral health clinic by his roommate. The patient’s roommate says that the patient has been looking for cameras that aliens planted in their apartment for the past 2 weeks. Approximately 3 months prior to the onset of this episode, the roommate says the patient stopped playing basketball daily because the sport no longer interested him. He stayed in his bedroom most of the day and was often tearful. The roommate recalls the patient talking about death frequently. The patient states he has been skipping many meals and has lost a significant amount of weight as a result. At the time his delusions about the aliens began, the depressive-related symptoms were no longer present. He has no other medical conditions. He does not drink but smokes 2 packs of cigarettes daily for the past 5 years. His vitals include: blood pressure 130/88 mm Hg, pulse 92/min, respiratory rate 16/min, temperature 37.3°C (99.1°F). On physical examination, the patient seems apathetic and uses an obscure word that appears to be ‘chinterfittle’. His affect is flat throughout the entire interaction. He is experiencing bizarre delusions but no hallucinations. The patient does not express suicidal or homicidal ideations. Urine drug screen results are provided below:
Amphetamine negative
Benzodiazepine negative
Cocaine negative
GHB negative
Ketamine negative
LSD negative
Marijuana positive
Opioids negative
PCP negative
Which of the following is the correct diagnosis?
- A. Depression with psychotic features
- B. Cannabis intoxication
- C. Schizophrenia with depression
- D. Schizoaffective disorder (Correct Answer)
- E. Brief psychotic disorder
Depression with psychotic features Explanation: ***Schizoaffective disorder***
- The patient experienced a **major depressive episode** (anhedonia, tearfulness, frequent talk of death, weight loss) lasting approximately 3 months, followed by **psychotic symptoms** (bizarre delusions) for 2 weeks.
- For **schizoaffective disorder**, the key criteria are: (1) mood symptoms present for the **majority** of the total illness duration, and (2) psychotic symptoms for **≥2 weeks in the absence of mood symptoms**.
- This case satisfies both: mood symptoms were present for ~3 out of 3.5 months (~85% of illness), and psychotic symptoms have been present for 2 weeks after mood symptoms resolved.
- This is **schizoaffective disorder, depressive type**.
*Depression with psychotic features*
- In **depression with psychotic features**, the psychotic symptoms (delusions or hallucinations) occur **only during** the depressive episode.
- The patient's depressive symptoms had **resolved** before the onset of his psychotic symptoms, which rules out this diagnosis.
*Cannabis intoxication*
- While the patient has a **positive marijuana screen**, his symptoms have been ongoing for **two weeks**, which is inconsistent with acute cannabis intoxication.
- The presence of a clear antecedent major depressive episode also points away from this being purely substance-induced.
*Schizophrenia with depression*
- For a diagnosis of **schizophrenia**, mood symptoms should be present for a **minority** of the total duration of the illness.
- In this case, depressive symptoms were present for the **majority** (~85%) of the total illness duration, which distinguishes this from schizophrenia.
*Brief psychotic disorder*
- **Brief psychotic disorder** is characterized by psychotic symptoms lasting **less than 1 month** with eventual full return to baseline.
- While the patient's psychotic symptoms have been present for only 2 weeks so far, the overall clinical picture with a prolonged prior depressive episode and ongoing illness course suggests a more chronic condition consistent with schizoaffective disorder.
Depression with psychotic features US Medical PG Question 9: A 25-year-old woman is brought to the emergency department by EMS after being found naked in a busy downtown square. The patient stated that she is liberating people from material desires and was found destroying objects. Her temperature is 99.5°F (37.5°C), blood pressure is 127/68 mmHg, pulse is 120/min, respirations are 22/min, and oxygen saturation is 98% on room air. Physical exam is deferred due to patient combativeness. The patient is given diphenhydramine and haloperidol and transferred to the psychiatric ward. On day 1 on the ward, the patient is no longer aggressive or agitated and has calmed down. She states that she feels severely depressed and wants to kill herself. The patient is started on a medication and monitored closely. On day 3 of the patient's stay in the hospital she is found in her room drawing up plans and states that she has major plans to revamp the current energy problems in the country. Which of the following is the most likely medication that was started in this patient?
- A. Quetiapine
- B. Olanzapine
- C. Lamotrigine
- D. Sertraline (Correct Answer)
- E. Lithium
Depression with psychotic features Explanation: ***Sertraline***
- This patient exhibits classic **bipolar I disorder** with rapid mood cycling from **mania** (naked in public, grandiose delusions, destroying objects) to **severe depression** (suicidal ideation on Day 1) and back to **mania** (grandiose plans on Day 3).
- The key clinical clue is the **rapid return to mania by Day 3** after starting medication during the depressive phase. This suggests **antidepressant-induced mania/mood switch**, a well-known complication of using **SSRI antidepressants** (like sertraline) **without adequate mood stabilization** in bipolar disorder.
- **Antidepressants can precipitate manic episodes** within days in bipolar patients, which is why they should be avoided or used only with concomitant mood stabilizers. This question tests recognition of this critical psychiatric principle.
*Lithium*
- Lithium is a first-line **mood stabilizer** for bipolar disorder and would be appropriate for long-term management. However, lithium **prevents manic episodes** rather than causing them.
- Lithium takes **1-2 weeks to reach therapeutic levels**, so it would not explain the rapid mood switch to mania by Day 3. If lithium had been started, we would expect **stabilization or improvement**, not a return to mania.
*Quetiapine*
- Quetiapine is an **atypical antipsychotic** effective for both acute mania and bipolar depression. It can provide rapid mood stabilization.
- If quetiapine was started on Day 1, we would expect **mood stabilization or sedation**, not a switch back to mania. Quetiapine does **not precipitate manic episodes**.
*Olanzapine*
- Olanzapine is another **atypical antipsychotic** used for acute mania and maintenance in bipolar disorder.
- Like quetiapine, olanzapine would **stabilize mood** and reduce manic symptoms, not trigger them. It would not explain the return to mania on Day 3.
*Lamotrigine*
- Lamotrigine is a mood stabilizer particularly effective for **preventing depressive episodes** in bipolar disorder, though less effective for acute mania.
- Lamotrigine **does not precipitate manic episodes** and takes weeks to titrate to therapeutic doses due to risk of Stevens-Johnson syndrome. It would not explain the rapid mood switch observed here.
Depression with psychotic features US Medical PG Question 10: A 30-year-old man presents with fatigue and low energy. He says that he has been "feeling down" and tired on most days for the last 3 years. He also says that he has had difficulty concentrating and has been sleeping excessively. The patient denies any manic or hypomanic symptoms. He also denies any suicidal ideation or preoccupation with death. A physical examination is unremarkable. Laboratory findings are significant for the following:
Serum glucose (fasting) 88 mg/dL
Serum electrolytes Sodium 142 mEq/L; Potassium: 3.9 mEq/L; Chloride: 101 mEq/L
Serum creatinine 0.8 mg/dL
Blood urea nitrogen 10 mg/dL
Hemoglobin (Hb %) 15 g/dL
Mean corpuscular volume (MCV) 85 fl
Reticulocyte count 1%
Erythrocyte count 5.1 million/mm3
Thyroid-stimulating hormone 3.5 μU/mL
Medication is prescribed to this patient that increases norepinephrine neurotransmission. After 2 weeks, the patient returns for follow-up and complains of dizziness, dry mouth, and constipation. Which of the following drugs was most likely prescribed to this patient?
- A. Clonidine
- B. Lithium
- C. Paroxetine
- D. Venlafaxine (Correct Answer)
- E. Phenylephrine
Depression with psychotic features Explanation: ***Venlafaxine***
- This patient likely suffers from **persistent depressive disorder (dysthymia)** given the chronic fatigue, low energy, and depressed mood for over 2 years without manic/hypomanic episodes.
- **Venlafaxine** is a **serotonin-norepinephrine reuptake inhibitor (SNRI)** that increases both serotonin and norepinephrine levels by blocking their reuptake at nerve terminals, thereby enhancing norepinephrine neurotransmission.
- Common side effects include **dizziness, dry mouth, and constipation** due to anticholinergic effects and increased noradrenergic activity.
*Clonidine*
- **Clonidine** is an **alpha-2 adrenergic agonist** that reduces sympathetic outflow by activating presynaptic alpha-2 receptors, effectively decreasing norepinephrine release, which is contrary to the question's premise of increasing norepinephrine neurotransmission.
- It is primarily used to treat **hypertension** and **ADHD**, and its side effects can include sedation and dry mouth, but it would not be prescribed to enhance norepinephrine activity.
*Lithium*
- **Lithium** is a mood stabilizer primarily used in the treatment of **bipolar disorder** and is not typically prescribed as a standalone antidepressant to increase norepinephrine neurotransmission.
- Its side effects include **tremor, polyuria, polydipsia, and thyroid dysfunction**, which do not match the described side effect profile.
*Paroxetine*
- **Paroxetine** is a **selective serotonin reuptake inhibitor (SSRI)**, primarily increasing serotonin levels. It does not significantly increase norepinephrine neurotransmission.
- While it can cause side effects like **dry mouth and constipation**, it would not fit the description of a drug that increases norepinephrine neurotransmission.
*Phenylephrine*
- **Phenylephrine** is an **alpha-1 adrenergic agonist** used as a decongestant or to increase blood pressure by directly stimulating postsynaptic alpha-1 receptors rather than enhancing neurotransmission through reuptake inhibition.
- It would not be used to treat depression, and its side effects include **hypertension and reflex bradycardia**, which are not reported in the patient.
More Depression with psychotic features US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.