Depression with atypical features US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Depression with atypical features. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Depression with atypical features US Medical PG Question 1: A 65-year-old male who is being treated for depression visits your emergency room complaining of being unable to urinate. In addition, the patient complains of tachycardia and dry mouth. He has no history of benign prostatic hyperplasia and reports of only being on one psychiatric medication. What type of psychiatric medication would cause such a side effect profile?
- A. Tricyclic antidepressant (Correct Answer)
- B. Serotonin norepinephrine reuptake inhibitor
- C. Monoamine oxidase inhibitor
- D. Selective serotonin reuptake inhibitor
- E. Aminoketone
Depression with atypical features Explanation: ***Tricyclic antidepressant***
- The patient's symptoms of **urinary retention**, dry mouth, and tachycardia are characteristic **anticholinergic side effects**, frequently seen with TCAs.
- TCAs block muscarinic acetylcholine receptors, leading to these peripheral effects.
*Serotonin norepinephrine reuptake inhibitor*
- SNRIs primarily affect serotonin and norepinephrine reuptake and are less likely to cause severe anticholinergic effects like urinary retention.
- While they can cause some dry mouth or tachycardia due to noradrenergic effects, the combination with significant urinary retention points away from SNRIs.
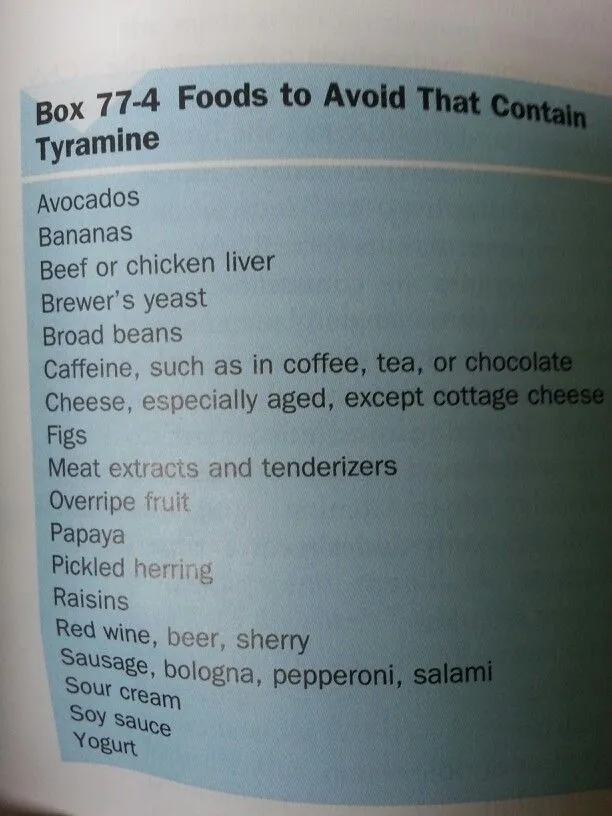
*Monoamine oxidase inhibitor*
- MAOIs are generally associated with side effects such as **hypertensive crisis** (with tyramine-rich foods), orthostatic hypotension, and insomnia.
- They do not typically cause the prominent anticholinergic syndrome described.
*Selective serotonin reuptake inhibitor*
- SSRIs primarily affect serotonin reuptake and are known for side effects such as **gastrointestinal upset**, sexual dysfunction, and anxiety.
- They have a low affinity for muscarinic receptors and are less likely to cause significant anticholinergic effects like urinary retention.
*Aminoketone*
- Aminoketones (e.g., bupropion) typically act by inhibiting the reuptake of dopamine and norepinephrine.
- Common side effects include **insomnia**, agitation, and **seizure risk** at high doses; they do not typically produce the anticholinergic profile seen here.
Depression with atypical features US Medical PG Question 2: A 28-year-old woman presents with depressed mood lasting for most days of the week for the past month. She also mentions that she has lost her appetite for the past 3 weeks. She adds that her job performance has significantly deteriorated because of these symptoms, and she feels like she will have to quit her job soon. Upon asking about her hobbies, she says that she used to enjoy dancing and music but does not have any desire to do them anymore. The patient’s husband says that she has had many sleepless nights last month. The patient denies any history of smoking, alcohol intake, or use of illicit substances. No significant past medical history. Physical examination is unremarkable. Routine laboratory tests are all within normal limits. Which of the following clinical features must be present, in addition to this patient’s current symptoms, to confirm the diagnosis of a major depressive episode?
- A. Intense fear of losing control
- B. Lack of concentration (Correct Answer)
- C. Weight loss
- D. Anterograde amnesia
- E. Nightmares
Depression with atypical features Explanation: ***Lack of concentration***
- The diagnostic criteria for a **major depressive episode** (DSM-5) require at least **5 out of 9 cardinal symptoms** present for at least 2 weeks, with at least one being either **depressed mood** or **anhedonia**.
- This patient currently has **4 symptoms**: (1) depressed mood, (2) anhedonia (loss of interest in dancing/music), (3) appetite disturbance (loss of appetite), and (4) sleep disturbance (insomnia).
- To meet diagnostic criteria, she needs **one more symptom** from the remaining options: fatigue, feelings of worthlessness/guilt, **diminished ability to concentrate or indecisiveness**, psychomotor changes, or suicidal ideation.
- **Lack of concentration** is one of the DSM-5 diagnostic criteria and would bring her total to 5 symptoms, confirming the diagnosis.
*Intense fear of losing control*
- This symptom is characteristic of **panic disorder** or anxiety disorders, where individuals experience sudden, intense episodes of fear with accompanying physical and cognitive symptoms.
- While anxiety can co-occur with depression, intense fear of losing control is **not a DSM-5 diagnostic criterion** for major depressive episode.
*Weight loss*
- The patient already has **loss of appetite**, which satisfies the weight/appetite criterion for major depressive episode.
- **Weight loss and appetite changes are part of the same diagnostic criterion**, not separate ones. Therefore, weight loss would not add an additional criterion to reach the required 5 symptoms.
- While clinically significant weight loss can occur in depression, it would not provide the "additional" criterion needed in this case.
*Anterograde amnesia*
- **Anterograde amnesia** (inability to form new memories) is associated with neurological conditions such as **hippocampal damage**, **Korsakoff syndrome**, or **traumatic brain injury**.
- It is **not a DSM-5 diagnostic criterion** for major depressive episode, though some cognitive impairment (concentration difficulties) may occur.
*Nightmares*
- The patient already has **insomnia** (sleep disturbance), which is one of the DSM-5 diagnostic criteria.
- While nightmares may occur in depression, they are not a separate diagnostic criterion and would not add to the symptom count since sleep disturbance is already present.
Depression with atypical features US Medical PG Question 3: A 25-year-old woman comes to the physician because of sadness that started 3 weeks after her daughter was born. Her daughter is now 9 months old and usually sleeps through the night, but the patient still has difficulty staying asleep. She has not returned to work since the birth. She is easily distracted from normal daily tasks. She used to enjoy cooking, but only orders delivery or take-out now. She says that she always feels too exhausted to do so and does not feel hungry much anyway. The pregnancy of the patient's child was complicated by gestational diabetes. The child was born at 36-weeks' gestation and has had no medical issues. The patient has no contact with the child's father. She is not sexually active. She does not smoke, drink alcohol, or use illicit drugs. She is 157 cm (5 ft 1 in) tall and weighs 47 kg (105 lb); BMI is 20 kg/m2. Vital signs are within normal limits. She is alert and cooperative but makes little eye contact. Physical examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Adjustment disorder
- B. Major depressive disorder
- C. Normal behavior
- D. Disruptive mood dysregulation disorder
- E. Depression with peripartum-onset (Correct Answer)
Depression with atypical features Explanation: ***Depression with peripartum-onset***
- The patient exhibits classic symptoms of **major depressive disorder**, including **anhedonia** (loss of enjoyment in cooking), **fatigue**, **insomnia**, and **changes in appetite/weight**, all appearing within 3 weeks post-childbirth and persisting for 9 months.
- According to **DSM-5-TR**, the **peripartum onset specifier** is applied when a major depressive episode begins during pregnancy or **within 4 weeks after delivery**.
- This patient's symptoms began at 3 weeks postpartum, meeting criteria for the peripartum onset specifier, which is clinically important for risk assessment (including infanticide risk) and treatment planning.
- The severity and duration of symptoms (persistent anhedonia, significant fatigue, insomnia despite adequate opportunity for sleep, appetite changes, functional impairment lasting months) clearly meet criteria for a **major depressive episode**.
*Adjustment disorder*
- This diagnosis involves emotional or behavioral symptoms in response to an identifiable stressor that do **not meet criteria for a major depressive episode**.
- The severity, number, and duration of symptoms (anhedonia, significant fatigue, insomnia, appetite changes, functional impairment lasting 9 months) exceed what is seen in adjustment disorder and meet full criteria for **major depressive disorder**.
*Major depressive disorder*
- While this patient's symptoms fully meet criteria for **Major Depressive Disorder (MDD)**, the onset within 4 weeks postpartum requires the addition of the **"with peripartum onset" specifier** per DSM-5-TR.
- Using the peripartum onset specifier is essential for clinical management, as it alerts clinicians to specific risks (including thoughts of harming the infant) and may influence treatment selection (e.g., considerations for breastfeeding-compatible medications).
*Normal behavior*
- The patient's symptoms—including **persistent sadness lasting 9 months**, **anhedonia**, **insomnia despite adequate sleep opportunity**, **significant fatigue**, **appetite loss**, and **inability to return to work**—represent severe functional impairment.
- These symptoms far exceed normal postpartum adjustment or transient "baby blues" (which typically resolve within 2 weeks postpartum) and indicate a serious mood disorder requiring treatment.
*Disruptive mood dysregulation disorder*
- This disorder is diagnosed **only in children and adolescents aged 6-18 years** and is characterized by persistent irritability and frequent, severe temper outbursts disproportionate to the situation.
- It is **not applicable to adults** and does not describe this patient's presentation of persistent depressed mood and neurovegetative symptoms.
Depression with atypical features US Medical PG Question 4: A 24-year-old woman comes to the physician because she feels sad and has had frequent, brief episodes of crying for the last month. During this period, she sleeps in every morning and spends most of her time in bed playing video games or reading. She has not been spending time with friends but still attends a weekly book club and continues to plan her annual family reunion. She stopped going to the gym, eats more, and has gained 4 kg (8.8 lb) over the past 4 weeks. Three weeks ago, she also started to smoke marijuana a few times a week. She drinks one glass of wine daily and does not smoke cigarettes. She is currently unemployed; she lost her job as a physical therapist 3 months ago. Her vital signs are within normal limits. On mental status examination, she is calm, alert, and oriented to person, place, and time. Her mood is depressed; her speech is organized, logical, and coherent. She denies suicidal thoughts. Which of the following is the most likely diagnosis?
- A. Bipolar disorder
- B. Substance use disorder
- C. Major depressive disorder
- D. Adjustment disorder (Correct Answer)
- E. Persistent Depressive Disorder (Dysthymia)
Depression with atypical features Explanation: ***Adjustment disorder***
- This diagnosis is characterized by the development of emotional or behavioral symptoms in response to an identifiable stressor (such as losing a job) occurring within **3 months** of the onset of the stressor.
- The patient exhibits depressive symptoms (sadness, crying, increased sleep, anhedonia, weight gain) that do not meet the full criteria for a major depressive episode and do not significantly impair social/occupational functioning, as evidenced by her continued participation in a book club and planning her family reunion.
*Bipolar disorder*
- This disorder typically involves episodes of **mania or hypomania** along with depressive episodes, neither of which are described in the patient's presentation.
- Her symptoms are consistently depressive in nature and linked to a specific stressor, without periods of elevated mood, increased energy, or decreased need for sleep.
*Substance use disorder*
- While the patient has recently started smoking marijuana and drinks alcohol, these behaviors developed *after* the onset of her depressive symptoms and a known stressor.
- Her marijuana use is still relatively recent ("a few times a week") and not yet described as causing significant impairment or dependence that would typically define a substance use disorder as the primary diagnosis.
*Major depressive disorder*
- This diagnosis requires a severe and pervasive depressive episode that lasts for at least **2 weeks** and significantly impairs functioning in multiple areas of life.
- Although she has several depressive symptoms, her continued ability to engage in some social activities (book club) and plan events (family reunion) suggests that the impairment is not as severe or pervasive as typically seen in MDD. Additionally, her symptoms are clearly linked to a recent life stressor, which points away from MDD as the primary diagnosis.
*Persistent Depressive Disorder (Dysthymia)*
- This disorder is characterized by a chronically depressed mood that lasts for at least **2 years** (or 1 year in children/adolescents), with symptoms that are generally milder than major depression but more persistent.
- The patient's symptoms have only been present for one month, which is far too short a duration to meet the diagnostic criteria for persistent depressive disorder.
Depression with atypical features US Medical PG Question 5: A 42-year-old female presents to her primary care provider for an annual checkup. She reports feeling sad over the past few months for no apparent reason. She has lost interest in swimming, which she previously found enjoyable. Additionally, she has had trouble getting a full night’s sleep and has had trouble concentrating during the day. She has lost 15 pounds since her last visit one year prior. Which of the following sets of neurotransmitter levels is associated with this patient’s condition?
- A. Decreased acetylcholine, normal serotonin, normal dopamine
- B. Decreased norepinephrine, decreased serotonin, decreased dopamine (Correct Answer)
- C. Decreased GABA, decreased acetylcholine, increased dopamine
- D. Increased norepinephrine, decreased serotonin, decreased GABA
- E. Increased acetylcholine, increased serotonin, decreased dopamine
Depression with atypical features Explanation: ***Decreased norepinephrine, decreased serotonin, decreased dopamine***
- The patient's symptoms of **sadness**, loss of interest (**anhedonia**), **insomnia**, **difficulty concentrating**, and **weight loss** are classic for **major depressive disorder**.
- **Depression** is strongly associated with deficiencies in **monoamine neurotransmitters**: **norepinephrine**, **serotonin**, and **dopamine**.
*Decreased acetylcholine, normal serotonin, normal dopamine*
- While **acetylcholine** is involved in mood regulation, its isolated decrease with normal serotonin and dopamine levels is not characteristic of generalized depression.
- More prominent roles for **acetylcholine dysfunction** are seen in conditions like **Alzheimer's disease** or **myasthenia gravis**.
*Decreased GABA, decreased acetylcholine, increased dopamine*
- **Decreased GABA** is often associated with **anxiety disorders** and seizures, not the primary presentation of depression here.
- **Increased dopamine** is more characteristic of conditions like **schizophrenia** or **mania**, which contrasts with the patient's depressive symptoms.
*Increased norepinephrine, decreased serotonin, decreased GABA*
- **Increased norepinephrine** is typically associated with **anxiety**, **stress**, or sometimes **mania**, which is inconsistent with this patient's depressive state.
- While **decreased serotonin** is correct for depression, the combination with increased norepinephrine and decreased GABA does not fit the typical neurotransmitter profile.
*Increased acetylcholine, increased serotonin, decreased dopamine*
- **Increased acetylcholine** is generally not associated with the full spectrum of depressive symptoms described.
- **Increased serotonin** is often the goal of antidepressant treatments (SSRIs), making an endogenous increase unlikely to cause depression.
Depression with atypical features US Medical PG Question 6: A 23-year-old woman is brought to the physician by her father because of irritability, mood swings, and difficulty sleeping over the past 10 days. A few days ago, she quit her job and spent all of her savings on supplies for a “genius business plan.” She has been energetic despite sleeping only 1–2 hours each night. She was diagnosed with major depressive disorder 2 years ago. Mental status examination shows pressured speech, a labile affect, and flight of ideas. Throughout the examination, she repeatedly states “I feel great, I don't need to be here.” Urine toxicology screening is negative. Which of the following is the most likely diagnosis?
- A. Schizoaffective disorder
- B. Bipolar disorder type II
- C. Bipolar disorder type I (Correct Answer)
- D. Delusional disorder
- E. Attention-deficit hyperactivity disorder
Depression with atypical features Explanation: ***Bipolar disorder type I***
- The patient's presentation of lasting **elevated mood**, decreased need for sleep, increased energy, pressured speech, flight of ideas, and impulsive behavior (quitting job, spending savings) are hallmark symptoms of a **manic episode**.
- A diagnosis of **Bipolar I Disorder** requires the occurrence of at least one manic episode, which is clearly evident here and distinguishes it from other mood disorders, especially given her prior history of major depressive disorder.
*Schizoaffective disorder*
- This disorder involves a period of illness during which there is an uninterrupted period of major mood episode (depressive or manic) concurrent with symptoms of **schizophrenia**, such as delusions or hallucinations, for at least 2 weeks in the absence of a major mood episode.
- The patient's symptoms are primarily mood-driven and do not include the characteristic psychotic features that persist independently of mood disturbances.
*Bipolar disorder type II*
- Bipolar II Disorder is characterized by at least one major depressive episode and at least one **hypomanic episode**.
- The patient's current symptoms, including significant impairment in social/occupational functioning, are indicative of a **manic episode**, not a hypomanic episode, which by definition does not cause marked impairment or require hospitalization.
*Delusional disorder*
- This disorder is characterized by the presence of **non-bizarre delusions** that last for at least one month, without other prominent psychotic symptoms or significant impairment in functioning.
- While the patient's "genius business plan" might seem delusional, her pervasive mood disturbance, flight of ideas, and significant functional impairment are not consistent with the primary features of delusional disorder.
*Attention-deficit hyperactivity disorder*
- ADHD is characterized by a persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development, often presenting in childhood.
- While there is some overlap in symptoms like impulsivity and difficulty sleeping, the episodic nature, the extent of **mood disturbance**, grandiosity, and **pressured speech** are more characteristic of a manic episode than ADHD.
Depression with atypical features US Medical PG Question 7: A 24-year-old woman presents to her primary care physician for a wellness exam. She currently has no acute concerns but has been feeling hopeless, has a poor appetite, difficulty with concentration, and trouble with sleep. She says that she has poor self-esteem and that her symptoms have been occurring for the past 3 years. She has had moments where she felt better, but it lasted a few weeks out of the year. She currently lives alone and does not pursue romantic relationships because she feels she is not attractive. She has a past medical history of asthma. Her mother is alive and healthy. Her father committed suicide and suffered from major depressive disorder. On physical exam, the patient has a gloomy demeanor and appears restless and anxious. Which of the following is the most likely diagnosis?
- A. Major depressive disorder
- B. Cyclothymia
- C. Persistent depressive disorder (Correct Answer)
- D. Seasonal affective disorder
- E. Disruptive mood dysregulation disorder
Depression with atypical features Explanation: ***Persistent depressive disorder***
- The patient exhibits chronic symptoms of depression (poor appetite, poor self-esteem, difficulty with concentration, trouble with sleep, hopelessness) lasting for at least **2 years**, with symptom-free periods lasting no more than **2 months**.
- Her long-standing symptoms (3 years) and the intermittent improvement, but never full resolution for extended periods, are characteristic of **persistent depressive disorder** (formerly dysthymia).
*Major depressive disorder*
- While the patient has many symptoms of depression, **major depressive disorder** is characterized by distinct episodes of at least 2 weeks, with significant functional impairment. The chronic, fluctuating course over 3 years is less typical.
- The presence of depressive symptoms for 3 years, with only brief periods of improvement, points away from episodic major depressive disorder alone and more towards a chronic form.
*Cyclothymia*
- **Cyclothymia** involves numerous periods of hypomanic symptoms and numerous periods of depressive symptoms for at least 2 years, with periods of stability lasting no more than 2 months. The patient describes only depressive symptoms, not hypomanic episodes.
- There is no mention of elevated mood, increased energy, or decreased need for sleep, which are characteristic of **hypomanic episodes** in cyclothymia.
*Seasonal affective disorder*
- **Seasonal affective disorder** is a type of depressive disorder that occurs during a specific season (most commonly winter) and resolves during other seasons; the patient's symptoms are year-round and chronic.
- The patient's symptoms are not described as tied to a particular season, making this diagnosis less likely.
*Disruptive mood dysregulation disorder*
- Predominantly diagnosed in **children and adolescents**, this disorder is characterized by severe recurrent temper outbursts and persistently irritable or angry mood between outbursts.
- The patient's age (24 years old) and the absence of temper outbursts make this diagnosis inappropriate.
Depression with atypical features US Medical PG Question 8: A 35-year-old banker is brought to a medical clinic by his concerned wife. For the past 3 weeks, he has not been eating well and has had a 10 kg (22 lb) weight loss. He wakes up very early in the mornings and feels extremely despondent. He no longer goes out on the weekends to hang out with his close friends nor does he go on date nights with his wife. He feels guilty for letting his friends and family down recently. He additionally has a history of fibromyalgia and deals with daily pain. What would be the most appropriate treatment plan for this patient?
- A. Amitriptyline
- B. Phenelzine
- C. Venlafaxine (Correct Answer)
- D. Electroconvulsive therapy
- E. Fluoxetine
Depression with atypical features Explanation: ***Venlafaxine***
- This patient presents with symptoms highly suggestive of **major depressive disorder**, including **anhedonia**, significant **weight loss**, **early morning awakening**, and **feelings of guilt**. His co-occurring **fibromyalgia** makes a **serotonin-norepinephrine reuptake inhibitor (SNRI)** like venlafaxine an excellent choice.
- SNRIs are effective for both depression and chronic pain conditions such as fibromyalgia, as they modulate both **serotonin** and **norepinephrine** pathways, which are implicated in both mood and pain perception.
*Amitriptyline*
- **Amitriptyline** is a **tricyclic antidepressant (TCA)** that can be used for both depression and chronic pain, including fibromyalgia.
- However, TCAs generally have a less favorable side effect profile (e.g., **anticholinergic effects**, **cardiac toxicity in overdose**) compared to SNRIs and SSRIs, making them less of a first-line choice unless other options fail or specific indications are present.
*Phenelzine*
- **Phenelzine** is a **monoamine oxidase inhibitor (MAOI)**, typically reserved for **atypical depression** or treatment-resistant depression due to its significant **food and drug interactions** (e.g., **hypertensive crisis** with tyramine-rich foods or sympathomimetics).
- Given this is likely a first-line treatment scenario, an MAOI would not be the most appropriate initial choice.
*Electroconvulsive therapy*
- **Electroconvulsive therapy (ECT)** is a highly effective treatment for severe depression, especially with **psychotic features**, **catatonia**, or **severe suicidality**, or in cases of **treatment resistance** where other modalities have failed.
- While the patient has significant symptoms of depression, there is no indication of immediate life-threatening severity (e.g., active suicidal intent with a plan) or treatment resistance to warrant ECT as a first-line option.
*Fluoxetine*
- **Fluoxetine** is a **selective serotonin reuptake inhibitor (SSRI)** and a common first-line treatment for major depressive disorder.
- While it would be effective for the patient's depression, it does not offer the additional specific benefit for **fibromyalgia pain** that an SNRI like venlafaxine provides through dual serotonin and norepinephrine reuptake inhibition.
Depression with atypical features US Medical PG Question 9: A 25-year-old woman is brought to the emergency department by EMS after being found naked in a busy downtown square. The patient stated that she is liberating people from material desires and was found destroying objects. Her temperature is 99.5°F (37.5°C), blood pressure is 127/68 mmHg, pulse is 120/min, respirations are 22/min, and oxygen saturation is 98% on room air. Physical exam is deferred due to patient combativeness. The patient is given diphenhydramine and haloperidol and transferred to the psychiatric ward. On day 1 on the ward, the patient is no longer aggressive or agitated and has calmed down. She states that she feels severely depressed and wants to kill herself. The patient is started on a medication and monitored closely. On day 3 of the patient's stay in the hospital she is found in her room drawing up plans and states that she has major plans to revamp the current energy problems in the country. Which of the following is the most likely medication that was started in this patient?
- A. Quetiapine
- B. Olanzapine
- C. Lamotrigine
- D. Sertraline (Correct Answer)
- E. Lithium
Depression with atypical features Explanation: ***Sertraline***
- This patient exhibits classic **bipolar I disorder** with rapid mood cycling from **mania** (naked in public, grandiose delusions, destroying objects) to **severe depression** (suicidal ideation on Day 1) and back to **mania** (grandiose plans on Day 3).
- The key clinical clue is the **rapid return to mania by Day 3** after starting medication during the depressive phase. This suggests **antidepressant-induced mania/mood switch**, a well-known complication of using **SSRI antidepressants** (like sertraline) **without adequate mood stabilization** in bipolar disorder.
- **Antidepressants can precipitate manic episodes** within days in bipolar patients, which is why they should be avoided or used only with concomitant mood stabilizers. This question tests recognition of this critical psychiatric principle.
*Lithium*
- Lithium is a first-line **mood stabilizer** for bipolar disorder and would be appropriate for long-term management. However, lithium **prevents manic episodes** rather than causing them.
- Lithium takes **1-2 weeks to reach therapeutic levels**, so it would not explain the rapid mood switch to mania by Day 3. If lithium had been started, we would expect **stabilization or improvement**, not a return to mania.
*Quetiapine*
- Quetiapine is an **atypical antipsychotic** effective for both acute mania and bipolar depression. It can provide rapid mood stabilization.
- If quetiapine was started on Day 1, we would expect **mood stabilization or sedation**, not a switch back to mania. Quetiapine does **not precipitate manic episodes**.
*Olanzapine*
- Olanzapine is another **atypical antipsychotic** used for acute mania and maintenance in bipolar disorder.
- Like quetiapine, olanzapine would **stabilize mood** and reduce manic symptoms, not trigger them. It would not explain the return to mania on Day 3.
*Lamotrigine*
- Lamotrigine is a mood stabilizer particularly effective for **preventing depressive episodes** in bipolar disorder, though less effective for acute mania.
- Lamotrigine **does not precipitate manic episodes** and takes weeks to titrate to therapeutic doses due to risk of Stevens-Johnson syndrome. It would not explain the rapid mood switch observed here.
Depression with atypical features US Medical PG Question 10: A 27-year-old woman visits a psychiatrist expressing her feelings of sadness which are present on most days of the week. She says that she has been feeling this way for about 2 to 3 years. During her first pregnancy 3 years ago, the fetus died in utero, and the pregnancy was terminated at 21 weeks. Ever since then, she hasn’t been able to sleep well at night and has difficulty concentrating on her tasks most of the time. However, for the past month, she has found it more difficult to cope. She says she has no will to have another child as she still feels guilty and responsible for the previous pregnancy. Over the past few days, she has completely lost her appetite and only eats once or twice a day. She doesn’t recall a single day in the last 3 years where she has not felt this way. The patient denies any past or current smoking, alcohol, or recreational drug use. Which of the following is the most likely diagnosis in this patient?
- A. Persistent depressive disorder (Correct Answer)
- B. Bipolar disorder
- C. Schizoaffective disorder
- D. Cyclothymia
- E. Major depressive disorder
Depression with atypical features Explanation: ***Persistent depressive disorder***
- The patient exhibits classic symptoms of **persistent depressive disorder (dysthymia)**: chronic depressed mood for **at least two years**, accompanied by other depressive symptoms like **insomnia**, **difficulty concentrating**, and changes in appetite.
- The duration of her symptoms (2-3 years) and the consistent feeling of sadness support this diagnosis, fitting the diagnostic criteria for **dysthymia**.
*Bipolar disorder*
- Bipolar disorder involves distinct episodes of **mania or hypomania** alternating with depressive episodes.
- The patient's history does not indicate any periods of elevated mood, increased energy, or decreased need for sleep, which are characteristic of **bipolar disorder**.
*Schizoaffective disorder*
- Schizoaffective disorder is characterized by a combination of **mood symptoms** (like depression or mania) and **psychotic symptoms** (like delusions or hallucinations) occurring simultaneously or in distinct episodes.
- This patient presents with no evidence of **psychotic symptoms** such as hallucinations or delusions.
*Cyclothymia*
- Cyclothymia is a milder, chronic form of **bipolar disorder** involving numerous periods of **hypomanic symptoms** and numerous periods of **depressive symptoms** for at least two years.
- The patient's presentation lacks any history of **hypomanic episodes**, making cyclothymia an unlikely diagnosis.
*Major depressive disorder*
- While the patient is experiencing a **major depressive episode** currently (as suggested by increased severity in the last month and complete loss of appetite), the underlying chronic nature of her symptoms (2-3 years) and the fact that she has not been symptom-free for more than two months indicate **persistent depressive disorder**.
- A diagnosis of **major depressive disorder** would typically be given if the symptoms were acute (less than 2 years) and severe, without the chronic, pervasive depressive state described.
More Depression with atypical features US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.