Neurobiological basis of delusions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neurobiological basis of delusions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neurobiological basis of delusions US Medical PG Question 1: Two dizygotic twins present to the university clinic because they believe they are being poisoned through the school's cafeteria food. They have brought these concerns up in the past, but no other students or cafeteria staff support this belief. Both of them are average students with strong and weak subject areas as demonstrated by their course grade-books. They have no known medical conditions and are not known to abuse illicit substances. Which statement best describes the condition these patients have?
- A. A trial separation is likely to worsen symptoms.
- B. The disorder is its own disease entity in DSM-5.
- C. Antipsychotic medications are rarely beneficial.
- D. Can affect two or more closely related individuals. (Correct Answer)
- E. Cognitive behavioral therapy is a good first-line.
Neurobiological basis of delusions Explanation: ***Can affect two or more closely related individuals.***
- The shared delusional belief in **folie à deux**, also known as **shared psychotic disorder**, typically occurs in two or more people who are closely associated.
- In this case, the **dizygotic twins** sharing the same delusional belief about being poisoned from cafeteria food fits this pattern.
*A trial separation is likely to worsen symptoms.*
- **Separating the individuals** involved in **folie à deux** is often a crucial step in treatment, as it can help break the cycle of shared delusion and allow for individual therapy.
- Separation typically IMPROVES rather than worsens symptoms by removing the reinforcement of the shared delusion.
*The disorder is its own disease entity in DSM-5.*
- In the **DSM-5**, **folie à deux** is no longer considered a separate diagnostic category.
- Instead, it is classified under **Other Specified Schizophrenia Spectrum and Other Psychotic Disorder** or **Unspecified Schizophrenia Spectrum and Other Psychotic Disorder**, with the specific context of shared delusion noted.
*Antipsychotic medications are rarely beneficial.*
- **Antipsychotics** are actually commonly used in treating folie à deux, particularly for the **primary individual** who initially developed the delusion.
- They can be an important component of treatment, often combined with separation and psychotherapy.
*Cognitive behavioral therapy is a good first-line.*
- **Cognitive Behavioral Therapy (CBT)** can be beneficial, particularly after separation, to help individuals challenge and reframe their delusional beliefs.
- However, the **first-line intervention** for shared psychotic disorder is **separation of the involved individuals**, followed by individual therapy (which may include CBT) and medication as needed.
Neurobiological basis of delusions US Medical PG Question 2: A 23-year-old woman is brought to the emergency department by her friend because of strange behavior. Two hours ago, she was at a night club where she got involved in a fight with the bartender. Her friend says that she was smoking a cigarette before she became irritable and combative. She repeatedly asked “Why are you pouring blood in my drink?” before hitting the bartender. She has no history of psychiatric illness. Her temperature is 38°C (100.4°F), pulse is 100/min, respirations are 19/min, and blood pressure is 158/95 mm Hg. Examination shows muscle rigidity. She has a reduced degree of facial expression. She has no recollection of her confrontation with the bartender. Which of the following is the most likely primary mechanism responsible for this patient's symptoms?
- A. Stimulation of cannabinoid receptors
- B. Inhibition of NMDA receptors (Correct Answer)
- C. Inhibition of norepinephrine, serotonin, and dopamine reuptake
- D. Stimulation of 5HT2A and dopamine D2 receptors
- E. Inhibition of dopamine D2 receptors
Neurobiological basis of delusions Explanation: ***Inhibition of NMDA receptors***
- The patient's symptoms, including **combativeness**, **erratic behavior**, **delusions** ("Why are you pouring blood in my drink?"), **hypertension**, **tachycardia**, and **muscle rigidity**, are characteristic of **PCP intoxication**.
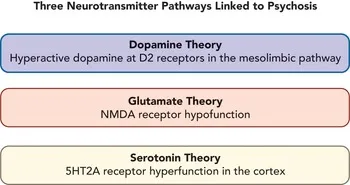
- **Phencyclidine (PCP)** acts primarily as an **NMDA receptor antagonist**, blocking calcium channels and leading to these neurotoxic effects.
*Stimulation of cannabinoid receptors*
- **Cannabis intoxication** typically involves **euphoria**, distorted perception, impaired memory, and increased appetite, which are not the primary features described here.
- While agitation can occur, the severe combativeness, delusions, and specific vital sign changes point away from cannabinoid receptor stimulation as the primary mechanism for this presentation.
*Inhibition of norepinephrine, serotonin, and dopamine reuptake*
- This mechanism is characteristic of stimulants like **cocaine** or **amphetamines**. While these drugs can cause agitation, paranoia, hypertension, and tachycardia, they typically do not cause the prominent **muscle rigidity** and **delusional thought** content as described.
- The "smoking a cigarette" context might suggest stimulants, but the overall clinical picture is more consistent with PCP.
*Stimulation of 5HT2A and dopamine D2 receptors*
- Stimulation of **5HT2A receptors** is associated with **hallucinogens** like LSD, causing perceptual distortions and altered consciousness, but typically not the intense combativeness, muscle rigidity, and specific delusions seen here.
- While **dopamine D2 receptor stimulation** can contribute to psychosis, it's not the primary mechanism that brings together all the described symptoms in this acute, severe presentation.
*Inhibition of dopamine D2 receptors*
- **Dopamine D2 receptor inhibition** is the mechanism of action for antipsychotic medications and generally leads to a reduction in psychotic symptoms, not the intense agitation, combativeness, and psychotic features observed in this patient.
- Such inhibition can lead to extrapyramidal symptoms, but not the acute, substance-induced presentation described.
Neurobiological basis of delusions US Medical PG Question 3: A 31-year-old woman is brought to the physician because of increasing restlessness over the past 2 weeks. She reports that she continuously paces around the house and is unable to sit still for more than 10 minutes at a time. During this period, she has had multiple episodes of anxiety with chest tightness and shortness of breath. She was diagnosed with a psychotic illness 2 months ago. Her current medications include haloperidol and a multivitamin. She appears agitated. Vital signs are within normal limits. Physical examination shows no abnormalities. The examination was interrupted multiple times when she became restless and began to walk around the room. To reduce the likelihood of the patient developing her current symptoms, a drug with which of the following mechanisms of action should have been prescribed instead of her current medication?
- A. H2 receptor antagonism
- B. 5-HT2A receptor antagonism (Correct Answer)
- C. α2 receptor antagonism
- D. NMDA receptor antagonism
- E. GABA receptor antagonism
Neurobiological basis of delusions Explanation: ***5-HT2A receptor antagonism***
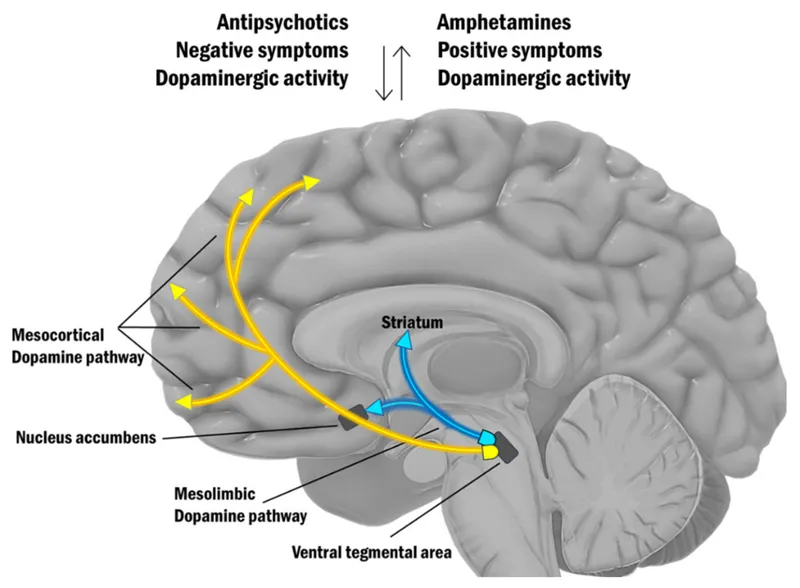
- The patient is experiencing **akathisia**, a common extrapyramidal side effect of **typical antipsychotics** like haloperidol, characterized by subjective or objective motor restlessness.
- Atypical antipsychotics, which exert their antipsychotic effects primarily through **5-HT2A receptor antagonism** along with D2 receptor antagonism, have a lower propensity to cause extrapyramidal symptoms, including akathisia, compared to typical antipsychotics.
*H2 receptor antagonism*
- **H2 receptor antagonists** are primarily used to reduce gastric acid secretion in conditions like peptic ulcer disease and GERD.
- They have no direct role in treating psychosis or preventing extrapyramidal side effects.
*α2 receptor antagonism*
- **Alpha-2 receptor antagonists** (e.g., mirtazapine) are typically used as antidepressants; their mechanism involves increasing norepinephrine and serotonin release.
- This mechanism is not directly therapeutic for psychosis and would not prevent akathisia caused by D2 receptor blockade.
*NMDA receptor antagonism*
- **NMDA receptor antagonists** (e.g., ketamine, memantine) are studied for various neurological and psychiatric conditions, but their primary use is not in typical psychosis treatment, nor do they prevent akathisia from antipsychotics.
- Instead, NMDA receptor hypofunction is hypothesized in schizophrenia, and antagonism could potentially worsen psychotic symptoms.
*GABA receptor antagonism*
- **GABA receptor antagonists** (e.g., flumazenil) block the effects of inhibitory neurotransmitter GABA and can cause seizures and increased anxiety, which would be detrimental in a patient with psychosis and anxiety.
- Medications that *enhance* GABAergic transmission (e.g., benzodiazepines) are sometimes used to treat acute akathisia or anxiety, but long-term antagonism would be contra-indicated.
Neurobiological basis of delusions US Medical PG Question 4: A 22-year-old man is brought to the emergency department by his father because he is having bizarre thoughts. The patient says that he is being haunted by aliens from outer space. The father is worried as his son has had these symptoms for the past 7 months and lately, it seems to be getting worse. He has become more self-obsessed and does not seem to have any interest in his favorite activities. He has no plans to harm himself or others but spends a lot of time and energy building ‘defenses’ in and around his room as he is absolutely sure that aliens will come to get him soon. His blood pressure is 121/79 mm Hg, pulse 86/min, respiratory rate 15/min, temperature 36.8°C (98.2°F). Which of the following is correct regarding the patient’s symptoms?
- A. It would benefit from psychosurgery.
- B. He has a fixed false belief. (Correct Answer)
- C. It is best treated with cognitive behavioral therapy alone.
- D. It is a negative symptom.
- E. It falls under the disorganized thinking domain.
Neurobiological basis of delusions Explanation: ***He has a fixed false belief.***
- The patient's conviction that he is being haunted by aliens, despite evidence to the contrary and the distress it causes, constitutes a **delusion**.
- A delusion is by definition a **fixed, false belief** that is not in keeping with the individual's cultural background.
*It would benefit from psychosurgery.*
- Psychosurgery, such as lobotomy, is an extreme and rarely used intervention for **severe, refractory mental disorders**, typically only after all other treatments have failed and with significant ethical considerations.
- While the patient's symptoms are impairing, **first-line treatments** for psychotic disorders involve antipsychotic medications and psychotherapy, not psychosurgery.
*It is best treated with cognitive behavioral therapy alone.*
- While CBT for psychosis (CBTp) can be a useful **adjunct** in managing delusions and reducing distress, it is **not sufficient as monotherapy** for active, severe psychotic symptoms.
- The primary intervention for profound delusions like those described is **antipsychotic medication**, with CBT added as an adjunctive treatment to help improve functioning and coping.
- CBT alone would be inadequate for someone with such fixed, impairing delusions actively building defenses against perceived threats.
*It is a negative symptom.*
- Negative symptoms of psychosis include features like **anhedonia** (lack of pleasure), **alogia** (poverty of speech), **avolition** (lack of motivation), and affective flattening.
- The patient's bizarre belief in aliens is a **positive symptom** as it represents an *addition* to normal experience, rather than a *reduction* or *absence* of normal functions.
- Note: The patient's decreased interest in activities suggests negative symptoms are also present, but the question asks about "the patient's symptoms" in context of the delusion described.
*It falls under the disorganized thinking domain.*
- Disorganized thinking or speech involves patterns like **loose associations, tangentiality, incoherence**, or word salad, where the logical connections between thoughts are lost.
- While the content of the patient's thoughts is bizarre, the core issue described is the *belief itself* (a delusion, which is a **positive symptom**), rather than disordered *thought processes* or the way he expresses them.
Neurobiological basis of delusions US Medical PG Question 5: A 21-year-old man presents to the emergency room requesting surgery to remove "microchips," which he believes were implanted in his brain by "Russian spies" 6 months ago to control his thoughts. He also reports hearing the "spies" talk to each other through embedded "microspeakers." You notice that his hair appears unwashed and some of his clothes are on backward. Urine toxicology is negative for illicit drugs. Which of the following additional findings are you most likely to see in this patient during the course of his illness?
- A. Anhedonia, guilty rumination, and insomnia
- B. Grandiose delusions, racing thoughts, and pressured speech
- C. Asociality, flat affect, and alogia (Correct Answer)
- D. Amnesia, multiple personality states, and de-realization
- E. Intrusive thoughts, ritualized behaviors, and anxious mood
Neurobiological basis of delusions Explanation: ***Asociality, flat affect, and alogia***
- This patient exhibits **delusions (persecutory, control)** and **auditory hallucinations**, classic positive symptoms of **schizophrenia**. The question asks about findings "during the course of his illness," which points to the **typical progression of schizophrenia**: patients initially present with **positive symptoms** (as seen in this case) and **over time develop negative symptoms** such as **asociality** (lack of motivation to engage in social interaction), **flat affect** (reduced emotional expression), and **alogia** (poverty of speech).
- The disorganized appearance (unwashed hair, clothes on backward) already demonstrates **disorganized behavior**, part of the schizophrenia spectrum. Negative symptoms typically emerge or worsen as the illness progresses, representing the most likely additional findings.
*Anhedonia, guilty rumination, and insomnia*
- While **anhedonia** and **insomnia** can be seen in schizophrenia, their presence alongside prominent **guilty rumination** would more strongly suggest a **depressive disorder with psychotic features**, rather than primary schizophrenia, especially with the patient's specific, classic psychotic symptoms.
- The primary symptoms described (delusions of control, auditory hallucinations) are more characteristic of primary psychotic disorders, and guilty rumination is not a typical feature of schizophrenia progression.
*Grandiose delusions, racing thoughts, and pressured speech*
- These symptoms are hallmark features of **mania** or a **manic episode with psychotic features**. While psychotic features can occur in bipolar disorder with mania, the patient's specific delusions of being controlled by spies and hearing voices discussing him are more typical of schizophrenia.
- The absence of information about elevated mood, increased energy, or decreased need for sleep also makes mania less likely compared to schizophrenia.
*Amnesia, multiple personality states, and de-realization*
- These symptoms are characteristic of **dissociative disorders**. **Amnesia** and **multiple personality states** (now known as identity alteration in dissociative identity disorder) involve disturbances in memory and identity.
- **De-realization** involves feelings of unreality regarding one's surroundings. None of these align with the patient's primary presentation of well-formed delusions and hallucinations characteristic of a psychotic disorder.
*Intrusive thoughts, ritualized behaviors, and anxious mood*
- These are core features of **obsessive-compulsive disorder (OCD)**. The patient's symptoms are clearly defined as delusions (fixed false beliefs) and hallucinations (perceptions without external stimuli), which are distinct from the ego-dystonic intrusive thoughts and ritualistic compulsions of OCD.
- While anxiety may be present in psychotic disorders, the primary presentation here is not dominated by OCD-like symptoms, and these would not be expected to develop as part of schizophrenia's natural course.
Neurobiological basis of delusions US Medical PG Question 6: Two studies are reviewed for submission to an oncology journal. In Study A, a novel MRI technology is evaluated as a screening tool for ovarian cancer. The authors find that the mean survival time is 4 years in the control group and 10 years in the MRI-screened group. In Study B, cognitive behavioral therapy (CBT) and a novel antidepressant are used to treat patients with comorbid pancreatic cancer and major depression. Patients receiving the new drug are told that they are expected to have quick resolution of their depression, while those who do not receive the drug are not told anything about their prognosis. Which of the following describes the likely type of bias in Study A and Study B?
- A. Latency Bias; Golem effect
- B. Confounding; Golem effect
- C. Lead time bias; Golem effect
- D. Lead time bias; Pygmalion effect (Correct Answer)
- E. Latency bias; Pygmalion effect
Neurobiological basis of delusions Explanation: ***Lead time bias; Pygmalion effect***
- In Study A, the MRI technology detects ovarian cancer earlier, artificially making the survival time appear longer simply due to earlier diagnosis, not necessarily improved outcomes, which is characteristic of **lead time bias**.
- In Study B, the patients receiving the new drug are told to expect quick resolution of their depression, leading to increased expectation of improvement, which describes the **Pygmalion effect** (a form of observer-expectancy effect where higher expectations lead to increased performance).
*Latency Bias; Golem effect*
- **Latency bias** refers to a delay in the manifestation of an outcome, which is not the primary issue in Study A's screening context.
- The **Golem effect** is a form of negative self-fulfilling prophecy where lower expectations placed upon individuals by superiors/researchers lead to poorer performance, which is opposite to what is described in Study B.
*Confounding; Golem effect*
- **Confounding** occurs when an unmeasured third variable is associated with both the exposure and the outcome, distorting the observed relationship; while confounding is common, the scenario in Study A specifically points to a screening effect on survival time.
- As mentioned, the **Golem effect** refers to negative expectations leading to poorer outcomes, which is not present in Study B.
*Lead time bias; Golem effect*
- **Lead time bias** correctly identifies the issue in Study A, as explaining the apparently longer survival as a result of earlier detection.
- However, the **Golem effect** incorrectly describes the scenario in Study B, where positive expectations are given, not negative ones.
*Latency bias; Pygmalion effect*
- **Latency bias** is not the primary bias described in Study A; the immediate impact of early detection on survival statistics points to lead time bias.
- The **Pygmalion effect** correctly describes the bias in Study B, where positive expectations from the researchers influence patient outcomes.
Neurobiological basis of delusions US Medical PG Question 7: A 15-year-old girl is brought to the physician by her mother for an annual well-child examination. Her mother complains that the patient has a poor diet and spends most of the evening at home texting her friends instead of doing homework. She has been caught smoking cigarettes in the school bathroom several times and appears indifferent to the dean's threats of suspension. Two weeks ago, the patient allowed a friend to pierce her ears with unsterilized safety pins. The mother appeals to the physician to lecture the patient about her behavior and “set her straight.” The patient appears aloof and does not make eye contact. Her grooming is poor. Upon questioning the daughter about her mood, the mother responds “She acts like a rebel. I can't wait until puberty is over.” Which of the following is the most appropriate response?
- A. You should listen to your mother's concerns. You don't want to make poor choices early on or else you might end up on the streets.
- B. Would it be possible for you to step out for a few moments so that I can interview your daughter alone? (Correct Answer)
- C. Let's run a routine urine toxicology screen to make sure your daughter is not doing drugs.
- D. I am very concerned that your daughter is displaying signs of depression, and I'd suggest that she is seen by a psychiatrist.
- E. Your daughter displays normal signs of puberty. Being overly critical of your daughter is not helpful.
Neurobiological basis of delusions Explanation: ***"Would it be possible for you to step out for a few moments so that I can interview your daughter alone?"***
- This approach respects the adolescent's **autonomy** and provides a safe space for her to disclose sensitive information without parental presence.
- Adolescents are more likely to be **candid** about risky behaviors like smoking, substance use, or sexual activity if they feel their privacy is protected.
*"You should listen to your mother's concerns. You don't want to make poor choices early on or else you might end up on the streets."*
- This response is **confrontational** and judgmental, which is likely to alienate the patient and shut down communication.
- It also uses **fear tactics** rather than fostering trust and a therapeutic relationship.
*"Let's run a routine urine toxicology screen to make sure your daughter is not doing drugs."*
- While drug use is a concern given her risky behaviors, immediately suggesting a **toxicology screen** without building rapport can feel accusatory and escalate distrust.
- It's often more effective to establish communication first before moving to definitive testing, especially in a well-child visit where drug use has not been directly admitted.
*"I am very concerned that your daughter is displaying signs of depression, and I'd suggest that she is seen by a psychiatrist."*
- While some of the patient's behaviors (poor grooming, aloofness, indifference) could be consistent with **depression**, immediately jumping to a diagnosis and referral without a direct interview is premature.
- It can also be perceived as labeling and might be rejected by the patient and mother without further exploration.
*"Your daughter displays normal signs of puberty. Being overly critical of your daughter is not helpful."*
- This response dismisses the mother's valid concerns about genuinely **risky behaviors** (smoking, unsterilized piercing, indifference to consequences) as "normal puberty."
- It also implicitly criticizes the mother, which can damage the therapeutic alliance with both the parent and the patient.
Neurobiological basis of delusions US Medical PG Question 8: A 20-year-old male is brought to a psychiatrist by his parents for bizarre behavior. His parents report that over the past two semesters in school, his personality and behavior have changed noticeably. He refuses to leave his room because he believes people are spying on him. He hears voices that are persecutory and is convinced that people at school have chips implanted in their brains to spy on him. Screenings for depression and mania are negative. His past medical history is unremarkable. His family history is notable for a maternal uncle with bipolar disorder. He does not drink alcohol or smoke. His temperature is 98.8°F (37.1°C), blood pressure is 115/70 mmHg, pulse is 85/min, and respirations are 18/min. On examination, he appears to be responding to internal stimuli. Which of the following pathways is primarily responsible for these symptoms?
- A. Papez circuit
- B. Mesocortical pathway
- C. Nigrostriatal pathway
- D. Tuberoinfundibular pathway
- E. Mesolimbic pathway (Correct Answer)
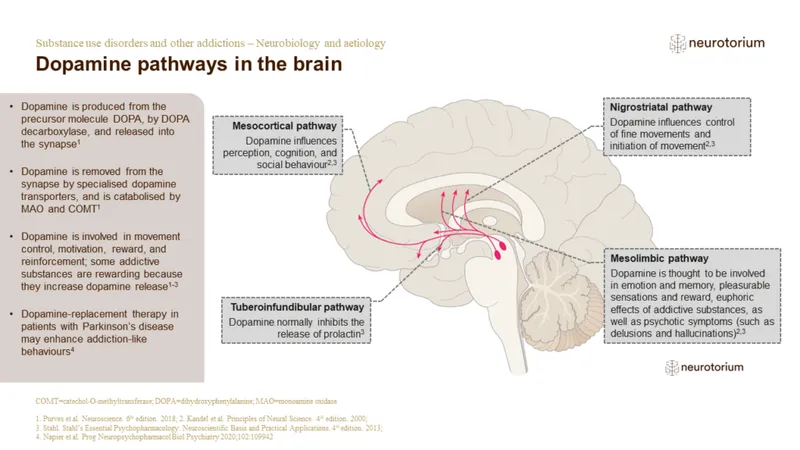
Neurobiological basis of delusions Explanation: ***Mesolimbic pathway***
- The **mesolimbic pathway** is primarily associated with the **positive symptoms of psychosis**, such as **hallucinations and delusions**, due to **dopamine hyperactivity**.
- The patient's **persecutory delusions, auditory hallucinations, and paranoia** are hallmark positive symptoms seen in conditions like schizophrenia, which are mediated by this pathway.
*Papez circuit*
- The **Papez circuit** is involved in **emotion and memory**, connecting structures like the hippocampus and cingulate gyrus.
- Dysregulation of this circuit would more likely manifest as deficits in memory or emotional regulation rather than the prominent psychotic features described.
*Mesocortical pathway*
- The **mesocortical pathway** projects to the **prefrontal cortex** and is implicated in **negative symptoms** (e.g., apathy, flat affect) and **cognitive deficits** (e.g., executive dysfunction) of psychosis, often due to **dopamine hypoactivity**.
- While cognitive and negative symptoms can co-occur in psychotic disorders, they are not the primary, most striking symptoms described here.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** is crucial for **motor control**, connecting the substantia nigra to the striatum.
- Dysfunction in this pathway leads to **extrapyramidal symptoms** (e.g., tremors, rigidity, dyskinesia), which are not present in this patient's presentation.
*Tuberoinfundibular pathway*
- The **tuberoinfundibular pathway** connects the hypothalamus to the pituitary gland and regulates **prolactin secretion**.
- Its primary role is in neuroendocrine function, and its dysfunction would lead to **hyperprolactinemia** and related symptoms, not the psychotic features described.
Neurobiological basis of delusions US Medical PG Question 9: Two days after undergoing hemicolectomy for colon cancer, a 78-year-old man is found agitated and confused in his room. He says that a burglar broke in. The patient points at one corner of the room and says “There he is, doctor!” Closer inspection reveals that the patient is pointing to his bathrobe, which is hanging on the wall. The patient has type 2 diabetes mellitus and arterial hypertension. Current medications include insulin and hydrochlorothiazide. His temperature is 36.9°C (98.4°F), pulse is 89/min, respirations are 15/min, and blood pressure is 145/98 mm Hg. Physical examination shows a nontender, nonerythematous midline abdominal wound. On mental status examination, the patient is agitated and oriented only to person. Which of the following best describes this patient's perception?
- A. Hallucination
- B. Illusion (Correct Answer)
- C. Loose association
- D. Delusion
- E. External attribution
Neurobiological basis of delusions Explanation: ***Illusion***
- An **illusion** is a **misinterpretation of an actual external stimulus**, as seen when the patient perceives his bathrobe as a burglar.
- This symptom, combined with **agitation**, **confusion**, and **recent surgery**, is highly suggestive of **delirium**.
*Hallucination*
- A **hallucination** is a **perception in the absence of an external stimulus**, meaning the patient would see or hear something that is not there at all.
- The patient here is clearly reacting to an existing object (the bathrobe), albeit misinterpreting it.
*Loose association*
- **Loose association** refers to a **thought disorder** where ideas shift from one subject to another in a way that is unrelated or minimally related, making the speech difficult to follow.
- This describes a pattern of thought, not a perceptual disturbance involving an external object.
*Delusion*
- A **delusion** is a **fixed, false belief** that is not amenable to change in light of conflicting evidence and is not in keeping with the individual's cultural background.
- While the patient believes a burglar is present, this belief arises from a direct misinterpretation of an object rather than a fixed, unfounded belief.
*External attribution*
- **External attribution** is a psychological concept where individuals ascribe responsibility for events or outcomes to **external factors** rather than internal ones.
- This term describes a cognitive bias in explaining causality, not a perceptual disturbance.
Neurobiological basis of delusions US Medical PG Question 10: A 23-year-old man presents to the emergency department with a chief complaint of being assaulted on the street. The patient claims that he has been followed by the government for quite some time and that he was assaulted by a government agent but was able to escape. He often hears voices telling him to hide. The patient has an unknown past medical history and admits to smoking marijuana frequently. On physical exam, the patient has no signs of trauma. When interviewing the patient, he is seen conversing with an external party that is not apparent to you. The patient states that he is afraid for his life and that agents are currently pursuing him. What is the best initial response to this patient’s statement?
- A. I think you are safe from the agents here.
- B. You have a mental disorder but don’t worry we will help you.
- C. I don’t think any agents are pursuing you.
- D. What medications are you currently taking?
- E. It sounds like you have been going through some tough experiences lately. (Correct Answer)
Neurobiological basis of delusions Explanation: ***It sounds like you have been going through some tough experiences lately.***
- This response **acknowledges the patient's distress** and experience without validating or refuting their delusional beliefs.
- It helps establish **rapport** and encourages the patient to share more about their symptoms, which is crucial for assessment in a psychiatric emergency.
*I think you are safe from the agents here.*
- While intended to reassure, directly addressing the delusion can be perceived as dismissive and may **escalate the patient's paranoia** or agitation.
- It does not validate their *feelings* of fear, which are real to them, even if the source is delusional.
*You have a mental disorder but don’t worry we will help you.*
- This statement is **confrontational** and judgmental, labeling the patient immediately with a diagnosis.
- This approach can cause the patient to become defensive, shut down, or feel stigmatized, making further assessment and trust-building very difficult in the **initial interaction**.
*I don’t think any agents are pursuing you.*
- Directly **challenging a patient's delusion** is generally unhelpful in acute settings and can lead to increased agitation.
- It invalidates their subjective reality and can make them feel misunderstood or distrustful of the healthcare provider.
*What medications are you currently taking?*
- While important information, asking about medications is too premature as an *initial response* to a patient expressing severe paranoia and fear.
- This question comes across as dismissive of their current emotional state and **prioritizes medical history over emotional support** and rapport-building.
More Neurobiological basis of delusions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.