Delusional disorder

On this page
🧠 The Delusional Mind: When Reality Gets Rewritten
You'll explore how the brain constructs unshakable false beliefs that resist all contradictory evidence, learning to recognize the seven distinct subtypes of delusional disorder and distinguish them from psychosis, mood disorders, and medical mimics. This lesson equips you to navigate the diagnostic challenge of patients whose reality has diverged from consensus while their personality and function remain largely intact, then master the pharmacological and psychotherapeutic strategies that can penetrate these fixed belief systems and restore insight.
The prevalence ranges from 0.02-0.05% in the general population, with equal gender distribution and typical onset between 40-49 years. The disorder's hallmark feature involves non-bizarre delusions-beliefs that could theoretically occur in real life, such as being followed, poisoned, or deceived by a spouse.
📌 Remember: DELUSIONAL - Delusions present, Everything else intact, Lasting >1 month, Unimpaired function, Specific themes, Insight absent, Occupational preserved, No bizarre content, Affect appropriate, Limited hallucinations
Core Diagnostic Architecture
- Primary Delusions (≥1 month duration)
- Fixed false beliefs resistant to contradictory evidence
- Non-bizarre content that could conceivably occur
- Maintained with complete conviction despite logical arguments
- Preserved Functioning
- Social relationships maintained outside delusional themes
- Occupational performance remains >80% of baseline
- Activities of daily living completely intact
- Absence of Prominent Psychotic Features
- Hallucinations rare or directly related to delusional theme
- No formal thought disorder or disorganized behavior
- Cognitive testing shows normal performance across domains
⭐ Clinical Pearl: 85% of patients with delusional disorder maintain employment throughout their illness, compared to only 15% of schizophrenia patients during active episodes.
| Feature | Delusional Disorder | Schizophrenia | Brief Psychotic Disorder | Substance-Induced | Major Depression with Psychosis |
|---|---|---|---|---|---|
| Duration | ≥1 month | ≥6 months | 1 day-1 month | Variable | ≥2 weeks |
| Functioning | Preserved | Severely impaired | Acutely impaired | Variable | Moderately impaired |
| Delusion Type | Non-bizarre | Often bizarre | Variable | Substance-related | Mood-congruent |
| Hallucinations | Rare/theme-related | Prominent | Variable | Common | Mood-congruent |
| Cognitive Impact | Minimal | Severe | Acute | Variable | Moderate |
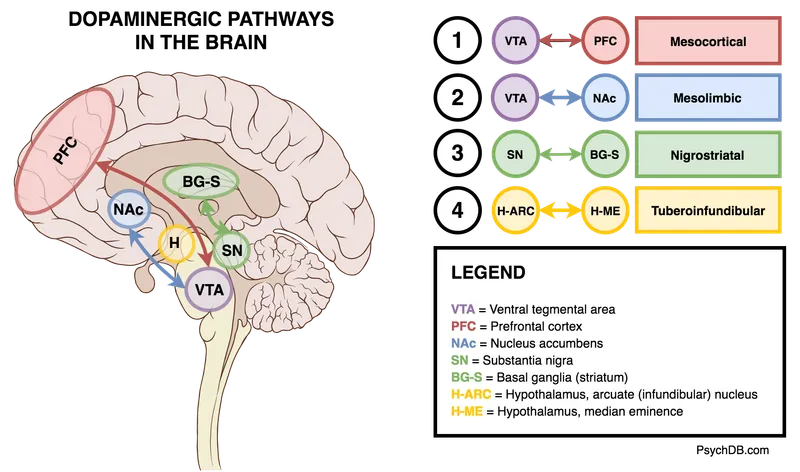
Understanding these foundational elements creates the framework for recognizing how aberrant salience and dopaminergic dysfunction generate the specific clinical presentations that follow.
🧠 The Delusional Mind: When Reality Gets Rewritten
🎭 The Delusion Spectrum: Mapping False Belief Territories
Persecutory Subtype: The Surveillance State
Most common subtype (60-70% of cases), involving beliefs of being conspired against, cheated, spied upon, or harmed. Patients maintain hypervigilance and may take protective actions that appear rational within their belief system.
- Core Themes
- Government surveillance or monitoring
- Workplace conspiracies or sabotage
- Neighbor harassment or property damage
- Identity theft or financial exploitation
- Risk Factors
- Male predominance (2:1 ratio)
- Social isolation increases risk 3-fold
- History of actual victimization in 40% of cases
- Violence Risk: 15-20% engage in protective behaviors that may harm perceived persecutors
📌 Remember: PARANOID - Persecution beliefs, Always vigilant, Rational within system, Actions protective, No other symptoms, Occupational preserved, Identity threatened, Danger to others possible
Jealous Subtype: The Relationship Detective
Involves unfounded conviction that sexual partner is unfaithful, leading to elaborate surveillance behaviors and evidence-gathering attempts. Shows highest violence potential among all subtypes.
- Demographics & Patterns
- Male predominance (3:1 ratio)
- Peak onset 35-45 years
- Alcohol use disorder comorbid in 60% of cases
- Behavioral Manifestations
- Checking partner's belongings, phone, computer
- Following or hiring investigators
- Interrogating about daily activities
- Installing surveillance equipment
- Violence Statistics: 35-40% commit domestic violence, 10% commit serious assault
Erotomanic Subtype: The Impossible Romance
Rare subtype (5% of cases) involving belief that someone of higher status is in love with the patient, typically communicated through special signs or messages.
- Classic Demographics
- Female predominance (3:1 ratio)
- Target usually male, higher social status
- Celebrity targets in 40% of cases
- Behavioral Escalation Pattern
- Phase 1: Hope and euphoria (weeks to months)
- Phase 2: Disappointment and anger (months to years)
- Phase 3: Resentment and potential violence (variable duration)
⭐ Clinical Pearl: 90% of celebrity stalking cases involve erotomanic delusions, with average pursuit duration of 2.5 years before intervention.
| Subtype | Prevalence | Gender Ratio | Violence Risk | Treatment Response | Typical Duration |
|---|---|---|---|---|---|
| Persecutory | 60-70% | M>F (2:1) | 15-20% | Moderate | Chronic |
| Jealous | 15-20% | M>F (3:1) | 35-40% | Poor | Chronic |
| Erotomanic | 5% | F>M (3:1) | 25-30% | Variable | Episodic |
| Grandiose | 5-10% | M=F | 5-10% | Good | Variable |
| Somatic | 5-10% | F>M (2:1) | <5% | Poor | Chronic |
Involves fixed beliefs about bodily functions, sensations, or appearance that cause significant distress and medical help-seeking behavior.
- Common Presentations
- Parasitic infestations (delusional parasitosis)
- Body odor or appearance defects
- Internal organ dysfunction
- Contamination or poisoning
- Medical Utilization: Average 8-12 medical consultations before psychiatric referral
- Treatment Challenges: 80% refuse psychiatric evaluation initially
💡 Master This: The "specimen sign" in delusional parasitosis-patients bring containers of skin debris, lint, or hair as "evidence" of infestation-occurs in 70% of cases and strongly suggests the diagnosis.
Understanding these subtype patterns enables clinicians to predict risk trajectories and tailor interventions to the specific neurobiological mechanisms driving each delusional theme.
🎭 The Delusion Spectrum: Mapping False Belief Territories
🔍 The Diagnostic Detective: Unraveling Delusional Presentations
The Clinical Interview Architecture
Establishing rapport becomes crucial since patients with delusional disorder maintain intact insight about everything except their specific delusion. Direct confrontation of beliefs triggers defensive responses and interview termination in 60% of cases.
- Opening Strategy
- Begin with neutral topics (work, family, hobbies)
- Assess general functioning and cognitive status
- Note any hypervigilance or guarded responses
- Gradually approach sensitive areas through indirect questioning
- Delusion Exploration Techniques
- "Some people have concerns about..." (normalizing approach)
- "Have you noticed anything unusual lately?" (open-ended)
- "How do you explain..." (understanding their logic)
- Avoid challenging beliefs directly during initial assessment
📌 Remember: INTERVIEW - Indirect approach, Neutral topics first, Trust building, Explore gradually, Rapport essential, Validate feelings, Insight preserved elsewhere, Evidence gathering, Watch for defensiveness
Mental Status Examination Patterns
The MSE in delusional disorder shows characteristic preservation of most functions with focal abnormalities related to the delusional theme.
- Appearance & Behavior
- Generally well-groomed and appropriate
- May show hypervigilance or scanning behaviors
- Guarded posture when discussing sensitive topics
- Normal psychomotor activity unless delusion-related
- Speech & Language
- Rate, rhythm, volume normal
- Vocabulary and syntax intact
- Content becomes circumstantial when discussing delusions
- Logical flow preserved outside delusional themes
- Mood & Affect
- Euthymic or mildly dysthymic baseline
- Intense affect when delusion discussed
- Appropriate emotional range in other contexts
- Anxiety present in 70% of cases
Cognitive Assessment Findings
Neuropsychological testing reveals the remarkable preservation that distinguishes delusional disorder from other psychotic conditions.
- Executive Function: Normal performance on Wisconsin Card Sort, Trail Making B
- Memory: Intact immediate, delayed, and working memory
- Attention: Sustained attention preserved except when delusion-triggered
- Language: Fluency, comprehension, naming normal
- Visuospatial: No deficits in construction or perception
⭐ Clinical Pearl: 95% of delusional disorder patients score within normal range on standardized cognitive batteries, compared to <20% of schizophrenia patients during active episodes.
| Assessment Domain | Delusional Disorder | Schizophrenia | Major Depression | Substance Use |
|---|---|---|---|---|
| Cognitive Testing | Normal (95%) | Impaired (80%) | Mild deficits (40%) | Variable |
| Insight Preservation | Partial (delusion-specific) | Severely impaired | Usually intact | Variable |
| Functional Capacity | Preserved (85%) | Severely impaired | Moderately impaired | Variable |
| Reality Testing | Focal impairment | Global impairment | Usually intact | Acute impairment |
| Social Cognition | Preserved | Severely impaired | Mildly impaired | Variable |
Family interviews provide crucial diagnostic information, as 85% of concerning behaviors occur outside clinical settings.
- Behavioral Changes Reported
- Social withdrawal from specific people/places
- Hypervigilance or checking behaviors
- Sleep disturbances related to fears
- Occupational conflicts with specific individuals
- Timeline Establishment
- Onset pattern: gradual vs. acute
- Trigger identification: stressors, losses, changes
- Progression tracking: worsening vs. stable
- Functional impact: work, relationships, self-care
💡 Master This: The "split-screen phenomenon"-patients function normally in non-delusion-related contexts while showing marked impairment in delusion-specific situations-occurs in 90% of delusional disorder cases and serves as a key diagnostic indicator.
This systematic assessment approach reveals the neurobiological specificity underlying delusional disorder and guides the targeted interventions that follow.
🔍 The Diagnostic Detective: Unraveling Delusional Presentations
⚖️ The Differential Diagnosis Matrix: Separating Signal from Noise
Primary Psychotic Disorder Differentiation
Schizophrenia represents the most critical differential, as treatment approaches and prognoses differ dramatically between conditions.
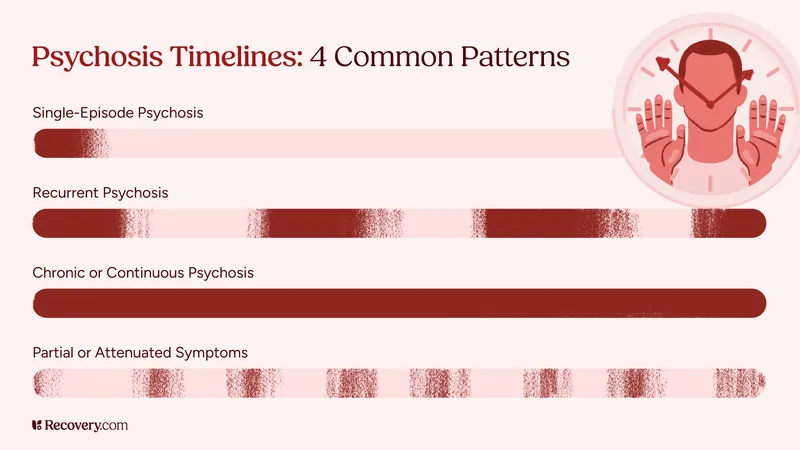
- Temporal Patterns
- Schizophrenia: Prodromal phase months to years, active symptoms ≥6 months
- Delusional Disorder: Acute onset possible, ≥1 month duration sufficient
- Brief Psychotic Disorder: 1 day to 1 month duration with full recovery
- Functional Trajectory
- Schizophrenia: Progressive decline in multiple domains
- Delusional Disorder: Preserved functioning outside delusion
- Brief Psychotic: Acute impairment with return to baseline
📌 Remember: FUNCTION - Functioning preserved, Unimpaired cognition, No formal thought disorder, Circumscribed delusions, Time limited hallucinations, Insight partially intact, Occupational maintained, Non-bizarre content
Substance-Induced Psychotic Disorders
Substance use accounts for 15-20% of psychotic presentations, requiring careful substance history and toxicology screening.
- High-Risk Substances
- Stimulants: Cocaine, amphetamines (paranoid delusions in 60%)
- Cannabis: THC concentrations >15% increase psychosis risk 5-fold
- Alcohol: Withdrawal delirium with paranoid features
- Hallucinogens: Persistent perceptual disturbances possible
- Temporal Relationships
- Intoxication: Symptoms during active use or within 24 hours
- Withdrawal: Symptoms during cessation period
- Persistent: Symptoms >1 month after substance clearance
Medical Condition Exclusions
Organic causes must be systematically excluded, as 10-15% of late-onset psychosis has identifiable medical etiology.
- Neurological Conditions
- Dementia: Alzheimer's (30% develop delusions), Lewy body (60%)
- Delirium: Acute confusional state with fluctuating consciousness
- Huntington's Disease: Paranoid delusions in 40% of cases
- Temporal Lobe Epilepsy: Interictal psychosis in 5-10%
- Endocrine Disorders
- Hyperthyroidism: Paranoid features in severe cases
- Cushing's Syndrome: Mood and psychotic symptoms
- Autoimmune Encephalitis: Anti-NMDA receptor antibodies
⭐ Clinical Pearl: Late-onset psychosis (>45 years) has 3-fold higher likelihood of organic etiology compared to early-onset cases, requiring comprehensive medical workup including neuroimaging and autoimmune panels.
| Condition | Onset Pattern | Duration | Functioning | Cognitive Status | Hallucinations |
|---|---|---|---|---|---|
| Delusional Disorder | Variable | ≥1 month | Preserved | Normal | Rare/theme-related |
| Schizophrenia | Gradual | ≥6 months | Severely impaired | Impaired | Prominent |
| Brief Psychotic | Acute | 1 day-1 month | Acutely impaired | Variable | Common |
| Substance-Induced | Related to use | Variable | Variable | Variable | Common |
| Medical Condition | Variable | Variable | Variable | Often impaired | Variable |
Major Depression with Psychotic Features and Bipolar Disorder can present with delusions, requiring careful mood episode assessment.
- Mood-Congruent Delusions
- Depression: Guilt, worthlessness, somatic themes
- Mania: Grandiose, special abilities themes
- Temporal relationship: Delusions only during mood episodes
- Functional Impairment Patterns
- Mood disorders: Global impairment during episodes
- Delusional disorder: Circumscribed impairment related to delusion
- Treatment Response
- Mood disorders: Mood stabilizers primary, antipsychotics adjunctive
- Delusional disorder: Antipsychotics primary treatment
💡 Master This: The "mood episode test"-if delusions occur exclusively during depressive or manic episodes and resolve with mood stabilization, consider mood disorder with psychotic features rather than primary delusional disorder.
This systematic differentiation process guides selection of targeted pharmacological interventions and psychotherapeutic approaches tailored to the underlying pathophysiology.
⚖️ The Differential Diagnosis Matrix: Separating Signal from Noise
💊 The Pharmacological Arsenal: Precision Targeting of Delusional Networks
Medication adherence represents the primary treatment challenge, with 60-70% of patients discontinuing therapy within 6 months due to side effects or lack of insight. Success requires strategic drug selection, gradual titration, and alliance building around functional goals rather than symptom elimination.
First-Line Antipsychotic Strategy
Atypical antipsychotics represent first-line treatment due to superior tolerability and lower extrapyramidal side effects, crucial for maintaining adherence in this population.
- Risperidone (Preferred Initial Choice)
- Starting dose: 0.5-1mg daily, titrate by 0.5mg weekly
- Target range: 2-6mg daily (lower than schizophrenia)
- Response timeline: 4-6 weeks for initial improvement
- Advantages: Extensive evidence base, predictable kinetics
- Monitoring: Prolactin levels, metabolic parameters
- Olanzapine (Alternative First-Line)
- Starting dose: 2.5-5mg daily, titrate by 2.5mg weekly
- Target range: 5-15mg daily
- Advantages: Lower EPS risk, good efficacy
- Disadvantages: Weight gain (7-10kg average), metabolic syndrome
📌 Remember: ATYPICAL - Adherence better, Tolerable profile, Yield good response, Prolactin elevation possible, Initial low dose, Careful titration, Adjust for function, Long-term monitoring
Dosing Optimization Principles
Lower doses than schizophrenia treatment often prove effective, as delusional disorder patients show enhanced sensitivity to antipsychotic effects.
- Dose-Response Relationships
- Therapeutic window: 50-70% of schizophrenia doses
- Minimum effective: Often 25-50% lower than package insert
- Maximum tolerated: Limited by side effect emergence
- Maintenance dosing: Lowest effective dose for long-term adherence
- Titration Strategies
- Start low: 25-50% of typical starting dose
- Go slow: Weekly increments maximum
- Monitor closely: Side effects before efficacy
- Functional goals: Preserve work/relationships while treating delusions
Second-Line and Adjunctive Options
Treatment-resistant cases (30-40% of patients) require alternative strategies and combination approaches.
- Aripiprazole (Partial Agonist Advantage)
- Mechanism: Dopamine partial agonist reduces side effect burden
- Dosing: 5-15mg daily (lower than schizophrenia)
- Benefits: Minimal weight gain, low EPS risk
- Timeline: 6-8 weeks for full effect
- Quetiapine (Sedating Option)
- Indication: Comorbid anxiety or sleep disturbance
- Dosing: 25-300mg daily (much lower than bipolar dosing)
- Advantages: Anxiolytic effects, sleep improvement
- Monitoring: Metabolic parameters, cataracts
⭐ Clinical Pearl: Clozapine shows superior efficacy in treatment-resistant delusional disorder, with 70% response rate vs. 40% for other antipsychotics, but requires weekly blood monitoring and specialized registration.
| Medication | Starting Dose | Target Range | Response Rate | Major Side Effects | Monitoring Required |
|---|---|---|---|---|---|
| Risperidone | 0.5-1mg | 2-6mg | 65-75% | Prolactin elevation, EPS | Prolactin, metabolic |
| Olanzapine | 2.5-5mg | 5-15mg | 60-70% | Weight gain, diabetes | Metabolic, lipids |
| Aripiprazole | 5mg | 5-15mg | 55-65% | Akathisia, nausea | Minimal |
| Quetiapine | 25mg | 50-300mg | 50-60% | Sedation, metabolic | Metabolic, eye exam |
| Clozapine | 12.5mg | 200-400mg | 70-80% | Agranulocytosis, seizures | Weekly CBC, ANC |
LAI formulations address adherence challenges in patients who acknowledge functional benefits but resist daily medication.
- Candidate Selection
- History of adherence problems with functional consequences
- Insight into medication benefits for work/relationship preservation
- Stable on oral formulation for ≥2 months
- Voluntary acceptance after education about advantages
- Preferred LAI Options
- Risperidone LAI: 25mg every 2 weeks, established efficacy
- Olanzapine pamoate: 150-300mg monthly, good tolerability
- Aripiprazole: 400mg monthly, minimal side effects
💡 Master This: Functional framing improves LAI acceptance-emphasize work performance, relationship stability, and reduced daily medication burden rather than symptom control, achieving 80% acceptance vs. 30% with symptom-focused discussions.
This pharmacological foundation enables integration with psychotherapeutic approaches that address the cognitive and behavioral aspects of delusional beliefs.
💊 The Pharmacological Arsenal: Precision Targeting of Delusional Networks
🧠 The Therapeutic Alliance: Rewiring Delusional Networks
Cognitive Behavioral Therapy (CBT) represents the evidence-based psychotherapeutic approach with demonstrated efficacy in reducing delusion conviction and improving functional outcomes. Success rates reach 60-70% when combined with appropriate pharmacotherapy and skilled therapeutic alliance building.
Therapeutic Alliance Foundation
Trust establishment proves crucial since 85% of patients enter therapy involuntarily or under external pressure from family, employers, or legal systems.
- Initial Engagement Strategies
- Validate emotional distress without confirming delusional content
- Focus on functional goals (work, relationships, sleep, anxiety)
- Avoid direct delusion challenges during first 4-6 sessions
- Demonstrate competence through accurate assessment and helpful interventions
- Alliance Building Techniques
- Collaborative goal setting around patient-identified problems
- Psychoeducation about stress, anxiety, and coping
- Skill building for emotional regulation and interpersonal effectiveness
- Gradual introduction of alternative explanations
📌 Remember: ALLIANCE - Accept their distress, Listen without judgment, Link to function, Introduce alternatives gradually, Avoid confrontation, Navigate resistance, Collaborate on goals, Emphasize coping
Cognitive Restructuring Methodology
CBT techniques target the cognitive biases and reasoning errors that maintain delusional beliefs while preserving therapeutic relationship.
- Thought Record Implementation
- Situation identification: Specific delusion-triggering events
- Emotion tracking: Intensity ratings (0-10 scale) for anxiety, anger, fear
- Thought identification: Automatic thoughts and underlying beliefs
- Evidence examination: Supporting and contradicting information
- Alternative generation: Multiple possible explanations for events
- Behavioral Experiments
- Hypothesis testing: Predictions based on delusional beliefs
- Data collection: Objective observation of predicted outcomes
- Result evaluation: Comparison of predictions vs. actual events
- Belief modification: Gradual adjustment based on contradictory evidence
Specific CBT Interventions
Structured techniques address the cognitive distortions characteristic of delusional thinking patterns.
- Jumping to Conclusions Bias
- Technique: Evidence gathering before conclusion formation
- Exercise: "What else could explain this?" questioning
- Goal: Increase consideration of alternative explanations
- Success rate: 40-50% reduction in hasty conclusions
- Confirmation Bias Correction
- Technique: Actively seeking disconfirming evidence
- Exercise: "Devil's advocate" role-playing
- Goal: Balanced information processing
- Outcome: 30-40% improvement in evidence evaluation
- Attribution Style Modification
- Technique: External attribution training for negative events
- Exercise: Multiple causation analysis
- Goal: Reduced personalization and blame attribution
- Effect: 25-35% decrease in persecutory interpretations
⭐ Clinical Pearl: Socratic questioning proves more effective than direct confrontation, with 65% of patients showing reduced delusion conviction when therapists use guided discovery rather than argumentative approaches.
| CBT Technique | Target Bias | Session Focus | Success Rate | Timeline |
|---|---|---|---|---|
| Thought Records | Multiple biases | Evidence evaluation | 60-70% | 8-12 sessions |
| Behavioral Experiments | Jumping to conclusions | Hypothesis testing | 50-60% | 6-10 sessions |
| Alternative Explanations | Confirmation bias | Perspective taking | 40-50% | 10-15 sessions |
| Attribution Training | Personalizing bias | Causation analysis | 35-45% | 12-16 sessions |
| Reality Testing | General distortions | Fact checking | 55-65% | 15-20 sessions |
Family involvement enhances treatment outcomes, as family stress correlates with symptom exacerbation and treatment dropout.
- Family Education Components
- Disorder psychoeducation: Symptoms, course, prognosis
- Communication training: Non-confrontational approaches
- Stress management: Family coping strategies
- Crisis planning: Warning signs and intervention protocols
- Supportive Therapy Elements
- Practical problem-solving for daily life challenges
- Social skills training for relationship maintenance
- Stress reduction techniques for anxiety management
- Medication adherence support and side effect management
💡 Master This: Family expressed emotion levels predict treatment outcomes-high criticism or emotional over-involvement increases relapse risk by 3-fold, while supportive, low-key family approaches improve long-term stability and functional recovery.
These psychotherapeutic interventions integrate with pharmacological treatments to address both the neurobiological and psychological aspects of delusional disorder, creating comprehensive recovery frameworks for sustained improvement.
🧠 The Therapeutic Alliance: Rewiring Delusional Networks
🎯 The Clinical Mastery Toolkit: Rapid Assessment and Intervention
Rapid Assessment Protocol
5-Minute Screening for delusional disorder in clinical settings:
- Functional Preservation Check
- Work performance: "Any problems at your job lately?"
- Relationship status: "How are things with family/friends?"
- Self-care: "Any changes in sleep, appetite, hygiene?"
- Red flag: Selective impairment in specific domains
- Delusion Detection Questions
- "Do you feel safe in your daily life?"
- "Are there people you avoid or don't trust?"
- "Have you noticed anything unusual happening around you?"
- "Do others understand your concerns?"
📌 Remember: RAPID - Relationships preserved, Assess safety concerns, Partial insight present, Isolated delusions, Daily function maintained
Essential Clinical Numbers
Critical thresholds for immediate clinical decision-making:
- Violence Risk Indicators
- Jealous subtype: 35-40% violence rate
- Command hallucinations: 50% compliance rate
- Substance use comorbidity: 3-fold increased risk
- Prior violence history: 5-fold increased risk
- Treatment Response Timelines
- Initial improvement: 4-6 weeks antipsychotic therapy
- Significant response: 8-12 weeks combined treatment
- Maintenance stability: 6-12 months continuous treatment
- Relapse prevention: 2+ years optimal duration
| Clinical Scenario | Immediate Action | Timeline | Success Rate |
|---|---|---|---|
| Acute agitation | Low-dose antipsychotic | 24-48 hours | 70-80% |
| Violence threat | Safety planning + medication | Immediate | Variable |
| Treatment refusal | Alliance building | 2-4 weeks | 60-70% |
| Family crisis | Crisis intervention | 1-2 sessions | 80-90% |
Emergency management protocols for high-risk presentations:
- Violence Risk Assessment
- Specific threats: Names, plans, weapons access
- Delusion content: Persecution, jealousy, grandiosity
- Substance use: Current intoxication or withdrawal
- Support system: Family availability and safety
- Immediate Interventions
- Safety planning: Remove weapons, increase supervision
- Rapid medication: Risperidone 1-2mg or olanzapine 5-10mg
- Family education: De-escalation techniques, crisis contacts
- Follow-up: 24-48 hour reassessment
⭐ Clinical Pearl: Involuntary commitment criteria met in 15-20% of delusional disorder presentations, typically involving imminent violence risk or severe functional deterioration rather than delusion presence alone.
Treatment Selection Algorithm
Systematic approach to medication and therapy selection:
Long-Term Management Essentials
Maintenance strategies for sustained recovery:
- Medication Optimization
- Minimum effective dose for side effect minimization
- LAI consideration for adherence problems
- Regular monitoring: Metabolic parameters every 3-6 months
- Dose adjustments: Stress-related or seasonal variations
- Psychosocial Maintenance
- Monthly therapy sessions during stable periods
- Family check-ins every 2-3 months
- Occupational support as needed
- Crisis plan updates annually
💡 Master This: Functional recovery rather than complete delusion elimination represents the realistic treatment goal-80% of patients achieve stable employment and relationship maintenance while retaining modified delusional beliefs with reduced conviction and behavioral impact.
This comprehensive toolkit enables clinicians to rapidly assess, appropriately treat, and effectively manage delusional disorder across acute presentations and long-term care scenarios, optimizing patient outcomes and functional recovery.
🎯 The Clinical Mastery Toolkit: Rapid Assessment and Intervention
Practice Questions: Delusional disorder
Test your understanding with these related questions
A 55-year-old male was picked up by police in the public library for harassing the patrons and for public nudity. He displayed disorganized speech and believed that the books were the only way to his salvation. Identification was found on the man and his sister was called to provide more information. She described that he recently lost his house and got divorced within the same week although he seemed fine three days ago. The man was sedated with diazepam and chlorpromazine because he was very agitated. His labs returned normal and within three days, he appeared normal, had no recollection of the past several days, and discussed in detail how stressful the past two weeks of his life were. He was discharged the next day. Which of the following is the most appropriate diagnosis for this male?













