Pharmacotherapy for cognitive disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pharmacotherapy for cognitive disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pharmacotherapy for cognitive disorders US Medical PG Question 1: A 31-year-old male presents to the emergency room following an altercation with patrons at a local grocery store. He is acting aggressively toward hospital staff and appears to be speaking to non-existent individuals. On examination he is tachycardic and diaphoretic. Horizontal and vertical nystagmus is noted. The patient eventually admits to taking an illegal substance earlier in the evening. Which of the following mechanisms of action is most consistent with the substance this patient took?
- A. Mu receptor agonist
- B. GABA agonist
- C. Biogenic amine reuptake inhibitor
- D. NMDA receptor antagonist (Correct Answer)
- E. Adenosine antagonist
Pharmacotherapy for cognitive disorders Explanation: ***NMDA receptor antagonist***
- The patient's presentation with **aggressiveness**, **psychosis** (speaking to non-existent individuals), **tachycardia**, **diaphoresis**, and particularly **horizontal and vertical nystagmus**, is highly consistent with **phencyclidine (PCP) intoxication**.
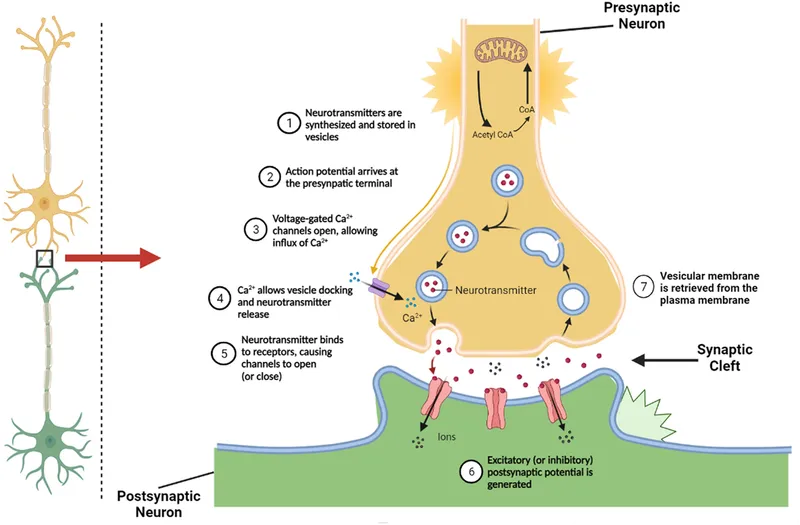
- PCP primarily acts as an **NMDA receptor antagonist**, blocking the activity of glutamate, which leads to its dissociative and psychotomimetic effects.
*Mu receptor agonist*
- **Mu receptor agonists** (e.g., opioids like heroin, morphine) typically cause central nervous system **depression**, miosis (pinpoint pupils), respiratory depression, and euphoria.
- The patient's **aggressiveness**, nystagmus, and tachycardia are **not characteristic of opioid intoxication**.
*GABA agonist*
- **GABA agonists** (e.g., benzodiazepines, barbiturates, alcohol) typically cause central nervous system **depression**, sedation, anxiolysis, and ataxia, and can lead to respiratory depression in overdose.
- The patient's agitation, psychosis, and nystagmus (especially vertical) are **not typical effects of GABAergic drugs**.
*Biogenic amine reuptake inhibitor*
- **Biogenic amine reuptake inhibitors** (e.g., cocaine, amphetamines) increase levels of neurotransmitters like dopamine, norepinephrine, and serotonin, leading to stimulant effects such as euphoria, agitation, paranoia, tachycardia, and hypertension.
- While some symptoms like tachycardia and agitation are consistent, the prominent **vertical nystagmus** and dissociative psychosis are generally **not hallmarks of stimulant intoxication**.
*Adenosine antagonist*
- **Adenosine antagonists** (e.g., caffeine) cause central nervous system stimulation, leading to increased alertness, restlessness, and mild tachycardia.
- The severe psychomotor agitation, prominent psychosis, and nystagmus seen in this patient are **far beyond the effects of typical adenosine antagonists**.
Pharmacotherapy for cognitive disorders US Medical PG Question 2: A 63-year-old woman is brought to the clinic by her husband with complaints of cognitive decline. The patient's husband says that she has had intermittent problems with her memory for the past few years. He says she has occasional 'bad days' where her memory deteriorates to the point where she cannot perform activities of daily living. She is also sometimes found conversing in an empty room and, when inquired, she confirms that she is talking to a friend. There have also been some recent falls. There is no history of fever, recent head trauma, loss of consciousness, or illicit drug use. Past medical history is significant for bronchial asthma and osteoarthritis, both managed medically. Her mother died due to metastatic breast cancer at age 71 and her father was diagnosed with Alzheimer's disease at age 65. The patient is afebrile and her vital signs are within normal limits. Physical examination reveals a tremor present in both her hands that attenuates with voluntary movement. Deep tendon reflexes are 2+ bilaterally. Romberg's sign is negative. She has a slow gait with a mild stooped posture. Her laboratory findings are significant for the following:
Hemoglobin 12.9 g/dL
White cell count 8,520/mm³
Platelets 295,000/mm³
Serum creatinine 1.0 mg/dL
Glucose 94 mg/dL
Sodium 141 mEq/L
Potassium 3.9 mEq/L
Calcium 92 mg/dL
Ferritin 125 ng/mL
Serum B12 305 ng/L
TSH 2.1 µU/mL
Ceruloplasmin 45 mg/dL
Which of the following is the most appropriate management for this patient?
- A. Escitalopram
- B. Penicillamine
- C. Haloperidol
- D. Ropinirole
- E. Rivastigmine (Correct Answer)
Pharmacotherapy for cognitive disorders Explanation: ***Rivastigmine***
- The patient exhibits classic symptoms of **dementia with Lewy bodies (DLB)**, including cognitive fluctuations, visual hallucinations (conversing in an empty room), and parkinsonism (tremor, slow gait, stooped posture, and falls). **Cholinesterase inhibitors** like **rivastigmine** are the first-line treatment for cognitive and neuropsychiatric symptoms in DLB as they can help improve cognitive function and reduce hallucinations.
- While Parkinson's disease itself is not the primary diagnosis, the presence of **parkinsonian features** and cognitive decline with hallucinations makes DLB a strong consideration. Rivastigmine increases the availability of **acetylcholine** in the brain, improving cognitive function and behavioral symptoms in DLB.
*Escitalopram*
- **Escitalopram** is an **SSRI antidepressant** and would be appropriate if the patient's primary symptoms were **depression or anxiety**.
- While depression can coexist with dementia, the described symptoms of cognitive fluctuations, hallucinations, and parkinsonism are not primarily indicative of depression.
*Penicillamine*
- **Penicillamine** is a **chelating agent** used primarily in the treatment of **Wilson's disease**, which is characterized by copper accumulation.
- The patient's **ceruloplasmin levels are normal**, making Wilson's disease unlikely, and the clinical presentation does not align with typical Wilson's disease symptoms.
*Haloperidol*
- **Haloperidol** is a **first-generation antipsychotic** that could be used for severe behavioral disturbances or psychosis.
- However, in patients with **dementia with Lewy bodies (DLB)**, antipsychotics, particularly typical ones like haloperidol, can significantly worsen parkinsonian symptoms and cognitive function due to **extreme sensitivity to neuroleptics**.
*Ropinirole*
- **Ropinirole** is a **dopamine agonist** primarily used in the treatment of **Parkinson's disease** to manage motor symptoms.
- While the patient has parkinsonian features, the prominent cognitive fluctuations and visual hallucinations point more towards **Dementia with Lewy Bodies (DLB)**, where dopamine agonists can sometimes exacerbate hallucinations and other neuropsychiatric symptoms.
Pharmacotherapy for cognitive disorders US Medical PG Question 3: A 70-year-old female presents to you for an office visit with complaints of forgetfulness. The patient states that over the last several years, the patient has stopped cooking for herself even though she lives alone. Recently, she also forgot how to drive back home from the grocery store and has difficulty paying her bills. The patient says she has been healthy over her whole life and does not take any medications. Her vitals are normal and her physical exam does not reveal any focal neurological deficits. Her mini-mental status exam is scored 19/30 and her MRI reveals diffuse cortical atrophy. What is the best initial treatment for this patient's condition?
- A. Rivastigmine (Correct Answer)
- B. Memantine
- C. Bromocriptine
- D. Pramipexole
- E. Ropinirole
Pharmacotherapy for cognitive disorders Explanation: ***Rivastigmine***
- This patient presents with symptoms and signs consistent with **Alzheimer's disease**, including gradual onset of **cognitive decline** impacting daily activities and diffuse cortical atrophy on MRI.
- **Rivastigmine** is an **acetylcholinesterase inhibitor** indicated for mild-to-moderate Alzheimer's disease, which works by increasing acetylcholine levels in the brain.
*Memantine*
- **Memantine** is an **NMDA receptor antagonist** typically used for **moderate-to-severe Alzheimer's disease**, often in combination with acetylcholinesterase inhibitors.
- While it can be beneficial, it is generally not considered the *initial* treatment for mild-to-moderate cases where acetylcholinesterase inhibitors are preferred.
*Bromocriptine*
- **Bromocriptine** is a **dopamine agonist** primarily used in the treatment of **Parkinson's disease** or hyperprolactinemia.
- It is not indicated for the management of Alzheimer's disease and would not address the underlying cholinergic deficit.
*Pramipexole*
- **Pramipexole** is a **dopamine agonist** used to treat **Parkinson's disease** and restless legs syndrome.
- It does not have a role in the treatment of Alzheimer's disease or other forms of dementia.
*Ropinirole*
- **Ropinirole** is another **dopamine agonist** primarily used for **Parkinson's disease** and restless legs syndrome.
- It is not an appropriate treatment for the cognitive decline seen in Alzheimer's disease.
Pharmacotherapy for cognitive disorders US Medical PG Question 4: A 72-year-old man is brought to the physician by his wife for forgetfulness, confusion, and mood changes for the past 4 months. His symptoms started with misplacing items such as his wallet and keys around the house. Two months ago, he became unable to manage their finances as it became too difficult for him. Last week, he became lost while returning home from the grocery store. His wife reports that he shows “no emotion” and that he is seemingly not concerned by his recent symptoms. He has hypertension, type 2 diabetes mellitus, and coronary artery disease. Current medications include aspirin, metoprolol, lisinopril, metformin, and rosuvastatin. His pulse is 56/min and blood pressure is 158/76 mm Hg. Neurologic examination shows loss of sensation on his right leg and an unsteady gait. When asked to stand with his eyes closed and palms facing upward, his right arm rotates inward. An MRI of the brain shows multiple deep white matter lesions. Which of the following is the most likely diagnosis?
- A. Vitamin B12 deficiency
- B. Frontotemporal dementia
- C. Alzheimer disease
- D. Lewy body dementia
- E. Vascular dementia (Correct Answer)
Pharmacotherapy for cognitive disorders Explanation: ***Vascular dementia***
- The patient's history of **hypertension, type 2 diabetes mellitus, and coronary artery disease** indicates significant vascular risk factors. The **multiple deep white matter lesions** on MRI are characteristic findings in vascular dementia, resulting from chronic **cerebral ischemia**.
- The **insidious onset** with progressive **cognitive decline** (forgetfulness, confusion, financial difficulties, getting lost) combined with **focal neurological deficits** (loss of sensation, unsteady gait, pronator drift), and "no emotion" or lack of concern, strongly points towards vascular dementia.
*Vitamin B12 deficiency*
- While vitamin B12 deficiency can cause cognitive impairment and neurological symptoms, it typically manifests with **megaloblastic anemia** and **peripheral neuropathy**, which are not noted in this case.
- The MRI findings of **multiple deep white matter lesions** are not characteristic of vitamin B12 deficiency, and the patient's extensive vascular risk factors are more indicative of a cerebrovascular etiology.
*Frontotemporal dementia*
- Characterized primarily by **early and prominent behavioral and personality changes** (e.g., disinhibition, apathy) or **language deficits**. While apathy is present ("no emotion"), the prominent **focal neurological deficits** and MRI findings of deep white matter lesions are less typical.
- Unlike this case, memory impairment is usually not the initial or most prominent symptom in frontotemporal dementia until later stages, which contrasts with the patient's initial presentation of forgetfulness.
*Alzheimer disease*
- Alzheimer disease typically presents with **progressive memory impairment** as the hallmark symptom, often preceding other cognitive or neurological deficits. While memory loss is present here, the rapid progression (4 months), prominent focal neurological signs, and vascular risk factors are less typical.
- MRI would typically show **cortical atrophy**, particularly in the hippocampus and medial temporal lobes, rather than multiple deep white matter lesions without significant atrophy.
*Lewy body dementia*
- Key features include **fluctuating cognition, recurrent visual hallucinations**, and spontaneous **parkinsonism**. None of these core features are explicitly described in the patient's presentation.
- While mood changes and apathy can occur, the presence of **focal neurological deficits** and deep white matter lesions on MRI are not primary characteristics of Lewy body dementia.
Pharmacotherapy for cognitive disorders US Medical PG Question 5: A 45-year-old woman comes to the physician because of a 6-month history of worsening involuntary movement of the left hand. Her symptoms are worse when she feels stressed at work. She has no history of serious illness and takes no medications. Neurological examination shows difficulty initiating movement and a tremor in the left hand at rest. The tremor decreases when the patient is asked to draw a circle. Which of the following is the most appropriate pharmacotherapy?
- A. Trihexyphenidyl
- B. Pramipexole (Correct Answer)
- C. Clonazepam
- D. Donepezil
- E. Methimazole
Pharmacotherapy for cognitive disorders Explanation: ***Pramipexole***
- This patient's symptoms of difficulty initiating movement, a **resting tremor** that improves with purposeful movement, and worsening with stress are characteristic of **Parkinson's disease**.
- **Pramipexole** is a **dopamine agonist** that directly stimulates dopamine receptors, effectively treating motor symptoms in Parkinson's disease.
*Trihexyphenidyl*
- **Trihexyphenidyl** is an **anticholinergic** agent primarily used for Parkinson's disease symptoms like **tremor** and **dystonia**, especially in younger patients.
- However, its side effects (e.g., dry mouth, blurred vision, confusion) are more pronounced in older patients, and **dopamine agonists** are generally preferred for initial treatment of motor symptoms in middle-aged adults.
*Clonazepam*
- **Clonazepam** is a **benzodiazepine** used to treat anxiety, seizures, and some movement disorders like essential tremor or restless legs syndrome.
- It is not a primary treatment for **Parkinson's disease** and would not address the underlying dopaminergic deficit or difficulty initiating movement.
*Donepezil*
- **Donepezil** is an **acetylcholinesterase inhibitor** used to treat the cognitive symptoms of Alzheimer's disease.
- It has no role in the treatment of the motor symptoms of **Parkinson's disease**.
*Methimazole*
- **Methimazole** is an **antithyroid medication** used to treat hyperthyroidism.
- It has no relevance to the neurological symptoms presented by the patient, which are indicative of a movement disorder.
Pharmacotherapy for cognitive disorders US Medical PG Question 6: A 7-year-old boy is brought in to clinic by his parents with a chief concern of poor performance in school. The parents were told by the teacher that the student often does not turn in assignments, and when he does they are partially complete. The child also often shouts out answers to questions and has trouble participating in class sports as he does not follow the rules. The parents of this child also note similar behaviors at home and have trouble getting their child to focus on any task such as reading. The child is even unable to watch full episodes of his favorite television show without getting distracted by other activities. The child begins a trial of behavioral therapy that fails. The physician then tries pharmacological therapy. Which of the following is most likely the mechanism of action of an appropriate treatment for this child's condition?
- A. Increases the frequency of GABAa channel opening
- B. Increases the duration of GABAa channel opening
- C. Decreases synaptic reuptake of norepinephrine and dopamine (Correct Answer)
- D. Blockade of D2 receptors
- E. Antagonizes NMDA receptors
Pharmacotherapy for cognitive disorders Explanation: ***Decreases synaptic reuptake of norepinephrine and dopamine***
- The presented symptoms (inattention, impulsivity, hyperactivity) are characteristic of **Attention-Deficit/Hyperactivity Disorder (ADHD)**.
- The most common pharmacological treatments for ADHD are **stimulants** (e.g., methylphenidate, amphetamines) which work by **inhibiting the reuptake of norepinephrine and dopamine**, thereby increasing their synaptic concentrations.
*Increases the frequency of GABAa channel opening*
- This is the mechanism of action for **benzodiazepines**, which are primarily used for anxiety, seizures, and insomnia.
- Benzodiazepines are not indicated for ADHD and would likely worsen symptoms due to their sedative effects.
*Increases the duration of GABAa channel opening*
- This describes the mechanism of action of **barbiturates**, which are potent central nervous system depressants.
- Like benzodiazepines, barbiturates are not used for ADHD and would have inappropriate sedative side effects.
*Blockade of D2 receptors*
- This is the primary mechanism of action for **antipsychotic medications**, used to treat conditions like schizophrenia or bipolar disorder.
- Blocking D2 receptors would likely cause side effects such as drowsiness and extrapyramidal symptoms, and would not address the core symptoms of ADHD.
*Antagonizes NMDA receptors*
- NMDA receptor antagonists (e.g., memantine, ketamine) are used in conditions like **Alzheimer's disease** or for anesthetic purposes.
- This mechanism is not relevant to the treatment of ADHD; enhancing NMDA receptor activity might actually be beneficial in some cognitive disorders.
Pharmacotherapy for cognitive disorders US Medical PG Question 7: A 65-year-old woman presents with memory problems for the past few weeks. Patient vividly describes how she forgot where she put her car keys this morning and did not remember to wish her grandson a happy birthday last week. Patient denies any cognitive problems, bowel/bladder incontinence, tremors, gait problems, or focal neurologic signs. Patient mentions she wants to take Ginkgo because her friend told her that it can help improve her brain function and prevent memory loss. Past medical history is significant for an acute cardiac event several years ago. Current medications are aspirin, carvedilol, and captopril. Patient denies any history of smoking, alcohol or recreational drug use. Patient is a widow, lives alone, and is able to perform all activities of daily living (ADLs) easily. No significant family history. Patient is afebrile and vital signs are within normal limits. Physical examination is unremarkable. Which of the following would be the most appropriate response to this patient’s request to take Ginkgo?
- A. "Yes, ginkgo is widely used for improving brain function and memory."
- B. “No, you have Alzheimer's disease and need to start donepezil.”
- C. “No, herbal preparations are unsafe because they are not regulated by the FDA.”
- D. "No, taking ginkgo will increase your risk for bleeding." (Correct Answer)
- E. Yes, ginkgo may not help with your memory, but there is no risk of adverse events so it is safe to take.
Pharmacotherapy for cognitive disorders Explanation: ***"No, taking ginkgo will increase your risk for bleeding."***
- **Ginkgo biloba** has known antithrombotic effects due to its inhibition of platelet-activating factor, which can increase the risk of **bleeding**, especially when combined with other antithrombotic agents like **aspirin**, which this patient is taking.
- Given her history of a cardiac event and current aspirin use, adding ginkgo would significantly raise her risk of hemorrhagic complications.
*"Yes, ginkgo is widely used for improving brain function and memory."*
- While ginkgo is popularly marketed for cognitive enhancement, there is **insufficient scientific evidence** to support its effectiveness in improving memory or preventing cognitive decline.
- Recommending it based solely on popular belief disregards evidence-based medicine and potential patient risks.
*"No, you have Alzheimer's disease and need to start donepezil.”*
- This is an inappropriate response as a diagnosis of **Alzheimer's disease** cannot be made based solely on the patient's self-reported memory issues; a comprehensive workup is required.
- Additionally, immediately prescribing **donepezil** without a confirmed diagnosis and without discussing potential risks or alternatives is premature and goes against diagnostic protocols.
*"No, herbal preparations are unsafe because they are not regulated by the FDA."*
- While it's true that **herbal preparations** are not regulated by the FDA in the same way as prescription drugs, labeling all such preparations as "unsafe" is an **overgeneralization**.
- The primary concern here is not just the lack of FDA regulation, but the specific **pharmacological interaction** of ginkgo with her current medications.
*"Yes, ginkgo may not help with your memory, but there is no risk of adverse events so it is safe to take."*
- This statement is incorrect because, as explained, ginkgo carries a significant **risk of adverse events**, particularly **increased bleeding risk**, especially in this patient due to her concomitant aspirin use.
- It is critical to acknowledge and address potential drug interactions and side effects, rather than dismissing them.
Pharmacotherapy for cognitive disorders US Medical PG Question 8: A 78-year-old man is brought to the physician by his daughter for a follow-up examination. The daughter noticed that he has gradually become more forgetful and withdrawn over the last year. He frequently misplaces his car keys and forgets the names of his neighbors, whom he has known for 30 years. He has difficulty recalling his address and telephone number. He recently had an episode of urinary and fecal incontinence. Last week, his neighbor found him wandering the parking lot of the grocery store. He has hypertension and hyperlipidemia. He had smoked one pack of cigarettes daily for 40 years but quit 18 years ago. His current medications include hydrochlorothiazide and atorvastatin. He appears healthy; BMI is 23 kg/m2. His temperature is 37.2°C (99.0°F), pulse is 86/min, respirations are 14/min, and blood pressure is 136/84 mm Hg. Mini-mental state examination score is 19/30. He is not bothered by his forgetfulness. Cranial nerves II–XII are intact. He has 5/5 strength and full sensation to light touch in all extremities. His patellar, Achilles, and biceps reflexes are 2+ bilaterally. His gait is steady. MRI scan of the brain shows ventriculomegaly and prominent cerebral sulci. Which of the following is the most appropriate pharmacotherapy?
- A. Acetazolamide
- B. Sertraline
- C. Memantine
- D. Thiamine
- E. Donepezil (Correct Answer)
Pharmacotherapy for cognitive disorders Explanation: ***Donepezil***
- The patient exhibits features consistent with **Alzheimer's disease**, including gradual memory loss, difficulty with daily tasks, episodes of incontinence, and a Mini-Mental State Examination (MMSE) score of 19/30. Donepezil, a **cholinesterase inhibitor**, is a first-line treatment for mild to moderate Alzheimer's to slow cognitive decline.
- The MRI findings of **ventriculomegaly and prominent cerebral sulci** are consistent with general cerebral atrophy often seen in Alzheimer's disease, not hydrocephalus requiring shunting or other specific brain pathologies (normal pressure hydrocephalus would have gait disturbance as a prominent feature, which is absent here).
*Acetazolamide*
- **Acetazolamide** is a **carbonic anhydrase inhibitor** used to treat conditions like glaucoma, altitude sickness, and idiopathic intracranial hypertension.
- There is no indication of elevated intracranial pressure or hydrocephalus that would warrant the use of acetazolamide in this patient.
*Sertraline*
- **Sertraline** is a **selective serotonin reuptake inhibitor (SSRI)** primarily used to treat depression, anxiety disorders, and obsessive-compulsive disorder.
- While depression can coexist with dementia, the primary cognitive symptoms described here are not primarily depressive; therefore, an antidepressant is not the most appropriate initial pharmacotherapy for cognitive decline.
*Memantine*
- **Memantine** is an **NMDA receptor antagonist** used in moderate to severe Alzheimer's disease, often in combination with cholinesterase inhibitors or when cholinesterase inhibitors are not tolerated.
- While appropriate for moderate to severe Alzheimer's, **cholinesterase inhibitors** are typically the initial treatment for mild to moderate stages, and the patient's MMSE score of 19/30 often falls into the mild-moderate category where donepezil is usually favored first.
*Thiamine*
- **Thiamine** (vitamin B1) supplementation is primarily used to treat **Wernicke-Korsakoff syndrome**, which is associated with chronic alcohol abuse and presents with ataxia, ophthalmoplegia, and confusion, none of which are the primary presenting symptoms here.
- There is no evidence of **nutritional deficiency** or alcohol abuse in this patient to suggest thiamine deficiency as the cause of his cognitive decline.
Pharmacotherapy for cognitive disorders US Medical PG Question 9: A 68-year-old man seeks evaluation by a physician with complaints of worsening forgetfulness and confusion for 1 year. According to his wife, he has always been in good health and is generally very happy; however, he has started to forget important things. He recently had his driving license revoked because of multiple tickets, but he cannot recall having done anything wrong. This morning, he neglected to put on his socks and was quite agitated when she pointed this out to him. He denies having a depressed mood, sleep problems, or loss of interest. He occasionally has a glass of wine with dinner and has never smoked or used recreational drugs. His medical history and family medical history are unremarkable. His pulse is 68/min, respirations are 14/min, and blood pressure is 130/84 mm Hg. Except for a mini-mental state examination (MMSE) score of 20/30, the remainder of the physical examination is unremarkable. Imaging studies, including a chest X-ray and CT of the brain, reveal no pathologic findings. An electrocardiogram (ECG) is also normal. Laboratory testing showed the following:
Serum glucose (fasting) 76 mg/dL
Serum electrolytes:
Sodium 140 mEq/L
Potassium 4.1 mEq/L
Chloride 100 mEq/L
Serum creatinine 0.9 mg/dL
Blood urea nitrogen 11 mg/dL
Cholesterol, total: 180 mg/dL
HDL-cholesterol 45 mg/dL
LDL-cholesterol 75 mg/dL
Triglycerides 135 mg/dL
Hemoglobin (Hb%) 16 g/dL
Mean corpuscular volume (MCV) 85 fL
Reticulocyte count 0.9%
Erythrocyte count 5 million/mm³
Thyroid-stimulating hormone 3.5 µU/mL
Urinalysis
Glucose Negative
Ketones Negative
Leucocytes Negative
Nitrite Negative
RBCs Negative
Casts Negative
Which of the following is the most likely diagnosis?
- A. Alzheimer’s dementia (Correct Answer)
- B. Creutzfeldt-Jakob disease
- C. Lewy body dementia
- D. Parkinson’s disease
- E. Vascular dementia
Pharmacotherapy for cognitive disorders Explanation: ***Alzheimer’s dementia***
- The patient presents with **progressive memory loss** and **confusion** that has worsened over a year, along with **agitational behavior** and difficulty with daily tasks (neglecting to put on socks), which are classic symptoms of Alzheimer's dementia.
- The **MMSE score of 20/30** indicates cognitive impairment, and the absence of other neurological findings or clear vascular risk factors supports this diagnosis.
*Creutzfeldt-Jakob disease*
- This is a rare, rapidly progressive, and fatal neurodegenerative disease that typically presents with **rapidly progressive dementia**, **myoclonus**, and other neurological signs, which are not described in this case.
- The patient's symptoms have progressed over a year, which is not as rapid as the typical course of CJD.
*Lewy body dementia*
- Characterized by **fluctuating cognition**, **recurrent visual hallucinations**, and **spontaneous parkinsonism**, which are not reported in this patient.
- While agitation can occur, the core features of Lewy body dementia are absent.
*Parkinson’s disease*
- Primarily a **movement disorder** characterized by **bradykinesia**, **rigidity**, **tremor**, and **postural instability**. While dementia can occur in later stages (Parkinson's disease dementia), the initial presentation in this patient is predominantly cognitive decline without prominent motor symptoms.
- The patient's physical examination is "unremarkable," suggesting an absence of parkinsonian motor signs.
*Vascular dementia*
- Typically associated with a history of **stroke** or significant **vascular risk factors** (e.g., uncontrolled hypertension, diabetes) and often presents with a **step-wise decline** in cognitive function.
- This patient has a largely unremarkable medical history, controlled blood pressure, and normal cholesterol, and a CT scan showed no pathological findings (e.g., infarcts), making vascular dementia less likely.
Pharmacotherapy for cognitive disorders US Medical PG Question 10: A 12-year-old boy is brought by his mother to a neurologist for continuing evaluation of seizures. His seizures were previously well-controlled on medication but over the last month he has been having seizures several times per week. The boy is non-verbal and has had severe developmental delays and cognitive disability since birth. On exam, the boy is found to be enthusiastically playing with the toys in the office and laughing at almost any stimulus. Furthermore, his movements are found to be uncoordinated with a wide based gait. Previous genetic testing has revealed an abnormality in an E3 ubiquitin ligase gene. Compared to unaffected individuals, which of the following patterns of gene expression is most likely seen in this patient?
- A. Abnormally increased expression of the gene from the maternal chromosome
- B. Abnormally decreased expression of the gene from the maternal chromosome (Correct Answer)
- C. Abnormally decreased expression of the gene from both chromosomes
- D. Abnormally decreased expression of the gene from the paternal chromosome
- E. Abnormally increased expression of the gene from the paternal chromosome
Pharmacotherapy for cognitive disorders Explanation: ***Abnormally decreased expression of the gene from the maternal chromosome***
- This patient's symptoms (non-verbal, severe developmental delays, cognitive disability, seizures, uncoordinated movements, wide-based gait, inappropriate laughter, and an abnormality in an E3 ubiquitin ligase gene) are characteristic of **Angelman syndrome**.
- Angelman syndrome is typically caused by a deletion or mutation on the **maternally inherited copy of chromosome 15q11-q13**, specifically affecting the *UBE3A* gene, which is an E3 ubiquitin ligase. This leads to reduced or absent expression of the *UBE3A* gene in critical brain regions where only the maternal allele is expressed.
*Abnormally increased expression of the gene from the maternal chromosome*
- Angelman syndrome is caused by a **loss of function** of the maternally inherited *UBE3A* gene, not an increase in its expression.
- Increased expression would not lead to the neurodevelopmental deficits seen in Angelman syndrome.
*Abnormally decreased expression of the gene from both chromosomes*
- While there is decreased expression of the functional *UBE3A* gene, the paternal allele is normally **silenced** in specific brain regions relevant to Angelman syndrome pathogenesis due to **genomic imprinting**. Therefore, the issue is with the maternal allele.
- If both chromosomes had decreased expression, it would imply a different genetic mechanism or a more severe, potentially lethal, condition.
*Abnormally decreased expression of the gene from the paternal chromosome*
- In the brain regions relevant to Angelman syndrome, the paternal *UBE3A* allele is normally **silenced** due to genomic imprinting. Therefore, its decreased expression would not be an abnormal finding or contribute to the pathology.
- Problems with the paternal allele in this region are associated with **Prader-Willi syndrome**, which has a different clinical presentation (e.g., hypotonia, hyperphagia, obesity).
*Abnormally increased expression of the gene from the paternal chromosome*
- The paternal *UBE3A* allele is normally **silenced** in the relevant brain regions; therefore, an increased expression would be abnormal but is not the genetic basis of Angelman syndrome.
- Angelman syndrome is caused by the **loss or absence of functional maternal *UBE3A*** expression, not altered paternal expression.
More Pharmacotherapy for cognitive disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.