Neuropsychological testing US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neuropsychological testing. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neuropsychological testing US Medical PG Question 1: A 66-year-old man is brought into the emergency department by his daughter for a change in behavior. Yesterday the patient seemed more confused than usual and was asking the same questions repetitively. His symptoms have not improved over the past 24 hours, thus the decision to bring him in today. Last year, the patient was almost completely independent but he then suffered a "series of falls," after which his ability to care for himself declined. After this episode he was no longer able to cook for himself or pay his bills but otherwise had been fine up until this episode. The patient has a past medical history of myocardial infarction, hypertension, depression, diabetes mellitus type II, constipation, diverticulitis, and peripheral neuropathy. His current medications include metformin, insulin, lisinopril, hydrochlorothiazide, sodium docusate, atorvastatin, metoprolol, fluoxetine, and gabapentin. On exam you note a confused man who is poorly kept. He has bruises over his legs and his gait seems unstable. He is alert to person and place, and answers some questions inappropriately. The patient's pulse is 90/minute and his blood pressure is 170/100 mmHg. Which of the following is the most likely diagnosis?
- A. Normal aging
- B. Lewy body dementia
- C. Vascular dementia (Correct Answer)
- D. Pseudodementia (depression-related cognitive impairment)
- E. Alzheimer's dementia
Neuropsychological testing Explanation: ***Vascular dementia***
- This diagnosis is strongly supported by the patient's **stepwise decline** in cognitive function following a "series of falls" (likely small strokes or transient ischemic attacks) and his extensive history of **vascular risk factors** including hypertension, diabetes, and previous myocardial infarction.
- The acute worsening of confusion over 24 hours, coupled with pre-existing impaired executive function (inability to cook or pay bills), is characteristic of **vascular dementia's fluctuating course** and presentation often linked to new cerebrovascular events.
*Incorrect: Normal aging*
- **Normal aging** involves a very gradual and mild decline in cognitive functions, primarily affecting processing speed and memory recall, without significant impairment in daily activities.
- This patient's rapid, stepwise decline and inability to perform instrumental activities of daily living (IADLs) such as cooking and managing finances go beyond what is considered normal cognitive changes with aging.
*Incorrect: Lewy body dementia*
- **Lewy body dementia** is characterized by prominent **fluctuations in attention and alertness**, recurrent visual hallucinations, and spontaneous parkinsonism, none of which are explicitly mentioned as primary features in this patient's presentation.
- While fluctuations in confusion are present, the history of a clear stepwise decline post-falls and significant vascular risk factors points away from Lewy body dementia as the most likely primary cause.
*Incorrect: Pseudodementia (depression-related cognitive impairment)*
- **Pseudodementia** refers to cognitive impairment that occurs in the context of **major depression**, where patients may exhibit poor concentration, memory difficulties, and psychomotor slowing that mimics dementia.
- While this patient is on fluoxetine for depression, the **stepwise decline** after clear vascular events (falls), multiple vascular risk factors, and impaired executive function point to a true neurodegenerative process rather than depression-induced cognitive changes, which typically improve with treatment of the underlying mood disorder.
*Incorrect: Alzheimer's dementia*
- **Alzheimer's dementia** typically presents with a **gradual and progressive decline** in memory, particularly episodic memory, followed by other cognitive domains over several years.
- The patient's history of a clear **stepwise decline** in function after acute events (falls) and the strong presence of **vascular risk factors** make vascular dementia a more fitting diagnosis than Alzheimer's, which is not typically associated with such a sudden, step-like progression.
Neuropsychological testing US Medical PG Question 2: A 72-year-old man is brought to the physician by his wife for forgetfulness, confusion, and mood changes for the past 4 months. His symptoms started with misplacing items such as his wallet and keys around the house. Two months ago, he became unable to manage their finances as it became too difficult for him. Last week, he became lost while returning home from the grocery store. His wife reports that he shows “no emotion” and that he is seemingly not concerned by his recent symptoms. He has hypertension, type 2 diabetes mellitus, and coronary artery disease. Current medications include aspirin, metoprolol, lisinopril, metformin, and rosuvastatin. His pulse is 56/min and blood pressure is 158/76 mm Hg. Neurologic examination shows loss of sensation on his right leg and an unsteady gait. When asked to stand with his eyes closed and palms facing upward, his right arm rotates inward. An MRI of the brain shows multiple deep white matter lesions. Which of the following is the most likely diagnosis?
- A. Vitamin B12 deficiency
- B. Frontotemporal dementia
- C. Alzheimer disease
- D. Lewy body dementia
- E. Vascular dementia (Correct Answer)
Neuropsychological testing Explanation: ***Vascular dementia***
- The patient's history of **hypertension, type 2 diabetes mellitus, and coronary artery disease** indicates significant vascular risk factors. The **multiple deep white matter lesions** on MRI are characteristic findings in vascular dementia, resulting from chronic **cerebral ischemia**.
- The **insidious onset** with progressive **cognitive decline** (forgetfulness, confusion, financial difficulties, getting lost) combined with **focal neurological deficits** (loss of sensation, unsteady gait, pronator drift), and "no emotion" or lack of concern, strongly points towards vascular dementia.
*Vitamin B12 deficiency*
- While vitamin B12 deficiency can cause cognitive impairment and neurological symptoms, it typically manifests with **megaloblastic anemia** and **peripheral neuropathy**, which are not noted in this case.
- The MRI findings of **multiple deep white matter lesions** are not characteristic of vitamin B12 deficiency, and the patient's extensive vascular risk factors are more indicative of a cerebrovascular etiology.
*Frontotemporal dementia*
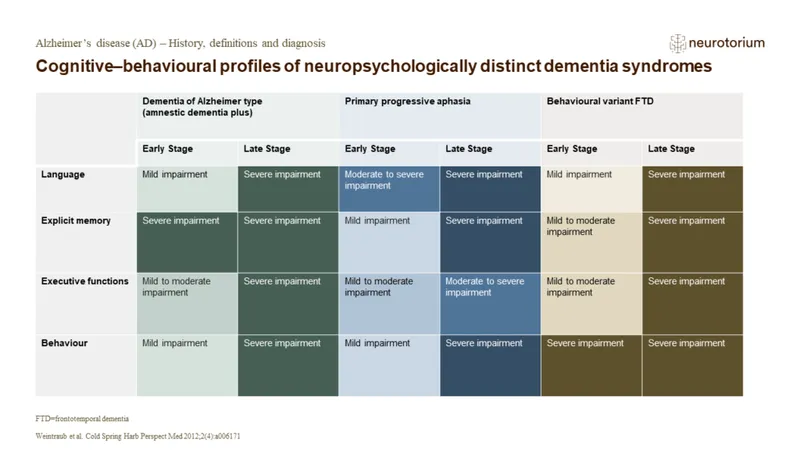
- Characterized primarily by **early and prominent behavioral and personality changes** (e.g., disinhibition, apathy) or **language deficits**. While apathy is present ("no emotion"), the prominent **focal neurological deficits** and MRI findings of deep white matter lesions are less typical.
- Unlike this case, memory impairment is usually not the initial or most prominent symptom in frontotemporal dementia until later stages, which contrasts with the patient's initial presentation of forgetfulness.
*Alzheimer disease*
- Alzheimer disease typically presents with **progressive memory impairment** as the hallmark symptom, often preceding other cognitive or neurological deficits. While memory loss is present here, the rapid progression (4 months), prominent focal neurological signs, and vascular risk factors are less typical.
- MRI would typically show **cortical atrophy**, particularly in the hippocampus and medial temporal lobes, rather than multiple deep white matter lesions without significant atrophy.
*Lewy body dementia*
- Key features include **fluctuating cognition, recurrent visual hallucinations**, and spontaneous **parkinsonism**. None of these core features are explicitly described in the patient's presentation.
- While mood changes and apathy can occur, the presence of **focal neurological deficits** and deep white matter lesions on MRI are not primary characteristics of Lewy body dementia.
Neuropsychological testing US Medical PG Question 3: A 75-year-old female presents to your office with her daughter. The patient states that she feels perfectly well and that she does not know why she is present. The daughter states that over the last several years, the patient has become forgetful and recently forgot her grandchild's name, along with the groceries she was supposed to buy. She was also found lost 10 miles away from her house last week. The daughter also states that the patient has had urinary incontinence over the last few months and has been seeing little children in the morning that are not present. The patient denies any recent falls. Her vitals are normal and her physical exam does not reveal any focal neurological deficits. Her mini-mental status exam is scored 22/30. What is the most accurate test for this patient?
- A. CT angiography of head
- B. CT scan of head
- C. Lumbar puncture
- D. MRI scan of head (Correct Answer)
- E. PET scan of head
Neuropsychological testing Explanation: ***MRI scan of head***
- An MRI scan of the head is the **most accurate initial test** to evaluate cognitive decline and rule out structural/reversible causes of dementia.
- This patient's presentation includes **progressive memory loss, disorientation, urinary incontinence, and visual hallucinations** - suggestive of **Lewy Body Dementia (LBD)** or potentially **Normal Pressure Hydrocephalus (NPH)**, though gait disturbance (a key NPH feature) is notably absent.
- MRI provides detailed visualization of **brain atrophy patterns**, **ventricular enlargement** (for NPH), **white matter lesions** (vascular dementia), **hippocampal atrophy** (Alzheimer's), and excludes other reversible causes like **subdural hematoma, tumor, or stroke**.
- **Must be performed first** before any invasive procedures like lumbar puncture.
*CT scan of head*
- A CT scan is useful for acute conditions like **hemorrhage, stroke, or mass lesions**, but it is **significantly less sensitive** than MRI for detecting subtle changes critical for dementia diagnosis.
- Cannot adequately visualize **cortical atrophy, hippocampal volume loss, or subtle white matter changes** that help differentiate dementia subtypes.
- While faster and more accessible, it is not the "most accurate" test for cognitive decline evaluation.
*CT angiography of head*
- CT angiography specifically visualizes **blood vessels** to detect **aneurysms, stenoses, or vascular malformations**.
- While vascular disease can contribute to dementia, this test does not evaluate the **brain parenchyma** or structural changes necessary for diagnosing neurodegenerative conditions.
- Not indicated as the initial test for cognitive impairment without focal vascular symptoms.
*Lumbar puncture*
- Lumbar puncture analyzes **cerebrospinal fluid (CSF)** for biomarkers (**amyloid-beta, tau, alpha-synuclein**), infection, or inflammation.
- It is an **invasive procedure** that should only be performed **after neuroimaging** to rule out increased intracranial pressure, hydrocephalus, or mass lesions.
- While useful for confirming specific dementia diagnoses (e.g., Alzheimer's or LBD biomarkers), it is a **second-line test**, not the initial most accurate diagnostic study.
*PET scan of head*
- PET imaging (FDG-PET or amyloid-PET) measures **metabolic activity** or **specific protein deposits** and is highly specific for certain dementias like **Alzheimer's disease** or **Frontotemporal dementia**.
- It is typically a **specialized second-line test** used after structural imaging when the diagnosis remains unclear.
- **More expensive and less available** than MRI, and not necessary as the initial most accurate test for broad cognitive impairment evaluation.
Neuropsychological testing US Medical PG Question 4: A 82-year-old woman is brought to the physician by her son because he is concerned about her forgetfulness for the past 2 years. She occasionally walks into a room and forgets why she went there and often forgets where she left her keys. She is sometimes unable to recall a familiar individual's name. She reports that she has become slower at completing sudoku puzzles. She has been living independently since the death of her husband 3 years ago. She goes shopping, cooks her own meals, and plays bridge with her friends every weekend. She is not anxious about her memory lapses. She has no trouble sleeping but has been getting up earlier than she used to. She has hypertension that is managed with hydrochlorothiazide. She appears healthy. Vital signs are within normal limits. She is oriented to person, place, and time. Examination shows a normal gait. She describes her mood as “good” and her speech is normal. Her thought process is organized and her judgement is intact. She makes one error when performing serial sevens. The remainder of the examination shows no abnormalities. Which of the following is the most likely cause of this patient's symptoms?
- A. Alzheimer's disease
- B. Normal pressure hydrocephalus
- C. Vascular dementia
- D. Lewy-body dementia
- E. Aging (Correct Answer)
Neuropsychological testing Explanation: ***Aging***
- The patient exhibits mild, age-associated cognitive changes such as occasional forgetfulness and slower cognitive processing (sudoku puzzles), without significant functional impairment in daily activities. This aligns with **normal cognitive aging**.
- Her ability to live independently, manage finances, perform household tasks, and engage in social activities (playing bridge) indicates that these memory lapses do not meet the criteria for a dementia syndrome.
*Alzheimer's disease*
- Alzheimer's disease typically presents with more pervasive and progressive memory loss, significantly impacting daily activities and **instrumental activities of daily living (IADLs)**, which are preserved in this patient.
- While forgetfulness is present, it's not severe enough to suggest the **pathological changes** characteristic of Alzheimer's, such as marked impairment in multiple cognitive domains and functional decline.
*Normal pressure hydrocephalus*
- This condition is characterized by the classic triad of **gait disturbance**, **urinary incontinence**, and **dementia (cognitive impairment)**.
- The patient has no issues with gait or urinary incontinence, and her cognitive symptoms are mild and do not constitute dementia.
*Vascular Dementia*
- Vascular dementia is usually associated with a history of **strokes** or significant **vascular risk factors** leading to step-wise cognitive decline.
- The patient's hypertension is managed, and there is no evidence of focal neurological deficits, stroke history, or a fluctuating course often seen in vascular dementia.
*Lewy-body dementia*
- Key features of Lewy body dementia include **fluctuating cognition**, **recurrent visual hallucinations**, and **spontaneous parkinsonism**.
- None of these defining symptoms are present in the patient's presentation; her mood is good, and her gait is normal.
Neuropsychological testing US Medical PG Question 5: A 77-year-old woman is brought to the physician for gradually increasing confusion and difficulty walking for the past 4 months. Her daughter is concerned because she has been forgetful and seems to be walking more slowly. She has been distracted during her weekly bridge games and her usual television shows. She has also had increasingly frequent episodes of urinary incontinence and now wears an adult diaper daily. She has hyperlipidemia and hypertension. Current medications include lisinopril and atorvastatin. Her temperature is 36.8°C (98.2°F), pulse is 84/min, respirations are 15/min, and blood pressure is 139/83 mmHg. She is confused and oriented only to person and place. She recalls 2 out of 3 words immediately and 1 out of 3 after five minutes. She has a broad-based gait and takes short steps. Sensation is intact and muscle strength is 5/5 throughout. Laboratory studies are within normal limits. Which of the following is the most likely diagnosis in this patient?
- A. Pseudodementia
- B. Normal pressure hydrocephalus (Correct Answer)
- C. Creutzfeldt-Jakob disease
- D. Frontotemporal dementia
- E. Dementia with Lewy-bodies
Neuropsychological testing Explanation: ***Normal pressure hydrocephalus***
- The constellation of **gradually increasing confusion**, an **ataxic gait** (broad-based, short steps), and **urinary incontinence** in an elderly patient is the classic triad of **normal pressure hydrocephalus (NPH)**.
- Lumbar puncture with temporary symptom improvement or **neuroimaging** showing ventriculomegaly without significant sulcal atrophy would further support this diagnosis.
*Pseudodementia*
- **Pseudodementia** is a cognitive impairment primarily caused by **depression**, characterized by rapid onset of symptoms and often a history of mood disturbances.
- The patient's progressive decline over 4 months and lack of overt depressive symptoms make this less likely.
*Creutzfeldt-Jakob disease*
- **Creutzfeldt-Jakob disease (CJD)** is a rapidly progressive and fatal neurodegenerative disorder characterized by a very fast decline in cognitive function, typically over months, along with **myoclonus**, ataxia, and other neurological signs.
- The slower, more subtle progression of symptoms and absence of myoclonus make CJD less likely.
*Frontotemporal dementia*
- **Frontotemporal dementia (FTD)** usually presents with prominent early changes in **personality, behavior**, or **language (aphasia)**, rather than the classic NPH triad.
- While confusion can occur, gait disturbance and incontinence are not typically primary or early features.
*Dementia with Lewy-bodies*
- **Dementia with Lewy bodies (DLB)** is characterized by **fluctuating cognition**, **recurrent visual hallucinations**, and **spontaneous parkinsonism**.
- While gait disturbance can occur (parkinsonism), the absence of hallucinations and significant cognitive fluctuations makes NPH a more fitting diagnosis for the specific triad presented.
Neuropsychological testing US Medical PG Question 6: A 75-year-old woman presents to her primary care physician with her son because she is convinced that people are stealing from her. Her son claims she has been misplacing her medications and money throughout the house. She recently lost her husband to old age and has become reclusive and no longer wants people to visit. Physical examination is unremarkable and the patient is oriented to person, time, and place. A mini-mental status examination (MMSE) is performed and she has difficulty recalling words after 5 minutes and also has problems with serial subtraction. Which of the following is the most likely diagnosis in this patient?
- A. Histrionic personality disorder
- B. Schizophrenia
- C. Delirium
- D. Schizoid personality disorder
- E. Dementia (Correct Answer)
Neuropsychological testing Explanation: ***Dementia***
- The patient has **primary cognitive impairment** evidenced by MMSE deficits (poor delayed recall, impaired serial subtraction) and functional decline (misplacing items).
- Her **delusions of theft are secondary to dementia**, a common behavioral and psychological symptom of dementia (BPSD), particularly in Alzheimer's disease.
- The **insidious onset** in a 75-year-old with progressive memory decline points to a neurodegenerative process.
- Orientation remains intact in early-to-moderate dementia, which doesn't rule out the diagnosis.
- The stressor (husband's death) may have unmasked or accelerated symptom recognition but doesn't explain the cognitive deficits.
*Histrionic personality disorder*
- Characterized by **excessive emotionality** and **attention-seeking behavior**, which are not evident in this presentation.
- Personality disorders are lifelong patterns, not new-onset conditions in elderly patients with cognitive decline.
- Does not explain the objective cognitive deficits on MMSE.
*Schizophrenia*
- Schizophrenia typically has onset in **late adolescence to early adulthood**, not at age 75.
- While late-onset schizophrenia exists, the **prominent cognitive impairment** (memory, executive function) as the PRIMARY feature points toward dementia rather than a primary psychotic disorder.
- Schizophrenia would show more pervasive psychotic symptoms without the specific pattern of memory and executive dysfunction seen here.
*Delirium*
- Delirium has **acute onset** (hours to days) with **fluctuating consciousness** and altered attention.
- This patient is **oriented to person, time, and place** and has a gradual, progressive course (misplacing items over time).
- No mention of acute medical illness, medication changes, or rapid cognitive fluctuation.
*Schizoid personality disorder*
- A lifelong pattern of **social detachment** and restricted emotional expression, not a new condition in late life.
- Does not explain the cognitive impairment, memory deficits, or delusional beliefs.
- The patient's reclusiveness is reactive to recent loss and concerns about theft, not a longstanding personality trait.
Neuropsychological testing US Medical PG Question 7: A 78-year-old man is brought to the physician by his daughter for a follow-up examination. The daughter noticed that he has gradually become more forgetful and withdrawn over the last year. He frequently misplaces his car keys and forgets the names of his neighbors, whom he has known for 30 years. He has difficulty recalling his address and telephone number. He recently had an episode of urinary and fecal incontinence. Last week, his neighbor found him wandering the parking lot of the grocery store. He has hypertension and hyperlipidemia. He had smoked one pack of cigarettes daily for 40 years but quit 18 years ago. His current medications include hydrochlorothiazide and atorvastatin. He appears healthy; BMI is 23 kg/m2. His temperature is 37.2°C (99.0°F), pulse is 86/min, respirations are 14/min, and blood pressure is 136/84 mm Hg. Mini-mental state examination score is 19/30. He is not bothered by his forgetfulness. Cranial nerves II–XII are intact. He has 5/5 strength and full sensation to light touch in all extremities. His patellar, Achilles, and biceps reflexes are 2+ bilaterally. His gait is steady. MRI scan of the brain shows ventriculomegaly and prominent cerebral sulci. Which of the following is the most appropriate pharmacotherapy?
- A. Acetazolamide
- B. Sertraline
- C. Memantine
- D. Thiamine
- E. Donepezil (Correct Answer)
Neuropsychological testing Explanation: ***Donepezil***
- The patient exhibits features consistent with **Alzheimer's disease**, including gradual memory loss, difficulty with daily tasks, episodes of incontinence, and a Mini-Mental State Examination (MMSE) score of 19/30. Donepezil, a **cholinesterase inhibitor**, is a first-line treatment for mild to moderate Alzheimer's to slow cognitive decline.
- The MRI findings of **ventriculomegaly and prominent cerebral sulci** are consistent with general cerebral atrophy often seen in Alzheimer's disease, not hydrocephalus requiring shunting or other specific brain pathologies (normal pressure hydrocephalus would have gait disturbance as a prominent feature, which is absent here).
*Acetazolamide*
- **Acetazolamide** is a **carbonic anhydrase inhibitor** used to treat conditions like glaucoma, altitude sickness, and idiopathic intracranial hypertension.
- There is no indication of elevated intracranial pressure or hydrocephalus that would warrant the use of acetazolamide in this patient.
*Sertraline*
- **Sertraline** is a **selective serotonin reuptake inhibitor (SSRI)** primarily used to treat depression, anxiety disorders, and obsessive-compulsive disorder.
- While depression can coexist with dementia, the primary cognitive symptoms described here are not primarily depressive; therefore, an antidepressant is not the most appropriate initial pharmacotherapy for cognitive decline.
*Memantine*
- **Memantine** is an **NMDA receptor antagonist** used in moderate to severe Alzheimer's disease, often in combination with cholinesterase inhibitors or when cholinesterase inhibitors are not tolerated.
- While appropriate for moderate to severe Alzheimer's, **cholinesterase inhibitors** are typically the initial treatment for mild to moderate stages, and the patient's MMSE score of 19/30 often falls into the mild-moderate category where donepezil is usually favored first.
*Thiamine*
- **Thiamine** (vitamin B1) supplementation is primarily used to treat **Wernicke-Korsakoff syndrome**, which is associated with chronic alcohol abuse and presents with ataxia, ophthalmoplegia, and confusion, none of which are the primary presenting symptoms here.
- There is no evidence of **nutritional deficiency** or alcohol abuse in this patient to suggest thiamine deficiency as the cause of his cognitive decline.
Neuropsychological testing US Medical PG Question 8: A 73-year-old woman is brought to the physician by her son because of increasing forgetfulness over the past 2 years. Initially, she used to misplace keys and forget her dog's name or her phone number. Now, she often forgets about what she has seen on television or read about the day before. She used to go for a walk every morning but stopped one month ago after she became lost on her way back home. Her son has prevented her from cooking because she has had episodes of leaving the gas stove on after making a meal. She becomes agitated when asked questions directly but is unconcerned when her son reports her history and says he is overprotective of her. She has hypertension, coronary artery disease, and hypercholesterolemia. Current medications include aspirin, enalapril, carvedilol, and atorvastatin. She is alert and oriented to place and person but not to time. Vital signs are within normal limits. Short- and long-term memory deficits are present. Her speech rhythm is normal but is frequently interrupted as she thinks of words to frame her sentences. She makes multiple errors while performing serial sevens. Her clock drawing is impaired and she draws 14 numbers. Which of the following is the most likely diagnosis?
- A. Lewy-body dementia
- B. Alzheimer disease (Correct Answer)
- C. Frontotemporal dementia
- D. Normal pressure hydrocephalus
- E. Creutzfeldt-Jakob disease
Neuropsychological testing Explanation: **Alzheimer disease**
- The patient's presentation with **progressive memory impairment** (misplacing keys, forgetting recent events), **executive dysfunction** (getting lost, leaving stove on, impaired clock drawing), and **language difficulties** (word-finding pauses) over 2 years is highly characteristic of Alzheimer disease.
- The **insidious onset** and gradual cognitive decline affecting multiple domains, along with relative preservation of motor function initially, are key diagnostic features.
*Lewy-body dementia*
- This condition is often characterized by **fluctuating cognition**, **visual hallucinations**, and **parkinsonism**, none of which are prominent in this patient's presentation.
- While memory impairment can occur, the core features of Lewy body dementia are not described here.
*Frontotemporal dementia*
- **Early behavioral changes** (e.g., disinhibition, apathy) or **prominent language deficits** (e.g., aphasia without initial memory problems) are common in frontotemporal dementia.
- This patient's primary complaint is memory loss, and behavioral changes are reactive rather than disinhibited, making frontotemporal dementia less likely.
*Normal pressure hydrocephalus*
- The classic triad for normal pressure hydrocephalus includes **gait disturbance**, **urinary incontinence**, and **dementia**.
- While dementia is present, there is no mention of gait abnormalities or urinary issues in this patient.
*Creutzfeldt-Jakob disease*
- This is a rapidly progressive and fatal neurodegenerative disorder with a typical course of **weeks to months**, not 2 years.
- It usually presents with **myoclonus**, **ataxia**, and **rapidly progressive dementia**, which are not seen in this case.
Neuropsychological testing US Medical PG Question 9: A 77-year-old woman is brought to her primary care provider by her daughter with behavioral changes and an abnormally bad memory for the past few months. The patient’s daughter says she sometimes gets angry and aggressive while at other times she seems lost and stares at her surroundings. Her daughter also reports that she has seen her mother talking to empty chairs. The patient says she sleeps well during the night but still feels sleepy throughout the day. She has no problems getting dressed and maintaining her one bedroom apartment. Past medical history is significant for mild depression and mild osteoporosis. Current medications include escitalopram, alendronic acid, and a multivitamin. The patient is afebrile, and her vital signs are within normal limits. On physical examination, the patient is alert and oriented and sitting comfortably in her chair. A mild left-hand tremor is noted. Muscle strength is 5 out of 5 in the upper and lower extremities bilaterally, but muscle tone is slightly increased. She can perform repetitive alternating movements albeit slowly. She walks with a narrow gait and has mild difficulty turning. Which of the following is the most likely diagnosis in this patient?
- A. Lewy body dementia (Correct Answer)
- B. Alzheimer's disease
- C. Serotonin syndrome
- D. Frontotemporal dementia
- E. Delirium
Neuropsychological testing Explanation: ***Lewy body dementia***
- This patient exhibits **fluctuating cognition** (being lost and staring, behavioral changes), **recurrent visual hallucinations** (talking to empty chairs), and spontaneous motor features of **parkinsonism** (mild left-hand tremor, increased muscle tone, slow alternating movements, narrow gait, difficulty turning), all core features of Lewy body dementia.
- The **insidious onset** and progressive decline over months, along with the symptom triad, fit the diagnostic criteria for Lewy body dementia.
*Alzheimer's disease*
- While Alzheimer's involves memory loss and cognitive decline, it is not typically associated with **prominent early visual hallucinations** or **parkinsonian features** at presentation.
- Alzheimer's disease often presents with **memory impairment as the most prominent early symptom**, often preceding other cognitive deficits by years.
*Serotonin syndrome*
- This is an acute drug reaction characterized by a triad of **mental status changes**, **autonomic hyperactivity**, and **neuromuscular abnormalities**, usually developing rapidly after medication changes affecting serotonin levels.
- The patient's symptoms have been present for months, the vital signs are stable, and her medications (escitalopram) have been stable, making an **acute syndrome** like serotonin syndrome unlikely.
*Frontotemporal dementia*
- This type of dementia primarily affects personality, behavior, and language, with **prominent disinhibition or apathy**.
- While behavioral changes are present, the patient's prominent **visual hallucinations** and **parkinsonian features** are not characteristic of frontotemporal dementia.
*Delirium*
- Delirium is characterized by an **acute onset** and fluctuating course of attention and awareness, often triggered by an underlying medical condition, medication, or infection.
- The patient's symptoms have progressed over **several months**, rather than hours or days, and she is afebrile with stable vital signs, making delirium less likely.
Neuropsychological testing US Medical PG Question 10: A 68-year-old man, accompanied by his wife, presents to his physician with cognitive decline and hallucinations. The patient’s wife tells that his cognitive impairment progressed gradually over the past 6 years, and first began with problems counting and attention. The hallucinations began approximately a year ago. The patient describes them as realistic and non-frightening; most often, he sees his cat accompanying him everywhere he goes. The patient’s wife also notes frequent episodes of staring spells in her husband and prolonged daytime napping. The blood pressure is 130/80 mm Hg with the orthostatic change to 110/60 mm Hg, heart rate is 75/min, respiratory rate is 13/min, and the temperature is 36.6°C (97.8°F). The patient is alert and responsive, but he is disoriented to time and place. He is pale and hypomimic. The cardiac, lung, and abdominal examinations are within normal limits for the patient’s age. The neurological examination is significant for a bilateral symmetrical cogwheel rigidity in the upper extremities. What would you most likely see on additional radiological investigations?
- A. Multiple lacunar infarcts on MRI
- B. Marked hippocampal atrophy on MRI
- C. Hypoperfusion and hypometabolism in frontal lobes on SPECT
- D. Decreased perfusion and dopaminergic activity in occipital lobes on PET (Correct Answer)
- E. Pontine 'hot-cross bun' sign on MRI
Neuropsychological testing Explanation: ***Decreased perfusion and dopaminergic activity in occipital lobes on PET***
- This finding is characteristic of **dementia with Lewy bodies (DLB)**, which is strongly suggested by the patient's presentation with **cognitive fluctuations**, **visual hallucinations** (non-frightening, realistic), **parkinsonism** (cogwheel rigidity), and **REM sleep behavior disorder** (daytime napping/staring spells could be a manifestation). PET scans in DLB often show reduced occipital lobe uptake.
- The combination of **parkinsonism** (cogwheel rigidity) and **visual hallucinations** preceding or appearing early in the course of cognitive decline is a hallmark of DLB, which differentiates it from other dementias.
*Multiple lacunar infarcts on MRI*
- While lacunar infarcts can cause cognitive decline (**vascular dementia**), the clinical picture of prominent, well-formed visual hallucinations, parkinsonism, and cognitive fluctuations is less typical for purely vascular dementia.
- Vascular dementia usually presents with a step-wise decline in cognition and focal neurological deficits, which are not the primary features here.
*Marked hippocampal atrophy on MRI*
- **Hippocampal atrophy** is a hallmark of **Alzheimer's disease**, which typically presents with insidious memory loss as the primary symptom.
- The prominent early visual hallucinations and parkinsonism are not typical initial features of Alzheimer's disease.
*Hypoperfusion and hypometabolism in frontal lobes on SPECT*
- **Frontal lobe hypoperfusion/hypometabolism** on SPECT/PET is characteristic of **frontotemporal dementia (FTD)**.
- FTD typically presents with early behavioral changes or language deficits, not prominent visual hallucinations, parkinsonism, or significant cognitive fluctuations in the way seen in this patient.
*Pontine 'hot-cross bun' sign on MRI*
- The **'hot-cross bun' sign** on MRI is pathognomonic for **multiple system atrophy (MSA)**, specifically the **MSA-C subtype (cerebellar)**.
- While MSA can cause parkinsonism and autonomic dysfunction, it typically does not feature prominent visual hallucinations or significant cognitive decline as early and striking features as seen in this patient.
More Neuropsychological testing US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.